Cori Cycle Role In Diabetes: Biomarkers And Clinical Implications
AUG 21, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Cori Cycle Overview
The Cori cycle, also known as the glucose-alanine cycle, is a metabolic pathway that plays a crucial role in glucose homeostasis and energy metabolism. Named after its discoverers, Carl and Gerty Cori, this cycle represents a bidirectional flow of glucose and lactate between the liver and peripheral tissues, particularly skeletal muscles.
In the context of glucose metabolism, the Cori cycle serves as a temporary measure to maintain blood glucose levels during periods of intense physical activity or fasting. When muscles engage in anaerobic glycolysis, they produce lactate as a byproduct. This lactate is then transported to the liver, where it is converted back into glucose through gluconeogenesis. The newly synthesized glucose can then be released into the bloodstream to maintain glucose homeostasis or stored as glycogen for future use.
The Cori cycle is intimately linked to the body's energy balance and plays a significant role in the regulation of blood glucose levels. During exercise or fasting, when glucose availability is limited, the cycle helps to preserve glucose for vital organs such as the brain while allowing muscles to continue functioning through anaerobic metabolism. This process is particularly important in maintaining energy supply during prolonged periods of physical exertion.
From a biochemical perspective, the Cori cycle involves several key enzymes and metabolic intermediates. In the muscles, glucose is broken down to pyruvate through glycolysis, and then converted to lactate by lactate dehydrogenase. The lactate is then transported to the liver, where it is converted back to pyruvate and subsequently to glucose through a series of enzymatic reactions, including those catalyzed by pyruvate carboxylase and phosphoenolpyruvate carboxykinase.
Understanding the Cori cycle is crucial in the context of diabetes, as this metabolic disorder is characterized by impaired glucose regulation. In diabetic patients, the efficiency of the Cori cycle may be altered, potentially contributing to the dysregulation of blood glucose levels. The cycle's function can be affected by insulin resistance, a hallmark of type 2 diabetes, which may lead to increased gluconeogenesis and exacerbate hyperglycemia.
Recent research has focused on the potential use of Cori cycle intermediates as biomarkers for diabetes and related metabolic disorders. Lactate levels, for instance, have been investigated as a potential indicator of insulin resistance and glucose intolerance. Additionally, the activity of key enzymes involved in the cycle, such as lactate dehydrogenase, may provide insights into the metabolic state of diabetic patients.
In the context of glucose metabolism, the Cori cycle serves as a temporary measure to maintain blood glucose levels during periods of intense physical activity or fasting. When muscles engage in anaerobic glycolysis, they produce lactate as a byproduct. This lactate is then transported to the liver, where it is converted back into glucose through gluconeogenesis. The newly synthesized glucose can then be released into the bloodstream to maintain glucose homeostasis or stored as glycogen for future use.
The Cori cycle is intimately linked to the body's energy balance and plays a significant role in the regulation of blood glucose levels. During exercise or fasting, when glucose availability is limited, the cycle helps to preserve glucose for vital organs such as the brain while allowing muscles to continue functioning through anaerobic metabolism. This process is particularly important in maintaining energy supply during prolonged periods of physical exertion.
From a biochemical perspective, the Cori cycle involves several key enzymes and metabolic intermediates. In the muscles, glucose is broken down to pyruvate through glycolysis, and then converted to lactate by lactate dehydrogenase. The lactate is then transported to the liver, where it is converted back to pyruvate and subsequently to glucose through a series of enzymatic reactions, including those catalyzed by pyruvate carboxylase and phosphoenolpyruvate carboxykinase.
Understanding the Cori cycle is crucial in the context of diabetes, as this metabolic disorder is characterized by impaired glucose regulation. In diabetic patients, the efficiency of the Cori cycle may be altered, potentially contributing to the dysregulation of blood glucose levels. The cycle's function can be affected by insulin resistance, a hallmark of type 2 diabetes, which may lead to increased gluconeogenesis and exacerbate hyperglycemia.
