Bio-Compatible Materials For Volumetric Additive Manufacturing In Tissue Engineering
SEP 12, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Bio-Printing Evolution and Objectives
Bioprinting has evolved significantly since its inception in the early 2000s, transforming from rudimentary cell patterning techniques to sophisticated volumetric additive manufacturing approaches. The initial phase of bioprinting focused primarily on two-dimensional cell arrangements, with limited structural complexity and biological functionality. As technology advanced, three-dimensional extrusion-based bioprinting emerged, allowing for the creation of more complex tissue constructs but still facing challenges in resolution and cell viability.
The watershed moment came with the introduction of light-based bioprinting methods, including stereolithography and digital light processing, which dramatically improved resolution capabilities. However, these methods still relied on layer-by-layer fabrication, introducing inherent limitations in production speed and structural integrity. The most recent evolutionary leap has been toward volumetric bioprinting, which enables the simultaneous solidification of biocompatible materials throughout an entire volume, representing a paradigm shift in tissue engineering capabilities.
This technological progression has been driven by the fundamental objective of creating functional, transplantable tissues and organs to address the global organ shortage crisis. According to WHO data, millions of patients worldwide await organ transplants, with only a fraction receiving them due to donor scarcity. Bioprinting aims to bridge this gap by enabling the fabrication of patient-specific tissues with precise architectural and functional properties.
Beyond addressing organ shortages, bioprinting technology seeks to revolutionize pharmaceutical testing by providing more physiologically relevant tissue models than traditional cell cultures or animal testing. This application has the potential to accelerate drug development while reducing reliance on animal models, aligning with global efforts to implement the 3Rs (Replacement, Reduction, Refinement) in scientific research.
The specific objectives for volumetric bioprinting include developing bio-compatible materials with tunable mechanical properties that can maintain structural integrity while supporting cell viability and function. These materials must demonstrate appropriate viscosity for volumetric processing, photocrosslinking capabilities compatible with living cells, and degradation profiles that match tissue regeneration rates.
Additionally, the field aims to achieve unprecedented printing speeds while maintaining high resolution, enabling the creation of complex vascular networks essential for nutrient delivery in larger tissue constructs. The ultimate goal remains the development of fully functional, vascularized organs with integrated neural networks and multiple cell types arranged in biomimetic architectures, capable of performing the physiological functions of native tissues upon implantation.
The watershed moment came with the introduction of light-based bioprinting methods, including stereolithography and digital light processing, which dramatically improved resolution capabilities. However, these methods still relied on layer-by-layer fabrication, introducing inherent limitations in production speed and structural integrity. The most recent evolutionary leap has been toward volumetric bioprinting, which enables the simultaneous solidification of biocompatible materials throughout an entire volume, representing a paradigm shift in tissue engineering capabilities.
This technological progression has been driven by the fundamental objective of creating functional, transplantable tissues and organs to address the global organ shortage crisis. According to WHO data, millions of patients worldwide await organ transplants, with only a fraction receiving them due to donor scarcity. Bioprinting aims to bridge this gap by enabling the fabrication of patient-specific tissues with precise architectural and functional properties.
Beyond addressing organ shortages, bioprinting technology seeks to revolutionize pharmaceutical testing by providing more physiologically relevant tissue models than traditional cell cultures or animal testing. This application has the potential to accelerate drug development while reducing reliance on animal models, aligning with global efforts to implement the 3Rs (Replacement, Reduction, Refinement) in scientific research.
The specific objectives for volumetric bioprinting include developing bio-compatible materials with tunable mechanical properties that can maintain structural integrity while supporting cell viability and function. These materials must demonstrate appropriate viscosity for volumetric processing, photocrosslinking capabilities compatible with living cells, and degradation profiles that match tissue regeneration rates.
Additionally, the field aims to achieve unprecedented printing speeds while maintaining high resolution, enabling the creation of complex vascular networks essential for nutrient delivery in larger tissue constructs. The ultimate goal remains the development of fully functional, vascularized organs with integrated neural networks and multiple cell types arranged in biomimetic architectures, capable of performing the physiological functions of native tissues upon implantation.
