The impact of hyperkalemia on T wave inversion morphology
AUG 19, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Hyperkalemia and T Wave Inversion Background
Hyperkalemia, a condition characterized by elevated levels of potassium in the blood, has significant implications for cardiac electrophysiology and, consequently, the morphology of the T wave on electrocardiograms (ECGs). The T wave, representing ventricular repolarization, is particularly sensitive to changes in extracellular potassium concentration. Understanding the relationship between hyperkalemia and T wave inversion is crucial for accurate diagnosis and management of this potentially life-threatening electrolyte imbalance.
Historically, the association between serum potassium levels and ECG changes has been recognized since the early 20th century. However, it was not until the 1950s and 1960s that researchers began to systematically study the specific effects of hyperkalemia on T wave morphology. These investigations laid the groundwork for our current understanding of how elevated potassium levels alter the electrical activity of the heart.
The normal T wave is typically upright in most ECG leads, reflecting the orderly repolarization of ventricular myocytes. As serum potassium levels rise, the T wave undergoes a series of characteristic changes. Initially, the T wave becomes tall and peaked, often described as "tented." This change is due to the accelerated repolarization of ventricular cells in the presence of high extracellular potassium. As hyperkalemia progresses, the T wave may broaden at its base and eventually invert in some or all ECG leads.
T wave inversion in hyperkalemia is a complex phenomenon influenced by multiple factors. The primary mechanism involves alterations in the transmembrane potassium gradient, which affects the resting membrane potential and the duration of the action potential. Additionally, hyperkalemia can lead to changes in sodium channel function and calcium homeostasis, further contributing to abnormal repolarization patterns.
The severity and distribution of T wave inversions can vary depending on the degree of hyperkalemia and individual patient factors. Mild to moderate hyperkalemia may cause subtle T wave changes, while severe hyperkalemia can result in dramatic T wave inversions across multiple leads. These inversions are often accompanied by other ECG abnormalities, such as PR interval prolongation and QRS widening, which collectively form the classic hyperkalemic ECG pattern.
It is important to note that T wave inversion is not specific to hyperkalemia and can occur in various other cardiac and non-cardiac conditions. Therefore, the interpretation of T wave changes must always be considered in the context of the patient's clinical presentation, laboratory findings, and other ECG features. This complexity underscores the need for a comprehensive approach to ECG analysis in suspected cases of hyperkalemia.
Historically, the association between serum potassium levels and ECG changes has been recognized since the early 20th century. However, it was not until the 1950s and 1960s that researchers began to systematically study the specific effects of hyperkalemia on T wave morphology. These investigations laid the groundwork for our current understanding of how elevated potassium levels alter the electrical activity of the heart.
The normal T wave is typically upright in most ECG leads, reflecting the orderly repolarization of ventricular myocytes. As serum potassium levels rise, the T wave undergoes a series of characteristic changes. Initially, the T wave becomes tall and peaked, often described as "tented." This change is due to the accelerated repolarization of ventricular cells in the presence of high extracellular potassium. As hyperkalemia progresses, the T wave may broaden at its base and eventually invert in some or all ECG leads.
T wave inversion in hyperkalemia is a complex phenomenon influenced by multiple factors. The primary mechanism involves alterations in the transmembrane potassium gradient, which affects the resting membrane potential and the duration of the action potential. Additionally, hyperkalemia can lead to changes in sodium channel function and calcium homeostasis, further contributing to abnormal repolarization patterns.
The severity and distribution of T wave inversions can vary depending on the degree of hyperkalemia and individual patient factors. Mild to moderate hyperkalemia may cause subtle T wave changes, while severe hyperkalemia can result in dramatic T wave inversions across multiple leads. These inversions are often accompanied by other ECG abnormalities, such as PR interval prolongation and QRS widening, which collectively form the classic hyperkalemic ECG pattern.
It is important to note that T wave inversion is not specific to hyperkalemia and can occur in various other cardiac and non-cardiac conditions. Therefore, the interpretation of T wave changes must always be considered in the context of the patient's clinical presentation, laboratory findings, and other ECG features. This complexity underscores the need for a comprehensive approach to ECG analysis in suspected cases of hyperkalemia.
