Examining Hypertonic Saline for Improved Patient Outcomes
Hypertonic Saline Background and Objectives
Hypertonic saline has emerged as a significant therapeutic intervention in various medical fields, particularly in critical care and emergency medicine. The evolution of this treatment modality spans several decades, with its roots tracing back to early observations of osmotic effects on biological systems. Initially utilized primarily for its ability to rapidly increase serum osmolality, hypertonic saline has since demonstrated a multitude of beneficial physiological effects that extend beyond simple fluid management.
The development of hypertonic saline solutions for medical use has been driven by the need for more effective fluid resuscitation strategies in conditions such as hypovolemic shock, traumatic brain injury, and severe sepsis. As research progressed, the unique properties of hypertonic saline, including its ability to expand intravascular volume with smaller fluid volumes and its potential anti-inflammatory effects, became increasingly apparent. This led to a broadening of its applications across various medical specialties.
The primary objective in examining hypertonic saline for improved patient outcomes is to comprehensively evaluate its efficacy, safety profile, and potential advantages over conventional isotonic fluid therapies. This investigation aims to elucidate the mechanisms by which hypertonic saline exerts its beneficial effects, including its impact on cerebral perfusion, systemic hemodynamics, and immune modulation. Furthermore, the research seeks to identify optimal concentrations, administration protocols, and patient populations that may derive the greatest benefit from this intervention.
Another crucial aspect of this examination is to explore the potential of hypertonic saline in addressing specific clinical challenges, such as reducing intracranial pressure in traumatic brain injury, improving outcomes in septic shock, and enhancing fluid management in patients with congestive heart failure. By focusing on these targeted applications, researchers aim to refine treatment strategies and develop evidence-based guidelines for the use of hypertonic saline across different medical scenarios.
The technological evolution in the production and administration of hypertonic saline solutions is also a key area of interest. This includes advancements in formulation to enhance stability, reduce adverse effects, and potentially combine hypertonic saline with other therapeutic agents for synergistic benefits. Additionally, the development of novel delivery systems and monitoring technologies to optimize the use of hypertonic saline in clinical practice is an important objective of ongoing research efforts.
Clinical Demand Analysis
The clinical demand for hypertonic saline solutions has been steadily increasing in recent years, driven by its potential to improve patient outcomes across various medical conditions. Hypertonic saline, typically defined as a sodium chloride solution with a concentration greater than 0.9%, has shown promise in treating a range of conditions, including traumatic brain injury, acute respiratory distress syndrome, and sepsis.
In the field of neurocritical care, hypertonic saline has emerged as a valuable tool for managing intracranial pressure (ICP) in patients with traumatic brain injury or other neurological conditions. The ability of hypertonic saline to reduce cerebral edema and improve cerebral perfusion has led to its widespread adoption in neurosurgical intensive care units. This growing demand is reflected in the increasing number of clinical trials and published studies exploring the efficacy of hypertonic saline in neurological patients.
Respiratory medicine has also seen a rising interest in hypertonic saline, particularly for the treatment of cystic fibrosis and bronchiectasis. The osmotic properties of hypertonic saline help to hydrate the airway surface liquid, improve mucociliary clearance, and reduce the viscosity of mucus. This has resulted in improved lung function and reduced exacerbations in patients with chronic respiratory conditions, driving the demand for hypertonic saline nebulizer solutions in both hospital and home care settings.
In the realm of emergency medicine and critical care, hypertonic saline has gained traction as a potential alternative to traditional crystalloid solutions for fluid resuscitation in patients with severe sepsis or septic shock. The ability of hypertonic saline to rapidly expand intravascular volume while minimizing fluid overload has sparked interest among clinicians seeking more effective resuscitation strategies.
The growing prevalence of chronic diseases and an aging population have further contributed to the increased demand for hypertonic saline. Conditions such as heart failure, where fluid management is crucial, have seen exploratory use of hypertonic saline as an adjunct therapy. Additionally, the rise in surgical procedures, particularly those involving significant fluid shifts, has led to greater consideration of hypertonic saline for perioperative fluid management.
Market analysis indicates that the global hypertonic saline market is expected to grow significantly in the coming years, driven by these expanding clinical applications and the ongoing research into novel uses. Healthcare providers and pharmaceutical companies are responding to this demand by developing new formulations and delivery systems to optimize the administration of hypertonic saline across various clinical settings.
Current Challenges in Hypertonic Saline Therapy
Another challenge lies in the potential adverse effects associated with HS therapy. Rapid infusion or excessive doses can lead to hypernatremia, which may cause neurological complications, particularly in patients with pre-existing conditions. Balancing the therapeutic benefits with the risks of electrolyte imbalances requires careful monitoring and individualized treatment plans, which can be resource-intensive and complex to manage.
The heterogeneity of patient populations receiving HS therapy further complicates its application. Different medical conditions, such as traumatic brain injury, sepsis, or hyponatremia, may require distinct approaches to HS administration. Tailoring the therapy to specific patient needs while maintaining safety and efficacy remains a significant challenge for healthcare providers.
