Hypertonic Osmotherapy in Critical Care: A Critical Review
Hypertonic Osmotherapy Evolution and Objectives
Hypertonic osmotherapy has been a cornerstone in critical care medicine for decades, evolving significantly since its inception. The concept of using hypertonic solutions to manage intracranial pressure and cerebral edema dates back to the early 20th century. Initially, the primary focus was on mannitol, a sugar alcohol that increases serum osmolality and promotes diuresis. As research progressed, the potential of hypertonic saline solutions became increasingly apparent, offering an alternative approach to osmotherapy.
The evolution of hypertonic osmotherapy has been driven by a deeper understanding of fluid dynamics, osmotic gradients, and their effects on cerebral physiology. Early studies in the 1960s and 1970s laid the groundwork for modern osmotherapy protocols, demonstrating the efficacy of hyperosmolar agents in reducing intracranial pressure. Subsequent research in the 1980s and 1990s refined these techniques, exploring optimal concentrations, infusion rates, and comparative efficacy of different osmotic agents.
In recent years, the objectives of hypertonic osmotherapy have expanded beyond merely reducing intracranial pressure. Current goals include improving cerebral blood flow, enhancing oxygen delivery to brain tissue, and modulating the inflammatory response associated with various neurological insults. This multifaceted approach reflects a more nuanced understanding of the complex pathophysiology underlying conditions such as traumatic brain injury, stroke, and post-operative cerebral edema.
The technological advancements in neuroimaging and intracranial monitoring have significantly contributed to the evolution of osmotherapy. These tools allow for real-time assessment of cerebral perfusion and intracranial dynamics, enabling more precise and targeted osmotherapy interventions. This has led to the development of individualized treatment protocols, tailored to the specific needs of each patient based on their unique physiological parameters.
As the field progresses, the objectives of hypertonic osmotherapy research continue to evolve. Current aims include optimizing the balance between the benefits of osmotic dehydration and potential adverse effects, such as rebound cerebral edema and electrolyte imbalances. Additionally, there is a growing focus on understanding the molecular mechanisms underlying the effects of hyperosmolar agents on the blood-brain barrier and neuroinflammation.
The future directions of hypertonic osmotherapy research are likely to explore novel osmotic agents, innovative delivery methods, and combination therapies that synergize with other neuroprotective strategies. The ultimate goal remains to improve patient outcomes in critical care settings, reducing mortality and morbidity associated with intracranial hypertension and cerebral edema across a spectrum of neurological conditions.
Critical Care Market Demand Analysis
The critical care market has been experiencing significant growth due to the increasing prevalence of chronic diseases, aging populations, and advancements in medical technologies. Within this market, hypertonic osmotherapy has emerged as a crucial treatment modality for various critical conditions, particularly in managing cerebral edema and intracranial pressure.
The demand for hypertonic osmotherapy in critical care settings is driven by its effectiveness in treating life-threatening conditions such as traumatic brain injury, stroke, and post-operative complications. The global critical care market, which encompasses hypertonic osmotherapy, was valued at approximately $85 billion in 2020 and is projected to grow at a compound annual growth rate (CAGR) of 7.5% from 2021 to 2028.
Hypertonic saline solutions, a key component of hypertonic osmotherapy, have seen increased adoption in intensive care units worldwide. This growth is attributed to their ability to rapidly reduce intracranial pressure and improve cerebral perfusion. The market for hypertonic saline solutions in critical care is expected to expand at a CAGR of 5.8% from 2021 to 2026.
The rising incidence of traumatic brain injuries, estimated at 69 million cases annually worldwide, is a significant factor driving the demand for hypertonic osmotherapy. Additionally, the growing prevalence of stroke, with approximately 15 million cases globally each year, further contributes to the market expansion.
Geographically, North America dominates the critical care market, including hypertonic osmotherapy, due to advanced healthcare infrastructure and high healthcare expenditure. Europe follows closely, while Asia-Pacific is expected to witness the fastest growth in the coming years due to improving healthcare access and rising awareness of advanced treatment modalities.
The COVID-19 pandemic has also influenced the critical care market, with increased demand for intensive care services and a focus on managing complications such as cytokine storms, where hypertonic solutions may play a role in fluid management strategies.
