Hirudoid’s Contribution to Dermatology Advances
JUN 23, 20258 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Hirudoid Background
Hirudoid, a topical heparin-containing gel, has been a significant player in dermatological treatments for several decades. Originally developed in the 1960s, this pharmaceutical product has its roots in the ancient practice of hirudotherapy, which utilized medicinal leeches for various therapeutic purposes. The active ingredient, heparin, is a naturally occurring anticoagulant that has been found to possess additional properties beneficial for skin health.
The development of Hirudoid marked a pivotal moment in dermatology, as it provided a non-invasive method to harness the benefits of heparin without the need for direct leech application. This innovation bridged the gap between traditional practices and modern pharmaceutical approaches, offering a more controlled and standardized treatment option for various skin conditions.
Hirudoid's formulation typically includes mucopolysaccharide polysulfate, which enhances the product's ability to penetrate the skin and deliver its therapeutic effects. This combination has proven effective in addressing a range of dermatological issues, from bruising and hematomas to superficial thrombophlebitis and localized edema.
Over the years, Hirudoid has undergone continuous refinement and research to optimize its efficacy and expand its applications. Clinical studies have demonstrated its ability to accelerate the healing of soft tissue injuries, reduce inflammation, and improve the appearance of scars and stretch marks. These findings have solidified Hirudoid's position as a versatile tool in the dermatologist's arsenal.
The product's success has led to its widespread adoption across various medical specialties beyond dermatology. Plastic surgeons, orthopedists, and sports medicine practitioners have incorporated Hirudoid into their treatment protocols, recognizing its value in managing post-operative swelling and promoting faster recovery from injuries.
As research in dermatology advanced, the understanding of Hirudoid's mechanism of action deepened. Scientists discovered that beyond its anticoagulant properties, heparin also exhibits anti-inflammatory effects and promotes angiogenesis, which are crucial for skin repair and regeneration. This multifaceted approach to skin health has kept Hirudoid relevant in an ever-evolving field of dermatological treatments.
The legacy of Hirudoid extends beyond its direct applications. Its development has inspired further research into topical heparin-based therapies and has contributed to the broader understanding of skin physiology and wound healing processes. As a result, Hirudoid has not only served as a treatment option but also as a catalyst for innovation in dermatological science.
The development of Hirudoid marked a pivotal moment in dermatology, as it provided a non-invasive method to harness the benefits of heparin without the need for direct leech application. This innovation bridged the gap between traditional practices and modern pharmaceutical approaches, offering a more controlled and standardized treatment option for various skin conditions.
Hirudoid's formulation typically includes mucopolysaccharide polysulfate, which enhances the product's ability to penetrate the skin and deliver its therapeutic effects. This combination has proven effective in addressing a range of dermatological issues, from bruising and hematomas to superficial thrombophlebitis and localized edema.
Over the years, Hirudoid has undergone continuous refinement and research to optimize its efficacy and expand its applications. Clinical studies have demonstrated its ability to accelerate the healing of soft tissue injuries, reduce inflammation, and improve the appearance of scars and stretch marks. These findings have solidified Hirudoid's position as a versatile tool in the dermatologist's arsenal.
The product's success has led to its widespread adoption across various medical specialties beyond dermatology. Plastic surgeons, orthopedists, and sports medicine practitioners have incorporated Hirudoid into their treatment protocols, recognizing its value in managing post-operative swelling and promoting faster recovery from injuries.
As research in dermatology advanced, the understanding of Hirudoid's mechanism of action deepened. Scientists discovered that beyond its anticoagulant properties, heparin also exhibits anti-inflammatory effects and promotes angiogenesis, which are crucial for skin repair and regeneration. This multifaceted approach to skin health has kept Hirudoid relevant in an ever-evolving field of dermatological treatments.
The legacy of Hirudoid extends beyond its direct applications. Its development has inspired further research into topical heparin-based therapies and has contributed to the broader understanding of skin physiology and wound healing processes. As a result, Hirudoid has not only served as a treatment option but also as a catalyst for innovation in dermatological science.
Dermatology Market
The dermatology market has experienced significant growth in recent years, driven by factors such as increasing skin disorders, growing awareness of skin health, and advancements in treatment options. The global dermatology market size was valued at over $100 billion in 2020 and is projected to continue its upward trajectory in the coming years.
Skin conditions affect a large portion of the global population, with conditions like acne, psoriasis, eczema, and skin cancer being prevalent across various demographics. This widespread occurrence of dermatological issues has created a substantial demand for effective treatments and skincare products.