Moreover, the long-term effects of repeated or prolonged HS therapy are not fully understood. While short-term benefits are well-documented in certain conditions, the impact on organ function, fluid balance, and overall patient outcomes over extended periods requires further investigation. This knowledge gap hinders the development of comprehensive treatment strategies for chronic conditions that may benefit from HS therapy.
The cost-effectiveness of HS therapy compared to alternative treatments is another area of concern. While HS is generally considered an affordable option, the total cost of care, including monitoring, potential complications management, and length of hospital stay, needs to be evaluated comprehensively. This economic aspect is crucial for healthcare systems striving to optimize resource allocation while improving patient outcomes.
Lastly, there is a need for more robust clinical evidence to support the use of HS in various indications. While some applications, such as in traumatic brain injury, have strong supporting data, other potential uses lack sufficient high-quality studies. This paucity of evidence makes it challenging for clinicians to make informed decisions about when and how to implement HS therapy effectively across different patient populations and clinical scenarios.
Existing Hypertonic Saline Protocols
01 Improved respiratory outcomes
Hypertonic saline treatment has shown positive effects on respiratory function in patients with various conditions. It can help improve mucus clearance, reduce airway inflammation, and enhance lung function. This therapy has been particularly beneficial for patients with cystic fibrosis, bronchiolitis, and other respiratory disorders.- Improved respiratory function in cystic fibrosis patients: Hypertonic saline treatment has shown positive outcomes in improving respiratory function for patients with cystic fibrosis. It helps to hydrate airway surfaces, enhance mucus clearance, and reduce pulmonary exacerbations, leading to better lung function and quality of life for these patients.
- Management of traumatic brain injury and intracranial pressure: Hypertonic saline solutions are used in the treatment of traumatic brain injury to manage intracranial pressure. The treatment has shown positive outcomes in reducing brain swelling, improving cerebral perfusion, and potentially enhancing neurological recovery in patients with severe head injuries.
- Treatment of acute hyponatremia: Hypertonic saline is effective in treating acute hyponatremia, a condition characterized by low sodium levels in the blood. The treatment helps to rapidly correct sodium levels, improving patient outcomes by reducing the risk of neurological complications associated with severe hyponatremia.
- Enhanced wound healing and infection control: Hypertonic saline solutions have demonstrated positive outcomes in wound care management. They can help in reducing bacterial load, promoting wound debridement, and enhancing the healing process, particularly in chronic wounds or surgical site infections.
- Improved outcomes in sepsis management: The use of hypertonic saline in sepsis management has shown promising results. It can help in fluid resuscitation, improving hemodynamics, and potentially reducing mortality rates in patients with severe sepsis or septic shock.
02 Enhanced wound healing
The application of hypertonic saline in wound care has demonstrated improved healing outcomes. It can help reduce edema, promote tissue regeneration, and prevent infection. This approach has been effective in treating various types of wounds, including surgical incisions and chronic ulcers.Expand Specific Solutions03 Neurological benefits
Hypertonic saline therapy has shown promise in managing neurological conditions. It can help reduce intracranial pressure, improve cerebral perfusion, and mitigate the effects of traumatic brain injury. This treatment approach has been explored for patients with various neurological disorders and head trauma.Expand Specific Solutions04 Cardiovascular effects
The use of hypertonic saline has demonstrated positive outcomes in cardiovascular patients. It can help improve hemodynamics, increase cardiac output, and enhance tissue perfusion. This therapy has been investigated for its potential benefits in managing various cardiovascular conditions and during resuscitation efforts.Expand Specific Solutions05 Gastrointestinal applications
Hypertonic saline treatment has shown promising results in gastrointestinal disorders. It can help manage fluid and electrolyte imbalances, reduce intestinal edema, and improve gut motility. This approach has been explored for conditions such as postoperative ileus and inflammatory bowel diseases.Expand Specific Solutions
Key Players in Hypertonic Saline Production
Novartis AG
Parion Sciences, Inc.
Innovative Hypertonic Saline Formulations
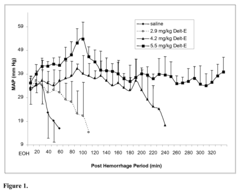
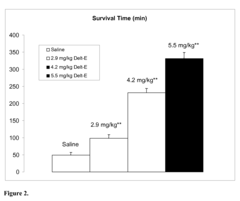
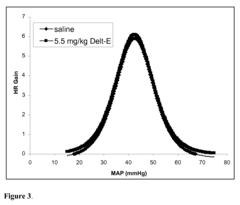
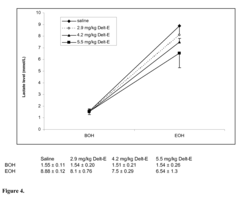
- Administration of an isolated polypeptide, Deltorphin-E, which comprises the amino acid sequence Tyr-(D-Ala)-Phe-Ala-Ile-Gly-Asp-Phe-Ser-Ile-NH2, to control bleeding and provide hemodynamic and metabolic support without the use of resuscitation fluids, thereby addressing the limitations of existing treatments.
