Examining augmented feedback loops in laryngoscope training.
JUL 14, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Laryngoscope Training Evolution and Objectives
Laryngoscopy, a critical procedure in airway management, has undergone significant evolution in training methodologies over the past decades. The primary objective of laryngoscope training has consistently been to develop proficient healthcare professionals capable of performing safe and effective intubations. This goal remains paramount as the complexity of medical procedures and patient care continues to increase.
The evolution of laryngoscope training can be traced back to the early 20th century when direct laryngoscopy was first introduced. Initially, training relied heavily on apprenticeship models, where novice practitioners learned through observation and guided practice under the supervision of experienced clinicians. This approach, while effective to some extent, had limitations in standardization and scalability.
As medical education advanced, simulation-based training emerged as a cornerstone in laryngoscope skill development. The introduction of mannequins and task trainers in the latter half of the 20th century marked a significant shift in training paradigms. These tools allowed for repeated practice in a controlled environment, reducing the risks associated with learning on actual patients and providing a standardized platform for skill acquisition.
The advent of video laryngoscopy in the late 1990s and early 2000s brought about another revolution in both clinical practice and training methodologies. This technology not only improved the success rates of difficult intubations but also enhanced the teaching process by allowing instructors and trainees to share the same view of the airway in real-time.
In recent years, the integration of augmented reality (AR) and virtual reality (VR) technologies has begun to reshape laryngoscope training objectives. These immersive technologies aim to bridge the gap between simulation and real-world practice by providing highly realistic, interactive training environments. The objective has expanded from mere skill acquisition to developing adaptive expertise, enabling practitioners to handle a wide array of clinical scenarios with confidence.
The current focus on augmented feedback loops in laryngoscope training represents the latest evolution in this field. This approach aims to provide trainees with real-time, data-driven feedback on their performance, allowing for more precise skill refinement and accelerated learning curves. The objective is to create a dynamic learning environment that adapts to individual learner needs, promoting faster skill acquisition and retention.
As we look to the future, the objectives of laryngoscope training continue to evolve. There is an increasing emphasis on developing not just technical proficiency, but also non-technical skills such as decision-making, situational awareness, and effective communication in high-stress environments. The ultimate goal remains to produce highly competent healthcare professionals capable of delivering optimal patient care in diverse and challenging clinical settings.
The evolution of laryngoscope training can be traced back to the early 20th century when direct laryngoscopy was first introduced. Initially, training relied heavily on apprenticeship models, where novice practitioners learned through observation and guided practice under the supervision of experienced clinicians. This approach, while effective to some extent, had limitations in standardization and scalability.
As medical education advanced, simulation-based training emerged as a cornerstone in laryngoscope skill development. The introduction of mannequins and task trainers in the latter half of the 20th century marked a significant shift in training paradigms. These tools allowed for repeated practice in a controlled environment, reducing the risks associated with learning on actual patients and providing a standardized platform for skill acquisition.
The advent of video laryngoscopy in the late 1990s and early 2000s brought about another revolution in both clinical practice and training methodologies. This technology not only improved the success rates of difficult intubations but also enhanced the teaching process by allowing instructors and trainees to share the same view of the airway in real-time.
In recent years, the integration of augmented reality (AR) and virtual reality (VR) technologies has begun to reshape laryngoscope training objectives. These immersive technologies aim to bridge the gap between simulation and real-world practice by providing highly realistic, interactive training environments. The objective has expanded from mere skill acquisition to developing adaptive expertise, enabling practitioners to handle a wide array of clinical scenarios with confidence.
The current focus on augmented feedback loops in laryngoscope training represents the latest evolution in this field. This approach aims to provide trainees with real-time, data-driven feedback on their performance, allowing for more precise skill refinement and accelerated learning curves. The objective is to create a dynamic learning environment that adapts to individual learner needs, promoting faster skill acquisition and retention.
As we look to the future, the objectives of laryngoscope training continue to evolve. There is an increasing emphasis on developing not just technical proficiency, but also non-technical skills such as decision-making, situational awareness, and effective communication in high-stress environments. The ultimate goal remains to produce highly competent healthcare professionals capable of delivering optimal patient care in diverse and challenging clinical settings.
