Innovations in laryngoscope blade sterilization processes.
JUL 14, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Laryngoscope Sterilization Evolution and Objectives
Laryngoscope sterilization has undergone significant evolution since the device's inception in the early 20th century. Initially, basic cleaning methods were employed, often involving simple washing and disinfection. As medical knowledge advanced, the importance of thorough sterilization became increasingly apparent, leading to more rigorous processes.
The 1950s and 1960s saw the introduction of chemical sterilization methods, such as ethylene oxide gas. This marked a significant improvement in infection control but came with its own set of challenges, including potential toxicity and lengthy aeration times. The 1970s brought about the widespread adoption of steam sterilization (autoclaving) for heat-resistant instruments, which remains a gold standard in many healthcare settings.
In recent decades, the focus has shifted towards developing more efficient, safer, and environmentally friendly sterilization techniques. Low-temperature hydrogen peroxide gas plasma sterilization, introduced in the 1990s, offered a quicker, non-toxic alternative for heat-sensitive equipment. Concurrently, advancements in materials science led to the development of disposable laryngoscope blades, addressing sterilization concerns through single-use applications.
The current technological landscape is characterized by a drive towards automation, traceability, and validation of sterilization processes. Modern sterilization equipment often incorporates computerized monitoring systems, ensuring consistent and verifiable results. There's also a growing emphasis on rapid sterilization techniques to meet the demands of high-turnover medical environments.
Looking forward, the objectives in laryngoscope blade sterilization are multifaceted. Primary goals include developing methods that are faster, more cost-effective, and less resource-intensive while maintaining or improving upon current sterility assurance levels. There's a push towards "green" sterilization technologies that reduce environmental impact and energy consumption.
Another key objective is the creation of sterilization processes specifically tailored to the unique challenges posed by laryngoscope blades, such as their complex shapes and the potential for biofilm formation. Innovations in this area may involve novel chemical formulations, advanced physical processes like cold plasma technology, or hybrid approaches combining multiple sterilization modalities.
Ultimately, the field aims to achieve a balance between efficacy, efficiency, and safety, ensuring that laryngoscope blades can be rapidly and reliably sterilized without compromising patient safety or environmental sustainability. This ongoing evolution reflects the broader trends in medical device sterilization, driven by advances in technology, changing regulatory landscapes, and an ever-increasing focus on infection prevention in healthcare settings.
The 1950s and 1960s saw the introduction of chemical sterilization methods, such as ethylene oxide gas. This marked a significant improvement in infection control but came with its own set of challenges, including potential toxicity and lengthy aeration times. The 1970s brought about the widespread adoption of steam sterilization (autoclaving) for heat-resistant instruments, which remains a gold standard in many healthcare settings.
In recent decades, the focus has shifted towards developing more efficient, safer, and environmentally friendly sterilization techniques. Low-temperature hydrogen peroxide gas plasma sterilization, introduced in the 1990s, offered a quicker, non-toxic alternative for heat-sensitive equipment. Concurrently, advancements in materials science led to the development of disposable laryngoscope blades, addressing sterilization concerns through single-use applications.
The current technological landscape is characterized by a drive towards automation, traceability, and validation of sterilization processes. Modern sterilization equipment often incorporates computerized monitoring systems, ensuring consistent and verifiable results. There's also a growing emphasis on rapid sterilization techniques to meet the demands of high-turnover medical environments.
Looking forward, the objectives in laryngoscope blade sterilization are multifaceted. Primary goals include developing methods that are faster, more cost-effective, and less resource-intensive while maintaining or improving upon current sterility assurance levels. There's a push towards "green" sterilization technologies that reduce environmental impact and energy consumption.
Another key objective is the creation of sterilization processes specifically tailored to the unique challenges posed by laryngoscope blades, such as their complex shapes and the potential for biofilm formation. Innovations in this area may involve novel chemical formulations, advanced physical processes like cold plasma technology, or hybrid approaches combining multiple sterilization modalities.
Ultimately, the field aims to achieve a balance between efficacy, efficiency, and safety, ensuring that laryngoscope blades can be rapidly and reliably sterilized without compromising patient safety or environmental sustainability. This ongoing evolution reflects the broader trends in medical device sterilization, driven by advances in technology, changing regulatory landscapes, and an ever-increasing focus on infection prevention in healthcare settings.
