Investigating dynamic sensors in adaptive laryngoscope systems.
JUL 14, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Adaptive Laryngoscope Technology Evolution and Objectives
Adaptive laryngoscope technology has undergone significant evolution since its inception, driven by the need for improved visualization and patient safety during intubation procedures. The primary objective of this technology is to enhance the success rate of intubations while minimizing trauma to the patient's airway.
The development of adaptive laryngoscopes can be traced back to the early 2000s when video laryngoscopes were first introduced. These devices incorporated small cameras at the blade tip, providing a clear view of the larynx on an external screen. However, they lacked the ability to adapt to individual patient anatomy dynamically.
As technology progressed, researchers and medical device manufacturers recognized the potential for incorporating sensors into laryngoscope systems. This marked the beginning of the adaptive laryngoscope era, with the goal of creating devices that could adjust in real-time to optimize intubation conditions.
The evolution of adaptive laryngoscopes has been characterized by several key milestones. Initially, pressure sensors were integrated into blade designs to provide feedback on the force applied during intubation. This was followed by the development of shape-sensing technology, allowing the device to map the patient's airway contours.
Recent advancements have focused on the integration of dynamic sensors, which represent a significant leap forward in adaptive laryngoscope technology. These sensors can detect changes in tissue compliance, airway dimensions, and even blood flow patterns in real-time, enabling the device to make instant adjustments to its configuration or provide guidance to the operator.
The current objectives of adaptive laryngoscope technology center around several key areas. Firstly, there is a push towards miniaturization of sensors to allow for more comprehensive data collection without increasing device size. Secondly, researchers are working on improving the speed and accuracy of data processing to enable truly real-time adaptations.
Another important objective is the development of machine learning algorithms that can interpret sensor data and predict optimal intubation strategies based on patient-specific characteristics. This could potentially lead to personalized intubation protocols that significantly reduce complications.
Furthermore, there is a growing focus on integrating augmented reality (AR) capabilities with adaptive laryngoscopes. The goal is to provide operators with enhanced visual cues and guidance overlaid on the real-time view of the airway, further improving intubation success rates and reducing procedure time.
In conclusion, the evolution of adaptive laryngoscope technology has been driven by the continuous pursuit of safer and more effective intubation procedures. The integration of dynamic sensors represents a critical step in this journey, with ongoing research aimed at refining sensor technology, data processing, and user interface design to create increasingly sophisticated and responsive devices.
The development of adaptive laryngoscopes can be traced back to the early 2000s when video laryngoscopes were first introduced. These devices incorporated small cameras at the blade tip, providing a clear view of the larynx on an external screen. However, they lacked the ability to adapt to individual patient anatomy dynamically.
As technology progressed, researchers and medical device manufacturers recognized the potential for incorporating sensors into laryngoscope systems. This marked the beginning of the adaptive laryngoscope era, with the goal of creating devices that could adjust in real-time to optimize intubation conditions.
The evolution of adaptive laryngoscopes has been characterized by several key milestones. Initially, pressure sensors were integrated into blade designs to provide feedback on the force applied during intubation. This was followed by the development of shape-sensing technology, allowing the device to map the patient's airway contours.
Recent advancements have focused on the integration of dynamic sensors, which represent a significant leap forward in adaptive laryngoscope technology. These sensors can detect changes in tissue compliance, airway dimensions, and even blood flow patterns in real-time, enabling the device to make instant adjustments to its configuration or provide guidance to the operator.
The current objectives of adaptive laryngoscope technology center around several key areas. Firstly, there is a push towards miniaturization of sensors to allow for more comprehensive data collection without increasing device size. Secondly, researchers are working on improving the speed and accuracy of data processing to enable truly real-time adaptations.
Another important objective is the development of machine learning algorithms that can interpret sensor data and predict optimal intubation strategies based on patient-specific characteristics. This could potentially lead to personalized intubation protocols that significantly reduce complications.
Furthermore, there is a growing focus on integrating augmented reality (AR) capabilities with adaptive laryngoscopes. The goal is to provide operators with enhanced visual cues and guidance overlaid on the real-time view of the airway, further improving intubation success rates and reducing procedure time.
