Laryngoscopes and the rise of personalized anesthesia.
JUL 14, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Laryngoscope Evolution
The evolution of laryngoscopes has been a remarkable journey in the field of anesthesiology and airway management. From the early 19th century to the present day, these devices have undergone significant transformations, driven by technological advancements and the growing need for more precise and less invasive procedures.
In the early 1800s, the first rudimentary laryngoscopes were developed, consisting of simple tongue depressors and mirrors. These basic tools allowed physicians to visualize the larynx and vocal cords, but their effectiveness was limited. The breakthrough came in 1854 when Manuel Garcia invented the indirect laryngoscope, using a small mirror to reflect light onto the larynx.
The late 19th and early 20th centuries saw the introduction of direct laryngoscopy. In 1895, Alfred Kirstein developed the first direct laryngoscope, which provided a more straightforward view of the larynx. This innovation paved the way for more accurate diagnoses and improved airway management during surgical procedures.
The mid-20th century brought about significant advancements in laryngoscope design. The Macintosh laryngoscope, introduced by Robert Macintosh in 1943, became the gold standard for decades. Its curved blade design allowed for easier visualization of the larynx and facilitated endotracheal intubation.
As technology progressed, video laryngoscopes emerged in the late 1990s and early 2000s. These devices incorporated small cameras and video screens, providing a magnified view of the airway and improving the success rate of intubations, especially in difficult cases. The GlideScope, introduced in 2001, was one of the pioneering video laryngoscopes that gained widespread adoption.
In recent years, the focus has shifted towards developing more portable and user-friendly laryngoscopes. Disposable laryngoscopes have become increasingly popular, addressing concerns about cross-contamination and reducing the need for sterilization between procedures. Additionally, advancements in LED technology have improved illumination, enhancing visibility during examinations and procedures.
The rise of personalized anesthesia has further influenced laryngoscope evolution. Manufacturers are now developing devices that can adapt to individual patient anatomies, utilizing artificial intelligence and machine learning algorithms to optimize blade positioning and intubation techniques. These smart laryngoscopes aim to reduce complications and improve patient outcomes by tailoring the procedure to each individual's unique airway characteristics.
Looking ahead, the future of laryngoscopes is likely to involve further integration with other medical technologies. Augmented reality systems may be incorporated to provide real-time guidance during intubations, while 3D printing technology could enable the production of custom-fit laryngoscope blades for patients with challenging airways. As the field continues to evolve, the goal remains to enhance patient safety, improve procedural success rates, and minimize complications in airway management and anesthesia administration.
In the early 1800s, the first rudimentary laryngoscopes were developed, consisting of simple tongue depressors and mirrors. These basic tools allowed physicians to visualize the larynx and vocal cords, but their effectiveness was limited. The breakthrough came in 1854 when Manuel Garcia invented the indirect laryngoscope, using a small mirror to reflect light onto the larynx.
The late 19th and early 20th centuries saw the introduction of direct laryngoscopy. In 1895, Alfred Kirstein developed the first direct laryngoscope, which provided a more straightforward view of the larynx. This innovation paved the way for more accurate diagnoses and improved airway management during surgical procedures.
The mid-20th century brought about significant advancements in laryngoscope design. The Macintosh laryngoscope, introduced by Robert Macintosh in 1943, became the gold standard for decades. Its curved blade design allowed for easier visualization of the larynx and facilitated endotracheal intubation.
As technology progressed, video laryngoscopes emerged in the late 1990s and early 2000s. These devices incorporated small cameras and video screens, providing a magnified view of the airway and improving the success rate of intubations, especially in difficult cases. The GlideScope, introduced in 2001, was one of the pioneering video laryngoscopes that gained widespread adoption.
In recent years, the focus has shifted towards developing more portable and user-friendly laryngoscopes. Disposable laryngoscopes have become increasingly popular, addressing concerns about cross-contamination and reducing the need for sterilization between procedures. Additionally, advancements in LED technology have improved illumination, enhancing visibility during examinations and procedures.
The rise of personalized anesthesia has further influenced laryngoscope evolution. Manufacturers are now developing devices that can adapt to individual patient anatomies, utilizing artificial intelligence and machine learning algorithms to optimize blade positioning and intubation techniques. These smart laryngoscopes aim to reduce complications and improve patient outcomes by tailoring the procedure to each individual's unique airway characteristics.