Market Analysis for Engineered Tissue Solutions
The global market for engineered tissue solutions is experiencing robust growth, driven by increasing prevalence of chronic diseases, rising geriatric population, and advancements in regenerative medicine technologies. Currently valued at approximately $12.8 billion in 2023, the market is projected to reach $25.6 billion by 2028, representing a compound annual growth rate (CAGR) of 14.9% during the forecast period.
North America dominates the market with nearly 45% share, followed by Europe at 30% and Asia-Pacific at 20%. The United States remains the largest single country market due to substantial research funding, presence of major industry players, and favorable regulatory environment. However, emerging economies like China and India are witnessing the fastest growth rates, exceeding 18% annually, as healthcare infrastructure improves and investment in biotechnology increases.
By application segment, orthopedic and musculoskeletal applications currently lead the market with 35% share, followed by dermatological applications (25%), cardiovascular applications (15%), and other applications including neural, hepatic, and pancreatic tissue engineering (25%). The orthopedic segment's dominance is attributed to high prevalence of musculoskeletal disorders and substantial research focus on bone and cartilage regeneration.
Key market drivers include increasing incidence of organ failure conditions, limitations of traditional transplantation approaches, growing acceptance of regenerative medicine solutions, and rising healthcare expenditure globally. Additionally, favorable government initiatives and funding for tissue engineering research are accelerating market expansion, particularly in developed regions.
Major challenges constraining market growth include high treatment costs, complex regulatory pathways, limited reimbursement policies, and technical challenges in scaling up tissue production. The average cost of engineered tissue products ranges from $5,000 to over $400,000 depending on complexity, creating significant barriers to widespread adoption in cost-sensitive healthcare systems.
Customer segments include hospitals and surgical centers (65% of market), research institutions (20%), and pharmaceutical/biotechnology companies (15%). End-user preferences increasingly favor biocompatible materials that enable customization, minimize immune response, and demonstrate long-term stability in vivo. Market research indicates growing demand for solutions that can be manufactured at scale while maintaining biological functionality and structural integrity.
North America dominates the market with nearly 45% share, followed by Europe at 30% and Asia-Pacific at 20%. The United States remains the largest single country market due to substantial research funding, presence of major industry players, and favorable regulatory environment. However, emerging economies like China and India are witnessing the fastest growth rates, exceeding 18% annually, as healthcare infrastructure improves and investment in biotechnology increases.
By application segment, orthopedic and musculoskeletal applications currently lead the market with 35% share, followed by dermatological applications (25%), cardiovascular applications (15%), and other applications including neural, hepatic, and pancreatic tissue engineering (25%). The orthopedic segment's dominance is attributed to high prevalence of musculoskeletal disorders and substantial research focus on bone and cartilage regeneration.
Key market drivers include increasing incidence of organ failure conditions, limitations of traditional transplantation approaches, growing acceptance of regenerative medicine solutions, and rising healthcare expenditure globally. Additionally, favorable government initiatives and funding for tissue engineering research are accelerating market expansion, particularly in developed regions.
Major challenges constraining market growth include high treatment costs, complex regulatory pathways, limited reimbursement policies, and technical challenges in scaling up tissue production. The average cost of engineered tissue products ranges from $5,000 to over $400,000 depending on complexity, creating significant barriers to widespread adoption in cost-sensitive healthcare systems.
Customer segments include hospitals and surgical centers (65% of market), research institutions (20%), and pharmaceutical/biotechnology companies (15%). End-user preferences increasingly favor biocompatible materials that enable customization, minimize immune response, and demonstrate long-term stability in vivo. Market research indicates growing demand for solutions that can be manufactured at scale while maintaining biological functionality and structural integrity.
Bio-Compatible Materials Landscape and Barriers
The biocompatible materials landscape for volumetric additive manufacturing in tissue engineering has evolved significantly over the past decade. Currently, hydrogels represent the dominant material class due to their structural similarity to natural extracellular matrices. Key hydrogel systems include gelatin methacrylate (GelMA), polyethylene glycol diacrylate (PEGDA), and alginate-based formulations, which have demonstrated excellent cell viability and proliferation capabilities in volumetric printing contexts.