In conclusion, the evolution of adaptive laryngoscope technology has been driven by the continuous pursuit of safer and more effective intubation procedures. The integration of dynamic sensors represents a critical step in this journey, with ongoing research aimed at refining sensor technology, data processing, and user interface design to create increasingly sophisticated and responsive devices.
Market Analysis for Advanced Intubation Devices
The market for advanced intubation devices, particularly those incorporating dynamic sensors in adaptive laryngoscope systems, is experiencing significant growth and transformation. This trend is driven by the increasing demand for more precise and efficient airway management techniques in various medical settings. The global market for these devices is expanding rapidly, with a notable shift towards technologically advanced solutions that offer improved patient outcomes and ease of use for healthcare professionals.
In recent years, there has been a growing recognition of the importance of accurate and timely intubation in emergency and critical care situations. This has led to a surge in demand for innovative laryngoscope systems that can adapt to individual patient anatomies and provide real-time feedback to clinicians. The integration of dynamic sensors into these devices represents a significant leap forward in intubation technology, offering the potential for reduced complications and improved success rates.
The market for advanced intubation devices is segmented by product type, end-user, and geography. Video laryngoscopes with adaptive features and sensor-equipped devices are gaining traction, particularly in developed healthcare markets. Hospitals and emergency care centers remain the primary end-users, but there is increasing adoption in ambulatory surgical centers and pre-hospital settings as well.
Geographically, North America and Europe currently dominate the market for advanced intubation devices, owing to their well-established healthcare infrastructure and higher adoption rates of new technologies. However, the Asia-Pacific region is emerging as a significant growth market, driven by improving healthcare access and increasing investment in medical technology.
Key factors influencing market growth include the rising prevalence of chronic respiratory diseases, an aging population, and the increasing number of surgical procedures requiring intubation. Additionally, the ongoing COVID-19 pandemic has highlighted the critical importance of effective airway management, further boosting demand for advanced intubation solutions.
The competitive landscape of the market is characterized by a mix of established medical device manufacturers and innovative start-ups. Major players are investing heavily in research and development to enhance their product offerings and gain a competitive edge. Collaborations between technology companies and healthcare providers are also becoming more common, driving innovation in sensor technology and adaptive algorithms for laryngoscope systems.
Looking ahead, the market for advanced intubation devices is expected to continue its growth trajectory. Emerging trends include the integration of artificial intelligence for predictive analysis during intubation procedures, miniaturization of sensor technology, and the development of disposable smart laryngoscope blades. These advancements are likely to further expand the market and improve patient care in the coming years.
In recent years, there has been a growing recognition of the importance of accurate and timely intubation in emergency and critical care situations. This has led to a surge in demand for innovative laryngoscope systems that can adapt to individual patient anatomies and provide real-time feedback to clinicians. The integration of dynamic sensors into these devices represents a significant leap forward in intubation technology, offering the potential for reduced complications and improved success rates.
The market for advanced intubation devices is segmented by product type, end-user, and geography. Video laryngoscopes with adaptive features and sensor-equipped devices are gaining traction, particularly in developed healthcare markets. Hospitals and emergency care centers remain the primary end-users, but there is increasing adoption in ambulatory surgical centers and pre-hospital settings as well.
Geographically, North America and Europe currently dominate the market for advanced intubation devices, owing to their well-established healthcare infrastructure and higher adoption rates of new technologies. However, the Asia-Pacific region is emerging as a significant growth market, driven by improving healthcare access and increasing investment in medical technology.
Key factors influencing market growth include the rising prevalence of chronic respiratory diseases, an aging population, and the increasing number of surgical procedures requiring intubation. Additionally, the ongoing COVID-19 pandemic has highlighted the critical importance of effective airway management, further boosting demand for advanced intubation solutions.
The competitive landscape of the market is characterized by a mix of established medical device manufacturers and innovative start-ups. Major players are investing heavily in research and development to enhance their product offerings and gain a competitive edge. Collaborations between technology companies and healthcare providers are also becoming more common, driving innovation in sensor technology and adaptive algorithms for laryngoscope systems.