Looking ahead, the future of laryngoscopes is likely to involve further integration with other medical technologies. Augmented reality systems may be incorporated to provide real-time guidance during intubations, while 3D printing technology could enable the production of custom-fit laryngoscope blades for patients with challenging airways. As the field continues to evolve, the goal remains to enhance patient safety, improve procedural success rates, and minimize complications in airway management and anesthesia administration.
Anesthesia Market Trends
The global anesthesia market has been experiencing significant growth and transformation in recent years, driven by technological advancements, increasing surgical procedures, and a growing emphasis on patient safety and comfort. The market is projected to continue its upward trajectory, with a compound annual growth rate (CAGR) expected to remain strong through the next decade.
One of the key factors contributing to market growth is the rising number of surgical procedures worldwide, particularly in emerging economies. As healthcare infrastructure improves and access to medical services expands, the demand for anesthesia products and services is increasing correspondingly. Additionally, the aging population in many developed countries is leading to a higher incidence of chronic diseases and conditions requiring surgical interventions, further fueling market growth.
Technological innovations are playing a crucial role in shaping the anesthesia market landscape. The development of advanced anesthesia delivery systems, monitoring devices, and drug formulations is enhancing the safety and efficacy of anesthetic procedures. In particular, the integration of artificial intelligence and machine learning algorithms into anesthesia management systems is enabling more precise dosing and personalized care.
The trend towards minimally invasive surgeries is also influencing the anesthesia market. These procedures often require specialized anesthetic techniques and equipment, driving demand for innovative products tailored to these applications. Furthermore, the growing adoption of ambulatory surgical centers is creating new opportunities for anesthesia providers and equipment manufacturers.
In terms of product segments, inhalation anesthetics continue to dominate the market, followed by intravenous anesthetics. However, regional anesthesia techniques are gaining popularity due to their potential for faster recovery times and reduced side effects. This shift is prompting manufacturers to invest in developing improved local anesthetic agents and delivery systems.
The COVID-19 pandemic has had a significant impact on the anesthesia market, initially causing disruptions in elective surgeries and supply chains. However, it has also accelerated certain trends, such as the adoption of telemedicine for pre-anesthesia consultations and the development of protocols for safe anesthesia administration during infectious disease outbreaks.
Looking ahead, personalized anesthesia is emerging as a major trend in the market. This approach involves tailoring anesthetic regimens to individual patient characteristics, including genetic factors, medical history, and physiological parameters. The rise of personalized anesthesia is driving research into pharmacogenomics and the development of more sophisticated monitoring technologies, including those integrated into laryngoscopes and other airway management devices.
One of the key factors contributing to market growth is the rising number of surgical procedures worldwide, particularly in emerging economies. As healthcare infrastructure improves and access to medical services expands, the demand for anesthesia products and services is increasing correspondingly. Additionally, the aging population in many developed countries is leading to a higher incidence of chronic diseases and conditions requiring surgical interventions, further fueling market growth.
Technological innovations are playing a crucial role in shaping the anesthesia market landscape. The development of advanced anesthesia delivery systems, monitoring devices, and drug formulations is enhancing the safety and efficacy of anesthetic procedures. In particular, the integration of artificial intelligence and machine learning algorithms into anesthesia management systems is enabling more precise dosing and personalized care.
The trend towards minimally invasive surgeries is also influencing the anesthesia market. These procedures often require specialized anesthetic techniques and equipment, driving demand for innovative products tailored to these applications. Furthermore, the growing adoption of ambulatory surgical centers is creating new opportunities for anesthesia providers and equipment manufacturers.
In terms of product segments, inhalation anesthetics continue to dominate the market, followed by intravenous anesthetics. However, regional anesthesia techniques are gaining popularity due to their potential for faster recovery times and reduced side effects. This shift is prompting manufacturers to invest in developing improved local anesthetic agents and delivery systems.
The COVID-19 pandemic has had a significant impact on the anesthesia market, initially causing disruptions in elective surgeries and supply chains. However, it has also accelerated certain trends, such as the adoption of telemedicine for pre-anesthesia consultations and the development of protocols for safe anesthesia administration during infectious disease outbreaks.
Looking ahead, personalized anesthesia is emerging as a major trend in the market. This approach involves tailoring anesthetic regimens to individual patient characteristics, including genetic factors, medical history, and physiological parameters. The rise of personalized anesthesia is driving research into pharmacogenomics and the development of more sophisticated monitoring technologies, including those integrated into laryngoscopes and other airway management devices.