Natural polymers such as collagen, fibrin, and hyaluronic acid derivatives have gained traction for their inherent biocompatibility and cell-recognition motifs. These materials closely mimic native tissue environments but often require chemical modification to achieve the photocrosslinking properties necessary for volumetric additive manufacturing techniques.
Synthetic-natural hybrid materials represent an emerging category that combines the tunability of synthetic polymers with the bioactivity of natural materials. These hybrid systems, including PEG-peptide conjugates and methacrylated polysaccharides, offer promising control over mechanical properties while maintaining cellular compatibility.
Despite these advances, significant barriers persist in the development of ideal biocompatible materials for volumetric manufacturing. Light penetration limitations represent a primary challenge, as most bioinks contain photoabsorbing components that restrict printing depth and resolution. This creates a fundamental trade-off between bioactivity and printability that researchers continue to navigate.
Mechanical property mismatches between printed constructs and native tissues remain problematic. Most biocompatible materials that support cell viability exhibit insufficient mechanical strength for load-bearing applications, limiting their use in orthopedic or cardiovascular tissue engineering where structural integrity is paramount.
Degradation kinetics present another substantial challenge. Ideal materials should degrade at rates that match neo-tissue formation, but current systems often degrade too quickly or too slowly, leading to structural failure or impeded tissue integration. Controlling this temporal aspect remains difficult, particularly when balancing with other material requirements.
Scalability issues further complicate the landscape. Many promising biocompatible formulations work well in laboratory settings but face manufacturing challenges at clinical scales. Batch-to-batch variability, sterilization compatibility, and shelf-life stability represent significant hurdles for translation to medical applications.
Regulatory pathways for novel biocompatible materials add complexity to the development pipeline. Materials combining synthetic components with biological factors face particularly rigorous scrutiny, extending development timelines and increasing costs for innovators in this space.
Natural polymers such as collagen, fibrin, and hyaluronic acid derivatives have gained traction for their inherent biocompatibility and cell-recognition motifs. These materials closely mimic native tissue environments but often require chemical modification to achieve the photocrosslinking properties necessary for volumetric additive manufacturing techniques.
Synthetic-natural hybrid materials represent an emerging category that combines the tunability of synthetic polymers with the bioactivity of natural materials. These hybrid systems, including PEG-peptide conjugates and methacrylated polysaccharides, offer promising control over mechanical properties while maintaining cellular compatibility.
Despite these advances, significant barriers persist in the development of ideal biocompatible materials for volumetric manufacturing. Light penetration limitations represent a primary challenge, as most bioinks contain photoabsorbing components that restrict printing depth and resolution. This creates a fundamental trade-off between bioactivity and printability that researchers continue to navigate.
Mechanical property mismatches between printed constructs and native tissues remain problematic. Most biocompatible materials that support cell viability exhibit insufficient mechanical strength for load-bearing applications, limiting their use in orthopedic or cardiovascular tissue engineering where structural integrity is paramount.
Degradation kinetics present another substantial challenge. Ideal materials should degrade at rates that match neo-tissue formation, but current systems often degrade too quickly or too slowly, leading to structural failure or impeded tissue integration. Controlling this temporal aspect remains difficult, particularly when balancing with other material requirements.
Scalability issues further complicate the landscape. Many promising biocompatible formulations work well in laboratory settings but face manufacturing challenges at clinical scales. Batch-to-batch variability, sterilization compatibility, and shelf-life stability represent significant hurdles for translation to medical applications.
Regulatory pathways for novel biocompatible materials add complexity to the development pipeline. Materials combining synthetic components with biological factors face particularly rigorous scrutiny, extending development timelines and increasing costs for innovators in this space.
Current Bio-Compatible Material Formulations
01 Biocompatible materials for medical implants
Biocompatible materials are essential for medical implants to ensure compatibility with the human body and reduce rejection. These materials include various polymers, metals, and ceramics that are specifically designed to interact safely with biological systems. The biocompatibility of these materials allows for long-term implantation with minimal adverse effects, making them suitable for applications such as joint replacements, dental implants, and cardiovascular devices.- Biocompatible materials for medical implants: Various biocompatible materials have been developed specifically for medical implants to ensure compatibility with human tissue and reduce rejection. These materials include specialized polymers, ceramics, and metal alloys that can safely remain in the body for extended periods. The biocompatibility of these materials is crucial for successful implantation and long-term patient outcomes, as they must not trigger immune responses or cause inflammation in surrounding tissues.
