How to Test Autoclave Vacuum Integrity Using Pressure Decay
SEP 2, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Autoclave Vacuum Testing Background and Objectives
Autoclave sterilization has been a cornerstone of medical and industrial safety protocols since its development in the late 19th century. The process relies on high-pressure saturated steam to eliminate microorganisms and ensure sterility of medical instruments, laboratory equipment, and pharmaceutical products. A critical component of this sterilization process is the vacuum system, which facilitates steam penetration into complex instruments and removes air that could otherwise create cold spots where sterilization might fail.
Pressure decay testing has emerged as a reliable method for verifying autoclave vacuum integrity, evolving from earlier leak detection methodologies used in various industrial applications. This testing approach measures the rate at which pressure changes within a sealed system, providing quantitative data on potential leaks that could compromise the sterilization process. The technique gained prominence in the 1980s and has since become increasingly sophisticated with the integration of digital monitoring systems and automated testing protocols.
The primary objective of autoclave vacuum integrity testing using pressure decay is to ensure that sterilization cycles maintain their efficacy by confirming the vacuum system's ability to achieve and maintain required negative pressure levels. This verification is essential for compliance with regulatory standards such as ISO 17665 and EN 285, which govern sterilization processes for medical devices and healthcare products.
Current technological trends in this field include the development of more sensitive pressure transducers capable of detecting minute leaks, integration of IoT capabilities for remote monitoring and data logging, and the implementation of machine learning algorithms to predict potential vacuum system failures before they occur. These advancements aim to enhance both the reliability and efficiency of sterilization processes across various industries.
The technical goals for pressure decay testing in autoclave systems include establishing standardized testing protocols that can be universally applied across different autoclave models and sizes, developing real-time monitoring systems that can detect vacuum integrity issues during actual sterilization cycles, and creating more energy-efficient testing methodologies that maintain accuracy while reducing operational costs.
As healthcare facilities and manufacturing environments face increasing pressure to ensure product safety while optimizing operational efficiency, the importance of reliable vacuum integrity testing continues to grow. The evolution of pressure decay testing represents a critical technological pathway for meeting these dual demands, positioning it as an essential component in the broader landscape of sterilization technology advancement.
Pressure decay testing has emerged as a reliable method for verifying autoclave vacuum integrity, evolving from earlier leak detection methodologies used in various industrial applications. This testing approach measures the rate at which pressure changes within a sealed system, providing quantitative data on potential leaks that could compromise the sterilization process. The technique gained prominence in the 1980s and has since become increasingly sophisticated with the integration of digital monitoring systems and automated testing protocols.
The primary objective of autoclave vacuum integrity testing using pressure decay is to ensure that sterilization cycles maintain their efficacy by confirming the vacuum system's ability to achieve and maintain required negative pressure levels. This verification is essential for compliance with regulatory standards such as ISO 17665 and EN 285, which govern sterilization processes for medical devices and healthcare products.
Current technological trends in this field include the development of more sensitive pressure transducers capable of detecting minute leaks, integration of IoT capabilities for remote monitoring and data logging, and the implementation of machine learning algorithms to predict potential vacuum system failures before they occur. These advancements aim to enhance both the reliability and efficiency of sterilization processes across various industries.
The technical goals for pressure decay testing in autoclave systems include establishing standardized testing protocols that can be universally applied across different autoclave models and sizes, developing real-time monitoring systems that can detect vacuum integrity issues during actual sterilization cycles, and creating more energy-efficient testing methodologies that maintain accuracy while reducing operational costs.
As healthcare facilities and manufacturing environments face increasing pressure to ensure product safety while optimizing operational efficiency, the importance of reliable vacuum integrity testing continues to grow. The evolution of pressure decay testing represents a critical technological pathway for meeting these dual demands, positioning it as an essential component in the broader landscape of sterilization technology advancement.
Market Demand for Reliable Sterilization Validation
The global sterilization market has witnessed substantial growth in recent years, driven primarily by increasing healthcare expenditures, rising surgical procedures, and growing concerns about healthcare-associated infections. The market for sterilization equipment and validation services was valued at approximately $7.5 billion in 2022 and is projected to reach $12.3 billion by 2028, representing a compound annual growth rate of 8.6%.
