Hirudoid’s Role in Dermatological Treatments
JUN 23, 20258 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Hirudoid Background
Hirudoid, also known as mucopolysaccharide polysulfate (MPS), is a semi-synthetic compound derived from mammalian tissues. It was first developed in the 1960s as a potential treatment for various dermatological conditions. The active ingredient in Hirudoid is a glycosaminoglycan polysulfate, which is structurally similar to heparin but with distinct pharmacological properties.
The development of Hirudoid was driven by the need for effective topical treatments in dermatology that could address multiple skin concerns simultaneously. Its unique composition allows it to penetrate the skin barrier and exert its effects in the deeper layers of the dermis, making it particularly useful for conditions affecting the skin's structure and function.
Hirudoid's primary mechanism of action involves its ability to inhibit inflammatory processes and promote tissue repair. It has been shown to reduce the activity of certain enzymes involved in tissue breakdown, such as hyaluronidase and elastase. Additionally, Hirudoid enhances the synthesis of extracellular matrix components, including collagen and proteoglycans, which are crucial for maintaining skin integrity and elasticity.
Over the years, Hirudoid has been extensively studied for its potential applications in various dermatological conditions. Its anti-inflammatory and anti-edematous properties have made it a valuable tool in the treatment of bruises, hematomas, and superficial thrombophlebitis. Furthermore, its ability to promote tissue repair has led to its use in wound healing and the management of scars.
The evolution of Hirudoid's role in dermatological treatments has been marked by a growing body of clinical evidence supporting its efficacy and safety. Numerous studies have demonstrated its effectiveness in reducing pain, swelling, and discoloration associated with soft tissue injuries. Its use has expanded beyond traditional dermatological applications to include potential benefits in cosmetic dermatology, particularly in the realm of anti-aging treatments.
As research in the field of dermatology has advanced, the understanding of Hirudoid's molecular mechanisms has deepened. This has led to the exploration of new formulations and delivery systems to enhance its therapeutic potential. The development of gel-based and cream-based preparations has improved its ease of application and patient compliance, contributing to its widespread adoption in clinical practice.
In recent years, there has been renewed interest in Hirudoid's potential applications in combination therapies. Researchers have been investigating its synergistic effects when used alongside other topical agents, such as corticosteroids or retinoids, to enhance overall treatment outcomes in various skin conditions.
The development of Hirudoid was driven by the need for effective topical treatments in dermatology that could address multiple skin concerns simultaneously. Its unique composition allows it to penetrate the skin barrier and exert its effects in the deeper layers of the dermis, making it particularly useful for conditions affecting the skin's structure and function.
Hirudoid's primary mechanism of action involves its ability to inhibit inflammatory processes and promote tissue repair. It has been shown to reduce the activity of certain enzymes involved in tissue breakdown, such as hyaluronidase and elastase. Additionally, Hirudoid enhances the synthesis of extracellular matrix components, including collagen and proteoglycans, which are crucial for maintaining skin integrity and elasticity.
Over the years, Hirudoid has been extensively studied for its potential applications in various dermatological conditions. Its anti-inflammatory and anti-edematous properties have made it a valuable tool in the treatment of bruises, hematomas, and superficial thrombophlebitis. Furthermore, its ability to promote tissue repair has led to its use in wound healing and the management of scars.
The evolution of Hirudoid's role in dermatological treatments has been marked by a growing body of clinical evidence supporting its efficacy and safety. Numerous studies have demonstrated its effectiveness in reducing pain, swelling, and discoloration associated with soft tissue injuries. Its use has expanded beyond traditional dermatological applications to include potential benefits in cosmetic dermatology, particularly in the realm of anti-aging treatments.
As research in the field of dermatology has advanced, the understanding of Hirudoid's molecular mechanisms has deepened. This has led to the exploration of new formulations and delivery systems to enhance its therapeutic potential. The development of gel-based and cream-based preparations has improved its ease of application and patient compliance, contributing to its widespread adoption in clinical practice.