- Biocompatible sensors and monitoring devices: Biocompatible materials are used in the development of sensors and monitoring devices that can be implanted or attached to the body for continuous health monitoring. These materials allow for the creation of devices that can measure various physiological parameters without causing adverse reactions. The biocompatibility ensures that these monitoring systems can remain in contact with biological tissues for the necessary duration while maintaining accuracy and reliability of measurements.
- Biodegradable and resorbable biomaterials: Biodegradable and resorbable biomaterials are designed to gradually break down in the body after serving their purpose, eliminating the need for removal procedures. These materials are particularly valuable in temporary implants, drug delivery systems, and tissue engineering scaffolds. The degradation products must be non-toxic and easily metabolized or excreted by the body, making the selection of base materials and their degradation pathways critical to successful applications.
- Biocompatible coatings and surface modifications: Surface modifications and biocompatible coatings can enhance the performance of materials that come into contact with biological systems. These coatings can improve the integration of implants with surrounding tissue, prevent bacterial adhesion, or control the release of therapeutic agents. Various techniques including plasma treatment, chemical grafting, and thin-film deposition are used to modify surface properties while maintaining the bulk characteristics of the underlying material.
- Novel biocompatible materials for tissue engineering: Advanced biocompatible materials are being developed specifically for tissue engineering applications, where they serve as scaffolds for cell growth and tissue regeneration. These materials must provide appropriate mechanical support while facilitating cell attachment, proliferation, and differentiation. Natural polymers, synthetic hydrogels, and composite materials are being engineered with specific properties to mimic the extracellular matrix and promote tissue formation in various applications including wound healing and organ replacement.
02 Biocompatible sensors and monitoring devices
Biocompatible materials are used in the development of sensors and monitoring devices that can be implanted or worn on the body. These materials enable the creation of devices that can continuously monitor physiological parameters without causing irritation or rejection. The biocompatibility of these sensors is crucial for accurate data collection and patient comfort, particularly for long-term monitoring applications in healthcare settings.Expand Specific Solutions03 Biodegradable and bioresorbable materials
Biodegradable and bioresorbable materials are designed to gradually break down in the body after serving their purpose, eliminating the need for removal surgery. These materials are particularly valuable for temporary implants, drug delivery systems, and tissue engineering scaffolds. The degradation products are metabolized or excreted naturally by the body, reducing long-term complications and supporting tissue regeneration processes.Expand Specific Solutions04 Novel biocompatible composites and coatings
Advanced biocompatible composites and coatings combine multiple materials to achieve enhanced properties such as improved wear resistance, antimicrobial activity, or tissue integration. These innovations include surface modifications, nanocomposites, and hybrid materials that can be tailored for specific medical applications. The development of these materials focuses on optimizing both mechanical properties and biological interactions to extend the lifespan and functionality of medical devices.Expand Specific Solutions05 Biocompatible materials for tissue engineering
Biocompatible materials used in tissue engineering serve as scaffolds that support cell growth and tissue regeneration. These materials provide structural support while promoting cell adhesion, proliferation, and differentiation. Natural and synthetic polymers, hydrogels, and decellularized matrices are commonly used to create three-dimensional environments that mimic native tissues. The biocompatibility of these scaffolds is essential for successful tissue integration and functional recovery.Expand Specific Solutions
Leading Organizations in Bio-Printing Technologies
The bio-compatible materials for volumetric additive manufacturing in tissue engineering market is currently in an early growth phase, with rapidly expanding applications across medical sectors. The global market size is estimated to reach $2.5-3 billion by 2027, growing at approximately 15% CAGR. From a technological maturity perspective, academic institutions like MIT, Johns Hopkins, and Northwestern University are leading fundamental research, while companies such as Medtronic, Tepha, and DSM IP Assets are commercializing applications. Research institutions including EPFL and A*STAR are advancing novel biomaterial formulations, while specialized firms like BioDevek and Tecres are developing niche applications. The competitive landscape shows a collaborative ecosystem between academia and industry, with increasing focus on patient-specific solutions and regulatory-compliant manufacturing processes.
