Phospholipid Strategies for Combating Antibiotic Resistance
JUL 16, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Phospholipid Antibiotic Resistance Background
Antibiotic resistance has emerged as one of the most pressing global health challenges of the 21st century. The widespread and often indiscriminate use of antibiotics has led to the evolution of bacterial strains that can withstand traditional antimicrobial treatments. This phenomenon threatens to undermine decades of progress in modern medicine, potentially returning us to an era where common infections could once again become life-threatening.
Phospholipids, the primary components of cellular membranes, have recently gained attention as a potential strategy to combat antibiotic resistance. These naturally occurring molecules play crucial roles in maintaining cellular structure and function. Their unique properties and interactions with bacterial cell membranes offer promising avenues for developing novel antimicrobial approaches.
The interest in phospholipid-based strategies stems from their ability to target bacterial membranes directly, potentially bypassing many of the resistance mechanisms that bacteria have developed against conventional antibiotics. This approach represents a paradigm shift from traditional antibiotic development, which has primarily focused on inhibiting specific cellular processes or enzymes within bacteria.
Historically, the development of antibiotics has followed a cyclical pattern of discovery, widespread use, and eventual resistance. The first major antibiotic, penicillin, was discovered in 1928 and widely used by the 1940s. However, penicillin-resistant strains emerged shortly after, necessitating the development of new antibiotics. This cycle has continued, with each new class of antibiotics eventually facing resistance issues.
The current antibiotic resistance crisis has its roots in several factors, including overuse in healthcare and agriculture, poor infection control in hospitals, and a lack of new antibiotic development by pharmaceutical companies. The World Health Organization has declared antibiotic resistance as one of the top ten global public health threats facing humanity.
In this context, phospholipid strategies offer a novel approach to addressing antibiotic resistance. By targeting the fundamental structure of bacterial cells, these strategies may provide a more robust and long-lasting solution to the problem. The exploration of phospholipids in combating antibiotic resistance represents a convergence of microbiology, biochemistry, and pharmaceutical science, highlighting the interdisciplinary nature of modern medical research.
Phospholipids, the primary components of cellular membranes, have recently gained attention as a potential strategy to combat antibiotic resistance. These naturally occurring molecules play crucial roles in maintaining cellular structure and function. Their unique properties and interactions with bacterial cell membranes offer promising avenues for developing novel antimicrobial approaches.
The interest in phospholipid-based strategies stems from their ability to target bacterial membranes directly, potentially bypassing many of the resistance mechanisms that bacteria have developed against conventional antibiotics. This approach represents a paradigm shift from traditional antibiotic development, which has primarily focused on inhibiting specific cellular processes or enzymes within bacteria.
Historically, the development of antibiotics has followed a cyclical pattern of discovery, widespread use, and eventual resistance. The first major antibiotic, penicillin, was discovered in 1928 and widely used by the 1940s. However, penicillin-resistant strains emerged shortly after, necessitating the development of new antibiotics. This cycle has continued, with each new class of antibiotics eventually facing resistance issues.
The current antibiotic resistance crisis has its roots in several factors, including overuse in healthcare and agriculture, poor infection control in hospitals, and a lack of new antibiotic development by pharmaceutical companies. The World Health Organization has declared antibiotic resistance as one of the top ten global public health threats facing humanity.
In this context, phospholipid strategies offer a novel approach to addressing antibiotic resistance. By targeting the fundamental structure of bacterial cells, these strategies may provide a more robust and long-lasting solution to the problem. The exploration of phospholipids in combating antibiotic resistance represents a convergence of microbiology, biochemistry, and pharmaceutical science, highlighting the interdisciplinary nature of modern medical research.
Market Demand Analysis
The market demand for phospholipid strategies in combating antibiotic resistance has been steadily increasing in recent years. This growth is primarily driven by the rising global concern over antimicrobial resistance (AMR) and the urgent need for innovative solutions to address this critical healthcare challenge.
The pharmaceutical industry has shown significant interest in phospholipid-based approaches, recognizing their potential to enhance antibiotic efficacy and overcome resistance mechanisms. Major pharmaceutical companies are investing in research and development of phospholipid-antibiotic combinations, indicating a strong market pull for these technologies.
Healthcare providers and hospitals are also contributing to the market demand, as they seek more effective treatments for drug-resistant infections. The increasing incidence of hospital-acquired infections caused by resistant pathogens has created a pressing need for novel antimicrobial strategies, including those involving phospholipids.