In recent years, there has been renewed interest in Hirudoid's potential applications in combination therapies. Researchers have been investigating its synergistic effects when used alongside other topical agents, such as corticosteroids or retinoids, to enhance overall treatment outcomes in various skin conditions.
Market Analysis
The market for dermatological treatments has been experiencing significant growth in recent years, driven by factors such as increasing skin disorders, growing awareness of skin health, and advancements in treatment options. Hirudoid, a topical medication containing mucopolysaccharide polysulfate (MPS), has established itself as a notable player in this expanding market.
The global dermatology drugs market, which encompasses Hirudoid and similar products, was valued at approximately $36.82 billion in 2022 and is projected to reach $63.99 billion by 2029, growing at a CAGR of 8.2% during the forecast period. This growth is attributed to the rising prevalence of skin conditions such as acne, psoriasis, and eczema, as well as an aging population more prone to skin-related issues.
Hirudoid's specific market segment, focusing on treatments for bruises, superficial thrombophlebitis, and scar management, has shown steady demand. The product's ability to reduce inflammation, improve blood circulation, and aid in tissue repair positions it well within the broader wound care and scar management markets.
The wound care market, which includes treatments for bruises and minor injuries, is expected to grow from $20.8 billion in 2021 to $25.8 billion by 2026, with a CAGR of 4.4%. Hirudoid's properties make it a relevant player in this sector, particularly for post-surgical care and sports-related injuries.
In the scar management market, which was valued at $15.8 billion in 2020 and is projected to reach $25.2 billion by 2028, Hirudoid has found a niche. The increasing number of surgical procedures and growing aesthetic consciousness among consumers are driving the demand for effective scar reduction treatments.
Geographically, Europe and North America currently dominate the dermatological treatments market, accounting for over 60% of the global market share. However, the Asia-Pacific region is expected to witness the fastest growth, with a CAGR of 9.5% from 2021 to 2028, presenting significant opportunities for products like Hirudoid.
Consumer trends indicate a growing preference for non-invasive and topical treatments, aligning well with Hirudoid's application method. Additionally, there is an increasing demand for products with natural or naturally derived ingredients, which may influence future formulations of Hirudoid or similar products.
The competitive landscape for Hirudoid includes both established pharmaceutical companies and emerging biotech firms focusing on innovative dermatological solutions. Key competitors in this space are developing advanced formulations and delivery systems to enhance efficacy and patient compliance, driving ongoing research and development efforts in the sector.
The global dermatology drugs market, which encompasses Hirudoid and similar products, was valued at approximately $36.82 billion in 2022 and is projected to reach $63.99 billion by 2029, growing at a CAGR of 8.2% during the forecast period. This growth is attributed to the rising prevalence of skin conditions such as acne, psoriasis, and eczema, as well as an aging population more prone to skin-related issues.
Hirudoid's specific market segment, focusing on treatments for bruises, superficial thrombophlebitis, and scar management, has shown steady demand. The product's ability to reduce inflammation, improve blood circulation, and aid in tissue repair positions it well within the broader wound care and scar management markets.
The wound care market, which includes treatments for bruises and minor injuries, is expected to grow from $20.8 billion in 2021 to $25.8 billion by 2026, with a CAGR of 4.4%. Hirudoid's properties make it a relevant player in this sector, particularly for post-surgical care and sports-related injuries.
In the scar management market, which was valued at $15.8 billion in 2020 and is projected to reach $25.2 billion by 2028, Hirudoid has found a niche. The increasing number of surgical procedures and growing aesthetic consciousness among consumers are driving the demand for effective scar reduction treatments.
Geographically, Europe and North America currently dominate the dermatological treatments market, accounting for over 60% of the global market share. However, the Asia-Pacific region is expected to witness the fastest growth, with a CAGR of 9.5% from 2021 to 2028, presenting significant opportunities for products like Hirudoid.