Market Analysis for Advanced Sterilization Solutions
The market for advanced sterilization solutions in the healthcare industry, particularly for laryngoscope blades, is experiencing significant growth driven by increasing awareness of infection control and patient safety. The global market for medical device sterilization is projected to reach substantial value in the coming years, with a compound annual growth rate (CAGR) outpacing many other healthcare segments. This growth is primarily attributed to the rising number of surgical procedures, stringent regulatory requirements, and the need for more efficient and cost-effective sterilization methods.
In the specific context of laryngoscope blade sterilization, there is a growing demand for innovative solutions that can address the unique challenges posed by these critical medical devices. Traditional sterilization methods, such as autoclaving, have been the standard for many years. However, there is an increasing recognition of their limitations, including potential damage to sensitive components and the time-consuming nature of the process. This has created a market opportunity for advanced sterilization technologies that can offer faster turnaround times, improved efficacy, and reduced risk of equipment damage.
The market is seeing a shift towards more advanced sterilization methods, such as low-temperature hydrogen peroxide gas plasma sterilization and ethylene oxide sterilization. These technologies are gaining traction due to their ability to sterilize heat-sensitive materials and complex instruments like laryngoscope blades more effectively. Additionally, there is a growing interest in single-use, disposable laryngoscope blades, which eliminate the need for sterilization altogether and reduce the risk of cross-contamination.
Geographically, North America and Europe currently dominate the market for advanced sterilization solutions, owing to their well-established healthcare infrastructure and stringent regulatory environments. However, emerging economies in Asia-Pacific and Latin America are expected to witness the highest growth rates in the coming years, driven by increasing healthcare expenditure and growing awareness of infection control practices.
The competitive landscape of the market is characterized by the presence of both established medical device companies and innovative startups. Key players are focusing on research and development to introduce novel sterilization technologies specifically designed for delicate instruments like laryngoscope blades. There is also a trend towards the development of integrated sterilization systems that can handle multiple types of medical devices, offering healthcare facilities greater flexibility and efficiency in their sterilization processes.
In the specific context of laryngoscope blade sterilization, there is a growing demand for innovative solutions that can address the unique challenges posed by these critical medical devices. Traditional sterilization methods, such as autoclaving, have been the standard for many years. However, there is an increasing recognition of their limitations, including potential damage to sensitive components and the time-consuming nature of the process. This has created a market opportunity for advanced sterilization technologies that can offer faster turnaround times, improved efficacy, and reduced risk of equipment damage.
The market is seeing a shift towards more advanced sterilization methods, such as low-temperature hydrogen peroxide gas plasma sterilization and ethylene oxide sterilization. These technologies are gaining traction due to their ability to sterilize heat-sensitive materials and complex instruments like laryngoscope blades more effectively. Additionally, there is a growing interest in single-use, disposable laryngoscope blades, which eliminate the need for sterilization altogether and reduce the risk of cross-contamination.
Geographically, North America and Europe currently dominate the market for advanced sterilization solutions, owing to their well-established healthcare infrastructure and stringent regulatory environments. However, emerging economies in Asia-Pacific and Latin America are expected to witness the highest growth rates in the coming years, driven by increasing healthcare expenditure and growing awareness of infection control practices.
The competitive landscape of the market is characterized by the presence of both established medical device companies and innovative startups. Key players are focusing on research and development to introduce novel sterilization technologies specifically designed for delicate instruments like laryngoscope blades. There is also a trend towards the development of integrated sterilization systems that can handle multiple types of medical devices, offering healthcare facilities greater flexibility and efficiency in their sterilization processes.
Current Challenges in Laryngoscope Blade Sterilization
Laryngoscope blade sterilization processes face several significant challenges in the current healthcare environment. One of the primary issues is the complexity of blade designs, which often include intricate components and hard-to-reach areas. These design features make thorough cleaning and sterilization difficult, potentially leaving residual contaminants that can compromise patient safety.
Another challenge is the time-sensitive nature of laryngoscope use in medical settings. The need for rapid turnaround between procedures puts pressure on sterilization processes, sometimes leading to shortcuts or inadequate sterilization times. This urgency can result in incomplete decontamination, especially for more resistant pathogens.
The variety of sterilization methods available also presents a challenge. Different healthcare facilities may use various techniques, including chemical disinfection, autoclaving, or low-temperature sterilization methods. Each method has its own set of protocols and limitations, making standardization across institutions difficult and potentially leading to inconsistencies in sterilization efficacy.