Despite the growing demand, challenges such as the risk of electrolyte imbalances and the need for careful monitoring during hypertonic osmotherapy administration persist. These factors necessitate ongoing research and development to optimize treatment protocols and improve patient outcomes.
In conclusion, the market demand for hypertonic osmotherapy in critical care is robust and expected to continue growing. This trend is supported by the increasing prevalence of conditions requiring intensive care, technological advancements, and a growing body of evidence supporting the efficacy of hypertonic solutions in managing critical neurological conditions.
Current Challenges in Hypertonic Osmotherapy
Hypertonic osmotherapy, while a promising treatment in critical care, faces several significant challenges that hinder its widespread adoption and optimal utilization. One of the primary concerns is the lack of standardized protocols for administration. The optimal concentration, volume, and infusion rate of hypertonic solutions vary widely across different clinical settings and patient populations, making it difficult to establish universal guidelines.
Another major challenge is the potential for adverse effects associated with hypertonic osmotherapy. Rapid changes in serum osmolality can lead to complications such as central pontine myelinolysis, particularly in patients with chronic hyponatremia. Additionally, the risk of fluid overload and electrolyte imbalances necessitates careful monitoring and adjustment of therapy, which can be resource-intensive in critical care settings.
The limited understanding of the long-term effects of hypertonic osmotherapy poses another significant challenge. While short-term benefits in reducing intracranial pressure and improving cerebral perfusion have been demonstrated, the impact on long-term neurological outcomes remains unclear. This uncertainty complicates decision-making processes for clinicians when weighing the potential risks and benefits of the treatment.
Furthermore, there is a notable lack of large-scale, randomized controlled trials comparing hypertonic osmotherapy to other treatment modalities in various critical care scenarios. This paucity of high-quality evidence makes it challenging to definitively establish the superiority of hypertonic solutions over other interventions, such as mannitol, in managing cerebral edema and intracranial hypertension.
The heterogeneity of patient populations in critical care settings also presents a challenge in determining the most appropriate candidates for hypertonic osmotherapy. Factors such as underlying medical conditions, concurrent medications, and the etiology of cerebral edema can significantly influence treatment outcomes, necessitating a more personalized approach to therapy.
Lastly, the cost-effectiveness of hypertonic osmotherapy compared to alternative treatments remains a point of contention. The need for specialized equipment, intensive monitoring, and potential complications may offset the benefits in some healthcare systems, particularly in resource-limited settings. This economic consideration adds another layer of complexity to the widespread implementation of hypertonic osmotherapy in critical care practice.
Existing Hypertonic Solutions in Critical Care
01 Hypertonic solutions for osmotherapy
Hypertonic solutions are used in osmotherapy to create an osmotic gradient, drawing excess fluid from tissues. This approach is particularly effective in treating conditions such as cerebral edema or increased intracranial pressure. Common hypertonic solutions include saline and mannitol, which can be administered intravenously to achieve the desired osmotic effect.- Hypertonic solutions for osmotherapy: Hypertonic solutions are used in osmotherapy to create an osmotic gradient, drawing excess fluid from tissues. These solutions, often containing high concentrations of solutes like mannitol or saline, are administered to reduce intracranial pressure or treat cerebral edema. The hypertonic nature of these solutions helps in managing various neurological conditions by altering fluid dynamics in the body.
- Devices for hypertonic osmotherapy administration: Specialized devices have been developed for the precise and controlled administration of hypertonic solutions in osmotherapy. These devices may include infusion pumps, catheters, or other delivery systems designed to ensure accurate dosing and optimal therapeutic effects. Such devices can help in maintaining the desired osmotic gradient and managing the treatment duration effectively.
- Combination therapies with hypertonic osmotherapy: Hypertonic osmotherapy is often combined with other treatment modalities to enhance therapeutic outcomes. This may include combining osmotherapy with pharmacological interventions, surgical procedures, or other medical therapies. The synergistic effects of these combinations can lead to improved patient outcomes in various neurological and systemic conditions.