Within this broader market, autoclave sterilization remains a cornerstone technology across multiple industries including healthcare, pharmaceuticals, biotechnology, and food processing. The demand for reliable sterilization validation methods, particularly for autoclave systems, has intensified due to stringent regulatory requirements and quality assurance standards.
Healthcare facilities worldwide are facing mounting pressure to ensure absolute sterility of medical devices and equipment. According to the World Health Organization, healthcare-associated infections affect hundreds of millions of patients globally each year, with a significant portion attributable to inadequately sterilized equipment. This has created an urgent market need for dependable validation methods like pressure decay testing for autoclave vacuum integrity.
The pharmaceutical and biotechnology sectors represent another significant market segment driving demand for reliable sterilization validation. With the global pharmaceutical market exceeding $1.4 trillion, manufacturers must adhere to strict Good Manufacturing Practice (GMP) guidelines that mandate thorough validation of sterilization processes. Pressure decay testing offers a quantifiable, reproducible method that aligns with these regulatory expectations.
Contract sterilization services, a rapidly growing segment valued at $3.2 billion globally, also require robust validation protocols to ensure service quality and regulatory compliance. These service providers are increasingly adopting advanced validation technologies to differentiate themselves in a competitive marketplace.
Regional analysis reveals particularly strong demand growth in emerging economies across Asia-Pacific and Latin America, where healthcare infrastructure development and increasing manufacturing capabilities are creating new markets for sterilization technologies. Meanwhile, in established markets like North America and Europe, the focus has shifted toward more sophisticated validation methods that offer greater precision and documentation capabilities.
Industry surveys indicate that end-users are willing to invest in advanced validation technologies that can reduce operational costs through early detection of sterilization failures. The economic impact of failed sterilization—including product recalls, regulatory penalties, and reputation damage—far outweighs the investment in comprehensive validation systems like pressure decay testing for autoclave vacuum integrity.
Within this broader market, autoclave sterilization remains a cornerstone technology across multiple industries including healthcare, pharmaceuticals, biotechnology, and food processing. The demand for reliable sterilization validation methods, particularly for autoclave systems, has intensified due to stringent regulatory requirements and quality assurance standards.
Healthcare facilities worldwide are facing mounting pressure to ensure absolute sterility of medical devices and equipment. According to the World Health Organization, healthcare-associated infections affect hundreds of millions of patients globally each year, with a significant portion attributable to inadequately sterilized equipment. This has created an urgent market need for dependable validation methods like pressure decay testing for autoclave vacuum integrity.
The pharmaceutical and biotechnology sectors represent another significant market segment driving demand for reliable sterilization validation. With the global pharmaceutical market exceeding $1.4 trillion, manufacturers must adhere to strict Good Manufacturing Practice (GMP) guidelines that mandate thorough validation of sterilization processes. Pressure decay testing offers a quantifiable, reproducible method that aligns with these regulatory expectations.
Contract sterilization services, a rapidly growing segment valued at $3.2 billion globally, also require robust validation protocols to ensure service quality and regulatory compliance. These service providers are increasingly adopting advanced validation technologies to differentiate themselves in a competitive marketplace.
Regional analysis reveals particularly strong demand growth in emerging economies across Asia-Pacific and Latin America, where healthcare infrastructure development and increasing manufacturing capabilities are creating new markets for sterilization technologies. Meanwhile, in established markets like North America and Europe, the focus has shifted toward more sophisticated validation methods that offer greater precision and documentation capabilities.
Industry surveys indicate that end-users are willing to invest in advanced validation technologies that can reduce operational costs through early detection of sterilization failures. The economic impact of failed sterilization—including product recalls, regulatory penalties, and reputation damage—far outweighs the investment in comprehensive validation systems like pressure decay testing for autoclave vacuum integrity.
Current Challenges in Autoclave Vacuum Integrity Testing
Despite significant advancements in autoclave technology, vacuum integrity testing using pressure decay methods continues to face several critical challenges that impact reliability, efficiency, and standardization across industries. The traditional pressure decay test, while conceptually straightforward, encounters numerous practical obstacles during implementation in modern manufacturing environments.
