How to Integrate PEMF Therapy with Other Pain Management Modalities?
AUG 11, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
PEMF Therapy Background and Integration Goals
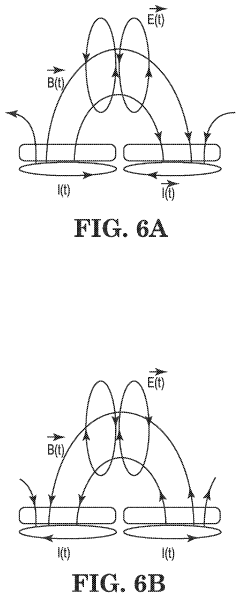
Pulsed Electromagnetic Field (PEMF) therapy has emerged as a promising non-invasive treatment for pain management over the past few decades. This technology utilizes electromagnetic fields to stimulate cellular repair and reduce inflammation, offering a unique approach to addressing various types of pain. The evolution of PEMF therapy can be traced back to the mid-20th century, with significant advancements in recent years due to improved understanding of cellular biology and electromagnetic interactions.
The primary goal of integrating PEMF therapy with other pain management modalities is to enhance overall treatment efficacy while minimizing side effects and reducing reliance on pharmacological interventions. This integration aims to create a more comprehensive and personalized approach to pain management, addressing the multifaceted nature of chronic pain conditions.
PEMF therapy's mechanism of action involves the generation of low-frequency electromagnetic fields that penetrate the body's tissues. These fields induce micro-currents within the cells, stimulating various physiological processes such as increased blood flow, enhanced cellular metabolism, and accelerated tissue repair. By modulating cellular activity, PEMF therapy can potentially complement other pain management techniques, offering synergistic effects.
The integration of PEMF therapy with conventional pain management approaches presents several objectives. Firstly, it seeks to reduce the dosage and frequency of pain medications, thereby minimizing potential side effects and dependency issues associated with long-term pharmaceutical use. Secondly, the integration aims to address pain from multiple angles, targeting both the symptoms and underlying causes of chronic pain conditions.
Furthermore, the incorporation of PEMF therapy into existing pain management protocols aims to improve patient outcomes by enhancing the overall quality of life. This includes not only pain reduction but also improvements in mobility, sleep quality, and general well-being. The non-invasive nature of PEMF therapy makes it an attractive option for patients who may be hesitant about more invasive procedures or those who have exhausted other treatment options.
As research in this field progresses, the integration goals extend to developing standardized protocols that combine PEMF therapy with other modalities such as physical therapy, acupuncture, and cognitive-behavioral therapy. These integrated approaches seek to create tailored treatment plans that address the individual needs of patients, recognizing the complex and often multifactorial nature of chronic pain.
In conclusion, the integration of PEMF therapy with other pain management modalities represents a significant step towards a more holistic and effective approach to pain treatment. By leveraging the unique properties of electromagnetic fields in conjunction with established pain management techniques, healthcare providers aim to offer patients a more comprehensive and personalized path to pain relief and improved quality of life.
The primary goal of integrating PEMF therapy with other pain management modalities is to enhance overall treatment efficacy while minimizing side effects and reducing reliance on pharmacological interventions. This integration aims to create a more comprehensive and personalized approach to pain management, addressing the multifaceted nature of chronic pain conditions.
PEMF therapy's mechanism of action involves the generation of low-frequency electromagnetic fields that penetrate the body's tissues. These fields induce micro-currents within the cells, stimulating various physiological processes such as increased blood flow, enhanced cellular metabolism, and accelerated tissue repair. By modulating cellular activity, PEMF therapy can potentially complement other pain management techniques, offering synergistic effects.
The integration of PEMF therapy with conventional pain management approaches presents several objectives. Firstly, it seeks to reduce the dosage and frequency of pain medications, thereby minimizing potential side effects and dependency issues associated with long-term pharmaceutical use. Secondly, the integration aims to address pain from multiple angles, targeting both the symptoms and underlying causes of chronic pain conditions.
Furthermore, the incorporation of PEMF therapy into existing pain management protocols aims to improve patient outcomes by enhancing the overall quality of life. This includes not only pain reduction but also improvements in mobility, sleep quality, and general well-being. The non-invasive nature of PEMF therapy makes it an attractive option for patients who may be hesitant about more invasive procedures or those who have exhausted other treatment options.
As research in this field progresses, the integration goals extend to developing standardized protocols that combine PEMF therapy with other modalities such as physical therapy, acupuncture, and cognitive-behavioral therapy. These integrated approaches seek to create tailored treatment plans that address the individual needs of patients, recognizing the complex and often multifactorial nature of chronic pain.
In conclusion, the integration of PEMF therapy with other pain management modalities represents a significant step towards a more holistic and effective approach to pain treatment. By leveraging the unique properties of electromagnetic fields in conjunction with established pain management techniques, healthcare providers aim to offer patients a more comprehensive and personalized path to pain relief and improved quality of life.