- Monitoring and assessment techniques for osmotherapy: Various monitoring and assessment techniques have been developed to evaluate the effectiveness of hypertonic osmotherapy and guide treatment decisions. These may include neuroimaging methods, biomarker analysis, or real-time monitoring of physiological parameters. Such techniques help in optimizing the osmotherapy regimen and ensuring patient safety during treatment.
- Novel formulations for hypertonic osmotherapy: Research has led to the development of novel formulations for hypertonic osmotherapy, aiming to improve efficacy and reduce side effects. These formulations may incorporate new osmotic agents, delivery systems, or additives that enhance the therapeutic effects of osmotherapy. Such innovations can potentially expand the applications of hypertonic osmotherapy in various medical fields.
02 Devices for administering hypertonic osmotherapy
Specialized devices have been developed for the precise administration of hypertonic solutions in osmotherapy. These may include infusion pumps, catheters, or other delivery systems designed to control the rate and volume of hypertonic solution administration. Such devices can improve the safety and efficacy of hypertonic osmotherapy treatments.Expand Specific Solutions03 Combination therapies with hypertonic osmotherapy
Hypertonic osmotherapy can be combined with other therapeutic approaches to enhance its effectiveness. This may include combining osmotherapy with pharmacological agents, physical interventions, or other medical procedures. Such combination therapies aim to provide synergistic effects in treating various medical conditions.Expand Specific Solutions04 Monitoring and control systems for osmotherapy
Advanced monitoring and control systems have been developed to optimize hypertonic osmotherapy treatments. These systems may include sensors to measure osmolarity, intracranial pressure, or other relevant parameters. Real-time monitoring allows for precise adjustment of treatment parameters, improving patient outcomes and reducing potential side effects.Expand Specific Solutions05 Novel hypertonic solutions for osmotherapy
Research has led to the development of new hypertonic solutions for osmotherapy, aiming to improve efficacy and reduce side effects. These may include novel osmotic agents, formulations with additional therapeutic properties, or solutions designed for specific medical conditions. Such innovations seek to expand the applications and effectiveness of hypertonic osmotherapy.Expand Specific Solutions
Key Players in Critical Care Osmotherapy
The field of hypertonic osmotherapy in critical care is in a mature stage of development, with a substantial market size driven by the increasing prevalence of critical illnesses. The technology has reached a high level of maturity, as evidenced by the involvement of major medical institutions and pharmaceutical companies. Key players like UCSF Benioff Children's Hospital Oakland, The Cleveland Clinic Foundation, and Allergan, Inc. are at the forefront of research and development. Universities such as Wuhan University and the University of California are contributing significantly to advancing the field. The competitive landscape is diverse, with pharmaceutical giants like GlaxoSmithKline and Genentech competing alongside specialized companies like Cytokinetics and Parion Sciences, indicating a robust and dynamic market with ongoing innovation and research.
The Cleveland Clinic Foundation
The Regents of the University of California
Core Innovations in Osmotherapy Techniques
- Development of ophthalmic compositions comprising an aqueous carrier with tonicity components such as erythritol, xylitol, carnitine, and polyanionic components like hyaluronic acid or polyanionic peptides, which provide a supra-tonic osmolality and reduce adverse effects of cationic species on ocular surfaces, enhancing cellular protection and lubrication.
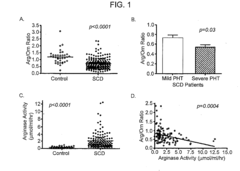
- A method and composition for diagnosing conditions with decreased arginine bioavailability by assessing the ratio of arginine to modulators of arginine bioavailability, such as ornithine and citrulline, in a patient sample, which helps in determining the nature and severity of the disease and guiding therapy.
Safety and Efficacy Considerations
Hypertonic osmotherapy has emerged as a promising treatment modality in critical care settings, particularly for managing intracranial hypertension and cerebral edema. However, the safety and efficacy of this approach require careful consideration and evaluation.
The primary mechanism of action for hypertonic solutions is the creation of an osmotic gradient, drawing fluid from the intracellular and interstitial spaces into the intravascular compartment. This effect can rapidly reduce intracranial pressure and improve cerebral perfusion. Clinical studies have demonstrated significant improvements in patient outcomes, particularly in cases of traumatic brain injury and post-operative neurosurgical care.