One primary challenge is the detection sensitivity limitations when dealing with extremely small leaks. Current pressure decay testing methods struggle to consistently identify microleaks that may still compromise sterilization efficacy but produce minimal pressure changes over standard test durations. This sensitivity threshold becomes particularly problematic in pharmaceutical and medical device manufacturing where absolute sterility assurance is non-negotiable.
Environmental factors significantly complicate test reliability. Temperature fluctuations during testing can cause pressure variations unrelated to actual leaks, leading to false positives or negatives. Even minor ambient temperature changes of 1-2°C can mask or mimic leak signatures, especially in larger autoclave chambers where thermal equilibrium is difficult to maintain throughout the testing period.
Calibration and standardization issues persist across different equipment manufacturers and industries. The lack of universally accepted calibration protocols means that pressure decay test results may not be directly comparable between different facilities or even between different autoclave units within the same facility. This inconsistency complicates validation processes and regulatory compliance efforts.
Test duration presents another significant challenge. Conventional pressure decay tests require extended periods (often 30 minutes or more) to achieve meaningful results, particularly when testing for smaller leaks. This extended testing time creates production bottlenecks and reduces overall equipment effectiveness in high-throughput manufacturing environments.
The interpretation of test results remains largely subjective and operator-dependent. Without sophisticated data analysis tools, determining whether a specific pressure decay rate indicates a problematic leak requires significant operator experience and judgment. This subjectivity introduces variability in test outcomes and complicates quality assurance processes.
Digital integration limitations further hinder progress in this field. Many autoclave systems still utilize analog pressure measurement systems or have limited data logging capabilities, making it difficult to implement advanced statistical process control or trend analysis that could improve leak detection accuracy and predictive maintenance.
Finally, regulatory requirements continue to evolve while testing methodologies remain relatively static. This growing disconnect creates compliance challenges for manufacturers, particularly those operating in multiple jurisdictions with varying standards for vacuum integrity validation and documentation.
One primary challenge is the detection sensitivity limitations when dealing with extremely small leaks. Current pressure decay testing methods struggle to consistently identify microleaks that may still compromise sterilization efficacy but produce minimal pressure changes over standard test durations. This sensitivity threshold becomes particularly problematic in pharmaceutical and medical device manufacturing where absolute sterility assurance is non-negotiable.
Environmental factors significantly complicate test reliability. Temperature fluctuations during testing can cause pressure variations unrelated to actual leaks, leading to false positives or negatives. Even minor ambient temperature changes of 1-2°C can mask or mimic leak signatures, especially in larger autoclave chambers where thermal equilibrium is difficult to maintain throughout the testing period.
Calibration and standardization issues persist across different equipment manufacturers and industries. The lack of universally accepted calibration protocols means that pressure decay test results may not be directly comparable between different facilities or even between different autoclave units within the same facility. This inconsistency complicates validation processes and regulatory compliance efforts.
Test duration presents another significant challenge. Conventional pressure decay tests require extended periods (often 30 minutes or more) to achieve meaningful results, particularly when testing for smaller leaks. This extended testing time creates production bottlenecks and reduces overall equipment effectiveness in high-throughput manufacturing environments.
The interpretation of test results remains largely subjective and operator-dependent. Without sophisticated data analysis tools, determining whether a specific pressure decay rate indicates a problematic leak requires significant operator experience and judgment. This subjectivity introduces variability in test outcomes and complicates quality assurance processes.
Digital integration limitations further hinder progress in this field. Many autoclave systems still utilize analog pressure measurement systems or have limited data logging capabilities, making it difficult to implement advanced statistical process control or trend analysis that could improve leak detection accuracy and predictive maintenance.
Finally, regulatory requirements continue to evolve while testing methodologies remain relatively static. This growing disconnect creates compliance challenges for manufacturers, particularly those operating in multiple jurisdictions with varying standards for vacuum integrity validation and documentation.