The market is segmented into several categories, including prescription drugs, over-the-counter medications, cosmeceuticals, and medical devices. Prescription drugs, particularly biologics for conditions like psoriasis, have been a major driver of market growth. The rise of personalized medicine and targeted therapies has also contributed to the expansion of the prescription segment.
Over-the-counter products, including moisturizers, sunscreens, and anti-aging creams, have seen increased consumer interest due to growing awareness of skin health and beauty. The cosmeceuticals segment, which bridges the gap between cosmetics and pharmaceuticals, has gained traction as consumers seek products with both aesthetic and therapeutic benefits.
Technological advancements have played a crucial role in shaping the dermatology market. Innovations in drug delivery systems, such as transdermal patches and nanoparticle-based formulations, have improved treatment efficacy and patient compliance. Additionally, the integration of artificial intelligence and telemedicine in dermatology has opened new avenues for diagnosis and treatment.
Geographically, North America and Europe have traditionally dominated the dermatology market, owing to high healthcare expenditure and advanced medical infrastructure. However, emerging markets in Asia-Pacific and Latin America are experiencing rapid growth, driven by increasing disposable incomes, urbanization, and improving healthcare access.
The competitive landscape of the dermatology market is characterized by the presence of both large pharmaceutical companies and specialized dermatology firms. Key players have been focusing on research and development to introduce novel therapies and expand their product portfolios. Mergers, acquisitions, and strategic partnerships have also been prevalent as companies seek to strengthen their market position and expand their geographical reach.
Looking ahead, the dermatology market is expected to continue its growth trajectory, with emerging trends such as biologics, regenerative medicine, and personalized skincare likely to shape its future. The increasing prevalence of skin disorders, coupled with rising consumer awareness and technological advancements, will continue to drive market expansion and innovation in dermatological treatments.
Skin conditions affect a large portion of the global population, with conditions like acne, psoriasis, eczema, and skin cancer being prevalent across various demographics. This widespread occurrence of dermatological issues has created a substantial demand for effective treatments and skincare products.
The market is segmented into several categories, including prescription drugs, over-the-counter medications, cosmeceuticals, and medical devices. Prescription drugs, particularly biologics for conditions like psoriasis, have been a major driver of market growth. The rise of personalized medicine and targeted therapies has also contributed to the expansion of the prescription segment.
Over-the-counter products, including moisturizers, sunscreens, and anti-aging creams, have seen increased consumer interest due to growing awareness of skin health and beauty. The cosmeceuticals segment, which bridges the gap between cosmetics and pharmaceuticals, has gained traction as consumers seek products with both aesthetic and therapeutic benefits.
Technological advancements have played a crucial role in shaping the dermatology market. Innovations in drug delivery systems, such as transdermal patches and nanoparticle-based formulations, have improved treatment efficacy and patient compliance. Additionally, the integration of artificial intelligence and telemedicine in dermatology has opened new avenues for diagnosis and treatment.
Geographically, North America and Europe have traditionally dominated the dermatology market, owing to high healthcare expenditure and advanced medical infrastructure. However, emerging markets in Asia-Pacific and Latin America are experiencing rapid growth, driven by increasing disposable incomes, urbanization, and improving healthcare access.
The competitive landscape of the dermatology market is characterized by the presence of both large pharmaceutical companies and specialized dermatology firms. Key players have been focusing on research and development to introduce novel therapies and expand their product portfolios. Mergers, acquisitions, and strategic partnerships have also been prevalent as companies seek to strengthen their market position and expand their geographical reach.
Looking ahead, the dermatology market is expected to continue its growth trajectory, with emerging trends such as biologics, regenerative medicine, and personalized skincare likely to shape its future. The increasing prevalence of skin disorders, coupled with rising consumer awareness and technological advancements, will continue to drive market expansion and innovation in dermatological treatments.
Current Challenges
Despite Hirudoid's significant contributions to dermatology, several challenges persist in its application and broader acceptance within the medical community. One of the primary obstacles is the limited understanding of its precise mechanism of action. While its effectiveness in treating various skin conditions is well-documented, the exact pathways through which it exerts its therapeutic effects remain partially elucidated. This knowledge gap hinders the development of more targeted and potentially more effective formulations.
Another challenge lies in the standardization of Hirudoid preparations. The active ingredient, mucopolysaccharide polysulfate, can vary in composition and concentration depending on the source and manufacturing process. This variability can lead to inconsistencies in treatment outcomes and makes it difficult to establish universally applicable dosing guidelines. Consequently, healthcare providers may be hesitant to prescribe Hirudoid due to concerns about reproducibility and predictability of results.