Recent research has focused on the potential use of Cori cycle intermediates as biomarkers for diabetes and related metabolic disorders. Lactate levels, for instance, have been investigated as a potential indicator of insulin resistance and glucose intolerance. Additionally, the activity of key enzymes involved in the cycle, such as lactate dehydrogenase, may provide insights into the metabolic state of diabetic patients.
Diabetes Market Analysis
The global diabetes market has been experiencing significant growth, driven by the increasing prevalence of diabetes worldwide. As of 2021, the International Diabetes Federation estimated that approximately 537 million adults were living with diabetes, a number projected to rise to 783 million by 2045. This surge in diabetes cases has led to a corresponding expansion in the market for diabetes-related products and services.
The diabetes market encompasses a wide range of offerings, including glucose monitoring devices, insulin delivery systems, oral medications, and lifestyle management tools. The glucose monitoring segment, in particular, has seen substantial innovation with the introduction of continuous glucose monitoring (CGM) systems and smart insulin pens. These technologies have not only improved patient outcomes but also contributed to market growth.
In terms of regional distribution, North America currently holds the largest share of the global diabetes market, followed by Europe and Asia-Pacific. The United States, in particular, represents a significant portion of the market due to its high diabetes prevalence and advanced healthcare infrastructure. However, emerging economies in Asia and Africa are expected to witness the fastest growth rates in the coming years, driven by improving healthcare access and rising diabetes awareness.
The competitive landscape of the diabetes market is characterized by the presence of both established pharmaceutical companies and innovative startups. Major players include Novo Nordisk, Sanofi, Eli Lilly, and Medtronic, which dominate the insulin and medical device segments. However, the market has also seen the entry of technology companies like Apple and Google, which are leveraging their expertise in data analytics and wearable technology to develop diabetes management solutions.
Recent trends in the diabetes market include a shift towards personalized medicine, with an increasing focus on tailoring treatments to individual patient profiles. This approach is supported by advancements in biomarker research, including studies on the Cori cycle's role in diabetes. Additionally, there is growing interest in non-invasive glucose monitoring technologies and the development of artificial pancreas systems, which could revolutionize diabetes management.
The market is also influenced by changing reimbursement policies and regulatory environments across different regions. For instance, the increasing coverage of CGM devices by insurance providers in developed countries has significantly boosted their adoption. Conversely, stringent regulatory requirements for new diabetes medications and devices can pose challenges to market entry and innovation.
The diabetes market encompasses a wide range of offerings, including glucose monitoring devices, insulin delivery systems, oral medications, and lifestyle management tools. The glucose monitoring segment, in particular, has seen substantial innovation with the introduction of continuous glucose monitoring (CGM) systems and smart insulin pens. These technologies have not only improved patient outcomes but also contributed to market growth.
In terms of regional distribution, North America currently holds the largest share of the global diabetes market, followed by Europe and Asia-Pacific. The United States, in particular, represents a significant portion of the market due to its high diabetes prevalence and advanced healthcare infrastructure. However, emerging economies in Asia and Africa are expected to witness the fastest growth rates in the coming years, driven by improving healthcare access and rising diabetes awareness.
The competitive landscape of the diabetes market is characterized by the presence of both established pharmaceutical companies and innovative startups. Major players include Novo Nordisk, Sanofi, Eli Lilly, and Medtronic, which dominate the insulin and medical device segments. However, the market has also seen the entry of technology companies like Apple and Google, which are leveraging their expertise in data analytics and wearable technology to develop diabetes management solutions.
Recent trends in the diabetes market include a shift towards personalized medicine, with an increasing focus on tailoring treatments to individual patient profiles. This approach is supported by advancements in biomarker research, including studies on the Cori cycle's role in diabetes. Additionally, there is growing interest in non-invasive glucose monitoring technologies and the development of artificial pancreas systems, which could revolutionize diabetes management.
The market is also influenced by changing reimbursement policies and regulatory environments across different regions. For instance, the increasing coverage of CGM devices by insurance providers in developed countries has significantly boosted their adoption. Conversely, stringent regulatory requirements for new diabetes medications and devices can pose challenges to market entry and innovation.