Government initiatives and funding programs aimed at tackling AMR have further stimulated market growth. Many countries have implemented national action plans to combat antibiotic resistance, allocating resources for research and development of innovative antimicrobial technologies, including phospholipid-based approaches.
The market for phospholipid strategies in antibiotic resistance is expected to expand across various geographic regions. North America and Europe currently lead in terms of research and development activities, but emerging markets in Asia-Pacific and Latin America are showing increasing interest and investment in this field.
Several factors are driving the potential market size for phospholipid-based antibiotic resistance solutions. The global rise in antibiotic-resistant infections, coupled with the limited pipeline of new antibiotics, creates a substantial market opportunity. Additionally, the growing awareness among healthcare professionals and patients about the risks of antibiotic resistance is likely to fuel demand for innovative treatment options.
The market trend indicates a shift towards combination therapies and novel drug delivery systems incorporating phospholipids. This approach is seen as a promising strategy to extend the lifespan of existing antibiotics and develop more effective treatments against resistant pathogens.
In conclusion, the market demand for phospholipid strategies in combating antibiotic resistance is robust and expected to grow significantly in the coming years. The convergence of scientific advancements, healthcare needs, and regulatory support is creating a favorable environment for the development and adoption of these innovative antimicrobial solutions.
The pharmaceutical industry has shown significant interest in phospholipid-based approaches, recognizing their potential to enhance antibiotic efficacy and overcome resistance mechanisms. Major pharmaceutical companies are investing in research and development of phospholipid-antibiotic combinations, indicating a strong market pull for these technologies.
Healthcare providers and hospitals are also contributing to the market demand, as they seek more effective treatments for drug-resistant infections. The increasing incidence of hospital-acquired infections caused by resistant pathogens has created a pressing need for novel antimicrobial strategies, including those involving phospholipids.
Government initiatives and funding programs aimed at tackling AMR have further stimulated market growth. Many countries have implemented national action plans to combat antibiotic resistance, allocating resources for research and development of innovative antimicrobial technologies, including phospholipid-based approaches.
The market for phospholipid strategies in antibiotic resistance is expected to expand across various geographic regions. North America and Europe currently lead in terms of research and development activities, but emerging markets in Asia-Pacific and Latin America are showing increasing interest and investment in this field.
Several factors are driving the potential market size for phospholipid-based antibiotic resistance solutions. The global rise in antibiotic-resistant infections, coupled with the limited pipeline of new antibiotics, creates a substantial market opportunity. Additionally, the growing awareness among healthcare professionals and patients about the risks of antibiotic resistance is likely to fuel demand for innovative treatment options.
The market trend indicates a shift towards combination therapies and novel drug delivery systems incorporating phospholipids. This approach is seen as a promising strategy to extend the lifespan of existing antibiotics and develop more effective treatments against resistant pathogens.
In conclusion, the market demand for phospholipid strategies in combating antibiotic resistance is robust and expected to grow significantly in the coming years. The convergence of scientific advancements, healthcare needs, and regulatory support is creating a favorable environment for the development and adoption of these innovative antimicrobial solutions.
Current Challenges
The field of antibiotic resistance presents several significant challenges that hinder the development and implementation of effective phospholipid-based strategies. One of the primary obstacles is the rapid evolution of bacterial resistance mechanisms, which can quickly render new treatments ineffective. This adaptability of bacteria necessitates continuous innovation in phospholipid-based approaches to stay ahead of emerging resistance patterns.
Another major challenge lies in the complexity of bacterial cell membranes and their interaction with phospholipids. The diverse composition of bacterial membranes across different species and strains makes it difficult to develop a one-size-fits-all solution. Researchers must navigate this variability to create phospholipid strategies that are both broadly effective and specific enough to target resistant bacteria without harming beneficial microorganisms or host cells.
The delivery of phospholipid-based treatments poses additional hurdles. Ensuring that these compounds reach their intended targets within the bacterial cell while maintaining stability and efficacy in various physiological environments is a significant technical challenge. This is particularly problematic when dealing with intracellular pathogens or bacteria protected by biofilms, which add layers of complexity to the delivery process.
Furthermore, the pharmaceutical industry faces regulatory and economic challenges in developing new antibiotic treatments, including those based on phospholipid strategies. The high costs of research and development, coupled with the relatively short market life of antibiotics due to resistance development, create a challenging economic landscape for innovation in this field.