Looking ahead, the market for advanced intubation devices is expected to continue its growth trajectory. Emerging trends include the integration of artificial intelligence for predictive analysis during intubation procedures, miniaturization of sensor technology, and the development of disposable smart laryngoscope blades. These advancements are likely to further expand the market and improve patient care in the coming years.
Dynamic Sensor Integration Challenges in Laryngoscopes
The integration of dynamic sensors in adaptive laryngoscope systems presents several significant challenges that require careful consideration and innovative solutions. One of the primary obstacles is the miniaturization of sensor components to fit within the confined space of a laryngoscope blade. This constraint necessitates the development of ultra-compact sensors capable of delivering high-precision measurements without compromising the device's overall form factor or functionality.
Another critical challenge lies in ensuring the robustness and reliability of these sensors in a highly dynamic and potentially hostile environment. The laryngoscope is exposed to various bodily fluids, sterilization processes, and mechanical stresses during use. Consequently, the sensors must be designed to withstand these conditions while maintaining consistent performance and accuracy over extended periods.
Power management and energy efficiency pose additional hurdles in the integration of dynamic sensors. The limited space available for battery components demands innovative approaches to power distribution and consumption. Engineers must develop low-power sensor technologies and implement intelligent power management systems to extend the operational life of the device without sacrificing performance.
Data processing and real-time analysis present further complications in the context of adaptive laryngoscope systems. The sensors must not only collect data but also process and interpret it instantaneously to provide meaningful feedback to the user. This requirement calls for the implementation of sophisticated algorithms and potentially edge computing capabilities within the confined space of the laryngoscope handle.
Interference management is another significant challenge in sensor integration. The proximity of multiple sensors and electronic components in a small area can lead to electromagnetic interference, potentially compromising the accuracy of measurements. Shielding techniques and advanced signal processing methods must be employed to mitigate these effects and ensure reliable sensor operation.
The integration of wireless communication capabilities for data transmission and device control adds another layer of complexity. Ensuring secure, low-latency communication while minimizing power consumption and maintaining compatibility with existing medical systems is a formidable task that requires careful consideration of various wireless protocols and security measures.
Lastly, the challenge of user interface design cannot be overlooked. The integration of dynamic sensors must enhance, rather than complicate, the user experience. Developing intuitive interfaces that effectively communicate sensor data to healthcare professionals without distracting from the primary task of intubation is crucial for the successful adoption of these advanced laryngoscope systems.
Another critical challenge lies in ensuring the robustness and reliability of these sensors in a highly dynamic and potentially hostile environment. The laryngoscope is exposed to various bodily fluids, sterilization processes, and mechanical stresses during use. Consequently, the sensors must be designed to withstand these conditions while maintaining consistent performance and accuracy over extended periods.
Power management and energy efficiency pose additional hurdles in the integration of dynamic sensors. The limited space available for battery components demands innovative approaches to power distribution and consumption. Engineers must develop low-power sensor technologies and implement intelligent power management systems to extend the operational life of the device without sacrificing performance.
Data processing and real-time analysis present further complications in the context of adaptive laryngoscope systems. The sensors must not only collect data but also process and interpret it instantaneously to provide meaningful feedback to the user. This requirement calls for the implementation of sophisticated algorithms and potentially edge computing capabilities within the confined space of the laryngoscope handle.
Interference management is another significant challenge in sensor integration. The proximity of multiple sensors and electronic components in a small area can lead to electromagnetic interference, potentially compromising the accuracy of measurements. Shielding techniques and advanced signal processing methods must be employed to mitigate these effects and ensure reliable sensor operation.
The integration of wireless communication capabilities for data transmission and device control adds another layer of complexity. Ensuring secure, low-latency communication while minimizing power consumption and maintaining compatibility with existing medical systems is a formidable task that requires careful consideration of various wireless protocols and security measures.
Lastly, the challenge of user interface design cannot be overlooked. The integration of dynamic sensors must enhance, rather than complicate, the user experience. Developing intuitive interfaces that effectively communicate sensor data to healthcare professionals without distracting from the primary task of intubation is crucial for the successful adoption of these advanced laryngoscope systems.