Laryngoscope Tech Challenges
Laryngoscopes have been a critical tool in anesthesia and airway management for decades. However, as medical technology advances and the demand for personalized healthcare grows, several challenges have emerged in the field of laryngoscopy. One of the primary challenges is the need for improved visualization techniques. Traditional laryngoscopes often struggle to provide clear views of the larynx in patients with difficult airways, leading to potential complications during intubation procedures.
Another significant challenge is the development of more ergonomic designs. Many anesthesiologists and healthcare professionals report discomfort and strain during prolonged use of conventional laryngoscopes. This has led to a push for more user-friendly designs that reduce physical stress and improve overall performance during procedures.
The integration of advanced imaging technologies into laryngoscopes presents both opportunities and challenges. While video laryngoscopes have shown promise in improving visualization, issues such as image quality, latency, and the learning curve associated with new technologies remain obstacles to widespread adoption.
Personalization of laryngoscopes to accommodate individual patient anatomies is another area of focus. The one-size-fits-all approach is becoming increasingly inadequate, particularly for patients with unique airway characteristics. Developing adaptable laryngoscope designs that can be customized for specific patient needs is a complex engineering challenge.
Infection control and sterilization present ongoing challenges in laryngoscope design and usage. As healthcare-associated infections remain a concern, creating laryngoscopes that are easy to clean and sterilize without compromising functionality is crucial. This includes addressing issues related to disposable components and the environmental impact of single-use devices.
The rise of personalized anesthesia has also highlighted the need for laryngoscopes that can integrate with other medical devices and information systems. Developing interoperable laryngoscopes that can communicate with anesthesia machines, patient monitoring systems, and electronic health records is a significant technical hurdle.
Lastly, the cost-effectiveness of advanced laryngoscope technologies remains a challenge. While innovative features can improve patient outcomes, balancing these benefits with the economic realities of healthcare systems is an ongoing struggle. Developing affordable solutions that maintain high performance standards is essential for widespread adoption and improved patient care across diverse healthcare settings.
Another significant challenge is the development of more ergonomic designs. Many anesthesiologists and healthcare professionals report discomfort and strain during prolonged use of conventional laryngoscopes. This has led to a push for more user-friendly designs that reduce physical stress and improve overall performance during procedures.
The integration of advanced imaging technologies into laryngoscopes presents both opportunities and challenges. While video laryngoscopes have shown promise in improving visualization, issues such as image quality, latency, and the learning curve associated with new technologies remain obstacles to widespread adoption.
Personalization of laryngoscopes to accommodate individual patient anatomies is another area of focus. The one-size-fits-all approach is becoming increasingly inadequate, particularly for patients with unique airway characteristics. Developing adaptable laryngoscope designs that can be customized for specific patient needs is a complex engineering challenge.
Infection control and sterilization present ongoing challenges in laryngoscope design and usage. As healthcare-associated infections remain a concern, creating laryngoscopes that are easy to clean and sterilize without compromising functionality is crucial. This includes addressing issues related to disposable components and the environmental impact of single-use devices.
The rise of personalized anesthesia has also highlighted the need for laryngoscopes that can integrate with other medical devices and information systems. Developing interoperable laryngoscopes that can communicate with anesthesia machines, patient monitoring systems, and electronic health records is a significant technical hurdle.
Lastly, the cost-effectiveness of advanced laryngoscope technologies remains a challenge. While innovative features can improve patient outcomes, balancing these benefits with the economic realities of healthcare systems is an ongoing struggle. Developing affordable solutions that maintain high performance standards is essential for widespread adoption and improved patient care across diverse healthcare settings.
Current Laryngoscope Solutions
01 Illumination systems for laryngoscopes
Laryngoscopes often incorporate advanced illumination systems to improve visibility during intubation procedures. These systems may include LED lights, fiber optic cables, or other innovative lighting technologies to provide clear and focused illumination of the larynx and surrounding structures.- Illumination systems for laryngoscopes: Laryngoscopes often incorporate advanced illumination systems to improve visibility during intubation procedures. These systems may include LED lights, fiber optic cables, or other innovative lighting technologies to provide clear and adjustable illumination of the larynx and surrounding areas.