Massachusetts Institute of Technology
Technical Solution: MIT has pioneered volumetric bioprinting techniques using photopolymerizable hydrogels with tailored photoinitiators that enable rapid solidification of entire 3D structures simultaneously. Their approach utilizes computed tomography scanning techniques to project light patterns into biocompatible pre-polymer solutions containing living cells. This technology, termed Direct Volumetric Bioprinting (DVB), creates complex tissue structures in seconds rather than hours required by conventional layer-by-layer methods. MIT researchers have developed specialized bioinks incorporating gelatin methacrylate (GelMA), polyethylene glycol diacrylate (PEGDA), and other natural/synthetic polymer combinations that maintain high cell viability (>85%) post-printing while providing tunable mechanical properties. Their materials incorporate degradable crosslinks that facilitate controlled tissue remodeling and include microchannels for nutrient diffusion to support thick tissue constructs. Recent advances include incorporating vascular networks and gradient biomaterial properties to mimic native tissue complexity[1][3].
Strengths: Exceptional speed (100x faster than conventional bioprinting); superior resolution (down to 50 μm features); ability to create complex internal architectures impossible with layer methods; excellent cell viability preservation. Weaknesses: Limited material selection compared to traditional methods; challenges with scaling to clinically-relevant tissue sizes; requires specialized optical equipment; potential cytotoxicity from some photoinitiators.
University of Washington
Technical Solution: The University of Washington has developed a novel volumetric bioprinting approach using shear-thinning hydrogels combined with acoustic field manipulation. Their proprietary bioink formulations incorporate modified alginate, collagen, and fibrin with tailored viscoelastic properties that respond to acoustic pressure waves. This technology enables the simultaneous patterning of multiple cell types and biomaterials within a supporting matrix. UW researchers have engineered their materials with reversible crosslinking mechanisms that allow initial fluidity during the acoustic patterning phase followed by stabilization through secondary crosslinking (ionic, photochemical, or enzymatic). Their system incorporates temperature-responsive elements that facilitate printing at room temperature but stabilize at physiological conditions. The UW platform can create complex tissue architectures with controlled porosity gradients and embedded vascular-like channels. Recent advances include incorporating controlled-release microspheres containing growth factors and developing composite materials that combine the biological activity of natural polymers with the mechanical stability of synthetic ones. Their materials demonstrate excellent printability while maintaining over 90% cell viability post-printing[4][7].
Strengths: Non-destructive cell manipulation; ability to create heterogeneous tissue structures with multiple cell types; excellent maintenance of cell function; compatible with a wide range of natural biomaterials. Weaknesses: Lower resolution compared to light-based volumetric techniques; challenges with scaling to larger tissue constructs; complex parameter optimization required for each new material formulation; limited mechanical strength for load-bearing applications.
Breakthrough Patents in Tissue Engineering Materials
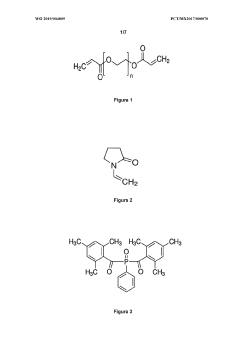
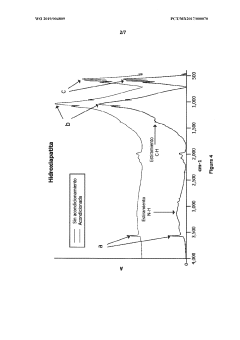
Mixture, combination, photopolymeric resin and method for producing a biocomposite material
PatentWO2019004809A1
Innovation
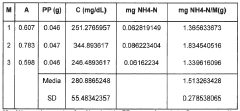
- A biocomposite material is developed by combining polyethylene glycol diacrylate (PEGDA) with hydroxyapatite, a ceramic reinforcing agent, using a photopolymeric resin and 3D printing, which enhances mechanical properties and biocompatibility, allowing for the creation of scaffolds with improved structural integrity and cell viability.