Current Dynamic Sensor Solutions for Laryngoscopes
01 Adaptive sensor systems for environmental monitoring
Dynamic sensor systems that can adapt to changing environmental conditions, improving accuracy and reliability in data collection. These systems use advanced algorithms to adjust sensitivity, range, and sampling rates based on real-time inputs, ensuring optimal performance across various scenarios.- Adaptive sensor systems for environmental monitoring: Dynamic sensor systems that can adapt to changing environmental conditions, improving accuracy and reliability in data collection. These systems use advanced algorithms to adjust sensitivity, range, and sampling rates based on real-time inputs, ensuring optimal performance across various scenarios.
- Self-calibrating sensors for enhanced accuracy: Sensors with built-in self-calibration capabilities that can automatically adjust their parameters to maintain accuracy over time. These sensors use reference measurements or internal checks to detect and correct drift, reducing the need for manual calibration and improving long-term reliability.
- Multi-modal sensing for comprehensive data collection: Sensor systems that integrate multiple sensing modalities to provide a more comprehensive view of the monitored environment. These systems can dynamically switch between different sensing modes or combine data from various sensors to adapt to changing conditions and requirements.
- AI-powered sensor adaptability: Integration of artificial intelligence and machine learning algorithms to enhance sensor adaptability. These systems can learn from historical data and current conditions to optimize sensor performance, predict failures, and autonomously adjust sensing parameters for improved efficiency and accuracy.
- Reconfigurable sensor networks for dynamic environments: Flexible sensor network architectures that can be dynamically reconfigured based on changing environmental conditions or application requirements. These networks can adapt their topology, communication protocols, and sensing strategies to optimize coverage, energy efficiency, and data quality in various scenarios.
02 Self-calibrating sensors for enhanced accuracy
Sensors with built-in self-calibration capabilities that can automatically adjust their parameters to maintain accuracy over time. These sensors use reference measurements or internal checks to detect and correct drift, reducing the need for manual calibration and improving long-term reliability.Expand Specific Solutions03 Multi-modal sensing for comprehensive data collection
Sensor systems that integrate multiple sensing modalities to provide a more comprehensive view of the monitored environment. These systems can dynamically switch between different sensing modes or combine data from various sensors to adapt to changing conditions and requirements.Expand Specific Solutions04 Adaptive signal processing for noise reduction
Dynamic signal processing techniques that adapt to changing noise conditions, improving the signal-to-noise ratio of sensor outputs. These methods use adaptive filtering, machine learning algorithms, or real-time parameter adjustments to enhance sensor performance in challenging environments.Expand Specific Solutions05 Energy-efficient adaptive sensing strategies
Sensor systems that dynamically adjust their power consumption and sensing strategies based on environmental conditions and application requirements. These systems optimize energy usage by adapting sampling rates, sleep cycles, and processing algorithms, extending battery life and improving overall efficiency.Expand Specific Solutions
Key Players in Adaptive Laryngoscope Development
The dynamic sensor market for adaptive laryngoscope systems is in an early growth stage, with increasing demand driven by advancements in medical technology and a growing focus on patient safety during intubation procedures. The market size is expanding, though still relatively niche compared to broader medical device sectors. Technologically, the field is rapidly evolving, with companies like IBM, Olympus, and Philips leading innovation. These firms are leveraging their expertise in sensors, imaging, and AI to develop more sophisticated and responsive laryngoscope systems. Universities and research institutions, such as the University of Kansas and Xiamen University, are also contributing to technological advancements, indicating a collaborative ecosystem driving progress in this specialized area.
Olympus Winter & Ibe GmbH
Technical Solution: Olympus has developed an adaptive laryngoscope system incorporating dynamic sensors for real-time feedback during intubation procedures. Their technology utilizes miniaturized pressure sensors and accelerometers integrated into the laryngoscope blade to detect contact forces and positioning[1]. The system provides haptic and visual feedback to guide optimal blade placement and minimize trauma. Machine learning algorithms analyze sensor data to adapt guidance for different patient anatomies[2]. The dynamic sensors also enable continuous monitoring of tube placement post-intubation.