- Blade design and materials: The design and materials used in laryngoscope blades are crucial for effective intubation. Innovations in this area include ergonomic shapes, disposable blades, and the use of advanced materials to improve strength, flexibility, and sterilization capabilities.
- Video laryngoscopes: Video laryngoscopes incorporate small cameras and screens to provide a clear view of the larynx during intubation. These devices often feature high-resolution imaging, recording capabilities, and ergonomic designs to improve the success rate of intubation procedures.
- Disposable and single-use laryngoscopes: To reduce the risk of cross-contamination and simplify sterilization processes, disposable and single-use laryngoscopes have been developed. These devices are designed to be cost-effective while maintaining the necessary functionality for successful intubation.
- Ergonomic handle designs: Innovations in laryngoscope handle designs focus on improving ergonomics and user comfort. These designs may include adjustable angles, textured grips, and lightweight materials to reduce hand fatigue and improve control during intubation procedures.
02 Blade design and materials
The design and materials used in laryngoscope blades are crucial for effective intubation. Innovations in this area may include ergonomic shapes, flexible or adjustable blades, and the use of advanced materials to improve strength, durability, and ease of sterilization.Expand Specific Solutions03 Video laryngoscopes
Video laryngoscopes incorporate small cameras and screens to provide a clear view of the larynx during intubation. These devices can improve the success rate of intubation procedures, especially in difficult cases, by offering a magnified and adjustable view of the airway.Expand Specific Solutions04 Disposable laryngoscope components
To reduce the risk of cross-contamination and simplify sterilization processes, many laryngoscopes now feature disposable components. These may include single-use blades, handles, or covers that can be easily replaced between patients.Expand Specific Solutions05 Ergonomic handle designs
Improved handle designs focus on ergonomics and user comfort during intubation procedures. These innovations may include adjustable grips, lightweight materials, and ergonomic shapes that reduce hand fatigue and improve control during use.Expand Specific Solutions
Key Laryngoscope Manufacturers
The research on laryngoscopes and personalized anesthesia is in a growth phase, with increasing market size and technological advancements. The global laryngoscope market is expanding due to rising demand for minimally invasive procedures and growing awareness of airway management. Companies like Zhejiang Youyi Medical Equipment, Olympus Medical Systems, and Verathon are driving innovation in visualized airway management tools. The technology is maturing rapidly, with firms such as Ambu A/S and Karl Storz developing single-use flexible intubation scopes and digital documentation systems. Academic institutions like MIT and Johns Hopkins University are contributing to research, potentially leading to breakthroughs in personalized anesthesia techniques.
Olympus Medical Systems Corp.
Technical Solution: Olympus has developed advanced video laryngoscopes with high-definition imaging capabilities. Their latest models incorporate 4K resolution cameras and LED illumination for superior visualization of the larynx[1]. The company has also integrated artificial intelligence algorithms to assist in identifying anatomical landmarks and guiding intubation[2]. Olympus's laryngoscopes feature ergonomic designs with adjustable handles and screens to improve user comfort during procedures. Additionally, they have implemented wireless connectivity to allow real-time sharing of laryngoscopic images with other medical team members[3].
Strengths: Superior image quality, AI-assisted intubation, ergonomic design. Weaknesses: Higher cost compared to traditional laryngoscopes, potential for technical issues with advanced features.
Covidien Pte Ltd.
Technical Solution: Covidien has focused on developing video laryngoscopes with disposable blades to address infection control concerns. Their technology incorporates a high-resolution camera at the blade tip, providing a clear view of the vocal cords on an attached monitor[4]. Covidien's laryngoscopes feature a unique blade curvature designed to minimize the force required for intubation, potentially reducing patient trauma. The company has also integrated a drug delivery system into some models, allowing for the administration of local anesthetics during the procedure[5]. Covidien's devices include data logging capabilities to support personalized anesthesia protocols and quality improvement initiatives.
Strengths: Disposable blades for improved hygiene, integrated drug delivery system. Weaknesses: Potential for higher ongoing costs due to disposable components, learning curve for practitioners transitioning from traditional laryngoscopes.