Material compatibility is another significant concern. Laryngoscope blades are often made from materials that may be sensitive to certain sterilization processes. High-temperature methods can damage delicate components, while chemical sterilants may cause corrosion or degradation of blade materials over time. This necessitates a careful balance between effective sterilization and maintaining the integrity of the equipment.
The emergence of new pathogens and drug-resistant microorganisms poses an ongoing challenge to current sterilization practices. Traditional methods may not be fully effective against these evolving threats, requiring continuous adaptation and improvement of sterilization protocols.
Cost and resource constraints also impact sterilization processes. Many healthcare facilities face budget limitations that may restrict access to advanced sterilization technologies or limit the frequency of blade replacement. This can lead to the continued use of older, less effective sterilization methods or the prolonged use of blades that should be retired.
Lastly, human factors play a crucial role in sterilization challenges. Proper training and adherence to sterilization protocols are essential, but staff turnover, time pressures, and varying levels of expertise can lead to inconsistencies in the application of sterilization procedures. Ensuring consistent compliance with best practices across all personnel involved in the sterilization process remains an ongoing challenge in many healthcare settings.
Another challenge is the time-sensitive nature of laryngoscope use in medical settings. The need for rapid turnaround between procedures puts pressure on sterilization processes, sometimes leading to shortcuts or inadequate sterilization times. This urgency can result in incomplete decontamination, especially for more resistant pathogens.
The variety of sterilization methods available also presents a challenge. Different healthcare facilities may use various techniques, including chemical disinfection, autoclaving, or low-temperature sterilization methods. Each method has its own set of protocols and limitations, making standardization across institutions difficult and potentially leading to inconsistencies in sterilization efficacy.
Material compatibility is another significant concern. Laryngoscope blades are often made from materials that may be sensitive to certain sterilization processes. High-temperature methods can damage delicate components, while chemical sterilants may cause corrosion or degradation of blade materials over time. This necessitates a careful balance between effective sterilization and maintaining the integrity of the equipment.
The emergence of new pathogens and drug-resistant microorganisms poses an ongoing challenge to current sterilization practices. Traditional methods may not be fully effective against these evolving threats, requiring continuous adaptation and improvement of sterilization protocols.
Cost and resource constraints also impact sterilization processes. Many healthcare facilities face budget limitations that may restrict access to advanced sterilization technologies or limit the frequency of blade replacement. This can lead to the continued use of older, less effective sterilization methods or the prolonged use of blades that should be retired.
Lastly, human factors play a crucial role in sterilization challenges. Proper training and adherence to sterilization protocols are essential, but staff turnover, time pressures, and varying levels of expertise can lead to inconsistencies in the application of sterilization procedures. Ensuring consistent compliance with best practices across all personnel involved in the sterilization process remains an ongoing challenge in many healthcare settings.
Cutting-edge Laryngoscope Blade Sterilization Techniques
01 Chemical sterilization methods
Various chemical agents can be used for sterilizing laryngoscope blades. These may include liquid disinfectants, sterilizing gases, or other chemical solutions that effectively eliminate microorganisms. The choice of chemical agent depends on the material of the blade and the level of sterilization required.- Chemical sterilization methods: Various chemical agents can be used for sterilizing laryngoscope blades. These may include liquid disinfectants, sterilizing gases, or other chemical solutions that effectively eliminate microorganisms. The choice of chemical agent depends on the material of the blade and the level of sterilization required.
- Heat-based sterilization techniques: Heat-based methods such as autoclaving or steam sterilization can be employed for laryngoscope blade sterilization. These methods use high-temperature steam under pressure to eliminate microorganisms. The effectiveness depends on the blade material's ability to withstand high temperatures without damage.
- Disposable blade covers or sheaths: Using disposable covers or sheaths for laryngoscope blades can provide a sterile barrier without the need for repeated sterilization of the blade itself. These covers are designed to be discarded after each use, reducing the risk of cross-contamination between patients.
- UV light sterilization: Ultraviolet (UV) light can be used to sterilize laryngoscope blades. This method involves exposing the blade to UV radiation, which effectively kills microorganisms on the surface. UV sterilization can be particularly useful for heat-sensitive materials or as a complementary method to other sterilization techniques.
- Integrated sterilization systems: Some laryngoscopes are designed with integrated sterilization systems. These may include built-in UV lights, self-cleaning mechanisms, or storage compartments that maintain sterility. Such designs aim to simplify the sterilization process and ensure consistent blade cleanliness between uses.