Clinical Significance and Diagnostic Demand
Hyperkalemia, a condition characterized by elevated potassium levels in the blood, has significant clinical implications, particularly in its impact on cardiac function and electrocardiogram (ECG) readings. The relationship between hyperkalemia and T wave inversion morphology is of paramount importance in both diagnostic and treatment contexts, driving a substantial demand for accurate and timely detection methods.
The clinical significance of hyperkalemia-induced T wave inversion lies in its potential to indicate severe cardiac disturbances. As potassium levels rise, the repolarization phase of cardiac action potentials is altered, leading to characteristic changes in T wave morphology. These changes can progress from peaked T waves to flattened and eventually inverted T waves as hyperkalemia worsens. The ability to recognize and interpret these ECG changes is crucial for healthcare providers, as they may precede life-threatening arrhythmias or cardiac arrest.
In emergency settings, rapid identification of hyperkalemia through ECG interpretation can be lifesaving. The distinctive T wave inversions associated with hyperkalemia serve as early warning signs, allowing for prompt intervention before more severe cardiac complications arise. This underscores the importance of ECG as a quick and non-invasive tool for initial assessment of potassium imbalances.
The diagnostic demand for accurate detection of hyperkalemia-induced T wave inversions stems from several factors. Firstly, hyperkalemia is a common electrolyte disorder, particularly in patients with kidney disease, heart failure, or those taking certain medications. The prevalence of these conditions in an aging population further amplifies the need for reliable diagnostic tools. Secondly, the consequences of missed or delayed diagnosis of hyperkalemia can be severe, including fatal arrhythmias.
Healthcare systems are increasingly recognizing the value of early detection and management of hyperkalemia. This has led to a growing demand for advanced ECG interpretation technologies and training programs for healthcare professionals. The ability to quickly and accurately identify T wave inversions associated with hyperkalemia can significantly improve patient outcomes and reduce healthcare costs associated with complications of undiagnosed or untreated hyperkalemia.
Moreover, the integration of artificial intelligence and machine learning algorithms in ECG analysis has opened new avenues for enhancing the detection of hyperkalemia-induced T wave inversions. These technologies offer the potential for more sensitive and specific identification of ECG changes, even in subtle cases that might be challenging for human interpreters. The development and implementation of such advanced diagnostic tools represent a significant area of research and investment in the medical technology sector.
The clinical significance of hyperkalemia-induced T wave inversion lies in its potential to indicate severe cardiac disturbances. As potassium levels rise, the repolarization phase of cardiac action potentials is altered, leading to characteristic changes in T wave morphology. These changes can progress from peaked T waves to flattened and eventually inverted T waves as hyperkalemia worsens. The ability to recognize and interpret these ECG changes is crucial for healthcare providers, as they may precede life-threatening arrhythmias or cardiac arrest.
In emergency settings, rapid identification of hyperkalemia through ECG interpretation can be lifesaving. The distinctive T wave inversions associated with hyperkalemia serve as early warning signs, allowing for prompt intervention before more severe cardiac complications arise. This underscores the importance of ECG as a quick and non-invasive tool for initial assessment of potassium imbalances.
The diagnostic demand for accurate detection of hyperkalemia-induced T wave inversions stems from several factors. Firstly, hyperkalemia is a common electrolyte disorder, particularly in patients with kidney disease, heart failure, or those taking certain medications. The prevalence of these conditions in an aging population further amplifies the need for reliable diagnostic tools. Secondly, the consequences of missed or delayed diagnosis of hyperkalemia can be severe, including fatal arrhythmias.
Healthcare systems are increasingly recognizing the value of early detection and management of hyperkalemia. This has led to a growing demand for advanced ECG interpretation technologies and training programs for healthcare professionals. The ability to quickly and accurately identify T wave inversions associated with hyperkalemia can significantly improve patient outcomes and reduce healthcare costs associated with complications of undiagnosed or untreated hyperkalemia.