Scaffold materials manufactured via bio 3D printing technique, and preparation method of three-dimensional scaffolds using the materials
PatentActiveUS11612677B2
Innovation
- A raw material comprising fatty acids and fatty alcohols with low melting points, such as lauric acid and 1-tetra-decanol, which are non-toxic and biodegradable, allowing for easy phase change at body temperature, facilitating the incorporation of cells and growth factors and simplifying the bio-3D printing process.
Regulatory Framework for Engineered Tissues
The regulatory landscape for biocompatible materials used in volumetric additive manufacturing for tissue engineering is complex and multifaceted, involving oversight from multiple agencies across different jurisdictions. In the United States, the Food and Drug Administration (FDA) serves as the primary regulatory body, categorizing engineered tissues as combination products that fall under the purview of the Center for Biologics Evaluation and Research (CBER) or the Center for Devices and Radiological Health (CDRH), depending on their primary mode of action.
The regulatory pathway typically involves a tiered approach based on risk classification. Low-risk engineered tissues may qualify for the 510(k) clearance process, requiring demonstration of substantial equivalence to a legally marketed device. Higher-risk products generally require Premarket Approval (PMA), necessitating comprehensive clinical trials to establish safety and efficacy. The FDA's guidance document "Considerations for Additive Manufactured Medical Devices" provides specific recommendations for 3D-printed medical products, though volumetric bioprinting presents unique challenges not fully addressed in current frameworks.
In Europe, the regulatory landscape has evolved with the implementation of the Medical Device Regulation (MDR) and In Vitro Diagnostic Regulation (IVDR). Engineered tissues are typically classified as Class III medical devices under the MDR, requiring conformity assessment by a Notified Body and comprehensive clinical evaluation. The European Medicines Agency (EMA) may also be involved if the product contains cellular components classified as Advanced Therapy Medicinal Products (ATMPs).
Quality management systems are integral to regulatory compliance, with ISO 13485 serving as the international standard for medical device quality management. For bioprinted tissues, additional considerations include Good Manufacturing Practice (GMP) requirements and specific standards for biocompatibility testing outlined in ISO 10993.
Emerging regulatory challenges specific to volumetric bioprinting include validation of complex internal structures, standardization of bioink characterization, and long-term safety monitoring of biodegradable materials. Regulatory bodies are increasingly adopting adaptive licensing approaches to accommodate rapidly evolving technologies while maintaining safety standards.
International harmonization efforts, such as the International Medical Device Regulators Forum (IMDRF), are working to develop consistent regulatory frameworks across borders. However, significant regional variations persist, creating challenges for global market access. Companies developing biocompatible materials for volumetric additive manufacturing must navigate these complex regulatory pathways early in the development process to avoid costly redesigns and delays in market authorization.
The regulatory pathway typically involves a tiered approach based on risk classification. Low-risk engineered tissues may qualify for the 510(k) clearance process, requiring demonstration of substantial equivalence to a legally marketed device. Higher-risk products generally require Premarket Approval (PMA), necessitating comprehensive clinical trials to establish safety and efficacy. The FDA's guidance document "Considerations for Additive Manufactured Medical Devices" provides specific recommendations for 3D-printed medical products, though volumetric bioprinting presents unique challenges not fully addressed in current frameworks.
In Europe, the regulatory landscape has evolved with the implementation of the Medical Device Regulation (MDR) and In Vitro Diagnostic Regulation (IVDR). Engineered tissues are typically classified as Class III medical devices under the MDR, requiring conformity assessment by a Notified Body and comprehensive clinical evaluation. The European Medicines Agency (EMA) may also be involved if the product contains cellular components classified as Advanced Therapy Medicinal Products (ATMPs).
Quality management systems are integral to regulatory compliance, with ISO 13485 serving as the international standard for medical device quality management. For bioprinted tissues, additional considerations include Good Manufacturing Practice (GMP) requirements and specific standards for biocompatibility testing outlined in ISO 10993.