Leading Manufacturers and Testing Equipment Providers
The autoclave vacuum integrity testing market is currently in a growth phase, with increasing demand driven by stringent regulatory requirements in pharmaceutical and medical device industries. The market size is expanding steadily, estimated to reach significant value due to growing emphasis on sterilization validation processes. Technologically, pressure decay testing has reached moderate maturity, with established players like EMD Millipore Corp., Baxter International, and Shinva Medical Instrument leading innovation. Companies such as Packaging Technologies & Inspection LLC and Olympus Corp. are advancing testing methodologies with automated solutions, while pharmaceutical equipment manufacturers like Truking Technology and DuPont are integrating these technologies into their sterilization systems. The competitive landscape shows a mix of specialized testing equipment providers and diversified medical/pharmaceutical equipment manufacturers competing for market share.
EMD Millipore Corp.
Technical Solution: EMD Millipore has developed a sophisticated pressure decay testing methodology for autoclave vacuum integrity verification that focuses on applications in biopharmaceutical manufacturing. Their system employs high-precision digital pressure transducers with accuracy of ±0.1% of reading, connected to a dedicated microprocessor control unit. The testing protocol begins with evacuation of the autoclave chamber to a predetermined vacuum level (typically 50-100 mbar absolute), followed by isolation and monitoring for pressure increases over a specified time period. Their proprietary algorithm incorporates barometric pressure compensation to account for ambient pressure fluctuations during testing. The system features automated pass/fail determination based on user-defined acceptance criteria, with pressure rise rates typically limited to 1.3 mbar/minute for a standard 30-minute test. EMD Millipore's solution includes comprehensive data management capabilities with electronic signatures and audit trails compliant with GMP requirements.
Strengths: Specifically optimized for biopharmaceutical applications; excellent reproducibility with barometric compensation; comprehensive data management for regulatory compliance. Weaknesses: Relatively long test cycles impact production throughput; requires careful environmental control for optimal performance; higher cost compared to basic testing systems.
Baxter International, Inc.
Technical Solution: Baxter International has developed an advanced pressure decay testing system specifically for autoclave vacuum integrity verification. Their approach utilizes differential pressure sensors that can detect minute changes in pressure over time, with sensitivity down to 0.001 psi. The system employs a two-phase testing protocol: first establishing a baseline vacuum level in the autoclave chamber, then isolating the system and monitoring pressure changes over a predetermined period (typically 15-30 minutes). Their proprietary algorithm accounts for thermal effects during cooling phases, which traditionally cause false readings. The system includes automated data logging capabilities that integrate with manufacturing execution systems (MES) for complete batch documentation and compliance with FDA 21 CFR Part 11 requirements for electronic records.
Strengths: Exceptional sensitivity for detecting even microscopic leaks; automated documentation for regulatory compliance; thermal compensation algorithms reduce false positives. Weaknesses: Higher initial investment compared to simpler systems; requires more frequent calibration of sensitive pressure transducers; more complex validation protocols.
Critical Parameters and Technical Specifications Analysis
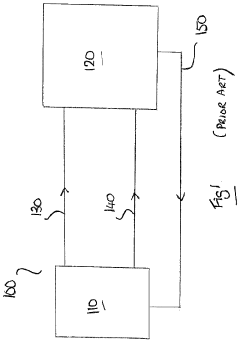
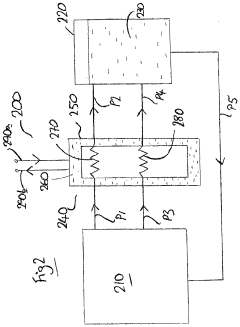
Autoclave system and method
PatentActiveUS20200147568A1
Innovation
- A heat exchanger is interposed between the autoclave vessel and the external support system, utilizing thermal exchange conduits and a medium to cool and manage both leaching and venting fluids, reducing their temperature and pressure before reintroduction, while also pre-heating the leaching fluid for efficient operation.
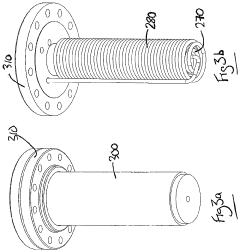
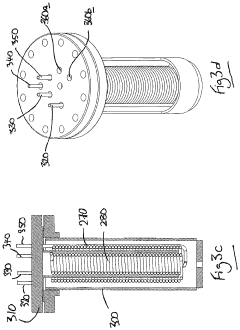
High pressure autoclave
PatentInactiveEP0099443A2
Innovation
- The pressure vessel is equipped with a skirt and spacer elements, such as steel balls, between its inner and outer walls, allowing the outer shell to absorb heat transfer medium and reducing the pressure vessel's structural requirements, with the spacer elements ensuring efficient pressure transmission and stress distribution.