Moreover, the integration of artificial intelligence and machine learning algorithms in ECG analysis has opened new avenues for enhancing the detection of hyperkalemia-induced T wave inversions. These technologies offer the potential for more sensitive and specific identification of ECG changes, even in subtle cases that might be challenging for human interpreters. The development and implementation of such advanced diagnostic tools represent a significant area of research and investment in the medical technology sector.
Current Challenges in ECG Interpretation
Electrocardiogram (ECG) interpretation remains a critical skill in clinical practice, yet it faces several significant challenges in the current healthcare landscape. One of the primary difficulties is the increasing complexity of ECG patterns due to the growing prevalence of comorbidities and polypharmacy in an aging population. This complexity often leads to subtle and atypical ECG changes that can be easily misinterpreted or overlooked.
The rapid advancement of technology has introduced automated ECG interpretation systems, which, while helpful, have created a new set of challenges. Overreliance on these systems can lead to deskilling of healthcare professionals and potential misdiagnosis when the automated interpretation fails to capture nuanced abnormalities. Moreover, the integration of these systems into clinical workflows has been inconsistent, leading to variability in interpretation quality across different healthcare settings.
Another significant challenge is the lack of standardization in ECG interpretation across different medical specialties and geographic regions. This inconsistency can result in conflicting diagnoses and treatment plans, particularly in cases of subtle ECG changes or rare conditions. The absence of a universally accepted, comprehensive training program for ECG interpretation further exacerbates this issue.
The impact of hyperkalemia on T wave inversion morphology exemplifies the intricate nature of ECG interpretation challenges. Hyperkalemia can cause various ECG changes, including T wave inversions, which can mimic other cardiac conditions such as ischemia or structural heart disease. Distinguishing between hyperkalemia-induced T wave inversions and those caused by other pathologies requires a nuanced understanding of electrolyte imbalances and their electrocardiographic manifestations.
Furthermore, the dynamic nature of ECG changes in response to acute conditions poses a significant challenge. Interpreting serial ECGs and understanding the temporal evolution of T wave inversions in the context of changing potassium levels demands a high level of expertise and clinical correlation. This complexity is compounded by the fact that the degree of hyperkalemia does not always correlate linearly with the severity of ECG changes, making interpretation even more challenging.
The increasing use of wearable ECG devices and remote monitoring systems has introduced new challenges in ECG interpretation. These devices generate vast amounts of data, often of variable quality, which can be overwhelming for clinicians to interpret accurately and efficiently. Additionally, the context in which these ECGs are recorded (e.g., during exercise or stress) may not always be clear, further complicating interpretation.
In conclusion, while ECG remains an invaluable diagnostic tool, the current challenges in its interpretation underscore the need for ongoing education, standardization of practices, and the development of more sophisticated interpretation aids that can account for complex clinical scenarios such as hyperkalemia-induced T wave inversions.
The rapid advancement of technology has introduced automated ECG interpretation systems, which, while helpful, have created a new set of challenges. Overreliance on these systems can lead to deskilling of healthcare professionals and potential misdiagnosis when the automated interpretation fails to capture nuanced abnormalities. Moreover, the integration of these systems into clinical workflows has been inconsistent, leading to variability in interpretation quality across different healthcare settings.
Another significant challenge is the lack of standardization in ECG interpretation across different medical specialties and geographic regions. This inconsistency can result in conflicting diagnoses and treatment plans, particularly in cases of subtle ECG changes or rare conditions. The absence of a universally accepted, comprehensive training program for ECG interpretation further exacerbates this issue.
The impact of hyperkalemia on T wave inversion morphology exemplifies the intricate nature of ECG interpretation challenges. Hyperkalemia can cause various ECG changes, including T wave inversions, which can mimic other cardiac conditions such as ischemia or structural heart disease. Distinguishing between hyperkalemia-induced T wave inversions and those caused by other pathologies requires a nuanced understanding of electrolyte imbalances and their electrocardiographic manifestations.
Furthermore, the dynamic nature of ECG changes in response to acute conditions poses a significant challenge. Interpreting serial ECGs and understanding the temporal evolution of T wave inversions in the context of changing potassium levels demands a high level of expertise and clinical correlation. This complexity is compounded by the fact that the degree of hyperkalemia does not always correlate linearly with the severity of ECG changes, making interpretation even more challenging.