02 Heat-based sterilization techniques
Heat-based methods such as autoclaving or steam sterilization can be employed for laryngoscope blade sterilization. These methods use high-temperature steam under pressure to eliminate microorganisms. The effectiveness of heat-based sterilization depends on the blade material's heat resistance and the specific sterilization parameters used.Expand Specific Solutions03 Disposable or single-use blade covers
To prevent cross-contamination, disposable or single-use covers can be used on laryngoscope blades. These covers act as a barrier between the blade and the patient, reducing the need for frequent sterilization. The covers are discarded after each use, ensuring a clean surface for each patient.Expand Specific Solutions04 UV light sterilization
Ultraviolet (UV) light can be used to sterilize laryngoscope blades. This method involves exposing the blades to UV radiation, which effectively kills microorganisms by damaging their DNA. UV sterilization can be particularly useful for heat-sensitive materials or as a complementary method to other sterilization techniques.Expand Specific Solutions05 Integrated sterilization systems
Some laryngoscopes feature integrated sterilization systems that allow for on-site or rapid sterilization of blades. These systems may incorporate various sterilization methods such as chemical, heat, or UV light treatments. Integrated systems can improve efficiency and ensure consistent sterilization practices in clinical settings.Expand Specific Solutions
Key Manufacturers and Sterilization Equipment Providers
The laryngoscope blade sterilization market is in a growth phase, driven by increasing focus on infection control in healthcare settings. The global market size is estimated to be in the hundreds of millions of dollars, with steady expansion expected. Technologically, innovations are emerging from both established medical device companies and newer entrants. Key players like Karl Storz, Olympus, and Teleflex are advancing sterilization processes through automated systems and disposable components. Smaller firms such as Zhejiang Youyi Medical Equipment and Creo Medical are also contributing novel approaches. While some technologies are mature, there is ongoing development in areas like rapid sterilization methods and eco-friendly solutions, indicating room for further innovation and market evolution.
Karl Storz SE & Co. KG
Technical Solution: Karl Storz has developed an innovative sterilization process for laryngoscope blades using low-temperature hydrogen peroxide gas plasma technology. This method effectively sterilizes the blades at temperatures below 50°C, preserving the integrity of heat-sensitive components[1]. The process utilizes a specialized sterilization chamber where hydrogen peroxide is vaporized and ionized to create a plasma state, which effectively eliminates microorganisms on the blade surface[3]. Additionally, Karl Storz has implemented a tracking system using RFID tags to monitor the sterilization history of each blade, ensuring proper reprocessing and enhancing patient safety[5].
Strengths: Low-temperature process preserves blade integrity; Effective against a wide range of pathogens; RFID tracking enhances safety and compliance. Weaknesses: Requires specialized equipment; Higher initial investment compared to traditional methods.
Medivators, Inc.
Technical Solution: Medivators has developed an automated endoscope reprocessor (AER) system that can be adapted for laryngoscope blade sterilization. The system utilizes a multi-stage process combining high-level disinfection with peracetic acid and terminal sterilization using ethylene oxide gas[7]. This approach ensures thorough decontamination of both the external surfaces and internal channels of complex laryngoscope blades. The AER system features advanced monitoring capabilities, including real-time tracking of chemical concentrations and sterilization parameters[9]. Medivators has also implemented a data logging system that provides comprehensive documentation of each sterilization cycle, facilitating quality control and regulatory compliance[11].
Strengths: Comprehensive sterilization of complex blade designs; Automated process reduces human error; Detailed documentation for quality assurance. Weaknesses: Longer processing time compared to some other methods; Requires handling of potentially hazardous chemicals.
Innovative Patents in Medical Instrument Sterilization
Automated laryngoscope blade disinfecting device
PatentUndeterminedPH12021050410A1
Innovation
- Automated multi-step disinfection process combining detergent, disinfectant, water rinse, and UV-C sterilization in a single chamber.
- Programmable control box for customizable temperature and timing settings of the disinfection process.
- Reduced human contact with contaminated equipment and hazardous disinfecting solutions through automation.