Innovative Laryngoscope Designs
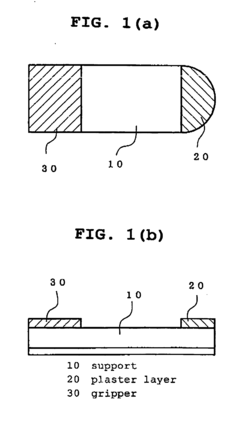
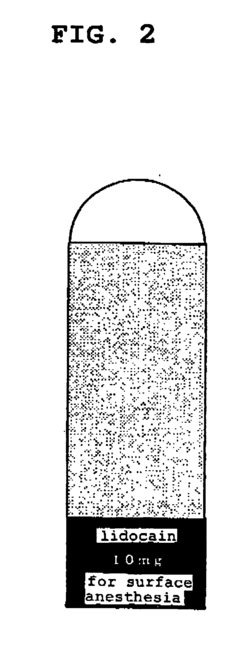
Topical anaesthetic preparation for pretreatment for upper gastrointestinal endoscopy
PatentInactiveEP1604652B1
Innovation
- A topical anesthetic preparation with a support having a specific stiffness and a plaster layer containing an adhesive polymer and anesthetic, accompanied by a gripper for easy identification and efficient delivery to the oral cavity, ensuring high drug utilization and reduced bitterness perception.
Regulatory Framework
The regulatory framework surrounding laryngoscopes and personalized anesthesia is complex and evolving, reflecting the critical nature of these medical devices and practices in patient care. In the United States, the Food and Drug Administration (FDA) classifies laryngoscopes as Class I medical devices, which are subject to general controls but typically exempt from premarket notification requirements. However, certain advanced laryngoscopes with additional features may be classified as Class II devices, requiring more stringent regulatory oversight.
Internationally, regulatory bodies such as the European Medicines Agency (EMA) and Japan's Pharmaceuticals and Medical Devices Agency (PMDA) have established their own guidelines for laryngoscope approval and use. These regulations often focus on safety, efficacy, and quality control measures to ensure patient protection and optimal performance in clinical settings.
As personalized anesthesia gains prominence, regulatory frameworks are adapting to address the unique challenges posed by individualized treatment approaches. This includes guidelines for the use of pharmacogenomic testing to tailor anesthetic agents and dosages to patient-specific genetic profiles. Regulatory bodies are increasingly emphasizing the importance of data privacy and security in the context of personalized medicine, given the sensitive nature of genetic information used in anesthesia planning.
The integration of advanced technologies, such as artificial intelligence and machine learning, into laryngoscopes and anesthesia delivery systems has prompted regulatory agencies to develop new guidelines for software as a medical device (SaMD). These regulations aim to ensure the reliability and safety of AI-driven decision support tools in anesthesia management.
Regulatory frameworks also address the training and certification requirements for healthcare professionals using advanced laryngoscopes and implementing personalized anesthesia protocols. This includes guidelines for continuing education and competency assessments to maintain high standards of patient care in the rapidly evolving field of anesthesiology.
As the field progresses, regulatory bodies are working to strike a balance between fostering innovation and maintaining patient safety. This involves collaborative efforts with industry stakeholders, academic institutions, and healthcare providers to develop adaptive regulatory pathways that can keep pace with technological advancements while upholding rigorous safety and efficacy standards.
Internationally, regulatory bodies such as the European Medicines Agency (EMA) and Japan's Pharmaceuticals and Medical Devices Agency (PMDA) have established their own guidelines for laryngoscope approval and use. These regulations often focus on safety, efficacy, and quality control measures to ensure patient protection and optimal performance in clinical settings.
As personalized anesthesia gains prominence, regulatory frameworks are adapting to address the unique challenges posed by individualized treatment approaches. This includes guidelines for the use of pharmacogenomic testing to tailor anesthetic agents and dosages to patient-specific genetic profiles. Regulatory bodies are increasingly emphasizing the importance of data privacy and security in the context of personalized medicine, given the sensitive nature of genetic information used in anesthesia planning.
The integration of advanced technologies, such as artificial intelligence and machine learning, into laryngoscopes and anesthesia delivery systems has prompted regulatory agencies to develop new guidelines for software as a medical device (SaMD). These regulations aim to ensure the reliability and safety of AI-driven decision support tools in anesthesia management.
Regulatory frameworks also address the training and certification requirements for healthcare professionals using advanced laryngoscopes and implementing personalized anesthesia protocols. This includes guidelines for continuing education and competency assessments to maintain high standards of patient care in the rapidly evolving field of anesthesiology.