The increasing use of wearable ECG devices and remote monitoring systems has introduced new challenges in ECG interpretation. These devices generate vast amounts of data, often of variable quality, which can be overwhelming for clinicians to interpret accurately and efficiently. Additionally, the context in which these ECGs are recorded (e.g., during exercise or stress) may not always be clear, further complicating interpretation.
In conclusion, while ECG remains an invaluable diagnostic tool, the current challenges in its interpretation underscore the need for ongoing education, standardization of practices, and the development of more sophisticated interpretation aids that can account for complex clinical scenarios such as hyperkalemia-induced T wave inversions.
Existing Methods for T Wave Analysis
01 T wave inversion detection and analysis
Methods and systems for detecting and analyzing T wave inversion in electrocardiogram (ECG) signals. This includes algorithms for identifying inverted T waves, measuring their amplitude and duration, and assessing their morphology. The analysis can help in diagnosing various cardiac conditions associated with T wave inversion.- T wave inversion detection methods: Various methods and systems are developed to detect and analyze T wave inversion in electrocardiogram (ECG) signals. These methods often involve signal processing techniques, machine learning algorithms, and pattern recognition to identify abnormal T wave morphologies. The detection of T wave inversion is crucial for diagnosing various cardiac conditions and assessing heart health.
- Characterization of T wave inversion morphology: Research focuses on characterizing different types of T wave inversion morphologies, including symmetric, asymmetric, biphasic, and global inversions. Advanced algorithms and imaging techniques are employed to analyze the shape, duration, and amplitude of inverted T waves. This detailed characterization aids in differentiating between benign and pathological T wave inversions.
- Clinical significance of T wave inversion patterns: Studies investigate the clinical implications of various T wave inversion patterns in different lead locations. The research explores correlations between specific T wave inversion morphologies and underlying cardiac pathologies, such as ischemia, cardiomyopathies, and electrolyte imbalances. This knowledge aids in improving diagnostic accuracy and risk stratification in patients with abnormal ECG findings.
- T wave inversion in specific patient populations: Research examines T wave inversion morphologies in specific patient groups, such as athletes, pediatric patients, and individuals with genetic cardiac disorders. These studies aim to distinguish between physiological and pathological T wave inversions in these populations, helping to prevent misdiagnosis and unnecessary interventions.
- Integration of T wave inversion analysis in ECG devices: Advancements in ECG devices and software incorporate sophisticated T wave inversion analysis capabilities. These innovations include real-time detection, automated classification of inversion morphologies, and integration with other ECG parameters for comprehensive cardiac assessment. Such integrations aim to enhance the diagnostic capabilities of ECG devices in both clinical and remote monitoring settings.
02 Machine learning for T wave morphology classification
Application of machine learning techniques to classify and interpret T wave morphologies, including inversions. These approaches can improve the accuracy of T wave inversion detection and provide more detailed characterization of the inversion patterns, potentially aiding in the diagnosis of specific cardiac conditions.Expand Specific Solutions03 T wave inversion in relation to other ECG features
Studies and methods focusing on the relationship between T wave inversion and other ECG features such as ST segment changes, QT interval, and R wave amplitude. This holistic approach can provide a more comprehensive understanding of the cardiac electrical activity and improve diagnostic accuracy.Expand Specific Solutions04 Dynamic T wave inversion analysis
Techniques for analyzing T wave inversion changes over time, including during exercise stress tests or continuous monitoring. This dynamic analysis can reveal transient T wave inversions and their potential clinical significance, which may not be apparent in static ECG recordings.Expand Specific Solutions05 T wave inversion localization and mapping
Methods for localizing the origin of T wave inversions in the heart and creating spatial maps of T wave inversion patterns. This can involve advanced ECG lead systems or integration with imaging techniques to provide more precise information about the anatomical location of the electrical abnormalities causing T wave inversion.Expand Specific Solutions
Key Players in ECG Technology
The impact of hyperkalemia on T wave inversion morphology is a complex technical issue in the field of cardiology, currently in a mature research phase. The market for related diagnostic and treatment solutions is substantial, driven by the prevalence of cardiovascular diseases. Companies like Merck & Co., Pacesetter (Abbott), and DexCom are at the forefront of developing technologies to address this challenge. Academic institutions such as Massachusetts Institute of Technology and Yale University contribute significantly to the research. The technology's maturity is evident in the advanced diagnostic tools and treatments available, with ongoing research focusing on improving accuracy and patient outcomes.