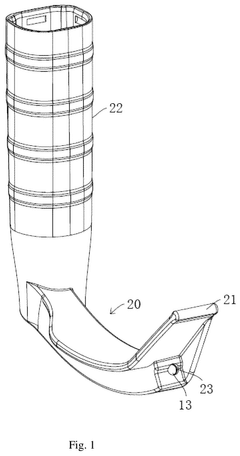
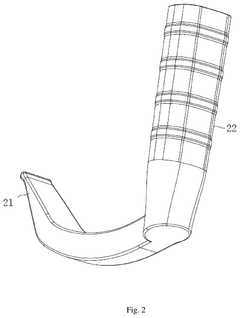
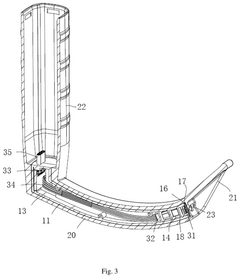
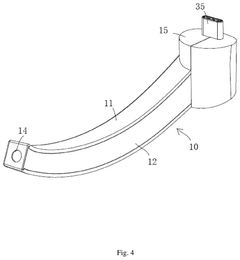
Disposable blade laryngoscope and processing method thereof
PatentInactiveUS20240415382A1
Innovation
- A disposable blade laryngoscope design featuring a buckled shell structure with a mounting channel, a coating shell, and an optical lens assembly, where the shells are connected by ultrasonic welding and coated with a secondary injection molding process to enhance sealing and simplify assembly, incorporating a tongue depressor and hollow handle for improved sealing and reduced manufacturing complexity.
Regulatory Framework for Medical Device Sterilization
The regulatory framework for medical device sterilization is a critical aspect of ensuring patient safety and maintaining the integrity of medical equipment. In the context of laryngoscope blade sterilization, several key regulations and guidelines govern the processes and standards that must be adhered to.
The U.S. Food and Drug Administration (FDA) plays a central role in regulating medical device sterilization. Under the Federal Food, Drug, and Cosmetic Act, the FDA has established specific requirements for the sterilization of medical devices, including laryngoscope blades. These regulations are outlined in 21 CFR Part 820, which covers Quality System Regulations for medical devices.
In Europe, the Medical Device Regulation (MDR) 2017/745 provides the regulatory framework for medical device sterilization. This regulation emphasizes the importance of proper sterilization processes and validation to ensure the safety and effectiveness of medical devices, including laryngoscope blades.
International standards also play a crucial role in shaping the regulatory landscape for medical device sterilization. ISO 11135 specifically addresses the requirements for the development, validation, and routine control of ethylene oxide sterilization for medical devices. This standard is widely recognized and adopted by regulatory bodies worldwide.
The Association for the Advancement of Medical Instrumentation (AAMI) has developed several standards relevant to medical device sterilization, including ANSI/AAMI ST79, which provides comprehensive guidance on steam sterilization in healthcare facilities. These standards are often referenced by regulatory bodies and serve as best practice guidelines for healthcare institutions.
Regulatory bodies also require manufacturers to validate their sterilization processes. This involves demonstrating that the chosen sterilization method consistently achieves the required Sterility Assurance Level (SAL), typically set at 10^-6 for medical devices like laryngoscope blades.
Environmental considerations have also become increasingly important in the regulatory framework. The Environmental Protection Agency (EPA) regulates the use of certain sterilization agents, such as ethylene oxide, due to their potential environmental impact. This has led to a growing emphasis on more environmentally friendly sterilization methods.
As innovations in laryngoscope blade sterilization processes emerge, they must be evaluated against these regulatory standards. New sterilization technologies or modifications to existing processes require thorough validation and may need to undergo regulatory review before implementation. This ensures that any advancements in sterilization techniques maintain or improve upon the established safety and efficacy standards for medical devices.
The U.S. Food and Drug Administration (FDA) plays a central role in regulating medical device sterilization. Under the Federal Food, Drug, and Cosmetic Act, the FDA has established specific requirements for the sterilization of medical devices, including laryngoscope blades. These regulations are outlined in 21 CFR Part 820, which covers Quality System Regulations for medical devices.
In Europe, the Medical Device Regulation (MDR) 2017/745 provides the regulatory framework for medical device sterilization. This regulation emphasizes the importance of proper sterilization processes and validation to ensure the safety and effectiveness of medical devices, including laryngoscope blades.
International standards also play a crucial role in shaping the regulatory landscape for medical device sterilization. ISO 11135 specifically addresses the requirements for the development, validation, and routine control of ethylene oxide sterilization for medical devices. This standard is widely recognized and adopted by regulatory bodies worldwide.
The Association for the Advancement of Medical Instrumentation (AAMI) has developed several standards relevant to medical device sterilization, including ANSI/AAMI ST79, which provides comprehensive guidance on steam sterilization in healthcare facilities. These standards are often referenced by regulatory bodies and serve as best practice guidelines for healthcare institutions.