As the field progresses, regulatory bodies are working to strike a balance between fostering innovation and maintaining patient safety. This involves collaborative efforts with industry stakeholders, academic institutions, and healthcare providers to develop adaptive regulatory pathways that can keep pace with technological advancements while upholding rigorous safety and efficacy standards.
Patient Safety Considerations
Patient safety is a paramount concern in the development and application of laryngoscopes and personalized anesthesia techniques. The integration of advanced technologies in these medical devices and procedures has significantly improved patient outcomes, but it also introduces new challenges that must be carefully addressed.
One of the primary safety considerations in laryngoscopy is the prevention of airway trauma. Traditional laryngoscopes can cause damage to soft tissues in the mouth and throat, leading to complications such as sore throat, hoarseness, and in rare cases, more severe injuries. Modern video laryngoscopes have been designed to reduce this risk by providing better visualization and requiring less force during intubation. However, proper training and technique remain crucial to maximize patient safety.
The rise of personalized anesthesia brings its own set of safety considerations. Tailoring anesthetic dosages and techniques to individual patient characteristics, such as age, weight, genetic factors, and medical history, can significantly reduce the risk of adverse events. However, this approach requires sophisticated monitoring systems and decision support tools to ensure accurate dosing and timely interventions.
Continuous monitoring of vital signs during anesthesia is essential for patient safety. Advanced monitoring devices now incorporate artificial intelligence algorithms to detect subtle changes that may indicate impending complications. These systems can alert anesthesiologists to potential issues before they become critical, allowing for proactive management.
Another critical aspect of patient safety in anesthesia is the prevention of medication errors. Automated drug delivery systems and barcode scanning technologies have been implemented to reduce the risk of incorrect drug administration. Additionally, electronic health records integrated with anesthesia information management systems help ensure that patient-specific factors are considered in anesthetic planning and delivery.
The emergence of closed-loop anesthesia delivery systems represents a significant advancement in patient safety. These systems use real-time physiological data to automatically adjust anesthetic delivery, maintaining optimal depth of anesthesia and reducing the risk of under- or over-sedation. However, the implementation of such systems requires careful validation and ongoing vigilance to prevent system-related errors.
Infection control is another crucial safety consideration, particularly in the context of reusable laryngoscopes. Stringent sterilization protocols and the development of single-use devices have been implemented to minimize the risk of cross-contamination between patients. The COVID-19 pandemic has further emphasized the importance of these measures and accelerated the adoption of disposable laryngoscope blades and video laryngoscopes with enhanced infection control features.
One of the primary safety considerations in laryngoscopy is the prevention of airway trauma. Traditional laryngoscopes can cause damage to soft tissues in the mouth and throat, leading to complications such as sore throat, hoarseness, and in rare cases, more severe injuries. Modern video laryngoscopes have been designed to reduce this risk by providing better visualization and requiring less force during intubation. However, proper training and technique remain crucial to maximize patient safety.
The rise of personalized anesthesia brings its own set of safety considerations. Tailoring anesthetic dosages and techniques to individual patient characteristics, such as age, weight, genetic factors, and medical history, can significantly reduce the risk of adverse events. However, this approach requires sophisticated monitoring systems and decision support tools to ensure accurate dosing and timely interventions.
Continuous monitoring of vital signs during anesthesia is essential for patient safety. Advanced monitoring devices now incorporate artificial intelligence algorithms to detect subtle changes that may indicate impending complications. These systems can alert anesthesiologists to potential issues before they become critical, allowing for proactive management.
Another critical aspect of patient safety in anesthesia is the prevention of medication errors. Automated drug delivery systems and barcode scanning technologies have been implemented to reduce the risk of incorrect drug administration. Additionally, electronic health records integrated with anesthesia information management systems help ensure that patient-specific factors are considered in anesthetic planning and delivery.
The emergence of closed-loop anesthesia delivery systems represents a significant advancement in patient safety. These systems use real-time physiological data to automatically adjust anesthetic delivery, maintaining optimal depth of anesthesia and reducing the risk of under- or over-sedation. However, the implementation of such systems requires careful validation and ongoing vigilance to prevent system-related errors.
Infection control is another crucial safety consideration, particularly in the context of reusable laryngoscopes. Stringent sterilization protocols and the development of single-use devices have been implemented to minimize the risk of cross-contamination between patients. The COVID-19 pandemic has further emphasized the importance of these measures and accelerated the adoption of disposable laryngoscope blades and video laryngoscopes with enhanced infection control features.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!