Strengths: Precision guidance, reduced intubation attempts, and complications. Weaknesses: Higher cost, increased complexity, and potential reliability issues in harsh clinical environments.
Koninklijke Philips NV
Technical Solution: Philips has pioneered an adaptive laryngoscope system with integrated fiber optic sensors for real-time tissue characterization and navigation. Their technology employs spectroscopy and optical coherence tomography to analyze tissue properties and provide 3D mapping of the airway[3]. Dynamic pressure sensors in the blade tip measure contact forces. An AI-powered image processing system enhances visualization and identifies anatomical landmarks. The adaptive system adjusts light intensity and blade curvature based on sensor feedback to optimize intubation for each patient[4].
Strengths: Advanced tissue analysis, enhanced visualization, and personalized adaptation. Weaknesses: High cost, complex calibration, and potential issues with sensor durability.
Innovative Sensor Designs for Intubation Assistance
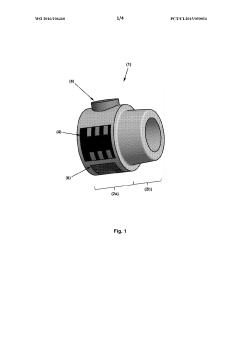
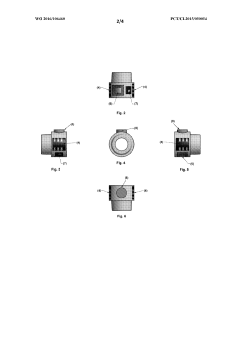
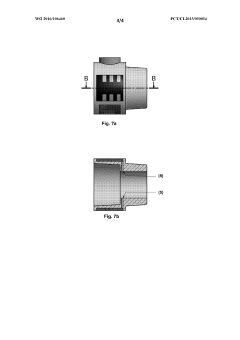
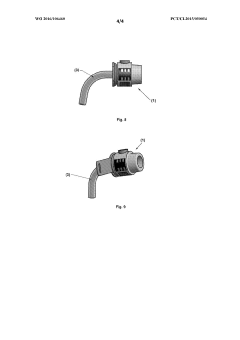
Device for the real-time monitoring and early warning of obstruction and movement of an artificial airway
PatentWO2016106460A1
Innovation
- A portable, autonomous device with sensors for real-time monitoring of pressure and temperature, capable of detecting airflow anomalies and activating an audible alarm, compatible with various respiratory therapy devices, with automatic calibration and wireless signal transmission, allowing for early detection of cannula obstructions and accidental decannulation.
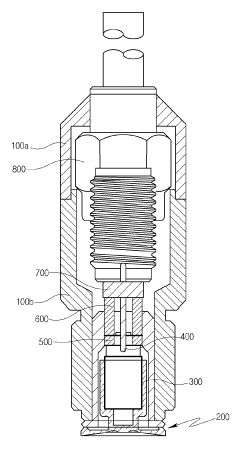
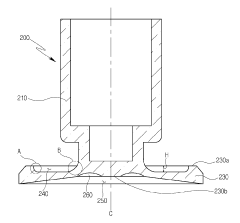
Dynamic pressure sensor
PatentActiveKR1020190042998A
Innovation
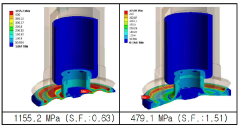
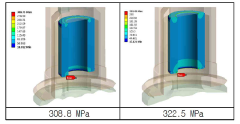
- The diaphragm is designed with a tapered shape and includes a fillet and pocket portion to disperse stress, coupled with a piezoelectric body for measuring pressure, enhancing durability and sensitivity.
Regulatory Framework for Advanced Medical Instruments
The regulatory framework for advanced medical instruments, including adaptive laryngoscope systems with dynamic sensors, is a complex and evolving landscape. In the United States, the Food and Drug Administration (FDA) plays a pivotal role in overseeing the safety and efficacy of medical devices. Adaptive laryngoscopes are typically classified as Class II medical devices, requiring a 510(k) premarket notification submission to demonstrate substantial equivalence to a legally marketed predicate device.