Market Analysis for Advanced Medical Training Tools
The market for advanced medical training tools, particularly those incorporating augmented feedback loops in laryngoscope training, is experiencing significant growth and transformation. This trend is driven by the increasing demand for more effective and efficient medical education methods, especially in critical care and anesthesiology fields.
The global medical simulation market, which includes advanced training tools for procedures like laryngoscopy, was valued at approximately $1.9 billion in 2020 and is projected to reach $3.7 billion by 2025, growing at a CAGR of 14.6%. This growth is primarily fueled by the rising focus on patient safety, the growing emphasis on minimizing medical errors, and the increasing adoption of simulation-based training in medical education curricula.
Specifically, the market for laryngoscope training tools with augmented feedback loops is a niche but rapidly expanding segment within this broader market. The demand for these advanced training tools is driven by several factors, including the complexity of laryngoscopy procedures, the need for precise skill development, and the potential for improved patient outcomes through better-trained medical professionals.
Healthcare institutions, medical schools, and simulation centers are the primary consumers of these advanced training tools. There is a growing recognition of the value of simulation-based training in reducing the learning curve for complex medical procedures like laryngoscopy. This has led to increased investment in high-fidelity simulation equipment, including those with augmented feedback capabilities.
The market is also influenced by technological advancements in augmented reality (AR) and virtual reality (VR) technologies. These innovations are enabling the development of more sophisticated and realistic training simulators that can provide real-time feedback and performance analysis. The integration of these technologies into laryngoscope training tools is expected to drive market growth further in the coming years.
Geographically, North America currently dominates the market for advanced medical training tools, followed by Europe and Asia-Pacific. However, emerging economies in Asia and Latin America are expected to witness the highest growth rates in the adoption of these technologies, driven by increasing healthcare expenditure and a growing focus on improving medical education standards.
Key market players in this space include medical simulation companies, healthcare technology firms, and educational technology providers. These companies are increasingly focusing on developing integrated solutions that combine hardware (like laryngoscope simulators) with software platforms that provide detailed feedback and performance analytics.
The global medical simulation market, which includes advanced training tools for procedures like laryngoscopy, was valued at approximately $1.9 billion in 2020 and is projected to reach $3.7 billion by 2025, growing at a CAGR of 14.6%. This growth is primarily fueled by the rising focus on patient safety, the growing emphasis on minimizing medical errors, and the increasing adoption of simulation-based training in medical education curricula.
Specifically, the market for laryngoscope training tools with augmented feedback loops is a niche but rapidly expanding segment within this broader market. The demand for these advanced training tools is driven by several factors, including the complexity of laryngoscopy procedures, the need for precise skill development, and the potential for improved patient outcomes through better-trained medical professionals.
Healthcare institutions, medical schools, and simulation centers are the primary consumers of these advanced training tools. There is a growing recognition of the value of simulation-based training in reducing the learning curve for complex medical procedures like laryngoscopy. This has led to increased investment in high-fidelity simulation equipment, including those with augmented feedback capabilities.
The market is also influenced by technological advancements in augmented reality (AR) and virtual reality (VR) technologies. These innovations are enabling the development of more sophisticated and realistic training simulators that can provide real-time feedback and performance analysis. The integration of these technologies into laryngoscope training tools is expected to drive market growth further in the coming years.
Geographically, North America currently dominates the market for advanced medical training tools, followed by Europe and Asia-Pacific. However, emerging economies in Asia and Latin America are expected to witness the highest growth rates in the adoption of these technologies, driven by increasing healthcare expenditure and a growing focus on improving medical education standards.
Key market players in this space include medical simulation companies, healthcare technology firms, and educational technology providers. These companies are increasingly focusing on developing integrated solutions that combine hardware (like laryngoscope simulators) with software platforms that provide detailed feedback and performance analytics.
Current Challenges in Laryngoscope Skill Acquisition
Laryngoscope skill acquisition presents several significant challenges in medical education and training. One of the primary obstacles is the steep learning curve associated with mastering the technique. Novice practitioners often struggle with proper hand-eye coordination and the ability to visualize the airway structures effectively. This difficulty is compounded by the limited opportunities for hands-on practice in real clinical settings, as patient safety is paramount.
The lack of immediate and objective feedback during training sessions poses another substantial challenge. Traditional methods often rely on subjective assessments from instructors, which may not provide learners with precise information about their performance. This gap in feedback can lead to the reinforcement of incorrect techniques or slow progress in skill development.