Consumer trends indicate a growing preference for non-invasive and topical treatments, aligning well with Hirudoid's application method. Additionally, there is an increasing demand for products with natural or naturally derived ingredients, which may influence future formulations of Hirudoid or similar products.
The competitive landscape for Hirudoid includes both established pharmaceutical companies and emerging biotech firms focusing on innovative dermatological solutions. Key competitors in this space are developing advanced formulations and delivery systems to enhance efficacy and patient compliance, driving ongoing research and development efforts in the sector.
Current Challenges
Hirudoid, a topical heparin-based medication, faces several challenges in its application for dermatological treatments. One of the primary issues is the limited penetration of the active ingredient through the skin barrier. The stratum corneum, the outermost layer of the epidermis, acts as a formidable obstacle to drug absorption, reducing the efficacy of topically applied medications. This challenge necessitates the development of advanced drug delivery systems to enhance the bioavailability of Hirudoid in targeted skin layers.
Another significant hurdle is the lack of comprehensive clinical data supporting Hirudoid's efficacy across a wide range of dermatological conditions. While it has shown promise in treating certain skin disorders, such as superficial thrombophlebitis and bruising, its effectiveness in other areas remains under-researched. This knowledge gap hinders the expansion of Hirudoid's applications in dermatology and limits its acceptance among healthcare professionals.
The potential for adverse reactions and drug interactions poses an ongoing challenge for Hirudoid's widespread use. Although generally well-tolerated, some patients may experience skin irritation, allergic reactions, or bleeding complications, particularly when used in conjunction with other anticoagulant medications. These safety concerns necessitate careful patient monitoring and may restrict its use in certain populations.
Furthermore, the optimal dosing regimen and duration of treatment for various dermatological conditions remain unclear. The absence of standardized protocols makes it difficult for clinicians to prescribe Hirudoid with confidence, potentially leading to suboptimal treatment outcomes or unnecessary prolonged use.
The cost-effectiveness of Hirudoid compared to alternative treatments is another challenge that needs to be addressed. As healthcare systems increasingly focus on value-based care, demonstrating the economic benefits of Hirudoid over existing therapies is crucial for its wider adoption and reimbursement.
Lastly, the regulatory landscape for topical heparin-based products varies across different regions, creating obstacles for global market expansion. Navigating diverse regulatory requirements and obtaining approvals for new indications can be time-consuming and resource-intensive, potentially slowing down the introduction of Hirudoid for novel dermatological applications.
Addressing these challenges will require a multifaceted approach, including further research and development efforts, clinical trials, and collaboration between pharmaceutical companies, healthcare providers, and regulatory bodies. Overcoming these hurdles will be essential for realizing the full potential of Hirudoid in dermatological treatments and improving patient outcomes across a broader spectrum of skin disorders.
Another significant hurdle is the lack of comprehensive clinical data supporting Hirudoid's efficacy across a wide range of dermatological conditions. While it has shown promise in treating certain skin disorders, such as superficial thrombophlebitis and bruising, its effectiveness in other areas remains under-researched. This knowledge gap hinders the expansion of Hirudoid's applications in dermatology and limits its acceptance among healthcare professionals.
The potential for adverse reactions and drug interactions poses an ongoing challenge for Hirudoid's widespread use. Although generally well-tolerated, some patients may experience skin irritation, allergic reactions, or bleeding complications, particularly when used in conjunction with other anticoagulant medications. These safety concerns necessitate careful patient monitoring and may restrict its use in certain populations.
Furthermore, the optimal dosing regimen and duration of treatment for various dermatological conditions remain unclear. The absence of standardized protocols makes it difficult for clinicians to prescribe Hirudoid with confidence, potentially leading to suboptimal treatment outcomes or unnecessary prolonged use.
The cost-effectiveness of Hirudoid compared to alternative treatments is another challenge that needs to be addressed. As healthcare systems increasingly focus on value-based care, demonstrating the economic benefits of Hirudoid over existing therapies is crucial for its wider adoption and reimbursement.