There is also a need for more comprehensive understanding of the mechanisms by which phospholipids can combat antibiotic resistance. While some pathways have been identified, such as membrane disruption or enhanced antibiotic uptake, the full spectrum of potential interactions and their long-term effects on bacterial populations remain to be fully elucidated.
Lastly, the translation of laboratory findings into clinically viable treatments represents a significant challenge. Many promising phospholipid strategies demonstrate efficacy in vitro but fail to show similar results in vivo due to factors such as host immune responses, pharmacokinetics, and the complex microenvironments found within the human body. Bridging this gap between laboratory success and clinical application requires extensive research and development efforts.
Another major challenge lies in the complexity of bacterial cell membranes and their interaction with phospholipids. The diverse composition of bacterial membranes across different species and strains makes it difficult to develop a one-size-fits-all solution. Researchers must navigate this variability to create phospholipid strategies that are both broadly effective and specific enough to target resistant bacteria without harming beneficial microorganisms or host cells.
The delivery of phospholipid-based treatments poses additional hurdles. Ensuring that these compounds reach their intended targets within the bacterial cell while maintaining stability and efficacy in various physiological environments is a significant technical challenge. This is particularly problematic when dealing with intracellular pathogens or bacteria protected by biofilms, which add layers of complexity to the delivery process.
Furthermore, the pharmaceutical industry faces regulatory and economic challenges in developing new antibiotic treatments, including those based on phospholipid strategies. The high costs of research and development, coupled with the relatively short market life of antibiotics due to resistance development, create a challenging economic landscape for innovation in this field.
There is also a need for more comprehensive understanding of the mechanisms by which phospholipids can combat antibiotic resistance. While some pathways have been identified, such as membrane disruption or enhanced antibiotic uptake, the full spectrum of potential interactions and their long-term effects on bacterial populations remain to be fully elucidated.
Lastly, the translation of laboratory findings into clinically viable treatments represents a significant challenge. Many promising phospholipid strategies demonstrate efficacy in vitro but fail to show similar results in vivo due to factors such as host immune responses, pharmacokinetics, and the complex microenvironments found within the human body. Bridging this gap between laboratory success and clinical application requires extensive research and development efforts.
Existing Phospholipid Solutions
01 Phospholipid-based antibiotic delivery systems
Phospholipids can be used to create liposomal or nanoparticle-based delivery systems for antibiotics. These systems can enhance the efficacy of antibiotics by improving their penetration into bacterial cells and biofilms, potentially overcoming some mechanisms of antibiotic resistance.- Phospholipid-based antibiotic resistance detection: Phospholipids can be used in methods for detecting antibiotic resistance in bacteria. These techniques often involve analyzing changes in bacterial membrane composition or integrity in response to antibiotics, providing a rapid and sensitive approach to identifying resistant strains.
- Phospholipid-antibiotic conjugates to combat resistance: Developing conjugates of phospholipids with antibiotics can enhance drug delivery and overcome certain resistance mechanisms. These conjugates may improve penetration through bacterial membranes or interfere with resistance-associated efflux pumps, potentially restoring antibiotic efficacy against resistant strains.
- Phospholipid membrane models for studying antibiotic resistance: Artificial phospholipid membrane models are used to study antibiotic resistance mechanisms and develop new strategies to combat them. These models allow for detailed investigation of drug-membrane interactions and the effects of membrane composition on antibiotic efficacy and resistance.
- Phospholipid-based nanocarriers for antibiotic delivery: Nanocarriers composed of phospholipids, such as liposomes, are being developed to improve antibiotic delivery and combat resistance. These systems can enhance drug penetration, protect antibiotics from degradation, and potentially overcome certain resistance mechanisms through targeted delivery.
- Phospholipid metabolism in antibiotic resistance: Research into bacterial phospholipid metabolism and its role in antibiotic resistance is ongoing. Understanding how changes in phospholipid composition or metabolism contribute to resistance can lead to new therapeutic targets or strategies for overcoming antibiotic resistance.