Cori Cycle Dysregulation
The Cori cycle, also known as the glucose-alanine cycle, plays a crucial role in glucose homeostasis and energy metabolism. In diabetes, this cycle becomes dysregulated, contributing to the pathophysiology of the disease. The dysregulation of the Cori cycle in diabetes is characterized by an imbalance between glucose production and utilization, leading to hyperglycemia and other metabolic disturbances.
In healthy individuals, the Cori cycle functions as a bidirectional pathway between the liver and peripheral tissues, primarily skeletal muscles. During exercise or fasting, muscles produce lactate from glucose through anaerobic glycolysis. This lactate is then transported to the liver, where it is converted back to glucose through gluconeogenesis. The newly synthesized glucose is released into the bloodstream, completing the cycle.
However, in diabetic patients, this delicate balance is disrupted. The liver exhibits increased gluconeogenesis, leading to excessive glucose production. Simultaneously, peripheral tissues, particularly skeletal muscles, show impaired glucose uptake and utilization due to insulin resistance. This combination results in a vicious cycle of hyperglycemia and further metabolic derangements.
The dysregulation of the Cori cycle in diabetes is closely linked to alterations in key enzymes and hormones. Insulin resistance leads to reduced activation of glycogen synthase and increased activity of glycogen phosphorylase, favoring glycogen breakdown. Additionally, the activity of gluconeogenic enzymes, such as phosphoenolpyruvate carboxykinase (PEPCK) and glucose-6-phosphatase, is upregulated in the diabetic liver.
Hormonal imbalances further exacerbate the Cori cycle dysregulation. Elevated levels of glucagon and cortisol, often observed in diabetes, stimulate hepatic glucose production. Conversely, the impaired insulin signaling fails to suppress gluconeogenesis effectively. This hormonal milieu creates a pro-gluconeogenic environment, contributing to persistent hyperglycemia.
The consequences of Cori cycle dysregulation extend beyond glucose metabolism. The increased flux through the cycle leads to elevated energy expenditure, as the conversion of lactate to glucose in the liver is an energy-consuming process. This may contribute to the catabolic state often observed in poorly controlled diabetes. Furthermore, the altered metabolic flux can impact other pathways, such as lipid metabolism and protein turnover, leading to a broader metabolic dysfunction.
Understanding the intricacies of Cori cycle dysregulation in diabetes is crucial for developing targeted therapeutic interventions. Potential strategies may include modulating key enzymes involved in the cycle, improving insulin sensitivity, or developing novel compounds that can regulate the flux through gluconeogenesis and glycolysis. By addressing the underlying mechanisms of Cori cycle dysregulation, it may be possible to achieve better glycemic control and mitigate the long-term complications associated with diabetes.
In healthy individuals, the Cori cycle functions as a bidirectional pathway between the liver and peripheral tissues, primarily skeletal muscles. During exercise or fasting, muscles produce lactate from glucose through anaerobic glycolysis. This lactate is then transported to the liver, where it is converted back to glucose through gluconeogenesis. The newly synthesized glucose is released into the bloodstream, completing the cycle.
However, in diabetic patients, this delicate balance is disrupted. The liver exhibits increased gluconeogenesis, leading to excessive glucose production. Simultaneously, peripheral tissues, particularly skeletal muscles, show impaired glucose uptake and utilization due to insulin resistance. This combination results in a vicious cycle of hyperglycemia and further metabolic derangements.
The dysregulation of the Cori cycle in diabetes is closely linked to alterations in key enzymes and hormones. Insulin resistance leads to reduced activation of glycogen synthase and increased activity of glycogen phosphorylase, favoring glycogen breakdown. Additionally, the activity of gluconeogenic enzymes, such as phosphoenolpyruvate carboxykinase (PEPCK) and glucose-6-phosphatase, is upregulated in the diabetic liver.