Furthermore, the variability in patient anatomy and clinical scenarios adds complexity to the learning process. Trainees need exposure to a wide range of situations to develop proficiency, but achieving this breadth of experience within the constraints of clinical rotations and patient availability is problematic.
The psychological stress associated with performing laryngoscopy, particularly in high-stakes situations, can significantly impact skill acquisition and performance. Learners may experience anxiety and hesitation, which can hinder their ability to apply learned techniques effectively in real-world scenarios.
Another challenge lies in the transfer of skills from simulation-based training to actual patient care. While simulators provide a safe environment for practice, they may not fully replicate the nuances and complexities of real human anatomy and physiology. This discrepancy can lead to a false sense of competence or difficulties in adapting learned skills to live patients.
The assessment of competency in laryngoscope skills also presents challenges. Standardized evaluation methods that accurately measure proficiency across various aspects of the procedure are not always consistently implemented or validated. This lack of uniformity in assessment can make it difficult to ensure that all practitioners meet the necessary skill levels before independent practice.
Lastly, the rapid evolution of technology in airway management, including video laryngoscopes and other advanced devices, creates an ongoing need for practitioners to adapt and update their skills. Balancing the acquisition of traditional direct laryngoscopy skills with newer techniques adds another layer of complexity to the training process.
The lack of immediate and objective feedback during training sessions poses another substantial challenge. Traditional methods often rely on subjective assessments from instructors, which may not provide learners with precise information about their performance. This gap in feedback can lead to the reinforcement of incorrect techniques or slow progress in skill development.
Furthermore, the variability in patient anatomy and clinical scenarios adds complexity to the learning process. Trainees need exposure to a wide range of situations to develop proficiency, but achieving this breadth of experience within the constraints of clinical rotations and patient availability is problematic.
The psychological stress associated with performing laryngoscopy, particularly in high-stakes situations, can significantly impact skill acquisition and performance. Learners may experience anxiety and hesitation, which can hinder their ability to apply learned techniques effectively in real-world scenarios.
Another challenge lies in the transfer of skills from simulation-based training to actual patient care. While simulators provide a safe environment for practice, they may not fully replicate the nuances and complexities of real human anatomy and physiology. This discrepancy can lead to a false sense of competence or difficulties in adapting learned skills to live patients.
The assessment of competency in laryngoscope skills also presents challenges. Standardized evaluation methods that accurately measure proficiency across various aspects of the procedure are not always consistently implemented or validated. This lack of uniformity in assessment can make it difficult to ensure that all practitioners meet the necessary skill levels before independent practice.
Lastly, the rapid evolution of technology in airway management, including video laryngoscopes and other advanced devices, creates an ongoing need for practitioners to adapt and update their skills. Balancing the acquisition of traditional direct laryngoscopy skills with newer techniques adds another layer of complexity to the training process.
Existing Augmented Feedback Solutions
01 Image processing and feedback in laryngoscopy
Advanced image processing techniques are applied to laryngoscope systems to enhance visualization and provide real-time feedback. These systems may include image analysis algorithms, augmented reality overlays, and automatic adjustments to improve image quality during procedures.- Image processing and feedback in laryngoscopy: Advanced image processing techniques are applied to laryngoscope systems to enhance visualization and provide real-time feedback. These systems may include image analysis algorithms, augmented reality overlays, and automatic adjustments to improve image quality during procedures. Such feedback loops help medical professionals make more accurate diagnoses and perform interventions more effectively.
- Wireless communication and control in laryngoscopes: Modern laryngoscopes incorporate wireless communication technologies to transmit data, receive commands, and integrate with other medical devices. This enables remote monitoring, control, and data sharing, enhancing the overall efficiency of laryngoscopic procedures. Wireless feedback loops allow for real-time adjustments and improved coordination among medical team members.
- Adaptive power management in laryngoscope systems: Laryngoscope designs now include sophisticated power management systems with feedback loops to optimize energy consumption. These systems can dynamically adjust power usage based on the device's operational state, environmental conditions, and user preferences. This adaptive approach extends battery life and ensures consistent performance during critical procedures.
- Sensor integration for enhanced laryngoscope performance: Advanced sensors are integrated into laryngoscopes to provide various types of feedback, including pressure sensing, temperature monitoring, and position tracking. These sensors create feedback loops that help prevent tissue damage, ensure proper device placement, and assist in navigation during intubation procedures. The sensor data can be processed in real-time to provide guidance to the operator.