02 Membrane-targeting antibiotics using phospholipids
Phospholipids can be used to develop novel antibiotics that target bacterial cell membranes. These compounds can disrupt membrane integrity or interfere with essential membrane-associated processes, providing a strategy to combat antibiotic-resistant bacteria.Expand Specific Solutions03 Phospholipid-based diagnostic methods for antibiotic resistance
Phospholipids can be utilized in diagnostic assays to detect and characterize antibiotic resistance in bacteria. These methods may involve analyzing changes in bacterial membrane composition or using phospholipid-based biosensors to identify resistant strains.Expand Specific Solutions04 Modulation of bacterial phospholipid metabolism
Targeting bacterial phospholipid biosynthesis or metabolism pathways can be a strategy to overcome antibiotic resistance. This approach may involve developing inhibitors of key enzymes in phospholipid synthesis or altering membrane composition to increase antibiotic susceptibility.Expand Specific Solutions05 Phospholipid-based adjuvants for antibiotic therapy
Phospholipids can be used as adjuvants in combination with existing antibiotics to enhance their effectiveness against resistant bacteria. These formulations may improve antibiotic penetration, reduce dosage requirements, or modulate the host immune response to combat infections.Expand Specific Solutions
Key Industry Players
The field of phospholipid strategies for combating antibiotic resistance is in an early developmental stage, with significant potential for growth. The market size is expanding due to the urgent need for novel approaches to address the global threat of antimicrobial resistance. While the technology is still evolving, several key players are making strides in research and development. Companies like Avanti Polar Lipids and Vascular Biogenics are at the forefront, leveraging their expertise in lipid-based technologies. Research institutions such as The Scripps Research Institute and The University of Queensland are contributing valuable insights through academic studies. Pharmaceutical giants like Novartis are also exploring this area, indicating growing industry interest. The technology's maturity varies, with some applications nearing clinical trials while others remain in preclinical stages.
The Scripps Research Institute
Technical Solution: The Scripps Research Institute has been at the forefront of developing phospholipid strategies to combat antibiotic resistance. Their approach involves the design of synthetic antimicrobial lipopeptides that mimic natural host defense peptides. These lipopeptides are composed of a short peptide sequence attached to a lipid tail, which enhances their ability to penetrate bacterial membranes[13]. The institute has also explored the use of phospholipid-based nanocarriers to improve the delivery of existing antibiotics to resistant bacteria. One of their notable innovations is the development of "trojan horse" liposomes that can fuse with bacterial membranes and release antibiotics directly into the cell[14]. Additionally, Scripps researchers have investigated the potential of lipid-based adjuvants to boost the immune response against antibiotic-resistant pathogens, potentially reducing the reliance on traditional antibiotics[15].
Strengths: Cutting-edge research capabilities, interdisciplinary approach combining chemistry and microbiology. Weaknesses: Potential challenges in scaling up production of complex lipopeptides, longer timeline for clinical translation.
Avanti Polar Lipids LLC
Technical Solution: Avanti Polar Lipids LLC has developed innovative phospholipid-based strategies to combat antibiotic resistance. Their approach involves creating specialized liposomal formulations that encapsulate antibiotics, enhancing their delivery and efficacy against resistant bacteria. These liposomes are designed with specific phospholipid compositions that can fuse with bacterial membranes, bypassing traditional resistance mechanisms[1]. The company has also explored the use of cationic lipids in combination with antibiotics to disrupt bacterial biofilms, a common factor in antibiotic resistance[2]. Additionally, Avanti has developed lipid nanoparticles that can target and deliver antimicrobial peptides directly to infection sites, potentially overcoming resistance issues associated with conventional antibiotics[3].
Strengths: Specialized expertise in lipid formulations, potential for enhanced antibiotic delivery and efficacy. Weaknesses: May require complex manufacturing processes, potential for higher costs compared to traditional antibiotics.
Core Innovations
Pharmaceutical composition comprising sophorolipid in combination with an antibiotic
PatentInactiveUS20150094273A1
Innovation
- A synergistic pharmaceutical composition combining sophorolipid with antibiotics like cefaclor and tetracycline, formulated to increase antibiotic permeability across the outer membrane of bacteria, potentially overcoming resistance by using sophorolipid's membrane-disrupting properties to facilitate drug entry.