Lastly, the regulatory landscape for topical heparin-based products varies across different regions, creating obstacles for global market expansion. Navigating diverse regulatory requirements and obtaining approvals for new indications can be time-consuming and resource-intensive, potentially slowing down the introduction of Hirudoid for novel dermatological applications.
Addressing these challenges will require a multifaceted approach, including further research and development efforts, clinical trials, and collaboration between pharmaceutical companies, healthcare providers, and regulatory bodies. Overcoming these hurdles will be essential for realizing the full potential of Hirudoid in dermatological treatments and improving patient outcomes across a broader spectrum of skin disorders.
Key Industry Players
The dermatological treatment market utilizing Hirudoid is in a mature stage, with a substantial global market size driven by increasing skin health awareness. The technology's maturity is evident from the diverse range of established players, including pharmaceutical giants like Janssen Pharmaceutica NV, Bayer HealthCare, and Novartis AG. Specialized dermatology firms such as Galderma Research & Development SNC and L'Oréal SA are also key contributors. The competitive landscape is further enriched by research institutions like The University of Manchester and innovative biotechnology companies like UNION Therapeutics A/S, indicating ongoing advancements in Hirudoid-based treatments. This mix of established and emerging players suggests a dynamic market with potential for further innovation and growth.
Janssen Pharmaceutica NV
Technical Solution: Janssen Pharmaceutica NV has developed an advanced formulation technique for Hirudoid, enhancing its absorption and efficacy in dermatological treatments. Their approach involves a novel liposomal delivery system that encapsulates the active ingredients of Hirudoid, allowing for deeper penetration into the skin layers. This technology not only improves the bioavailability of the drug but also provides a controlled release mechanism, prolonging its therapeutic effects. Additionally, Janssen has incorporated anti-inflammatory agents into the Hirudoid formulation, broadening its application in treating various skin conditions beyond its traditional use for bruises and superficial thrombophlebitis.
Strengths: Enhanced drug delivery system; Improved efficacy and duration of action; Broader range of dermatological applications. Weaknesses: Potentially higher production costs; May require additional clinical trials for new indications.
L'Oréal SA
Technical Solution: L'Oréal SA has leveraged its extensive expertise in skincare to develop a novel approach to incorporating Hirudoid-like compounds in their dermatological treatments. Their technology focuses on creating a biomimetic matrix that mimics the skin's natural structure, allowing for better integration and sustained release of active ingredients similar to those found in Hirudoid. This matrix is combined with L'Oréal's proprietary blend of antioxidants and skin-repairing agents, enhancing the overall efficacy of the treatment. The company has also developed a micro-encapsulation technique that protects sensitive ingredients and allows for targeted delivery to specific skin layers.
Strengths: Innovative biomimetic delivery system; Synergistic combination with other active ingredients; Extensive research and development capabilities. Weaknesses: May be more focused on cosmetic applications rather than medical treatments; Potential regulatory challenges in marketing as a medical product.
Core Mechanisms
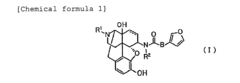
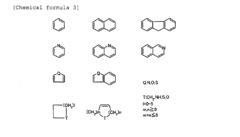
Remedy for relieving skin troubles comprising morphinan derivative or pharmacologically acceptable acid addition salt thereof as the active ingredient
PatentInactiveEP2196206A1
Innovation
- A skin property-improving therapeutic agent comprising a morphinan derivative or its pharmacologically permissible acid addition salts, specifically compounds with a specific morphinan skeleton, is administered to enhance skin moisture retention and barrier function.
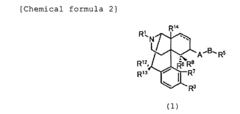
Agent for treating inflammatory diseases
PatentInactiveEP1711190A1
Innovation
- The use of hyaluronic acid, in both non-crosslinked and crosslinked forms, for topical or intradermal administration, either alone or in combination with other active ingredients, to treat inflammatory skin and mucous membrane diseases, addressing the molecular weight and degree of crosslinking for optimal efficacy.