Hormonal imbalances further exacerbate the Cori cycle dysregulation. Elevated levels of glucagon and cortisol, often observed in diabetes, stimulate hepatic glucose production. Conversely, the impaired insulin signaling fails to suppress gluconeogenesis effectively. This hormonal milieu creates a pro-gluconeogenic environment, contributing to persistent hyperglycemia.
The consequences of Cori cycle dysregulation extend beyond glucose metabolism. The increased flux through the cycle leads to elevated energy expenditure, as the conversion of lactate to glucose in the liver is an energy-consuming process. This may contribute to the catabolic state often observed in poorly controlled diabetes. Furthermore, the altered metabolic flux can impact other pathways, such as lipid metabolism and protein turnover, leading to a broader metabolic dysfunction.
Understanding the intricacies of Cori cycle dysregulation in diabetes is crucial for developing targeted therapeutic interventions. Potential strategies may include modulating key enzymes involved in the cycle, improving insulin sensitivity, or developing novel compounds that can regulate the flux through gluconeogenesis and glycolysis. By addressing the underlying mechanisms of Cori cycle dysregulation, it may be possible to achieve better glycemic control and mitigate the long-term complications associated with diabetes.
Current Diagnostic Methods
01 Metabolic biomarkers for Cori cycle assessment
Various metabolic biomarkers can be used to assess the Cori cycle activity. These may include glucose, lactate, pyruvate, and other intermediates involved in the cycle. Measuring these biomarkers in blood or tissue samples can provide insights into the functioning of the Cori cycle and overall metabolic health.- Metabolic biomarkers for Cori cycle assessment: Various metabolic biomarkers can be used to assess the Cori cycle activity. These may include glucose, lactate, pyruvate, and other intermediates involved in the cycle. Measuring these biomarkers in blood or tissue samples can provide insights into the functioning of the Cori cycle and overall metabolic health.
- Genetic markers associated with Cori cycle regulation: Genetic markers related to enzymes and regulatory proteins involved in the Cori cycle can serve as biomarkers. These may include genes encoding for glucose-6-phosphatase, phosphoenolpyruvate carboxykinase, and other key enzymes. Analyzing these genetic markers can help identify individuals with altered Cori cycle function or susceptibility to related metabolic disorders.
- Imaging techniques for Cori cycle visualization: Advanced imaging techniques can be used to visualize and quantify Cori cycle activity in vivo. These may include positron emission tomography (PET) or magnetic resonance spectroscopy (MRS) with specific tracers or contrast agents designed to track glucose and lactate metabolism. Such imaging biomarkers can provide real-time insights into Cori cycle dynamics.
- Proteomic biomarkers for Cori cycle components: Proteomic analysis can identify and quantify proteins involved in the Cori cycle. These protein biomarkers may include enzymes, transporters, and regulatory proteins associated with glucose and lactate metabolism. Measuring these proteins in biological samples can provide information about Cori cycle activity and potential dysregulation.
- Hormonal biomarkers influencing Cori cycle: Hormones that regulate glucose metabolism and influence the Cori cycle can serve as biomarkers. These may include insulin, glucagon, cortisol, and catecholamines. Measuring these hormonal biomarkers can provide insights into the endocrine regulation of the Cori cycle and help identify potential metabolic imbalances.