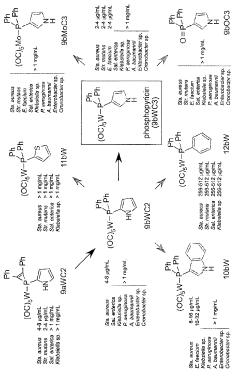
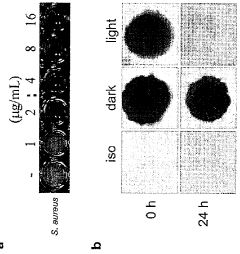
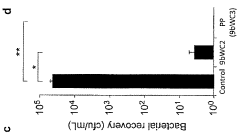
A potent synthetic inorganic antibacterial with activity against drug-resistant pathogens
PatentInactiveCA2972079A1
Innovation
- Development of a novel synthetic inorganic antibiotic, phosphopyricin, with a photosensitive chemical architecture that degrades in light, reducing selective pressure for resistance evolution, and targeting specific bacterial enzymes through competitive binding with molybdenum cofactors.
Regulatory Considerations
The regulatory landscape surrounding phospholipid strategies for combating antibiotic resistance is complex and evolving. Regulatory bodies, such as the FDA in the United States and the EMA in Europe, play crucial roles in overseeing the development and approval of novel antimicrobial therapies. These agencies have established specific guidelines for the evaluation of new antibiotics and alternative approaches to address antibiotic resistance.
One key consideration is the classification of phospholipid-based therapies. Depending on their mechanism of action and intended use, these strategies may be regulated as drugs, medical devices, or combination products. This classification significantly impacts the regulatory pathway and requirements for approval.
Safety and efficacy assessments for phospholipid-based approaches require rigorous preclinical and clinical studies. Regulatory agencies typically demand comprehensive data on the pharmacokinetics, pharmacodynamics, and toxicology of these novel therapies. Additionally, the potential for resistance development and the impact on the human microbiome must be thoroughly evaluated.
The regulatory framework also emphasizes the importance of antimicrobial stewardship. Developers of phospholipid strategies must demonstrate how their products align with efforts to preserve antibiotic effectiveness and minimize the emergence of resistance. This may involve specific labeling requirements, post-market surveillance plans, and restrictions on use.
Accelerated approval pathways, such as the FDA's Qualified Infectious Disease Product (QIDP) designation, may be applicable to certain phospholipid-based therapies. These programs aim to expedite the development and review of novel antimicrobial agents, providing incentives for innovation in this critical area.
International harmonization efforts, like those led by the International Council for Harmonisation (ICH), are increasingly important in the regulatory landscape. These initiatives seek to streamline the development and approval processes across different regions, potentially facilitating global access to new antimicrobial strategies.
Regulatory considerations also extend to manufacturing processes and quality control. Good Manufacturing Practices (GMP) and stringent quality assurance measures are essential for ensuring the consistency and safety of phospholipid-based products. Regulatory agencies may require specific validation studies and ongoing monitoring to maintain compliance.
As the field of phospholipid strategies for combating antibiotic resistance continues to advance, regulatory frameworks are likely to evolve. Ongoing dialogue between researchers, industry stakeholders, and regulatory authorities will be crucial in shaping appropriate and effective regulatory approaches for these innovative therapies.
One key consideration is the classification of phospholipid-based therapies. Depending on their mechanism of action and intended use, these strategies may be regulated as drugs, medical devices, or combination products. This classification significantly impacts the regulatory pathway and requirements for approval.
Safety and efficacy assessments for phospholipid-based approaches require rigorous preclinical and clinical studies. Regulatory agencies typically demand comprehensive data on the pharmacokinetics, pharmacodynamics, and toxicology of these novel therapies. Additionally, the potential for resistance development and the impact on the human microbiome must be thoroughly evaluated.
The regulatory framework also emphasizes the importance of antimicrobial stewardship. Developers of phospholipid strategies must demonstrate how their products align with efforts to preserve antibiotic effectiveness and minimize the emergence of resistance. This may involve specific labeling requirements, post-market surveillance plans, and restrictions on use.
Accelerated approval pathways, such as the FDA's Qualified Infectious Disease Product (QIDP) designation, may be applicable to certain phospholipid-based therapies. These programs aim to expedite the development and review of novel antimicrobial agents, providing incentives for innovation in this critical area.
International harmonization efforts, like those led by the International Council for Harmonisation (ICH), are increasingly important in the regulatory landscape. These initiatives seek to streamline the development and approval processes across different regions, potentially facilitating global access to new antimicrobial strategies.
Regulatory considerations also extend to manufacturing processes and quality control. Good Manufacturing Practices (GMP) and stringent quality assurance measures are essential for ensuring the consistency and safety of phospholipid-based products. Regulatory agencies may require specific validation studies and ongoing monitoring to maintain compliance.