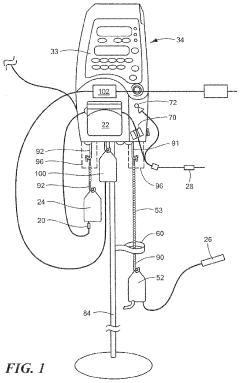
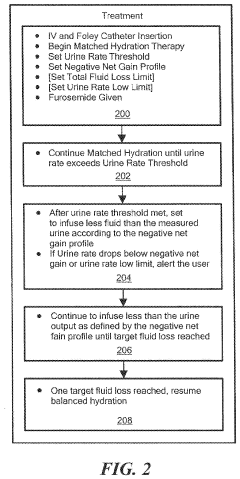
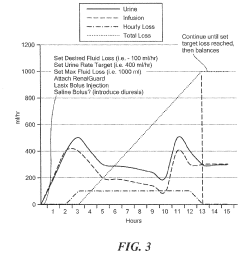
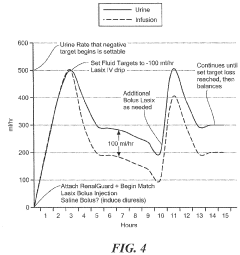
- A fluid management system and method that automatically adjusts hydration fluid delivery based on urine output and clinician settings to achieve a desired urine rate and net fluid loss, using a diuretic and osmotic agents like hypertonic saline to induce diuresis and prevent dehydration.
Safety and Efficacy Considerations
In terms of efficacy, HS has shown promising results in several clinical scenarios. For traumatic brain injury patients, HS administration has been associated with improved cerebral perfusion and reduced intracranial pressure. Studies have also indicated its effectiveness in treating hyponatremia, especially in cases of syndrome of inappropriate antidiuretic hormone secretion (SIADH). Additionally, HS has demonstrated potential benefits in managing acute heart failure and certain types of shock.
However, the safety profile of HS requires careful consideration. One of the primary concerns is the risk of rapid changes in serum sodium levels, which can lead to osmotic demyelination syndrome if not properly managed. This risk is particularly pronounced in patients with chronic hyponatremia. Other potential adverse effects include hyperchloremic metabolic acidosis, volume overload, and electrolyte imbalances.
To mitigate these risks, precise dosing and administration protocols are essential. Continuous monitoring of serum electrolytes, particularly sodium levels, is crucial during HS therapy. The rate of sodium correction should be carefully controlled, typically not exceeding 8-10 mEq/L in 24 hours for most patients. In cases of severe hyponatremia, even slower correction rates may be necessary.
The efficacy of HS can be influenced by various factors, including the concentration used, the rate of administration, and the underlying condition being treated. Higher concentrations (e.g., 3% or 7.5%) may be more effective for certain indications but also carry a higher risk of adverse effects. Therefore, the choice of concentration should be tailored to the specific clinical scenario and patient characteristics.
Long-term safety data on HS use is still limited, particularly for repeated or prolonged administration. This gap in knowledge underscores the need for ongoing research and vigilant post-marketing surveillance. Future studies should focus on optimizing dosing regimens, identifying patient subgroups most likely to benefit, and developing strategies to minimize long-term risks.
In conclusion, while hypertonic saline has demonstrated significant efficacy in various clinical settings, its use must be balanced against potential safety concerns. Careful patient selection, precise administration protocols, and vigilant monitoring are essential to maximize its therapeutic benefits while minimizing risks. As research continues, our understanding of the optimal use of HS is likely to evolve, potentially expanding its applications while refining safety protocols.
Pharmacoeconomic Analysis
Initial studies suggest that HS therapy may lead to faster resolution of symptoms and improved clinical outcomes compared to standard treatments. This could translate to significant cost savings for healthcare systems by reducing the overall resource utilization per patient. However, the upfront costs of HS administration, including the solution itself and any specialized equipment or training required, must be factored into the economic equation.
Long-term cost-effectiveness analyses have shown promising results for HS in certain patient populations. For instance, in pediatric bronchiolitis cases, HS nebulization has demonstrated potential for reducing hospital admissions and shortening inpatient stays, leading to substantial cost savings. Similarly, in neurocritical care settings, HS has been associated with improved outcomes and potentially reduced intensive care unit costs compared to mannitol.
The economic impact of HS extends beyond direct medical costs. Improved patient outcomes can lead to faster recovery times, potentially reducing lost productivity for patients and caregivers. This societal perspective on pharmacoeconomics suggests broader economic benefits that may not be immediately apparent in hospital-centric analyses.
However, the cost-effectiveness of HS varies significantly depending on the specific clinical context and patient population. Some studies have found minimal economic benefit in certain conditions, highlighting the need for targeted use based on evidence-based guidelines. Additionally, the potential for adverse effects and the need for close monitoring may offset some of the economic gains in certain scenarios.
Future pharmacoeconomic research should focus on large-scale, long-term studies to better quantify the economic impact of HS across various clinical settings. This should include not only direct medical costs but also indirect costs and quality of life measures to provide a comprehensive economic evaluation. As healthcare systems increasingly emphasize value-based care, understanding the full economic implications of HS therapy will be crucial for informed decision-making and resource allocation.