02 Genetic markers associated with Cori cycle regulation
Genetic markers related to enzymes and regulatory proteins involved in the Cori cycle can serve as biomarkers. These may include genes encoding for glucose-6-phosphatase, phosphoenolpyruvate carboxykinase, and other key enzymes. Analyzing these genetic markers can help identify individuals with altered Cori cycle function or predisposition to related metabolic disorders.Expand Specific Solutions03 Imaging techniques for Cori cycle visualization
Advanced imaging techniques can be used to visualize and quantify Cori cycle activity in vivo. These may include positron emission tomography (PET) or magnetic resonance spectroscopy (MRS) with specific tracers or contrast agents designed to track glucose and lactate metabolism. Such imaging biomarkers can provide real-time information on Cori cycle dynamics.Expand Specific Solutions04 Proteomic biomarkers for Cori cycle components
Proteomic analysis can identify and quantify proteins involved in the Cori cycle. These protein biomarkers may include enzymes, transporters, and regulatory proteins associated with glucose and lactate metabolism. Measuring these proteomic biomarkers can provide insights into the expression and activity of key Cori cycle components.Expand Specific Solutions05 Hormonal biomarkers influencing Cori cycle regulation
Hormones that regulate glucose metabolism and influence the Cori cycle can serve as biomarkers. These may include insulin, glucagon, cortisol, and catecholamines. Measuring these hormonal biomarkers can provide information on the endocrine regulation of the Cori cycle and its adaptation to various physiological states.Expand Specific Solutions
Key Research Institutions
The Cori Cycle's role in diabetes presents a complex competitive landscape in the biomedical research and healthcare industry. The field is in a mature stage of development, with significant market potential due to the global prevalence of diabetes. The technology's maturity is evident through the involvement of established players like Roche Diagnostics GmbH and F. Hoffmann-La Roche Ltd, who are leveraging their expertise in diabetes care and diagnostics. Emerging companies such as Metabolon, Inc. and GATC Health Corp are driving innovation in metabolomics and AI-driven biomarker discovery, potentially revolutionizing diabetes management. Academic institutions like MIT and Johns Hopkins University contribute cutting-edge research, while specialized centers like City of Hope National Cancer Institute focus on diabetes-related complications, collectively advancing the field's understanding and clinical applications.
F. Hoffmann-La Roche Ltd.
Technical Solution: Roche has developed advanced biomarker technologies to study the Cori cycle's role in diabetes. Their approach involves high-throughput metabolomics to identify key metabolites in the glucose-lactate shuttle. They've created a panel of biomarkers including lactate, pyruvate, and glucose-6-phosphate to assess Cori cycle activity[1]. Roche's platform integrates these biomarkers with machine learning algorithms to predict diabetes progression and treatment response[2]. Their research has shown that alterations in Cori cycle metabolites can precede clinical diabetes diagnosis by several years, potentially enabling earlier intervention[3].
Strengths: Comprehensive biomarker panel, integration with AI for predictive analytics, and potential for early diabetes detection. Weaknesses: Requires specialized equipment and expertise, potentially high cost for widespread implementation.
Metabolon, Inc.
Technical Solution: Metabolon has developed a proprietary metabolomics platform to study the Cori cycle in diabetes. Their technology, called Global Metabolomics, can simultaneously measure thousands of metabolites, including those central to the Cori cycle[4]. They've identified novel biomarkers related to glucose and lactate metabolism that correlate with insulin resistance and diabetes progression. Metabolon's approach includes longitudinal studies to track changes in Cori cycle metabolites over time, providing insights into disease trajectory and treatment efficacy[5]. They've also developed targeted assays for key Cori cycle intermediates, allowing for more focused and cost-effective clinical applications[6].
Strengths: Comprehensive metabolite profiling, longitudinal study capabilities, and targeted assays for clinical use. Weaknesses: Complex data interpretation, potential for false positives due to the broad scope of metabolite analysis.
Innovative Biomarkers
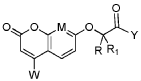
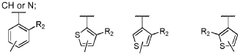
Coumarin derivatives, processes for their preparation and uses thereof for the treatment of cancer
PatentWO2019057821A1
Innovation
- Development of specific coumarin derivatives that inhibit POLRMT, capable of inhibiting mitochondrial DNA replication and transcription, offering a novel approach for cancer treatment, including use in combination with other cancer therapies.
Regulatory Considerations
The regulatory landscape surrounding the Cori cycle's role in diabetes and its associated biomarkers is complex and multifaceted. Regulatory bodies, such as the Food and Drug Administration (FDA) in the United States and the European Medicines Agency (EMA) in Europe, play crucial roles in overseeing the development, validation, and implementation of biomarkers related to the Cori cycle in diabetes management.
These agencies have established guidelines for the qualification and validation of biomarkers, which are essential for their use in clinical practice and drug development. For instance, the FDA's Biomarker Qualification Program provides a framework for evaluating and accepting biomarkers for specific contexts of use. This process ensures that biomarkers related to the Cori cycle meet rigorous scientific standards before being integrated into diabetes management protocols.
