
What is Hemodialysis?
Hemodialysis is a medical treatment used for patients with end-stage renal disease (ESRD) or chronic kidney disease (CKD) when their kidneys are no longer able to effectively filter and remove waste products from the blood. It involves the extracorporeal circulation of blood through a semi-permeable membrane, known as a dialyzer, where toxins, excess fluids, and electrolytes are removed from the blood and transferred into a dialysate solution. The purified blood is then returned to the patient’s body.

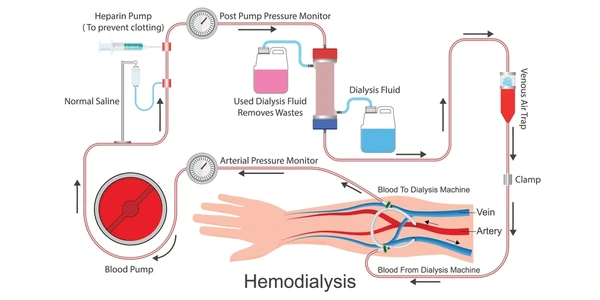
How Does Hemodialysis Work?
Hemodialysis is a medical process used to filter waste products from the blood when the kidneys are no longer able to perform this function effectively. It is commonly used for patients with end-stage renal disease (ESRD) or those experiencing acute kidney injury. During hemodialysis, the patient’s blood is pumped through a machine called a dialyzer, which acts as an artificial kidney. The dialyzer contains a semipermeable membrane that allows waste products, such as urea, creatinine, and excess fluids, to be removed from the blood and transferred into a dialysate solution. The purified blood is then returned to the patient’s body. This process helps to maintain the proper chemical balance and fluid levels in the blood, which is essential for the patient’s overall health and well-being.
Types of Vascular Access
Arteriovenous Fistula (AVF)
- Description: An AVF is created by surgically joining an artery directly to a vein, usually in the forearm or upper arm.
- Advantages: It is considered the best type of vascular access due to lower rates of complications, such as infection and clotting. It also provides better blood flow, which is essential for efficient dialysis.
- Disadvantages: It takes time to develop and mature, typically 4-6 weeks, before it can be used for dialysis.
Arteriovenous Graft (AVG):
- Description: An AVG is created by connecting an artery to a vein using a synthetic tube or graft.
- Advantages: It can be used sooner than an AVF, usually within a few days after surgery, as it does not require maturation time.
- Disadvantages: It has a higher risk of complications, such as clotting and infection, compared to an AVF.
Central Venous Catheter (CVC)
- Description: A CVC is a catheter inserted into a large vein in the neck, chest, or arm. It is usually used as a temporary access option until a more permanent access, such as an AVF or AVG, is established.
- Advantages: It can be placed quickly and is useful in emergency situations.
- Disadvantages: It has a higher risk of complications, including infection, clotting, and central vein stenosis, which can limit its long-term use.
Benefits of Hemodialysis
- Effective Waste Removal: Hemodialysis is highly effective in removing waste products such as urea and creatinine from the blood, which helps to reduce the symptoms of uremia and improve overall health.
- Fluid Management: It helps in managing excess fluid in the body, which is crucial for patients with fluid retention issues.
- Electrolyte Balance: The process helps maintain the body’s electrolyte balance by removing or adding necessary ions, thus preventing complications like hyperkalemia or hyponatremia.
- Acid-Base Balance: Hemodialysis aids in correcting the body’s acid-base balance by removing excess hydrogen ions or adding bicarbonate as needed.
- Improved Quality of Life: By effectively managing waste products and maintaining fluid and electrolyte balance, hemodialysis improves the quality of life for patients with renal failure, allowing them to lead more active and healthier lives.
- Temporary Solution: For some patients, hemodialysis serves as a temporary solution until a kidney transplant can be performed.
Challenges and Risks
- Bio-incompatibility reactions: These can occur due to the interaction between blood proteins and the dialyzer membrane, leading to inflammation and other complications.
- Hypotension: A drop in blood pressure can occur during dialysis due to the removal of excess fluids, which can be a significant risk.
- Electrolyte imbalances: The removal of electrolytes during dialysis can lead to imbalances if not properly monitored and corrected.
- Infection risk: Access sites for blood flow can become infected, and there is a risk of infection in the dialyzer itself.
- Protein loss: The process can lead to the loss of valuable proteins from the blood, which can have negative effects on the patient’s health.
- Cardiovascular risks: The process can also lead to cardiovascular instability and potential damage over time.
Patient Care and Lifestyle Considerations
- Frequent hospital visits and dependence on healthcare facilities, which can be inconvenient and stressful.
- Potential dietary restrictions and the need for a specialized diet to manage electrolyte levels.
- The risk of developing secondary health conditions such as cardiovascular disease and infections.
- The impact on employment and social activities due to the time commitment required for dialysis sessions.
- The psychological burden of living with a chronic illness and the potential for depression and anxiety.
Alternatives to Hemodialysis
Arteriovenous Grafts and Fistulae
- Arteriovenous Fistulae (AVF): Considered the gold standard for vascular access, AVFs are surgically created connections between an artery and a vein, typically in the forearm. They provide high-flow access and are preferred for their durability and lower complication rates compared to grafts.
