
For decades, Hirudoid has been a mainstay in treating skin trauma, vein inflammation, and scarring. But what makes it clinically effective? And how do its different formulations—Hirudoid Cream, Gel, and Forte—serve distinct therapeutic purposes?
In this post, we delve into the science of mucopolysaccharide polysulfate (MPS), the key active component in Hirudoid, and how this drug works, how it’s used, and what makes each variant unique. We’ll also highlight insights from official medication guidelines and analyze how Hirudoid fits into the modern innovation landscape in topical therapies through PatSnap Eureka AI Agent..
What is Hirudoid?
Hirudoid is a topical medication primarily used to treat bruises, inflammation, and superficial vein conditions like thrombophlebitis. Its active ingredient is mucopolysaccharide polysulfate (MPS), a compound with anti-inflammatory, antithrombotic, and fibrinolytic (blood clot–dissolving) properties.
The Evolution of Hirudoid: From Leech Secretions to Modern Topical Therapy
Eureka Technical Q&A reveals how modern Hirudoid formulations are optimized for enhanced skin retention, absorption, and bioactivity, while minimizing systemic exposure and side effects.
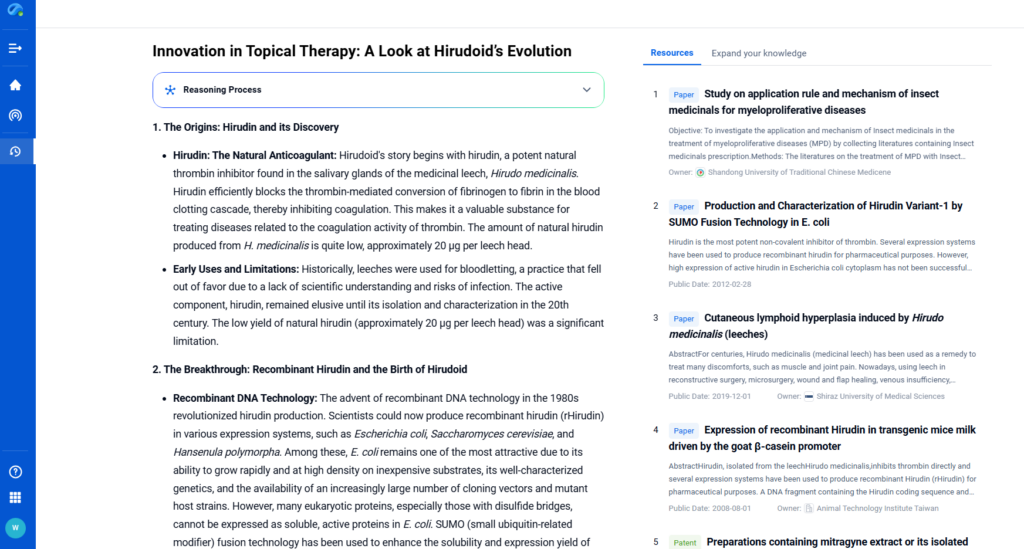
The Origins: Hirudin and Its Discovery
Hirudoid traces its roots to hirudin, a strong natural anticoagulant found in the saliva of Hirudo medicinalis (medicinal leech). Hirudin blocks thrombin, preventing the conversion of fibrinogen to fibrin, which stops blood clotting. This made it useful in treating clot-related conditions. However, the natural yield was very low—about 20 µg per leech—limiting its use.

Leeches were once used for bloodletting, but the practice declined due to infection risks and poor scientific understanding. Hirudin remained largely unexplored until isolated and studied in the 20th century.
The Breakthrough: Recombinant Hirudin and the Birth of Hirudoid
In the 1980s, recombinant DNA technology transformed hirudin production. Scientists began producing recombinant hirudin (rHirudin) using systems like E. coli, S. cerevisiae, and H. polymorpha. Among these, E. coli offered fast growth and high yield, although expressing complex proteins remained challenging. SUMO fusion technology helped improve protein solubility and expression.
These advances led to the development of Hirudoid Cream, a topical drug used to treat bruises, swelling, and superficial thrombophlebitis. Launched by Luitpold Welk Pharmaceuticals in Germany, Hirudoid offered localized treatment with minimal systemic side effects.
The Evolution: Innovations in Formulation and Application
Hirudoid’s formulation has improved to boost stability, absorption, and skin retention. Eureka Technical Q&A explores how these advancements enhance topical bioavailability and ensure consistent therapeutic delivery through optimized excipients and delivery systems. Modern versions use optimized excipients and have explored adding cannabinoids or alkaloids to enhance bioactivity while reducing dosage and side effects. Topical delivery makes Hirudoid ideal for localized skin conditions.
Researchers have tested Hirudoid in broader settings, including osteoarthritis, tendinitis, and post-surgical swelling. While hirudotherapy offers benefits, some patients experienced adverse reactions like skin inflammation or papules following leech use. Studies suggest that Hirudoid mimics therapeutic mechanisms without such risks.