The limited range of approved indications for Hirudoid also presents a significant hurdle. While it has shown promise in treating various dermatological conditions, regulatory approvals often lag behind clinical observations. This discrepancy between off-label use and officially sanctioned applications creates a complex landscape for both practitioners and patients, potentially limiting access to beneficial treatments.
Furthermore, there is a notable lack of large-scale, long-term clinical trials evaluating Hirudoid's efficacy and safety profile. Most existing studies are small in scale or of short duration, which makes it challenging to draw definitive conclusions about its long-term effects and potential side effects. This paucity of robust clinical data can lead to skepticism among healthcare professionals and regulatory bodies, impeding wider adoption and approval for new indications.
Lastly, the integration of Hirudoid into modern dermatological practices faces challenges related to patient education and adherence. The product's unique properties and application methods may require specific instructions and patient compliance to achieve optimal results. Developing effective patient education strategies and ensuring proper adherence to treatment protocols remain ongoing challenges in maximizing Hirudoid's therapeutic potential.
Another challenge lies in the standardization of Hirudoid preparations. The active ingredient, mucopolysaccharide polysulfate, can vary in composition and concentration depending on the source and manufacturing process. This variability can lead to inconsistencies in treatment outcomes and makes it difficult to establish universally applicable dosing guidelines. Consequently, healthcare providers may be hesitant to prescribe Hirudoid due to concerns about reproducibility and predictability of results.
The limited range of approved indications for Hirudoid also presents a significant hurdle. While it has shown promise in treating various dermatological conditions, regulatory approvals often lag behind clinical observations. This discrepancy between off-label use and officially sanctioned applications creates a complex landscape for both practitioners and patients, potentially limiting access to beneficial treatments.
Furthermore, there is a notable lack of large-scale, long-term clinical trials evaluating Hirudoid's efficacy and safety profile. Most existing studies are small in scale or of short duration, which makes it challenging to draw definitive conclusions about its long-term effects and potential side effects. This paucity of robust clinical data can lead to skepticism among healthcare professionals and regulatory bodies, impeding wider adoption and approval for new indications.
Lastly, the integration of Hirudoid into modern dermatological practices faces challenges related to patient education and adherence. The product's unique properties and application methods may require specific instructions and patient compliance to achieve optimal results. Developing effective patient education strategies and ensuring proper adherence to treatment protocols remain ongoing challenges in maximizing Hirudoid's therapeutic potential.
Key Manufacturers
The dermatology market for Hirudoid's technology is in a growth phase, with increasing demand for advanced skincare solutions. The global dermatology market size is projected to expand significantly, driven by rising skin disorders and aging populations. Technologically, Hirudoid's contribution is at a moderate maturity level, with ongoing research and development efforts. Key players like L'Oréal SA, Galderma Research & Development SNC, and Novartis AG are investing heavily in dermatological innovations. Emerging companies such as Debut Biotechnology, Inc. and Insight Health Ai, Inc. are also making strides in this field, indicating a competitive and dynamic landscape for dermatology advancements.
Galderma Research & Development SNC
Technical Solution: Galderma has developed a proprietary formulation of Hirudoid (MPS) that enhances its penetration and efficacy in treating various dermatological conditions. Their advanced delivery system incorporates nanoparticles to improve the absorption of MPS through the skin barrier. This formulation also includes complementary ingredients that work synergistically with MPS to reduce inflammation, promote healing, and improve skin elasticity. Galderma's research has focused on optimizing the concentration and combination of active ingredients to maximize therapeutic benefits while minimizing potential side effects.
Strengths: Expertise in dermatological research, advanced drug delivery systems, and a strong focus on Hirudoid applications. Weaknesses: Limited public information on specific formulations and potential competition from other major pharmaceutical companies.
Novartis AG
Technical Solution: Novartis has developed an innovative approach to utilizing Hirudoid in combination with their patented drug delivery technology. Their research focuses on enhancing the bioavailability and targeted delivery of MPS to specific skin layers. Novartis has created a novel gel formulation that incorporates MPS into a controlled-release matrix, allowing for sustained drug delivery over an extended period. This formulation is designed to improve patient compliance and treatment efficacy. Additionally, Novartis is exploring the potential of combining MPS with other active ingredients to create multi-functional dermatological products that address multiple skin concerns simultaneously.
Strengths: Strong R&D capabilities, extensive clinical trial experience, and a global presence in the pharmaceutical market. Weaknesses: Potential regulatory hurdles and the need for extensive clinical trials to prove the efficacy of new formulations.