Efficacy considerations for hypertonic osmotherapy include the optimal concentration and volume of the solution, as well as the duration and frequency of administration. Research indicates that 7.5% saline solutions have shown superior results compared to lower concentrations, with faster and more sustained reductions in intracranial pressure. However, the efficacy may vary depending on the underlying pathology and individual patient characteristics.
Safety concerns associated with hypertonic osmotherapy primarily revolve around electrolyte imbalances, particularly hypernatremia and hypochloremia. Rapid shifts in serum osmolality can lead to central pontine myelinolysis, a severe neurological complication. Additionally, there is a risk of rebound intracranial hypertension upon discontinuation of therapy, necessitating careful monitoring and gradual tapering of treatment.
Cardiovascular effects of hypertonic solutions must also be considered, as they can cause transient increases in blood pressure and potential fluid overload in susceptible patients. Renal function should be closely monitored, as hypertonic solutions may exacerbate pre-existing renal impairment or precipitate acute kidney injury in critically ill patients.
The long-term safety profile of hypertonic osmotherapy remains an area of ongoing research. While short-term benefits are well-documented, the impact of prolonged or repeated use on neurological outcomes and overall patient survival requires further investigation. Prospective, randomized controlled trials are needed to establish optimal treatment protocols and identify patient populations most likely to benefit from this intervention.
In conclusion, while hypertonic osmotherapy shows promise in critical care settings, its use must be carefully balanced against potential risks. Individualized treatment approaches, close monitoring, and adherence to evidence-based protocols are essential to maximize efficacy and minimize adverse events. Future research should focus on refining treatment strategies and exploring novel formulations to enhance the safety and efficacy of this important therapeutic modality.
Pharmacoeconomic Analysis of Osmotherapy
Pharmacoeconomic analysis of osmotherapy in critical care settings is essential for evaluating the cost-effectiveness of this treatment modality. Hypertonic osmotherapy, particularly using mannitol or hypertonic saline, is a crucial intervention for managing intracranial pressure in various neurological emergencies. However, its economic impact on healthcare systems and patients requires careful consideration.
The direct costs associated with osmotherapy include the medication itself, administration equipment, and monitoring devices. Mannitol and hypertonic saline have different price points, with mannitol generally being less expensive. However, the total cost of treatment extends beyond the drug price, encompassing potential side effects and the need for additional interventions.
Indirect costs must also be factored into the analysis. These may include the length of stay in the intensive care unit, potential complications, and long-term outcomes. Osmotherapy can potentially reduce the duration of mechanical ventilation and overall ICU stay, leading to significant cost savings. However, adverse effects such as electrolyte imbalances or renal dysfunction may offset these benefits.
Comparative effectiveness research is crucial in determining the most cost-effective osmotherapy regimen. Studies comparing mannitol to hypertonic saline have shown varying results in terms of efficacy and safety profiles. The choice between these agents can have substantial economic implications, considering their different costs and potential for adverse events.
Quality-adjusted life years (QALYs) and disability-adjusted life years (DALYs) are important metrics in pharmacoeconomic evaluations of osmotherapy. These measures help quantify the impact of treatment on patient outcomes and quality of life, providing a more comprehensive view of the therapy's value beyond immediate clinical effects.
Healthcare system perspectives must be considered when analyzing the pharmacoeconomics of osmotherapy. Different reimbursement models and healthcare delivery systems can significantly influence the cost-effectiveness of these treatments. For instance, bundled payment models may incentivize more efficient use of osmotherapy and associated resources.
Long-term economic impacts of osmotherapy should not be overlooked. Improved neurological outcomes can lead to reduced rehabilitation costs and increased productivity, potentially offsetting the initial treatment expenses. Conversely, poor outcomes may result in prolonged care needs and substantial societal costs.
In conclusion, a comprehensive pharmacoeconomic analysis of osmotherapy in critical care must balance immediate treatment costs with long-term outcomes and societal impacts. This analysis is crucial for informing evidence-based decision-making in clinical practice and healthcare policy regarding the use of hypertonic osmotherapy in neurological emergencies.