It also works well with combination therapies. In one study, using Hirudoid with ice packs significantly reduced Gemcitabine-induced phlebitis compared to ice alone (5% vs. 20% incidence).
The Future: Ongoing Research and Potential Developments
New delivery methods—such as liposomes and nanoparticles—aim to improve how hirudin penetrates the skin. Enhancers and ethosomal carriers show potential for poorly soluble molecules like THC and mitragynine.
Advances in genomics could enable personalized Hirudoid therapies. In studies on myeloproliferative disorders, components from Hirudo and Pheretima targeted hundreds of biological pathways. Key ingredients like ursolic acid showed strong binding to proteins involved in cancer and inflammation.
Future research may expand Hirudoid’s uses. Pathway enrichment analyses link its compounds to conditions like cancer, atherosclerosis, and apoptosis, suggesting broader therapeutic potential.
Mechanism of Action
Hirudoid is a topical medication primarily known for its anti-inflammatory and antithrombotic effects, making it effective in treating issues like poor circulation, swelling, and superficial vein disorders. It works by reducing inflammation and preventing blood clots in affected tissues.
PatSnap Eurekaanalyzes how Hirudoid’s dual-action profile—targeting both inflammation and thrombus formation—contributes to faster healing in localized vascular and soft tissue conditions.

Anti-Inflammatory Effects
Hirudoid’s anti-inflammatory properties are primarily attributed to its ability to reduce inflammation and swelling in the affected area. This is achieved through several mechanisms:
- Inhibition of Pro-Inflammatory Mediators: It helps in reducing the levels of pro-inflammatory mediators such as prostaglandins and leukotrienes, which are responsible for causing inflammation and swelling.
- Reduction of Capillary Permeability: It reduces the permeability of capillaries, which helps in preventing the leakage of fluid and proteins into the surrounding tissues, thereby reducing swelling and inflammation.
- Promotion of Tissue Repair: Hirudoid promotes the repair of damaged tissues by stimulating the production of collagen and other extracellular matrix components.
Antithrombotic Effects
The antithrombotic effects of Hirudoid are mainly due to the presence of heparinoids, such as chondroitin sulfate, which are similar in structure and function to heparin. These heparinoids exert their antithrombotic effects through the following mechanisms:
- Enhancement of Antithrombin III Activity: Heparinoids bind to antithrombin III, a natural anticoagulant in the blood, and enhance its activity. This increased activity leads to the inhibition of thrombin and other clotting factors, thereby preventing the formation of blood clots.
- Inhibition of Thrombin: Thrombin is a key enzyme in the blood clotting process that converts fibrinogen to fibrin, forming a blood clot. By inhibiting thrombin, heparinoids prevent the formation of fibrin and thus prevent blood clot formation.
- Prevention of Platelet Aggregation: Heparinoids also help in preventing the aggregation of platelets, which are essential for the formation of blood clots.
Three Key Forms of Hirudoid
While the core ingredient—MPS—remains the same, Hirudoid is available in three main forms tailored to different needs:Hirudoid Cream, Gel, anHirudoid Forte. They are all topical medications containing mucopolysaccharide polysulfate (MPS) as the active ingredient. MPS is a heparinoid, which means it has similar properties to heparin, including anticoagulant and anti-inflammatory effects. The main differences between these products lie in their formulations, consistency, and potentially their concentrations of active ingredients, which may affect their intended uses and how they are applied.
Hirudoid Cream
- Consistency: A smooth, white cream.
- Active Ingredient Concentration: The concentration of MPS in Hirudoid Cream is typically 0.3% (3 mg/g).
- Intended Use: Hirudoid commonly prevents and treats various skin conditions and circulatory problems. It effectively prevents phlebitis after PICC catheterization in cancer patients, showing no significant difference in incidence or severity versus a wet-hot compress. Studies have also proven its efficacy in treating postinfusion phlebitis, though it may require more applications than Notoginseny cream to match results. Hirudoid cream works effectively and safely for infantile dry sub-acute eczema, achieving a 75.3% total effective rate versus 53.7% for heparin sodium cream. A meta-analysis confirms its superiority to magnesium sulfate in preventing and treating chemotherapy-induced phlebitis in cancer patients. Additionally, it prevents psoriasis-like dermatitis in mice by inhibiting IL-17A and TNF-α expression. Topical Hirudoid cream partially counteracts glucocorticoid-induced epidermal changes, such as transepidermal water loss (TEWL) and barrier function impairment.编辑分享
- Can you provide some examples of how to use Hirudoid in active voice?
- How can I ensure that the active voice sentences are clear and easy to understand?
- Are there any specific rules or guidelines for converting passive voice to active voice?

Hirudoid Gel
- Consistency: It has a lighter, less greasy texture than the cream, making it easier to spread and absorb.
- Active Ingredient Concentration: The concentration of MPS in Hirudoid Gel is typically the same as in the cream, 0.3% (3 mg/g).