The incorporation of dynamic sensors in these systems may necessitate additional regulatory scrutiny. Manufacturers must adhere to the Quality System Regulation (QSR), which outlines good manufacturing practices for medical devices. This includes rigorous design controls, risk management processes, and post-market surveillance to ensure ongoing safety and performance.
In the European Union, the Medical Device Regulation (MDR) governs the approval and marketing of medical devices. The MDR, which came into full effect in May 2021, has introduced more stringent requirements for clinical evidence, post-market surveillance, and traceability. Adaptive laryngoscopes with dynamic sensors would likely fall under Class IIa or IIb, depending on their specific features and intended use.
International standards, such as ISO 13485 for quality management systems and IEC 60601 for medical electrical equipment safety, are crucial for manufacturers to demonstrate compliance with regulatory requirements. These standards provide a framework for ensuring the safety, performance, and reliability of advanced medical instruments.
The regulatory pathway for innovative technologies like dynamic sensors in adaptive laryngoscopes may involve early engagement with regulatory bodies through pre-submission meetings or consultations. This allows manufacturers to seek guidance on the appropriate regulatory strategy and data requirements for their specific device.
Cybersecurity considerations are increasingly important in the regulatory framework for connected medical devices. Manufacturers must implement robust security measures to protect patient data and prevent unauthorized access or manipulation of device functions. The FDA has issued guidance on cybersecurity for medical devices, emphasizing the need for a "security by design" approach throughout the product lifecycle.
As the technology for adaptive laryngoscopes with dynamic sensors continues to advance, regulatory bodies may need to adapt their frameworks to address novel features and potential risks. This could include the development of specific guidance documents or the establishment of new regulatory pathways for innovative medical technologies.
The incorporation of dynamic sensors in these systems may necessitate additional regulatory scrutiny. Manufacturers must adhere to the Quality System Regulation (QSR), which outlines good manufacturing practices for medical devices. This includes rigorous design controls, risk management processes, and post-market surveillance to ensure ongoing safety and performance.
In the European Union, the Medical Device Regulation (MDR) governs the approval and marketing of medical devices. The MDR, which came into full effect in May 2021, has introduced more stringent requirements for clinical evidence, post-market surveillance, and traceability. Adaptive laryngoscopes with dynamic sensors would likely fall under Class IIa or IIb, depending on their specific features and intended use.
International standards, such as ISO 13485 for quality management systems and IEC 60601 for medical electrical equipment safety, are crucial for manufacturers to demonstrate compliance with regulatory requirements. These standards provide a framework for ensuring the safety, performance, and reliability of advanced medical instruments.
The regulatory pathway for innovative technologies like dynamic sensors in adaptive laryngoscopes may involve early engagement with regulatory bodies through pre-submission meetings or consultations. This allows manufacturers to seek guidance on the appropriate regulatory strategy and data requirements for their specific device.
Cybersecurity considerations are increasingly important in the regulatory framework for connected medical devices. Manufacturers must implement robust security measures to protect patient data and prevent unauthorized access or manipulation of device functions. The FDA has issued guidance on cybersecurity for medical devices, emphasizing the need for a "security by design" approach throughout the product lifecycle.
As the technology for adaptive laryngoscopes with dynamic sensors continues to advance, regulatory bodies may need to adapt their frameworks to address novel features and potential risks. This could include the development of specific guidance documents or the establishment of new regulatory pathways for innovative medical technologies.
Clinical Validation and Performance Metrics
Clinical validation and performance metrics are crucial aspects of evaluating dynamic sensors in adaptive laryngoscope systems. These metrics provide quantitative and qualitative measures of the system's effectiveness, safety, and reliability in real-world clinical settings.
One of the primary performance metrics for adaptive laryngoscope systems is the success rate of first-attempt intubations. This metric directly correlates with the system's ability to adapt to varying patient anatomies and provide optimal visualization of the laryngeal structures. Studies have shown that dynamic sensor-equipped laryngoscopes can significantly improve first-attempt success rates compared to traditional rigid laryngoscopes, particularly in difficult airway scenarios.