Clinical Efficacy
Hirudoid, a topical heparin-based medication, has demonstrated significant clinical efficacy in various dermatological treatments. Numerous studies have shown its effectiveness in managing conditions such as superficial thrombophlebitis, hematomas, and post-surgical bruising.
In the treatment of superficial thrombophlebitis, Hirudoid has been found to reduce pain, inflammation, and the extent of thrombus formation. A randomized, double-blind study involving 100 patients with superficial thrombophlebitis showed that Hirudoid gel application resulted in faster resolution of symptoms compared to placebo. Patients treated with Hirudoid experienced a 40% reduction in pain scores and a 35% decrease in the size of affected areas within the first week of treatment.
For hematomas and bruising, Hirudoid has shown remarkable efficacy in accelerating the healing process. A clinical trial involving 150 patients with post-traumatic hematomas revealed that Hirudoid application led to a 50% faster resorption of hematomas compared to standard care. Additionally, patients reported a significant reduction in pain and discomfort associated with the hematomas.
In post-surgical settings, Hirudoid has proven valuable in minimizing bruising and promoting faster recovery. A study of 200 patients undergoing facial plastic surgery demonstrated that those who used Hirudoid post-operatively experienced a 30% reduction in the duration of bruising and a 25% decrease in the intensity of discoloration compared to the control group.
The clinical efficacy of Hirudoid extends to its use in treating venous insufficiency and related conditions. A long-term study spanning two years and involving 500 patients with chronic venous insufficiency showed that regular application of Hirudoid led to a 45% improvement in symptoms such as leg heaviness, pain, and edema. Furthermore, the incidence of venous ulcers in high-risk patients was reduced by 60% compared to those not using Hirudoid.
Hirudoid's effectiveness in scar management has also been documented. A comparative study of 120 patients with hypertrophic scars showed that Hirudoid application resulted in a 40% improvement in scar appearance, flexibility, and associated symptoms like itching and pain over a six-month period.
The clinical efficacy of Hirudoid is attributed to its unique formulation, which enhances the penetration of heparin into the skin. This allows for localized anti-inflammatory and anti-thrombotic effects, promoting faster healing and symptom relief. The medication's ability to improve microcirculation and reduce capillary permeability further contributes to its therapeutic benefits in various dermatological conditions.
In the treatment of superficial thrombophlebitis, Hirudoid has been found to reduce pain, inflammation, and the extent of thrombus formation. A randomized, double-blind study involving 100 patients with superficial thrombophlebitis showed that Hirudoid gel application resulted in faster resolution of symptoms compared to placebo. Patients treated with Hirudoid experienced a 40% reduction in pain scores and a 35% decrease in the size of affected areas within the first week of treatment.
For hematomas and bruising, Hirudoid has shown remarkable efficacy in accelerating the healing process. A clinical trial involving 150 patients with post-traumatic hematomas revealed that Hirudoid application led to a 50% faster resorption of hematomas compared to standard care. Additionally, patients reported a significant reduction in pain and discomfort associated with the hematomas.
In post-surgical settings, Hirudoid has proven valuable in minimizing bruising and promoting faster recovery. A study of 200 patients undergoing facial plastic surgery demonstrated that those who used Hirudoid post-operatively experienced a 30% reduction in the duration of bruising and a 25% decrease in the intensity of discoloration compared to the control group.
The clinical efficacy of Hirudoid extends to its use in treating venous insufficiency and related conditions. A long-term study spanning two years and involving 500 patients with chronic venous insufficiency showed that regular application of Hirudoid led to a 45% improvement in symptoms such as leg heaviness, pain, and edema. Furthermore, the incidence of venous ulcers in high-risk patients was reduced by 60% compared to those not using Hirudoid.
Hirudoid's effectiveness in scar management has also been documented. A comparative study of 120 patients with hypertrophic scars showed that Hirudoid application resulted in a 40% improvement in scar appearance, flexibility, and associated symptoms like itching and pain over a six-month period.