In the context of diabetes, regulatory considerations extend to the development of diagnostic tests and medical devices that measure Cori cycle-related biomarkers. These products must undergo thorough evaluation to demonstrate their accuracy, reliability, and clinical utility. Regulatory bodies require extensive clinical data to support claims about a biomarker's ability to predict, diagnose, or monitor diabetes progression.
Furthermore, the use of Cori cycle biomarkers in clinical trials for diabetes treatments is subject to regulatory scrutiny. Sponsors must provide robust scientific evidence to support the use of these biomarkers as surrogate endpoints or as tools for patient stratification. This often involves demonstrating a clear link between the biomarker and clinically meaningful outcomes in diabetes management.
Privacy and data protection regulations also come into play when dealing with biomarker data. As the collection and analysis of Cori cycle biomarkers often involve sensitive patient information, compliance with regulations such as the General Data Protection Regulation (GDPR) in Europe and the Health Insurance Portability and Accountability Act (HIPAA) in the United States is paramount.
Regulatory bodies are increasingly focusing on the standardization of biomarker measurements across different laboratories and healthcare settings. This standardization is crucial for ensuring the consistency and comparability of Cori cycle biomarker results, which is essential for their widespread adoption in clinical practice.
As research into the Cori cycle's role in diabetes progresses, regulatory frameworks may need to evolve to keep pace with scientific advancements. This could involve updating guidelines for biomarker validation, revising clinical trial designs, or developing new regulatory pathways for innovative diagnostic approaches based on Cori cycle insights.
These agencies have established guidelines for the qualification and validation of biomarkers, which are essential for their use in clinical practice and drug development. For instance, the FDA's Biomarker Qualification Program provides a framework for evaluating and accepting biomarkers for specific contexts of use. This process ensures that biomarkers related to the Cori cycle meet rigorous scientific standards before being integrated into diabetes management protocols.
In the context of diabetes, regulatory considerations extend to the development of diagnostic tests and medical devices that measure Cori cycle-related biomarkers. These products must undergo thorough evaluation to demonstrate their accuracy, reliability, and clinical utility. Regulatory bodies require extensive clinical data to support claims about a biomarker's ability to predict, diagnose, or monitor diabetes progression.
Furthermore, the use of Cori cycle biomarkers in clinical trials for diabetes treatments is subject to regulatory scrutiny. Sponsors must provide robust scientific evidence to support the use of these biomarkers as surrogate endpoints or as tools for patient stratification. This often involves demonstrating a clear link between the biomarker and clinically meaningful outcomes in diabetes management.
Privacy and data protection regulations also come into play when dealing with biomarker data. As the collection and analysis of Cori cycle biomarkers often involve sensitive patient information, compliance with regulations such as the General Data Protection Regulation (GDPR) in Europe and the Health Insurance Portability and Accountability Act (HIPAA) in the United States is paramount.
Regulatory bodies are increasingly focusing on the standardization of biomarker measurements across different laboratories and healthcare settings. This standardization is crucial for ensuring the consistency and comparability of Cori cycle biomarker results, which is essential for their widespread adoption in clinical practice.
As research into the Cori cycle's role in diabetes progresses, regulatory frameworks may need to evolve to keep pace with scientific advancements. This could involve updating guidelines for biomarker validation, revising clinical trial designs, or developing new regulatory pathways for innovative diagnostic approaches based on Cori cycle insights.
Personalized Medicine
The Cori cycle's role in diabetes has significant implications for personalized medicine approaches in managing this complex metabolic disorder. By understanding the intricate relationship between glucose and lactate metabolism, healthcare providers can tailor treatment strategies to individual patients, optimizing glycemic control and reducing complications.