Hirudoid Mechanisms
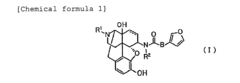
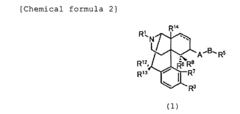
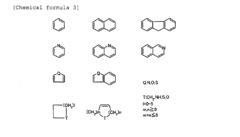
Remedy for relieving skin troubles comprising morphinan derivative or pharmacologically acceptable acid addition salt thereof as the active ingredient
PatentInactiveEP2196206A1
Innovation
- A skin property-improving therapeutic agent comprising a morphinan derivative or its pharmacologically permissible acid addition salts, specifically compounds with a specific morphinan skeleton, is administered to enhance skin moisture retention and barrier function.
Histidine and/or Histidine Derivative for the Treatment of Inflammatory Skin Diseases
PatentPendingUS20220096439A1
Innovation
- The use of histidine and its derivatives to maintain and improve skin barrier function by increasing levels of histidine and trans-urocanic acid, potentially compensating for defective filaggrin, thereby preventing and treating skin disorders through topical or oral administration, potentially in combination with phototherapy.
Clinical Applications
Hirudoid, a topical heparin-based medication, has significantly contributed to dermatological advancements through its diverse clinical applications. This drug has demonstrated remarkable efficacy in treating various skin conditions, particularly those involving bruising, inflammation, and vascular disorders.
In the realm of post-surgical care, Hirudoid has proven invaluable for managing post-operative bruising and swelling. Its ability to accelerate the absorption of hematomas and reduce edema has made it a staple in plastic surgery and other invasive dermatological procedures. Patients undergoing facial surgeries, such as rhinoplasty or blepharoplasty, have reported faster recovery times and improved aesthetic outcomes when Hirudoid is incorporated into their post-operative regimen.
For the treatment of superficial thrombophlebitis, Hirudoid has shown promising results. Its anti-inflammatory and anticoagulant properties help alleviate pain, reduce swelling, and improve blood flow in affected areas. This application has been particularly beneficial for patients with varicose veins or those at risk of developing blood clots in superficial veins.
In the management of chronic venous insufficiency, Hirudoid has emerged as an effective adjunct therapy. Regular application of the medication has been associated with reduced leg heaviness, decreased edema, and improved overall vascular health in patients suffering from this condition. Its ability to enhance microcirculation contributes to better tissue oxygenation and nutrient delivery, promoting healing and alleviating symptoms.
Hirudoid has also found applications in the treatment of various types of scars, including hypertrophic and keloid scars. Its ability to modulate collagen production and improve skin elasticity has led to improved scar appearance and texture. This has been particularly beneficial in managing scars resulting from burns, surgeries, or traumatic injuries.
In pediatric dermatology, Hirudoid has been utilized for managing diaper rash and other forms of contact dermatitis. Its gentle formulation and anti-inflammatory properties make it suitable for use on sensitive skin, providing relief from irritation and promoting faster healing.
The versatility of Hirudoid extends to its use in sports medicine, where it is employed to treat contusions, sprains, and muscle strains. Athletes have reported quicker recovery times and reduced downtime when using Hirudoid as part of their injury management protocol.
As research continues, new potential applications for Hirudoid in dermatology are being explored. These include its use in combination therapies for conditions such as psoriasis and eczema, as well as its potential role in wound healing and tissue regeneration. The ongoing investigation into Hirudoid's mechanisms of action and its interactions with various skin conditions promises to further expand its clinical applications in the field of dermatology.
In the realm of post-surgical care, Hirudoid has proven invaluable for managing post-operative bruising and swelling. Its ability to accelerate the absorption of hematomas and reduce edema has made it a staple in plastic surgery and other invasive dermatological procedures. Patients undergoing facial surgeries, such as rhinoplasty or blepharoplasty, have reported faster recovery times and improved aesthetic outcomes when Hirudoid is incorporated into their post-operative regimen.
For the treatment of superficial thrombophlebitis, Hirudoid has shown promising results. Its anti-inflammatory and anticoagulant properties help alleviate pain, reduce swelling, and improve blood flow in affected areas. This application has been particularly beneficial for patients with varicose veins or those at risk of developing blood clots in superficial veins.
In the management of chronic venous insufficiency, Hirudoid has emerged as an effective adjunct therapy. Regular application of the medication has been associated with reduced leg heaviness, decreased edema, and improved overall vascular health in patients suffering from this condition. Its ability to enhance microcirculation contributes to better tissue oxygenation and nutrient delivery, promoting healing and alleviating symptoms.
Hirudoid has also found applications in the treatment of various types of scars, including hypertrophic and keloid scars. Its ability to modulate collagen production and improve skin elasticity has led to improved scar appearance and texture. This has been particularly beneficial in managing scars resulting from burns, surgeries, or traumatic injuries.