Regulatory Compliance and Industry Standards
Autoclave vacuum integrity testing is governed by a comprehensive framework of regulatory requirements and industry standards that ensure sterilization processes meet established safety and efficacy benchmarks. The FDA's Quality System Regulation (21 CFR Part 820) mandates that medical device manufacturers validate their sterilization processes, including the performance verification of autoclaves. Specifically, vacuum integrity testing using pressure decay methods must comply with these regulations to ensure patient safety and product sterility.
ISO 17665-1:2006 provides detailed specifications for the development, validation, and routine control of moist heat sterilization processes for medical devices. This standard explicitly addresses the importance of vacuum integrity in achieving proper air removal during the sterilization cycle. The pressure decay test methodology must align with these requirements, ensuring that test parameters, acceptance criteria, and documentation practices meet international standards.
European standards, particularly EN 285 for large steam sterilizers, establish specific requirements for vacuum leak tests. This standard stipulates that the pressure rise during a vacuum leak test should not exceed 13 mbar (1.3 kPa) over a 10-minute period after achieving a pressure of 7 kPa absolute. These precise parameters serve as critical benchmarks for pressure decay testing protocols.
The Association for the Advancement of Medical Instrumentation (AAMI) provides additional guidance through AAMI ST79, which outlines comprehensive recommendations for steam sterilization and sterility assurance in healthcare facilities. This document includes specific protocols for vacuum leak testing, including frequency requirements and acceptance criteria that vary based on autoclave type and application.
Industry best practices recommend daily vacuum leak testing before the first sterilization cycle of the day, with documentation of test results as part of quality assurance records. These records are subject to regulatory inspection and audit, making standardized testing procedures essential for compliance.
For pharmaceutical applications, USP <797> and <800> guidelines contain additional requirements related to sterile compounding environments, which may influence autoclave validation requirements. Similarly, in laboratory settings, compliance with Good Laboratory Practice (GLP) regulations necessitates adherence to validated sterilization processes with documented vacuum integrity verification.
The implementation of pressure decay testing must also consider regional variations in regulatory requirements, particularly when equipment is intended for global markets. Documentation systems must be designed to demonstrate compliance with all applicable standards while maintaining traceability throughout the equipment lifecycle.
ISO 17665-1:2006 provides detailed specifications for the development, validation, and routine control of moist heat sterilization processes for medical devices. This standard explicitly addresses the importance of vacuum integrity in achieving proper air removal during the sterilization cycle. The pressure decay test methodology must align with these requirements, ensuring that test parameters, acceptance criteria, and documentation practices meet international standards.
European standards, particularly EN 285 for large steam sterilizers, establish specific requirements for vacuum leak tests. This standard stipulates that the pressure rise during a vacuum leak test should not exceed 13 mbar (1.3 kPa) over a 10-minute period after achieving a pressure of 7 kPa absolute. These precise parameters serve as critical benchmarks for pressure decay testing protocols.
The Association for the Advancement of Medical Instrumentation (AAMI) provides additional guidance through AAMI ST79, which outlines comprehensive recommendations for steam sterilization and sterility assurance in healthcare facilities. This document includes specific protocols for vacuum leak testing, including frequency requirements and acceptance criteria that vary based on autoclave type and application.
Industry best practices recommend daily vacuum leak testing before the first sterilization cycle of the day, with documentation of test results as part of quality assurance records. These records are subject to regulatory inspection and audit, making standardized testing procedures essential for compliance.
For pharmaceutical applications, USP <797> and <800> guidelines contain additional requirements related to sterile compounding environments, which may influence autoclave validation requirements. Similarly, in laboratory settings, compliance with Good Laboratory Practice (GLP) regulations necessitates adherence to validated sterilization processes with documented vacuum integrity verification.
The implementation of pressure decay testing must also consider regional variations in regulatory requirements, particularly when equipment is intended for global markets. Documentation systems must be designed to demonstrate compliance with all applicable standards while maintaining traceability throughout the equipment lifecycle.