Thomas Jefferson University
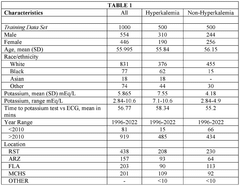
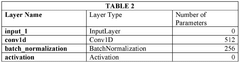
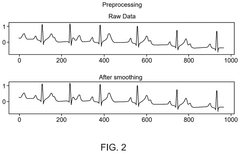
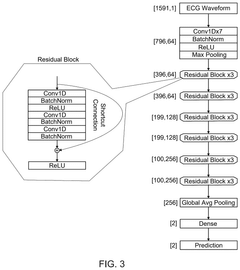
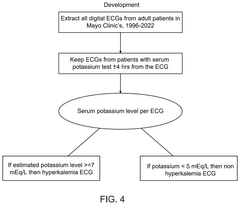
Technical Solution: Thomas Jefferson University has developed a comprehensive approach to studying the impact of hyperkalemia on T wave inversion morphology. Their research utilizes advanced electrocardiogram (ECG) analysis techniques, including high-resolution digital ECG recordings and sophisticated signal processing algorithms. The university's team has created a proprietary software that can detect subtle changes in T wave morphology associated with varying levels of serum potassium. This technology allows for early detection of hyperkalemia, potentially before clinical symptoms manifest. Their method incorporates machine learning algorithms trained on large datasets of ECGs from patients with confirmed hyperkalemia, enabling more accurate interpretation of T wave changes[1][3]. Additionally, they have conducted clinical studies correlating the degree of T wave inversion with serum potassium levels, establishing a quantitative relationship between the two parameters[5].
Strengths: Advanced ECG analysis techniques, early detection capability, and machine learning integration. Weaknesses: May require specialized equipment and training for widespread implementation.
Massachusetts Institute of Technology
Technical Solution: MIT has pioneered a novel approach to analyzing the impact of hyperkalemia on T wave inversion morphology using artificial intelligence and wearable technology. Their system combines data from wearable ECG devices with a sophisticated AI algorithm that can detect minute changes in T wave morphology indicative of hyperkalemia. The AI model has been trained on a vast database of ECGs from patients with various levels of serum potassium, allowing it to recognize patterns that may be imperceptible to the human eye. MIT's technology also incorporates real-time analysis, enabling continuous monitoring of patients at risk for hyperkalemia. The system can alert healthcare providers to potential hyperkalemia before traditional blood tests would typically be performed, potentially reducing the risk of serious cardiac events[2][4]. Furthermore, MIT researchers have developed a method to quantify the degree of T wave inversion, providing a more objective measure of the severity of hyperkalemia[6].
Strengths: AI-powered analysis, real-time monitoring capability, and integration with wearable technology. Weaknesses: May face challenges in regulatory approval and widespread adoption due to its innovative nature.
Innovations in Hyperkalemia Detection
Systems and processes for hyperkalemia detection using lead i ECG data
PatentWO2025096518A1
Innovation
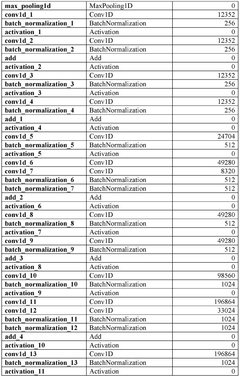
- The system employs Lead I ECG data to detect hyperkalemia through segmentation, normalization, and machine learning-based classification, allowing for the identification of hyperkalemia without the need for blood potassium measurements.