- Intended Use: People often prefer it for larger body areas or conditions requiring a lighter formulation. It treats the same indications as the cream—improving skin circulation, reducing the appearance of scars and burns, and alleviating related discomfort.
Hirudoid Forte
- Consistency: Hirudoid Forte is available in both cream and gel forms.
- Active Ingredient Concentration: The key difference between Hirudoid Forte and the regular Hirudoid products is the higher concentration of MPS. It contains 0.6% (6 mg/g) MPS, which is double the concentration found in the regular cream and gel.
- Intended Use: With its higher MPS concentration, Hirudoid Forte targets more severe cases or situations requiring a faster response. It addresses the same conditions as regular Hirudoid products but more effectively reduces inflammation and pain.The mucopolysaccharide polysulfate in Hirudoid Forte Ointment has an anti-inflammatory effect.
Summary of Differences:
| Feature | Hirudoid Cream | Hirudoid Gel | Hirudoid Forte |
|---|---|---|---|
| Consistency | Smooth, white cream | Lighter, less greasy | Available in cream and gel forms |
| Active Ingredient Concentration | 0.3% (3 mg/g) MPS | 0.3% (3 mg/g) MPS | 0.6% (6 mg/g) MPS |
| Intended Use | Prevention and treatment of various skin conditions and circulatory problems | Larger areas of the body or lighter formulation | More severe cases or faster response |
Important Notes:
- Individual Variability: The choice between these products may depend on individual preferences, such as the desired consistency or the severity of the condition.
- Consultation with Healthcare Provider: It is essential to consult with a healthcare provider before using any medication, including topical products, to ensure it is appropriate for the specific condition and to determine the correct dosage and application.
- Mechanism of Action: One of the main mechanisms by which it operates is through its action on blood coagulation pathways. Heparinoid exerts an antithrombotic effect. Heparinoid is a local anticoagulant preparation as skin application that relieves pain and inflammation with addition to promoting.
Side Effects and Safety
Common Side Effects
- Skin Reactions: These are the most frequently reported issues and include:
- Itching (Pruritus): This is a common reaction, especially in sensitive individuals.
- Redness (Erythema): May occur at the application site.
- Rash: Can manifest as various types, including:
- Red blotches
- Papules
- Pustules
- Burning Sensation: Some people may feel a slight burning feeling.
- Stinging: Similar to the burning sensation.
- Skin Discoloration: Uncommon, but possible.
Serious Side Effects (Rare)
While rare, certain severe reactions can occur, necessitating immediate medical attention:
- Allergic Reaction (Anaphylaxis): Although uncommon, this is a medical emergency. Symptoms include:
- Difficulty breathing
- Swelling of the face, lips, tongue, or throat
- Rapid heartbeat
- Dizziness or fainting
- Hives
- Severe Skin Reactions: Including conditions like:
- Stevens-Johnson Syndrome (SJS)
- Toxic Epidermal Necrolysis (TEN)
- Acute Generalized Exanthematous Pustulosis (AGEP)
Precautions and Contraindications
- Allergies: Individuals allergic to Hirudoid or any of its components should avoid using it.
- Pregnancy and Breastfeeding: Consult a healthcare provider before using Hirudoid in these situations, as safety data may be limited.
- Open Wounds or Infections: Avoid using Hirudoid on open wounds or areas with active infection, as it may exacerbate the condition.
Safety Measures:
Avoid Contact: Keep Hirudoid away from the eyes and mucous membranes.
Patch Test: For individuals with sensitive skin or a history of allergies, conducting a patch test is advisable before widespread application.
Discontinue Use: If any adverse effects are experienced, discontinue use and consult a healthcare professional.
Conclusion
From its origins in leech-derived hirudin to modern formulations like Hirudoid Cream, Gel, and Forte, Hirudoid represents decades of innovation in topical therapy. Whether in cream, gel, or Forte form, Hirudoid remains a gold standard for non-invasive treatment of skin trauma, vascular inflammation, and post-surgical bruising. Backed by decades of safe use, real-world results, and evolving formulations, it remains relevant in modern dermatological and vascular therapy.
And with powerful platforms like PatSnap Eureka AI Agent, innovators can track not just what Hirudoid is, but where its category is headed next.
FAQs
Yes. It improves blood flow in bruised areas, absorbs leaked blood, reduces inflammation, and speeds natural healing. Results vary by bruise severity.
For minor issues (small bruises), improvement may show in days. Severe cases (large bruises) need 1+ week of 2–3 daily applications. Skin type, condition severity, and consistency affect timing.
Both reduce swelling and bruising, but Hirudoid (MPS) may be preferred for its additional skin-regenerative properties and fewer systemic concerns.
Yes, it can be used multiple times a day, following dosage guidelines on the leaflet.
While systemic absorption is minimal, always consult a doctor before use during pregnancy or breastfeeding.
Try PatSnap Eureka AI Agent to explore the R&D and competitive intelligence behind topical pharmaceutical trends.