- Prosthetic Arteriovenous Grafts: Used when autogenous options are not feasible, these grafts can be placed in anatomical or extra-anatomical locations. They offer a reliable alternative, although with potentially higher infection rates compared to AVFs.
Lab-on-a-Chip Devices and Wearable Technology
- Lab-on-a-Chip Devices: These microfluidic devices use electrokinetic means to remove uremic toxins continuously, offering a potential alternative to traditional hemodialysis with improved mobility and reduced need for trained personnel.
- Wearable Kidney Devices: Emerging technologies aim to develop wearable devices that can perform continuous kidney disease treatment, enhancing the convenience and effectiveness of renal support outside of traditional dialysis settings.
Alternative Hemodialysis Regimens
- Short Daily and Nocturnal Hemodialysis: These alternative regimens involve more frequent or longer dialysis sessions, which have shown to improve survival rates, reduce left ventricular mass, and enhance quality of life. However, they require significant patient cooperation and access to specialized equipment.
Home Hemodialysis (HHD)
- Daily Home Hemodialysis (DHHD): Patients who perform dialysis at home can achieve better preservation of residual renal function, improved blood pressure control, and reduced need for antihypertensive medications and erythropoietin. HHD also offers better quality of life and social rehabilitation.
Extracorporeal Blood Purification Techniques
- These techniques utilize various membrane materials to modulate inflammatory mediators and may be used in septic conditions, although their application in hemodialysis remains controversial and requires further research.
Peritoneal Dialysis (PD)
- Compared to hemodialysis, PD has been shown to be a lower-cost alternative with comparable or sometimes superior outcomes in terms of patient survival and quality of life. However, it requires a different set of skills and patient compliance.
Applications of Hemodialysis
Treatment of Kidney Diseases
- Hemodialysis is the most common treatment for patients with end-stage renal disease (ESRD), where the kidneys have lost nearly all their ability to do their job properly.
- It helps remove waste products, excess fluids, and electrolytes from the blood when the kidneys are failing.
- The process involves using a machine to filter the blood outside the body, which is then returned to the patient.
Management of Related Conditions
- Hemodialysis can help manage conditions such as high blood pressure, diabetes, and heart disease, which are often associated with kidney disease.
- It can also help control electrolyte levels, such as potassium and phosphate, which can become imbalanced in kidney failure.
- The treatment can improve symptoms like swelling, fatigue, and shortness of breath, which are common in advanced kidney disease.
Application in Different Patient Groups
- Hemodialysis is commonly performed in outpatient dialysis centers, but it can also be done at home, especially with newer, more portable machines.
- The treatment is typically done three to four times a week, with each session lasting several hours.
- Hemodialysis is not just limited to adults; it is also used in pediatric patients with severe kidney disease.
Application Cases
| Product/Project | Technical Outcomes | Application Scenarios |
|---|---|---|
| Hemodialysis Systems Fresenius Medical Care Holdings, Inc. | Provides more physiologically desirable proportions of dialysate constituents like sodium and bicarbonate for improved dialysis. | Treatment of end-stage renal disease and kidney failure requiring hemodialysis. |
| Peritoneal Dialysis Systems Baxter International, Inc. | Uses large dialysate volumes and simplified peritoneal equilibration tests for improved peritoneal dialysis efficacy. | Home-based peritoneal dialysis treatment for end-stage renal disease patients. |
| Hemodialysis Systems with Nanoclay Sorbents Baxter International, Inc. | Nanoclay sorbents like montmorillonite and bentonite enhance absorption of waste products like ammonium, phosphate and creatinine. | Wearable or conventional hemodialysis systems for effective removal of toxins from blood. |
Latest Technical Innovations in Hemodialysis
High-Flux Bicarbonate Dialysis and Hemodiafiltration
- These techniques have gained popularity due to their ability to remove a broader range of waste products, including middle molecules, compared to traditional low-flux dialysis. High-flux dialysis is particularly beneficial for patients with low serum albumin levels and diabetics.
Wearable Artificial Kidney
- This innovative device aims to provide continuous renal replacement therapy outside the hospital setting, enhancing the quality of life for patients with ESRD. Although still in the early stages of clinical development, it represents a significant advancement towards more convenient and effective hemodialysis options.
Advanced Dialysis Membranes
- Recent developments in dialysis membrane materials focus on improving biocompatibility and enhancing the removal of protein-bound uremic toxins, which are poorly cleared by conventional hemodialysis. Membranes are being modified to reduce protein adsorption and improve the selectivity of toxin removal.
User-Friendly Hemodialysis Machines
- New designs aim to make hemodialysis more accessible for home use, with a focus on improving the user interface and reducing the size and weight of the devices. This trend towards home hemodialysis (HHD) is driven by the need for more convenient and patient-centered treatment options.
Integrated Fluid Circuits and Safety Features
- Recent innovations include the development of fluid circuits that enhance the efficiency and safety of hemodialysis. Features such as automated blood volume monitoring and biofeedback modules help in managing complications like intradialytic hypotension.
Continuous Renal Replacement Therapies (CRRT)
- CRRT offers continuous clearance of waste products and provides stable blood flow dynamics, making it suitable for critically ill patients, including those with conditions such as sepsis and acute pancreatitis.
To get detailed scientific explanations of hemodialysis, try Patsnap Eureka.