Systems and processes for hyperkalemia detection using lead i ECG data
PatentPendingUS20250134441A1
Innovation
- The system employs Lead I ECG signals to detect hyperkalemia by segmenting and normalizing the ECG data. This involves breaking down the ECG signal into smaller segments, applying a consistent time-frame and amplitude scale, and using a machine learning model to identify patterns indicative of hyperkalemia.
Regulatory Aspects of ECG Diagnostics
The regulatory landscape for ECG diagnostics is complex and multifaceted, with various governing bodies and standards influencing the development, approval, and implementation of ECG-related technologies. In the context of hyperkalemia's impact on T wave inversion morphology, regulatory considerations play a crucial role in ensuring the accuracy, reliability, and safety of diagnostic tools and interpretations.
The U.S. Food and Drug Administration (FDA) is a key regulatory agency overseeing ECG devices and software. Under the FDA's medical device classification system, ECG-related products are typically categorized as Class II devices, requiring premarket notification (510(k)) clearance. This process involves demonstrating substantial equivalence to a legally marketed predicate device, ensuring that new technologies meet established safety and effectiveness standards.
International standards, such as IEC 60601-2-25 for electrocardiographs and IEC 60601-2-47 for ambulatory ECG systems, provide guidelines for the safety and performance of ECG equipment. These standards are often adopted or referenced by regulatory bodies worldwide, promoting consistency in device quality and performance across different jurisdictions.
The European Union's Medical Device Regulation (MDR) imposes stringent requirements on ECG devices and related software. Manufacturers must comply with essential safety and performance requirements, conduct clinical evaluations, and implement post-market surveillance systems. The CE marking process ensures that products meet all applicable EU health, safety, and environmental protection standards.
Regulatory bodies also focus on the validation of algorithms used in ECG interpretation, particularly those involving machine learning and artificial intelligence. The FDA has issued guidance on the clinical performance assessment of software as a medical device (SaMD), which is relevant to ECG analysis software that may be used to detect T wave inversions associated with hyperkalemia.
Data privacy and security regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States and the General Data Protection Regulation (GDPR) in the European Union, have significant implications for ECG diagnostics. These regulations govern the collection, storage, and transmission of patient ECG data, requiring robust data protection measures and patient consent protocols.
Regulatory agencies are increasingly emphasizing the importance of real-world evidence in the evaluation of medical devices and diagnostics. This approach allows for the continuous assessment of ECG diagnostic tools' performance in clinical practice, potentially leading to refinements in the detection and interpretation of hyperkalemia-induced T wave inversions.
The U.S. Food and Drug Administration (FDA) is a key regulatory agency overseeing ECG devices and software. Under the FDA's medical device classification system, ECG-related products are typically categorized as Class II devices, requiring premarket notification (510(k)) clearance. This process involves demonstrating substantial equivalence to a legally marketed predicate device, ensuring that new technologies meet established safety and effectiveness standards.
International standards, such as IEC 60601-2-25 for electrocardiographs and IEC 60601-2-47 for ambulatory ECG systems, provide guidelines for the safety and performance of ECG equipment. These standards are often adopted or referenced by regulatory bodies worldwide, promoting consistency in device quality and performance across different jurisdictions.
The European Union's Medical Device Regulation (MDR) imposes stringent requirements on ECG devices and related software. Manufacturers must comply with essential safety and performance requirements, conduct clinical evaluations, and implement post-market surveillance systems. The CE marking process ensures that products meet all applicable EU health, safety, and environmental protection standards.
Regulatory bodies also focus on the validation of algorithms used in ECG interpretation, particularly those involving machine learning and artificial intelligence. The FDA has issued guidance on the clinical performance assessment of software as a medical device (SaMD), which is relevant to ECG analysis software that may be used to detect T wave inversions associated with hyperkalemia.
Data privacy and security regulations, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States and the General Data Protection Regulation (GDPR) in the European Union, have significant implications for ECG diagnostics. These regulations govern the collection, storage, and transmission of patient ECG data, requiring robust data protection measures and patient consent protocols.