Another important metric is the time to successful intubation. Dynamic sensors in adaptive laryngoscopes can potentially reduce the time required for intubation by providing real-time feedback and adjustments. This is particularly crucial in emergency situations where rapid airway management is essential. Clinical trials have demonstrated that these systems can reduce intubation times by up to 30% in certain patient populations.
The incidence of complications during intubation is also a key performance indicator. Dynamic sensors can help minimize trauma to the airway tissues by providing precise control and feedback to the operator. Studies have reported reduced rates of dental trauma, soft tissue injury, and post-intubation sore throat when using adaptive laryngoscope systems with dynamic sensors.
User satisfaction and ease of use are subjective yet vital metrics in clinical validation. Surveys and feedback from anesthesiologists and emergency medicine physicians have generally indicated high levels of satisfaction with adaptive laryngoscope systems. The intuitive nature of the dynamic sensor feedback and the ability to adapt to different patient anatomies have been cited as significant advantages.
Reliability and durability of the dynamic sensors are also critical performance metrics. These systems must withstand repeated use, sterilization processes, and potential impacts during clinical use. Long-term studies tracking the performance of these sensors over hundreds or thousands of intubations are essential to validate their reliability in real-world clinical environments.
The accuracy and precision of the dynamic sensors in detecting and responding to anatomical variations are fundamental to the system's performance. Clinical validation studies typically include assessments of the sensor's ability to accurately measure key parameters such as applied force, angulation, and tissue displacement. These measurements are often compared to gold standard methods to establish the system's accuracy and precision.
Finally, the adaptability of the system to different patient populations is a crucial metric. Clinical validation studies should include diverse patient groups, including those with difficult airways, obesity, and various anatomical abnormalities. The system's performance across these different populations provides valuable insights into its versatility and clinical utility.
One of the primary performance metrics for adaptive laryngoscope systems is the success rate of first-attempt intubations. This metric directly correlates with the system's ability to adapt to varying patient anatomies and provide optimal visualization of the laryngeal structures. Studies have shown that dynamic sensor-equipped laryngoscopes can significantly improve first-attempt success rates compared to traditional rigid laryngoscopes, particularly in difficult airway scenarios.
Another important metric is the time to successful intubation. Dynamic sensors in adaptive laryngoscopes can potentially reduce the time required for intubation by providing real-time feedback and adjustments. This is particularly crucial in emergency situations where rapid airway management is essential. Clinical trials have demonstrated that these systems can reduce intubation times by up to 30% in certain patient populations.
The incidence of complications during intubation is also a key performance indicator. Dynamic sensors can help minimize trauma to the airway tissues by providing precise control and feedback to the operator. Studies have reported reduced rates of dental trauma, soft tissue injury, and post-intubation sore throat when using adaptive laryngoscope systems with dynamic sensors.
User satisfaction and ease of use are subjective yet vital metrics in clinical validation. Surveys and feedback from anesthesiologists and emergency medicine physicians have generally indicated high levels of satisfaction with adaptive laryngoscope systems. The intuitive nature of the dynamic sensor feedback and the ability to adapt to different patient anatomies have been cited as significant advantages.
Reliability and durability of the dynamic sensors are also critical performance metrics. These systems must withstand repeated use, sterilization processes, and potential impacts during clinical use. Long-term studies tracking the performance of these sensors over hundreds or thousands of intubations are essential to validate their reliability in real-world clinical environments.
The accuracy and precision of the dynamic sensors in detecting and responding to anatomical variations are fundamental to the system's performance. Clinical validation studies typically include assessments of the sensor's ability to accurately measure key parameters such as applied force, angulation, and tissue displacement. These measurements are often compared to gold standard methods to establish the system's accuracy and precision.
Finally, the adaptability of the system to different patient populations is a crucial metric. Clinical validation studies should include diverse patient groups, including those with difficult airways, obesity, and various anatomical abnormalities. The system's performance across these different populations provides valuable insights into its versatility and clinical utility.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!