- Machine learning and AI in laryngoscope feedback systems: Artificial intelligence and machine learning algorithms are being incorporated into laryngoscope feedback systems to enhance decision-making and automate certain aspects of the procedure. These intelligent systems can analyze patterns, predict potential issues, and provide personalized recommendations to healthcare providers. The continuous learning capability of these systems allows for ongoing improvement in laryngoscope performance and patient outcomes.
02 Wireless communication and control in laryngoscopes
Laryngoscopes incorporate wireless communication technologies for data transmission, remote control, and integration with other medical devices. This enables real-time sharing of visual data, remote guidance, and improved coordination during procedures.Expand Specific Solutions03 Adaptive power management and feedback loops
Laryngoscope systems implement adaptive power management techniques and feedback loops to optimize performance and energy efficiency. These systems may include automatic power adjustments based on usage patterns, environmental conditions, and real-time sensor data.Expand Specific Solutions04 Sensor integration and data fusion in laryngoscopes
Modern laryngoscopes integrate multiple sensors to gather diverse data during procedures. These may include pressure sensors, temperature sensors, and motion sensors. Data fusion techniques are employed to combine sensor inputs and provide comprehensive feedback to the user.Expand Specific Solutions05 User interface and feedback mechanisms
Advanced user interfaces are developed for laryngoscopes to provide intuitive feedback to the operator. These may include haptic feedback systems, audio cues, and visual displays that offer real-time guidance and alerts during procedures.Expand Specific Solutions
Key Players in Medical Simulation Industry
The augmented feedback loops in laryngoscope training market is in its early growth stage, with increasing adoption of advanced technologies in medical education. The market size is expanding as healthcare institutions recognize the value of enhanced training methods. Technologically, the field is evolving rapidly, with companies like Google, Microsoft, and Apple contributing to innovations in augmented reality and feedback systems. Smaller specialized firms like MedRhythms and Bell Therapeutics are developing targeted digital therapeutic solutions. Academic institutions such as MIT and the University of Cincinnati are conducting research to improve training methodologies. While not yet fully mature, the technology is progressing quickly, driven by collaborations between tech giants, medical device companies, and research institutions.
Massachusetts Institute of Technology
Technical Solution: MIT has developed an advanced augmented reality (AR) system for laryngoscope training. Their solution integrates computer vision and machine learning algorithms to create a dynamic, interactive training environment. The system uses a combination of cameras and depth sensors to track the laryngoscope's position and orientation in 3D space. This data is then used to generate real-time AR overlays that guide the trainee through the intubation process. The AR system projects anatomical landmarks, optimal insertion paths, and potential obstacles directly onto the trainee's field of view[2][5]. Additionally, the system incorporates a haptic feedback mechanism that simulates tissue resistance and provides subtle cues to guide proper technique. Machine learning algorithms analyze the trainee's performance over time, adapting the difficulty and focus of training scenarios to optimize learning outcomes.
Strengths: Highly immersive and interactive training experience; personalized learning through AI adaptation; non-invasive guidance system. Weaknesses: Requires sophisticated hardware and software integration; may have a steep learning curve for instructors and trainees.
Cincinnati Children's Hospital Medical Center
Technical Solution: Cincinnati Children's Hospital Medical Center has developed an innovative augmented feedback system for laryngoscope training. Their approach utilizes real-time video feedback combined with motion tracking sensors to provide trainees with immediate visual and haptic feedback during simulated intubation procedures. The system incorporates a high-resolution camera mounted on the laryngoscope blade, which transmits live video to a head-mounted display worn by the trainee. This allows for a first-person view of the airway during the procedure. Additionally, force sensors on the laryngoscope handle measure the applied pressure, providing tactile feedback to prevent excessive force[1][3]. The system also includes a machine learning algorithm that analyzes the trainee's technique and provides personalized recommendations for improvement.
Strengths: Provides real-time, multi-modal feedback; enhances situational awareness; allows for objective assessment of technique. Weaknesses: May be costly to implement; requires additional equipment that could interfere with natural movement.