Risk Management in Sterilization Process Validation
Risk management is a critical component of sterilization process validation, particularly when employing autoclaves with vacuum systems. The pressure decay test for vacuum integrity represents a key risk control measure that helps ensure sterilization efficacy and patient safety. Effective risk management begins with comprehensive hazard identification, where potential failure modes of autoclave vacuum systems are systematically cataloged, including leaks, pump malfunctions, and control system errors.
Risk assessment methodologies such as Failure Mode and Effects Analysis (FMEA) and Fault Tree Analysis (FTA) provide structured approaches to evaluate the likelihood and severity of vacuum system failures. These tools help prioritize risks based on their potential impact on sterilization outcomes. For instance, a minor vacuum leak might be assigned a higher risk priority number than a pressure gauge calibration issue due to its direct impact on sterilization efficacy.
Establishing acceptance criteria for pressure decay tests constitutes a fundamental risk control measure. These criteria must be scientifically justified and aligned with regulatory expectations, typically allowing for no more than 1.3 mbar/minute of pressure rise during the test period. The frequency of testing represents another risk management decision, with daily tests before the first load being common practice in healthcare settings, while pharmaceutical manufacturers might implement continuous monitoring systems.
Documentation plays a crucial role in risk management, serving as evidence of compliance and facilitating continuous improvement. Records of pressure decay test results, along with any deviations and corrective actions, should be maintained according to regulatory requirements. These records enable trend analysis that can identify gradual deterioration in vacuum system performance before critical failures occur.
Training programs for personnel conducting pressure decay tests represent another risk mitigation strategy. Operators must understand not only the technical aspects of performing the test but also the significance of results and appropriate responses to test failures. This human factors approach recognizes that even well-designed technical systems depend on proper implementation by trained personnel.
Periodic validation of the pressure decay test methodology itself constitutes a meta-level risk management activity. This includes challenging the test with known leaks to verify its sensitivity and comparing results with alternative methods such as helium leak detection to ensure the test remains fit for purpose as equipment ages.
Integration of pressure decay testing into a broader quality management system ensures that identified risks are systematically addressed through appropriate corrective and preventive actions (CAPA). This closed-loop approach transforms risk management from a static assessment into a dynamic process of continuous improvement in sterilization validation.
Risk assessment methodologies such as Failure Mode and Effects Analysis (FMEA) and Fault Tree Analysis (FTA) provide structured approaches to evaluate the likelihood and severity of vacuum system failures. These tools help prioritize risks based on their potential impact on sterilization outcomes. For instance, a minor vacuum leak might be assigned a higher risk priority number than a pressure gauge calibration issue due to its direct impact on sterilization efficacy.
Establishing acceptance criteria for pressure decay tests constitutes a fundamental risk control measure. These criteria must be scientifically justified and aligned with regulatory expectations, typically allowing for no more than 1.3 mbar/minute of pressure rise during the test period. The frequency of testing represents another risk management decision, with daily tests before the first load being common practice in healthcare settings, while pharmaceutical manufacturers might implement continuous monitoring systems.
Documentation plays a crucial role in risk management, serving as evidence of compliance and facilitating continuous improvement. Records of pressure decay test results, along with any deviations and corrective actions, should be maintained according to regulatory requirements. These records enable trend analysis that can identify gradual deterioration in vacuum system performance before critical failures occur.
Training programs for personnel conducting pressure decay tests represent another risk mitigation strategy. Operators must understand not only the technical aspects of performing the test but also the significance of results and appropriate responses to test failures. This human factors approach recognizes that even well-designed technical systems depend on proper implementation by trained personnel.
Periodic validation of the pressure decay test methodology itself constitutes a meta-level risk management activity. This includes challenging the test with known leaks to verify its sensitivity and comparing results with alternative methods such as helium leak detection to ensure the test remains fit for purpose as equipment ages.
Integration of pressure decay testing into a broader quality management system ensures that identified risks are systematically addressed through appropriate corrective and preventive actions (CAPA). This closed-loop approach transforms risk management from a static assessment into a dynamic process of continuous improvement in sterilization validation.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!