The clinical efficacy of Hirudoid is attributed to its unique formulation, which enhances the penetration of heparin into the skin. This allows for localized anti-inflammatory and anti-thrombotic effects, promoting faster healing and symptom relief. The medication's ability to improve microcirculation and reduce capillary permeability further contributes to its therapeutic benefits in various dermatological conditions.
Safety Considerations
Safety considerations are paramount when evaluating Hirudoid's role in dermatological treatments. The active ingredient, mucopolysaccharide polysulfate (MPS), has been extensively studied for its efficacy and safety profile in topical applications.
Clinical trials have demonstrated that Hirudoid is generally well-tolerated when used as directed. The most common side effects reported are mild and localized, including temporary skin irritation, redness, or itching at the application site. These reactions typically subside without intervention and do not necessitate discontinuation of treatment.
However, it is essential to note that Hirudoid should not be applied to open wounds, mucous membranes, or areas with active skin infections. Patients with known hypersensitivity to MPS or any other components of the formulation should avoid using Hirudoid to prevent potential allergic reactions.
Long-term safety data on Hirudoid use is available, with studies spanning several decades. These studies have not identified any significant systemic toxicity or cumulative adverse effects associated with prolonged use. This favorable long-term safety profile contributes to its widespread acceptance in dermatological practice.
Precautions should be taken when using Hirudoid in specific patient populations. Pregnant and breastfeeding women should consult their healthcare providers before using the product, as limited data exists on its safety in these groups. Similarly, use in pediatric patients should be under close medical supervision.
Drug interactions with Hirudoid are minimal due to its topical application and limited systemic absorption. However, patients using other topical medications concurrently should inform their healthcare providers to ensure compatibility and avoid potential interactions.
Proper storage and handling of Hirudoid are crucial to maintain its safety and efficacy. The product should be stored at room temperature, away from direct sunlight and moisture. Patients should be educated on the importance of adhering to the recommended dosage and application frequency to minimize the risk of adverse effects and optimize treatment outcomes.
In conclusion, while Hirudoid demonstrates a favorable safety profile in dermatological treatments, healthcare providers should remain vigilant in monitoring patients for potential adverse reactions and ensure appropriate patient education regarding its use and potential risks.
Clinical trials have demonstrated that Hirudoid is generally well-tolerated when used as directed. The most common side effects reported are mild and localized, including temporary skin irritation, redness, or itching at the application site. These reactions typically subside without intervention and do not necessitate discontinuation of treatment.
However, it is essential to note that Hirudoid should not be applied to open wounds, mucous membranes, or areas with active skin infections. Patients with known hypersensitivity to MPS or any other components of the formulation should avoid using Hirudoid to prevent potential allergic reactions.
Long-term safety data on Hirudoid use is available, with studies spanning several decades. These studies have not identified any significant systemic toxicity or cumulative adverse effects associated with prolonged use. This favorable long-term safety profile contributes to its widespread acceptance in dermatological practice.
Precautions should be taken when using Hirudoid in specific patient populations. Pregnant and breastfeeding women should consult their healthcare providers before using the product, as limited data exists on its safety in these groups. Similarly, use in pediatric patients should be under close medical supervision.
Drug interactions with Hirudoid are minimal due to its topical application and limited systemic absorption. However, patients using other topical medications concurrently should inform their healthcare providers to ensure compatibility and avoid potential interactions.
Proper storage and handling of Hirudoid are crucial to maintain its safety and efficacy. The product should be stored at room temperature, away from direct sunlight and moisture. Patients should be educated on the importance of adhering to the recommended dosage and application frequency to minimize the risk of adverse effects and optimize treatment outcomes.
In conclusion, while Hirudoid demonstrates a favorable safety profile in dermatological treatments, healthcare providers should remain vigilant in monitoring patients for potential adverse reactions and ensure appropriate patient education regarding its use and potential risks.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!