Innovative Feedback Mechanisms for Laryngoscopy
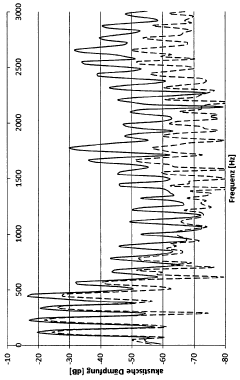
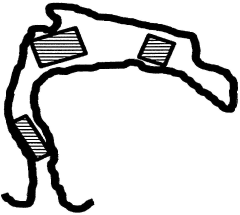
apparatus and method for adjusting the human vocal tract using feedback
PatentInactiveDE102019002734A1
Innovation
- A computer-aided training method using visual and acoustic feedback to guide users in adjusting the vocal tract by displaying predetermined vocal tract shapes and resonance ranges, allowing for real-time analysis and simulation of acoustic signals to facilitate targeted geometric changes.
Regulatory Framework for Medical Training Devices
The regulatory framework for medical training devices, including augmented feedback systems for laryngoscope training, is complex and multifaceted. In the United States, the Food and Drug Administration (FDA) plays a crucial role in overseeing these devices. Medical training devices are typically classified as Class I or Class II medical devices, depending on their level of risk and intended use.
For laryngoscope training systems with augmented feedback loops, the FDA's Center for Devices and Radiological Health (CDRH) is responsible for their regulation. These devices often fall under the category of "simulation technology for health care education and training," which the FDA recognizes as an important tool for improving patient safety and healthcare outcomes.
The regulatory pathway for such devices usually involves a 510(k) premarket notification submission. This process requires manufacturers to demonstrate that their device is substantially equivalent to a legally marketed predicate device in terms of safety and effectiveness. For novel technologies like augmented feedback systems, the FDA may require additional clinical data or usability studies to ensure their safety and efficacy in training settings.
In the European Union, medical training devices are regulated under the Medical Device Regulation (MDR). The MDR places a strong emphasis on clinical evaluation and post-market surveillance, which is particularly relevant for innovative training technologies. Manufacturers must obtain CE marking to indicate compliance with EU health, safety, and environmental protection standards.
Internationally, the International Medical Device Regulators Forum (IMDRF) provides guidance on the harmonization of medical device regulations across different countries. Their recommendations often influence national regulatory frameworks, including those pertaining to training devices.
Specific to augmented feedback systems in laryngoscope training, regulators are increasingly focusing on the software components of these devices. The FDA's guidance on "Software as a Medical Device" (SaMD) is particularly relevant, as it addresses the unique challenges posed by software-driven medical technologies.
Regulatory bodies also consider the potential risks associated with these training devices, such as the accuracy of feedback mechanisms and the transfer of skills from simulated to real-world environments. As a result, manufacturers may be required to conduct validation studies to demonstrate the effectiveness of their augmented feedback systems in improving laryngoscopy skills and patient outcomes.
For laryngoscope training systems with augmented feedback loops, the FDA's Center for Devices and Radiological Health (CDRH) is responsible for their regulation. These devices often fall under the category of "simulation technology for health care education and training," which the FDA recognizes as an important tool for improving patient safety and healthcare outcomes.
The regulatory pathway for such devices usually involves a 510(k) premarket notification submission. This process requires manufacturers to demonstrate that their device is substantially equivalent to a legally marketed predicate device in terms of safety and effectiveness. For novel technologies like augmented feedback systems, the FDA may require additional clinical data or usability studies to ensure their safety and efficacy in training settings.
In the European Union, medical training devices are regulated under the Medical Device Regulation (MDR). The MDR places a strong emphasis on clinical evaluation and post-market surveillance, which is particularly relevant for innovative training technologies. Manufacturers must obtain CE marking to indicate compliance with EU health, safety, and environmental protection standards.
Internationally, the International Medical Device Regulators Forum (IMDRF) provides guidance on the harmonization of medical device regulations across different countries. Their recommendations often influence national regulatory frameworks, including those pertaining to training devices.
Specific to augmented feedback systems in laryngoscope training, regulators are increasingly focusing on the software components of these devices. The FDA's guidance on "Software as a Medical Device" (SaMD) is particularly relevant, as it addresses the unique challenges posed by software-driven medical technologies.
Regulatory bodies also consider the potential risks associated with these training devices, such as the accuracy of feedback mechanisms and the transfer of skills from simulated to real-world environments. As a result, manufacturers may be required to conduct validation studies to demonstrate the effectiveness of their augmented feedback systems in improving laryngoscopy skills and patient outcomes.