Regulatory bodies also require manufacturers to validate their sterilization processes. This involves demonstrating that the chosen sterilization method consistently achieves the required Sterility Assurance Level (SAL), typically set at 10^-6 for medical devices like laryngoscope blades.
Environmental considerations have also become increasingly important in the regulatory framework. The Environmental Protection Agency (EPA) regulates the use of certain sterilization agents, such as ethylene oxide, due to their potential environmental impact. This has led to a growing emphasis on more environmentally friendly sterilization methods.
As innovations in laryngoscope blade sterilization processes emerge, they must be evaluated against these regulatory standards. New sterilization technologies or modifications to existing processes require thorough validation and may need to undergo regulatory review before implementation. This ensures that any advancements in sterilization techniques maintain or improve upon the established safety and efficacy standards for medical devices.
Environmental Impact of Sterilization Processes
The environmental impact of sterilization processes for laryngoscope blades is a critical consideration in healthcare settings. Traditional sterilization methods, such as ethylene oxide (EtO) and steam autoclaving, have been widely used but are associated with significant environmental concerns.
EtO sterilization, while effective, poses risks due to its toxicity and potential for environmental contamination. The process releases harmful emissions and requires careful handling of residual gases. Steam autoclaving, on the other hand, consumes substantial amounts of water and energy, contributing to increased carbon footprints in healthcare facilities.
Recent innovations in laryngoscope blade sterilization have focused on developing more environmentally friendly alternatives. Low-temperature hydrogen peroxide gas plasma sterilization has emerged as a promising option. This method produces minimal toxic residues and requires less energy compared to traditional techniques. Additionally, it eliminates the need for aeration time, reducing overall process duration and resource consumption.
Another eco-friendly approach gaining traction is the use of ultraviolet (UV) light sterilization. UV-C light effectively inactivates microorganisms without the need for chemicals or high temperatures. This method significantly reduces water and energy usage, as well as chemical waste production. However, its efficacy on complex surfaces and shadowed areas of laryngoscope blades requires further investigation.
Ozone-based sterilization is also being explored as an environmentally conscious alternative. Ozone naturally decomposes into oxygen, leaving no harmful residues. This process operates at lower temperatures and consumes less energy than conventional methods. However, the potential for ozone leakage and its impact on air quality must be carefully managed.
The development of single-use, disposable laryngoscope blades has introduced a new dimension to the environmental discussion. While these products eliminate the need for sterilization, they generate increased plastic waste. Biodegradable materials and improved recycling processes are being researched to mitigate this issue.
As healthcare facilities strive to reduce their environmental footprint, the adoption of these innovative sterilization processes for laryngoscope blades is likely to increase. Future research should focus on optimizing these methods to further minimize resource consumption and waste generation while maintaining high sterilization efficacy.
EtO sterilization, while effective, poses risks due to its toxicity and potential for environmental contamination. The process releases harmful emissions and requires careful handling of residual gases. Steam autoclaving, on the other hand, consumes substantial amounts of water and energy, contributing to increased carbon footprints in healthcare facilities.
Recent innovations in laryngoscope blade sterilization have focused on developing more environmentally friendly alternatives. Low-temperature hydrogen peroxide gas plasma sterilization has emerged as a promising option. This method produces minimal toxic residues and requires less energy compared to traditional techniques. Additionally, it eliminates the need for aeration time, reducing overall process duration and resource consumption.
Another eco-friendly approach gaining traction is the use of ultraviolet (UV) light sterilization. UV-C light effectively inactivates microorganisms without the need for chemicals or high temperatures. This method significantly reduces water and energy usage, as well as chemical waste production. However, its efficacy on complex surfaces and shadowed areas of laryngoscope blades requires further investigation.
Ozone-based sterilization is also being explored as an environmentally conscious alternative. Ozone naturally decomposes into oxygen, leaving no harmful residues. This process operates at lower temperatures and consumes less energy than conventional methods. However, the potential for ozone leakage and its impact on air quality must be carefully managed.
The development of single-use, disposable laryngoscope blades has introduced a new dimension to the environmental discussion. While these products eliminate the need for sterilization, they generate increased plastic waste. Biodegradable materials and improved recycling processes are being researched to mitigate this issue.
As healthcare facilities strive to reduce their environmental footprint, the adoption of these innovative sterilization processes for laryngoscope blades is likely to increase. Future research should focus on optimizing these methods to further minimize resource consumption and waste generation while maintaining high sterilization efficacy.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!