Personalized medicine in diabetes management involves utilizing biomarkers associated with the Cori cycle to assess an individual's metabolic profile. These biomarkers, such as lactate levels, glucose-to-lactate ratios, and enzyme activities involved in gluconeogenesis, can provide valuable insights into a patient's unique metabolic state. By analyzing these parameters, clinicians can identify specific metabolic imbalances and develop targeted interventions.
One key aspect of personalized medicine in this context is the potential for customized dietary recommendations. Patients with altered Cori cycle function may benefit from specific macronutrient ratios or timing of meals to optimize glucose utilization and minimize excessive lactate production. This tailored approach can lead to improved glycemic control and reduced risk of complications.
Furthermore, personalized medicine strategies can leverage genetic information related to enzymes involved in the Cori cycle. Genetic variations affecting key enzymes such as glucose-6-phosphatase or phosphoenolpyruvate carboxykinase may influence an individual's response to certain medications or lifestyle interventions. By incorporating genetic profiling into treatment plans, healthcare providers can select the most effective therapies for each patient.
The integration of continuous glucose monitoring (CGM) technology with Cori cycle biomarkers offers another avenue for personalized diabetes management. Real-time data on glucose fluctuations, combined with periodic assessments of lactate levels and other relevant biomarkers, can provide a comprehensive picture of an individual's metabolic status. This information enables healthcare providers to make dynamic adjustments to treatment regimens, optimizing glycemic control on an ongoing basis.
Personalized medicine approaches also extend to the selection and dosing of diabetes medications. By considering an individual's Cori cycle function and related biomarkers, clinicians can choose pharmacological interventions that specifically target the patient's metabolic deficits. For example, patients with impaired gluconeogenesis may benefit from medications that enhance insulin sensitivity or reduce hepatic glucose output.
In conclusion, the integration of Cori cycle-related biomarkers and clinical implications into personalized medicine strategies holds great promise for improving diabetes management. By tailoring interventions to each patient's unique metabolic profile, healthcare providers can enhance treatment efficacy, minimize adverse effects, and ultimately improve long-term outcomes for individuals living with diabetes.
Personalized medicine in diabetes management involves utilizing biomarkers associated with the Cori cycle to assess an individual's metabolic profile. These biomarkers, such as lactate levels, glucose-to-lactate ratios, and enzyme activities involved in gluconeogenesis, can provide valuable insights into a patient's unique metabolic state. By analyzing these parameters, clinicians can identify specific metabolic imbalances and develop targeted interventions.
One key aspect of personalized medicine in this context is the potential for customized dietary recommendations. Patients with altered Cori cycle function may benefit from specific macronutrient ratios or timing of meals to optimize glucose utilization and minimize excessive lactate production. This tailored approach can lead to improved glycemic control and reduced risk of complications.
Furthermore, personalized medicine strategies can leverage genetic information related to enzymes involved in the Cori cycle. Genetic variations affecting key enzymes such as glucose-6-phosphatase or phosphoenolpyruvate carboxykinase may influence an individual's response to certain medications or lifestyle interventions. By incorporating genetic profiling into treatment plans, healthcare providers can select the most effective therapies for each patient.
The integration of continuous glucose monitoring (CGM) technology with Cori cycle biomarkers offers another avenue for personalized diabetes management. Real-time data on glucose fluctuations, combined with periodic assessments of lactate levels and other relevant biomarkers, can provide a comprehensive picture of an individual's metabolic status. This information enables healthcare providers to make dynamic adjustments to treatment regimens, optimizing glycemic control on an ongoing basis.
Personalized medicine approaches also extend to the selection and dosing of diabetes medications. By considering an individual's Cori cycle function and related biomarkers, clinicians can choose pharmacological interventions that specifically target the patient's metabolic deficits. For example, patients with impaired gluconeogenesis may benefit from medications that enhance insulin sensitivity or reduce hepatic glucose output.
In conclusion, the integration of Cori cycle-related biomarkers and clinical implications into personalized medicine strategies holds great promise for improving diabetes management. By tailoring interventions to each patient's unique metabolic profile, healthcare providers can enhance treatment efficacy, minimize adverse effects, and ultimately improve long-term outcomes for individuals living with diabetes.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!