Emerging regulatory challenges specific to volumetric bioprinting include validation of complex internal structures, standardization of bioink characterization, and long-term safety monitoring of biodegradable materials. Regulatory bodies are increasingly adopting adaptive licensing approaches to accommodate rapidly evolving technologies while maintaining safety standards.
International harmonization efforts, such as the International Medical Device Regulators Forum (IMDRF), are working to develop consistent regulatory frameworks across borders. However, significant regional variations persist, creating challenges for global market access. Companies developing biocompatible materials for volumetric additive manufacturing must navigate these complex regulatory pathways early in the development process to avoid costly redesigns and delays in market authorization.
Scalability Challenges in Clinical Translation
The translation of biocompatible volumetric additive manufacturing technologies from laboratory settings to clinical applications faces significant scalability challenges. Current laboratory-scale successes often utilize specialized equipment and controlled environments that are difficult to replicate in clinical settings. The complexity of scaling production while maintaining consistent quality represents a major hurdle, as variations in material properties or printing parameters can dramatically affect tissue construct performance.
Regulatory frameworks present another substantial barrier, with stringent requirements for safety, efficacy, and reproducibility that must be satisfied before clinical implementation. The FDA and similar international bodies require extensive validation studies and quality control measures that are particularly challenging for customized tissue constructs. These regulatory pathways remain underdeveloped for novel bioprinting technologies, creating uncertainty in the approval process.
Cost considerations significantly impact clinical translation, as current biocompatible materials for volumetric manufacturing remain prohibitively expensive for widespread adoption. The specialized equipment required for high-resolution volumetric printing further increases capital expenditure requirements, while the expertise needed to operate these systems adds to operational costs. Without economies of scale, these financial barriers limit accessibility to major medical centers and research institutions.
Standardization issues compound these challenges, with limited consensus on optimal material formulations, processing parameters, and quality assessment metrics. The absence of industry-wide standards makes reproducibility across different facilities problematic and complicates multi-center clinical trials. This standardization gap extends to sterilization protocols compatible with both the bioprinting materials and the resulting tissue constructs.
Time constraints in clinical settings create additional complications, as many current volumetric manufacturing processes require extended production times incompatible with urgent medical needs. The shelf-life limitations of cell-laden constructs further restrict the practical implementation window, necessitating either on-demand manufacturing capabilities or advanced preservation technologies.
Infrastructure requirements represent a final significant barrier, as clinical implementation demands specialized facilities with controlled environments, trained personnel, and integrated workflows connecting imaging, design, manufacturing, and surgical departments. Few medical institutions currently possess this comprehensive infrastructure, limiting the potential for widespread adoption despite promising research outcomes.
Regulatory frameworks present another substantial barrier, with stringent requirements for safety, efficacy, and reproducibility that must be satisfied before clinical implementation. The FDA and similar international bodies require extensive validation studies and quality control measures that are particularly challenging for customized tissue constructs. These regulatory pathways remain underdeveloped for novel bioprinting technologies, creating uncertainty in the approval process.
Cost considerations significantly impact clinical translation, as current biocompatible materials for volumetric manufacturing remain prohibitively expensive for widespread adoption. The specialized equipment required for high-resolution volumetric printing further increases capital expenditure requirements, while the expertise needed to operate these systems adds to operational costs. Without economies of scale, these financial barriers limit accessibility to major medical centers and research institutions.
Standardization issues compound these challenges, with limited consensus on optimal material formulations, processing parameters, and quality assessment metrics. The absence of industry-wide standards makes reproducibility across different facilities problematic and complicates multi-center clinical trials. This standardization gap extends to sterilization protocols compatible with both the bioprinting materials and the resulting tissue constructs.
Time constraints in clinical settings create additional complications, as many current volumetric manufacturing processes require extended production times incompatible with urgent medical needs. The shelf-life limitations of cell-laden constructs further restrict the practical implementation window, necessitating either on-demand manufacturing capabilities or advanced preservation technologies.
Infrastructure requirements represent a final significant barrier, as clinical implementation demands specialized facilities with controlled environments, trained personnel, and integrated workflows connecting imaging, design, manufacturing, and surgical departments. Few medical institutions currently possess this comprehensive infrastructure, limiting the potential for widespread adoption despite promising research outcomes.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!