Regulatory agencies are increasingly emphasizing the importance of real-world evidence in the evaluation of medical devices and diagnostics. This approach allows for the continuous assessment of ECG diagnostic tools' performance in clinical practice, potentially leading to refinements in the detection and interpretation of hyperkalemia-induced T wave inversions.
AI Integration in ECG Interpretation
The integration of artificial intelligence (AI) in ECG interpretation represents a significant advancement in cardiac diagnostics, particularly in the context of hyperkalemia-induced T wave inversion morphology. Machine learning algorithms have demonstrated remarkable capabilities in analyzing complex ECG patterns, offering potential improvements in accuracy and efficiency of diagnosis.
Recent studies have shown that AI models can effectively detect subtle changes in T wave morphology associated with hyperkalemia. These models are trained on large datasets of ECG recordings, allowing them to recognize patterns that may be challenging for human interpreters to consistently identify. The ability of AI to process vast amounts of data quickly and objectively makes it a valuable tool in emergency settings where rapid diagnosis of hyperkalemia is crucial.
One of the key advantages of AI integration in ECG interpretation is its potential to reduce inter-observer variability. Traditional ECG interpretation can be subject to differences in individual expertise and experience. AI algorithms, once properly trained and validated, can provide consistent analysis across different healthcare settings, potentially standardizing the interpretation of hyperkalemia-induced T wave changes.
Moreover, AI systems can be designed to continuously learn and improve their performance over time. As more ECG data becomes available, these systems can be updated to enhance their accuracy in detecting subtle T wave inversions associated with varying degrees of hyperkalemia. This adaptive learning capability is particularly valuable in capturing the nuanced effects of hyperkalemia on ECG morphology across diverse patient populations.
The integration of AI in ECG interpretation also opens up possibilities for predictive analytics. By analyzing historical ECG data and patient outcomes, AI models could potentially predict the likelihood of hyperkalemia before overt ECG changes become apparent. This predictive capability could be invaluable in proactive patient management, especially for high-risk individuals with chronic kidney disease or those on certain medications.
However, it is important to note that while AI shows great promise, its integration into clinical practice requires careful validation and ongoing monitoring. The interpretability of AI decisions remains a challenge, and there is a need for transparent algorithms that can provide explanations for their findings. Additionally, the integration of AI systems must be balanced with the expertise of healthcare professionals, ensuring that AI serves as a supportive tool rather than a replacement for clinical judgment.
Recent studies have shown that AI models can effectively detect subtle changes in T wave morphology associated with hyperkalemia. These models are trained on large datasets of ECG recordings, allowing them to recognize patterns that may be challenging for human interpreters to consistently identify. The ability of AI to process vast amounts of data quickly and objectively makes it a valuable tool in emergency settings where rapid diagnosis of hyperkalemia is crucial.
One of the key advantages of AI integration in ECG interpretation is its potential to reduce inter-observer variability. Traditional ECG interpretation can be subject to differences in individual expertise and experience. AI algorithms, once properly trained and validated, can provide consistent analysis across different healthcare settings, potentially standardizing the interpretation of hyperkalemia-induced T wave changes.
Moreover, AI systems can be designed to continuously learn and improve their performance over time. As more ECG data becomes available, these systems can be updated to enhance their accuracy in detecting subtle T wave inversions associated with varying degrees of hyperkalemia. This adaptive learning capability is particularly valuable in capturing the nuanced effects of hyperkalemia on ECG morphology across diverse patient populations.
The integration of AI in ECG interpretation also opens up possibilities for predictive analytics. By analyzing historical ECG data and patient outcomes, AI models could potentially predict the likelihood of hyperkalemia before overt ECG changes become apparent. This predictive capability could be invaluable in proactive patient management, especially for high-risk individuals with chronic kidney disease or those on certain medications.
However, it is important to note that while AI shows great promise, its integration into clinical practice requires careful validation and ongoing monitoring. The interpretability of AI decisions remains a challenge, and there is a need for transparent algorithms that can provide explanations for their findings. Additionally, the integration of AI systems must be balanced with the expertise of healthcare professionals, ensuring that AI serves as a supportive tool rather than a replacement for clinical judgment.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!