As the field of phospholipid strategies for combating antibiotic resistance continues to advance, regulatory frameworks are likely to evolve. Ongoing dialogue between researchers, industry stakeholders, and regulatory authorities will be crucial in shaping appropriate and effective regulatory approaches for these innovative therapies.
Environmental Impact
The environmental impact of phospholipid strategies for combating antibiotic resistance is a critical consideration in the development and implementation of these novel approaches. As antibiotics and their resistant counterparts enter the environment, they can have far-reaching consequences on ecosystems and human health. Phospholipid-based strategies offer potential advantages in mitigating these environmental concerns.
One of the primary environmental benefits of phospholipid approaches is their potential to reduce the overall use of conventional antibiotics. By enhancing the efficacy of existing antibiotics or providing alternative antimicrobial mechanisms, these strategies may lead to a decrease in the quantity of antibiotics released into the environment. This reduction can help minimize the selective pressure on bacterial populations, potentially slowing the development and spread of antibiotic resistance in environmental settings.
Phospholipids are naturally occurring compounds found in cell membranes, which suggests they may have a lower environmental impact compared to synthetic antibiotics. Their biodegradability and biocompatibility could result in reduced persistence in the environment, limiting long-term ecological effects. However, the environmental fate and potential bioaccumulation of modified or synthetic phospholipids used in these strategies require thorough investigation to ensure their safety.
The use of phospholipid strategies may also contribute to the preservation of beneficial microbial communities in various ecosystems. By targeting specific pathogens or resistance mechanisms, these approaches could potentially have less broad-spectrum effects on environmental microbiota compared to traditional antibiotics. This selectivity could help maintain the delicate balance of microbial ecosystems in soil, water, and other natural habitats.
Furthermore, phospholipid-based technologies might offer opportunities for more environmentally friendly manufacturing processes. The production of these compounds could potentially be achieved through sustainable methods, such as microbial fermentation or green chemistry approaches, reducing the environmental footprint associated with antibiotic production.
However, it is crucial to consider potential negative environmental impacts as well. The large-scale production and use of phospholipid-based antimicrobials could lead to increased phosphorus loading in aquatic environments, potentially contributing to eutrophication. Additionally, the introduction of novel phospholipid compounds into ecosystems may have unforeseen consequences on non-target organisms and food webs.
Comprehensive environmental risk assessments and life cycle analyses are essential to fully understand and mitigate any potential adverse effects of phospholipid strategies. These evaluations should consider the entire lifecycle of these compounds, from production to disposal, and their interactions with various environmental compartments.
One of the primary environmental benefits of phospholipid approaches is their potential to reduce the overall use of conventional antibiotics. By enhancing the efficacy of existing antibiotics or providing alternative antimicrobial mechanisms, these strategies may lead to a decrease in the quantity of antibiotics released into the environment. This reduction can help minimize the selective pressure on bacterial populations, potentially slowing the development and spread of antibiotic resistance in environmental settings.
Phospholipids are naturally occurring compounds found in cell membranes, which suggests they may have a lower environmental impact compared to synthetic antibiotics. Their biodegradability and biocompatibility could result in reduced persistence in the environment, limiting long-term ecological effects. However, the environmental fate and potential bioaccumulation of modified or synthetic phospholipids used in these strategies require thorough investigation to ensure their safety.
The use of phospholipid strategies may also contribute to the preservation of beneficial microbial communities in various ecosystems. By targeting specific pathogens or resistance mechanisms, these approaches could potentially have less broad-spectrum effects on environmental microbiota compared to traditional antibiotics. This selectivity could help maintain the delicate balance of microbial ecosystems in soil, water, and other natural habitats.
Furthermore, phospholipid-based technologies might offer opportunities for more environmentally friendly manufacturing processes. The production of these compounds could potentially be achieved through sustainable methods, such as microbial fermentation or green chemistry approaches, reducing the environmental footprint associated with antibiotic production.
However, it is crucial to consider potential negative environmental impacts as well. The large-scale production and use of phospholipid-based antimicrobials could lead to increased phosphorus loading in aquatic environments, potentially contributing to eutrophication. Additionally, the introduction of novel phospholipid compounds into ecosystems may have unforeseen consequences on non-target organisms and food webs.
Comprehensive environmental risk assessments and life cycle analyses are essential to fully understand and mitigate any potential adverse effects of phospholipid strategies. These evaluations should consider the entire lifecycle of these compounds, from production to disposal, and their interactions with various environmental compartments.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!