In pediatric dermatology, Hirudoid has been utilized for managing diaper rash and other forms of contact dermatitis. Its gentle formulation and anti-inflammatory properties make it suitable for use on sensitive skin, providing relief from irritation and promoting faster healing.
The versatility of Hirudoid extends to its use in sports medicine, where it is employed to treat contusions, sprains, and muscle strains. Athletes have reported quicker recovery times and reduced downtime when using Hirudoid as part of their injury management protocol.
As research continues, new potential applications for Hirudoid in dermatology are being explored. These include its use in combination therapies for conditions such as psoriasis and eczema, as well as its potential role in wound healing and tissue regeneration. The ongoing investigation into Hirudoid's mechanisms of action and its interactions with various skin conditions promises to further expand its clinical applications in the field of dermatology.
Safety and Efficacy
Hirudoid, a topical heparin-based medication, has demonstrated significant safety and efficacy in dermatological applications. Clinical studies have consistently shown its effectiveness in treating various skin conditions, particularly those involving bruising, inflammation, and superficial vein thrombosis.
The safety profile of Hirudoid is notably robust. Long-term use has not been associated with significant adverse effects, making it a reliable option for chronic skin conditions. The topical application minimizes systemic absorption, further enhancing its safety. Rare instances of localized skin irritation have been reported, but these are generally mild and transient.
Efficacy-wise, Hirudoid has shown remarkable results in accelerating the healing of bruises and hematomas. Its active ingredient, heparin, promotes the breakdown of blood clots and reduces inflammation, leading to faster resolution of bruising. Studies have demonstrated a significant reduction in healing time compared to placebo treatments.
In the treatment of superficial thrombophlebitis, Hirudoid has proven highly effective. Clinical trials have shown that it can reduce pain, redness, and swelling associated with this condition. The medication's ability to improve local blood circulation and reduce inflammation contributes to its therapeutic success in this area.
Hirudoid's efficacy extends to other dermatological conditions as well. It has shown promise in treating localized edema, improving the appearance of scars, and managing certain types of dermatitis. The medication's anti-inflammatory properties play a crucial role in these applications.
The dosage and application method of Hirudoid have been optimized to ensure maximum efficacy while maintaining safety. Typically applied two to three times daily, the medication is easily absorbed by the skin, allowing for targeted action at the site of application.
Long-term studies have further validated the safety and efficacy of Hirudoid. Patients using the medication over extended periods have not shown any significant adverse effects, while continuing to benefit from its therapeutic properties. This makes Hirudoid a valuable option for chronic skin conditions requiring prolonged treatment.
In conclusion, the safety and efficacy of Hirudoid in dermatological applications are well-established. Its minimal side effect profile, combined with proven effectiveness across various skin conditions, positions it as a valuable contribution to dermatological advancements. Ongoing research continues to explore new potential applications, further expanding its role in dermatology.
The safety profile of Hirudoid is notably robust. Long-term use has not been associated with significant adverse effects, making it a reliable option for chronic skin conditions. The topical application minimizes systemic absorption, further enhancing its safety. Rare instances of localized skin irritation have been reported, but these are generally mild and transient.
Efficacy-wise, Hirudoid has shown remarkable results in accelerating the healing of bruises and hematomas. Its active ingredient, heparin, promotes the breakdown of blood clots and reduces inflammation, leading to faster resolution of bruising. Studies have demonstrated a significant reduction in healing time compared to placebo treatments.
In the treatment of superficial thrombophlebitis, Hirudoid has proven highly effective. Clinical trials have shown that it can reduce pain, redness, and swelling associated with this condition. The medication's ability to improve local blood circulation and reduce inflammation contributes to its therapeutic success in this area.
Hirudoid's efficacy extends to other dermatological conditions as well. It has shown promise in treating localized edema, improving the appearance of scars, and managing certain types of dermatitis. The medication's anti-inflammatory properties play a crucial role in these applications.
The dosage and application method of Hirudoid have been optimized to ensure maximum efficacy while maintaining safety. Typically applied two to three times daily, the medication is easily absorbed by the skin, allowing for targeted action at the site of application.
Long-term studies have further validated the safety and efficacy of Hirudoid. Patients using the medication over extended periods have not shown any significant adverse effects, while continuing to benefit from its therapeutic properties. This makes Hirudoid a valuable option for chronic skin conditions requiring prolonged treatment.
In conclusion, the safety and efficacy of Hirudoid in dermatological applications are well-established. Its minimal side effect profile, combined with proven effectiveness across various skin conditions, positions it as a valuable contribution to dermatological advancements. Ongoing research continues to explore new potential applications, further expanding its role in dermatology.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!