Cost-Benefit Analysis of Augmented Feedback Systems
The implementation of augmented feedback systems in laryngoscope training presents a complex cost-benefit scenario that requires careful analysis. On the cost side, the initial investment in hardware and software for augmented reality (AR) or virtual reality (VR) systems can be substantial. High-quality headsets, haptic feedback devices, and specialized training software often come with significant upfront expenses. Additionally, there are ongoing costs associated with system maintenance, software updates, and potential hardware replacements.
Training personnel to effectively use and manage these systems also incurs costs in terms of time and resources. Healthcare institutions may need to allocate staff hours for learning the new technology and integrating it into existing training protocols. There might also be costs related to redesigning training spaces to accommodate the AR/VR equipment.
However, the potential benefits of augmented feedback systems in laryngoscope training are considerable. One of the primary advantages is the accelerated learning curve for trainees. Studies have shown that AR-enhanced training can significantly reduce the time required for novice practitioners to achieve proficiency in laryngoscopy techniques. This faster skill acquisition can lead to more efficient use of training resources and potentially earlier deployment of competent professionals in clinical settings.
The improved accuracy and reduced error rates associated with augmented feedback training can have far-reaching benefits. By providing real-time guidance and immediate feedback on technique, these systems can help prevent the development of poor habits and reduce the risk of patient injury during actual procedures. This enhanced safety profile could lead to reduced liability costs and improved patient outcomes.
From a long-term perspective, the scalability of augmented feedback systems offers potential cost savings. Once developed, the training software can be easily distributed and updated across multiple institutions, potentially reducing the need for expensive physical simulators or cadaver labs. This scalability also allows for more consistent training experiences across different locations, ensuring standardized skill development.
The data collection capabilities of these systems present another valuable benefit. By tracking trainee performance metrics over time, institutions can gain insights into the effectiveness of their training programs and identify areas for improvement. This data-driven approach to medical education can lead to more efficient allocation of resources and continuous refinement of training methodologies.
In conclusion, while the initial costs of implementing augmented feedback systems for laryngoscope training can be substantial, the long-term benefits in terms of improved training efficiency, enhanced patient safety, and data-driven educational insights suggest a potentially favorable cost-benefit ratio. As technology costs continue to decrease and the systems become more sophisticated, the value proposition of these augmented feedback loops in medical training is likely to become increasingly compelling.
Training personnel to effectively use and manage these systems also incurs costs in terms of time and resources. Healthcare institutions may need to allocate staff hours for learning the new technology and integrating it into existing training protocols. There might also be costs related to redesigning training spaces to accommodate the AR/VR equipment.
However, the potential benefits of augmented feedback systems in laryngoscope training are considerable. One of the primary advantages is the accelerated learning curve for trainees. Studies have shown that AR-enhanced training can significantly reduce the time required for novice practitioners to achieve proficiency in laryngoscopy techniques. This faster skill acquisition can lead to more efficient use of training resources and potentially earlier deployment of competent professionals in clinical settings.
The improved accuracy and reduced error rates associated with augmented feedback training can have far-reaching benefits. By providing real-time guidance and immediate feedback on technique, these systems can help prevent the development of poor habits and reduce the risk of patient injury during actual procedures. This enhanced safety profile could lead to reduced liability costs and improved patient outcomes.
From a long-term perspective, the scalability of augmented feedback systems offers potential cost savings. Once developed, the training software can be easily distributed and updated across multiple institutions, potentially reducing the need for expensive physical simulators or cadaver labs. This scalability also allows for more consistent training experiences across different locations, ensuring standardized skill development.
The data collection capabilities of these systems present another valuable benefit. By tracking trainee performance metrics over time, institutions can gain insights into the effectiveness of their training programs and identify areas for improvement. This data-driven approach to medical education can lead to more efficient allocation of resources and continuous refinement of training methodologies.
In conclusion, while the initial costs of implementing augmented feedback systems for laryngoscope training can be substantial, the long-term benefits in terms of improved training efficiency, enhanced patient safety, and data-driven educational insights suggest a potentially favorable cost-benefit ratio. As technology costs continue to decrease and the systems become more sophisticated, the value proposition of these augmented feedback loops in medical training is likely to become increasingly compelling.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!