Market Analysis for Integrated Pain Management Solutions
The global pain management market is experiencing significant growth, driven by an aging population, increasing prevalence of chronic diseases, and a growing demand for non-invasive treatment options. Within this context, the integration of Pulsed Electromagnetic Field (PEMF) therapy with other pain management modalities presents a promising opportunity for market expansion and innovation.
The pain management market is projected to reach substantial value in the coming years, with a compound annual growth rate (CAGR) that reflects the increasing demand for effective pain relief solutions. This growth is particularly evident in developed regions such as North America and Europe, where healthcare infrastructure is advanced and there is a higher awareness of alternative therapies.
PEMF therapy, as a non-invasive and drug-free approach to pain management, is gaining traction among both healthcare providers and patients. Its potential to be integrated with other pain management modalities, such as physical therapy, acupuncture, and traditional pharmacological treatments, positions it as a versatile solution in the market.
The market for integrated pain management solutions that incorporate PEMF therapy is characterized by several key trends. There is a growing preference for multimodal approaches to pain management, which combine different therapies to achieve better outcomes. This trend aligns well with the integration of PEMF therapy into comprehensive pain management protocols.
Additionally, there is an increasing focus on personalized medicine in pain management. Integrated solutions that can be tailored to individual patient needs are likely to see higher adoption rates. PEMF therapy's adaptability to various pain conditions and its potential for customization make it an attractive component of personalized pain management strategies.
The market is also seeing a shift towards home-based and portable pain management solutions. This trend has been accelerated by recent global events, leading to a higher demand for treatments that can be administered outside of clinical settings. Integrated pain management solutions that incorporate PEMF therapy and are suitable for home use are likely to find a receptive market.
From a competitive landscape perspective, the market for integrated pain management solutions is diverse, with both established medical device manufacturers and innovative startups vying for market share. Companies that can successfully integrate PEMF therapy with other modalities and demonstrate clinical efficacy through robust studies are likely to gain a competitive edge.
Regulatory considerations play a significant role in shaping the market for integrated pain management solutions. As PEMF therapy gains more recognition, regulatory bodies are likely to develop more specific guidelines for its use in combination with other modalities. Companies that can navigate these regulatory challenges effectively will be well-positioned to capitalize on market opportunities.
The pain management market is projected to reach substantial value in the coming years, with a compound annual growth rate (CAGR) that reflects the increasing demand for effective pain relief solutions. This growth is particularly evident in developed regions such as North America and Europe, where healthcare infrastructure is advanced and there is a higher awareness of alternative therapies.
PEMF therapy, as a non-invasive and drug-free approach to pain management, is gaining traction among both healthcare providers and patients. Its potential to be integrated with other pain management modalities, such as physical therapy, acupuncture, and traditional pharmacological treatments, positions it as a versatile solution in the market.
The market for integrated pain management solutions that incorporate PEMF therapy is characterized by several key trends. There is a growing preference for multimodal approaches to pain management, which combine different therapies to achieve better outcomes. This trend aligns well with the integration of PEMF therapy into comprehensive pain management protocols.
Additionally, there is an increasing focus on personalized medicine in pain management. Integrated solutions that can be tailored to individual patient needs are likely to see higher adoption rates. PEMF therapy's adaptability to various pain conditions and its potential for customization make it an attractive component of personalized pain management strategies.
The market is also seeing a shift towards home-based and portable pain management solutions. This trend has been accelerated by recent global events, leading to a higher demand for treatments that can be administered outside of clinical settings. Integrated pain management solutions that incorporate PEMF therapy and are suitable for home use are likely to find a receptive market.
From a competitive landscape perspective, the market for integrated pain management solutions is diverse, with both established medical device manufacturers and innovative startups vying for market share. Companies that can successfully integrate PEMF therapy with other modalities and demonstrate clinical efficacy through robust studies are likely to gain a competitive edge.
Regulatory considerations play a significant role in shaping the market for integrated pain management solutions. As PEMF therapy gains more recognition, regulatory bodies are likely to develop more specific guidelines for its use in combination with other modalities. Companies that can navigate these regulatory challenges effectively will be well-positioned to capitalize on market opportunities.
Current PEMF Integration Challenges
The integration of Pulsed Electromagnetic Field (PEMF) therapy with other pain management modalities presents several challenges that need to be addressed for effective implementation. One of the primary obstacles is the lack of standardized protocols for combining PEMF with other treatments. This absence of established guidelines makes it difficult for healthcare providers to determine optimal treatment combinations, dosages, and timing.
Another significant challenge is the limited understanding of potential interactions between PEMF and other pain management techniques. While PEMF has shown promising results in various studies, its synergistic or antagonistic effects when used alongside pharmaceutical interventions, physical therapy, or other non-invasive treatments remain largely unexplored. This knowledge gap hinders the development of comprehensive, multi-modal pain management strategies that incorporate PEMF effectively.
The variability in PEMF devices and treatment parameters further complicates integration efforts. Different devices may produce varying electromagnetic field strengths, frequencies, and waveforms, making it challenging to establish consistent treatment protocols across different clinical settings. This lack of standardization also impedes the comparison of research results and the development of evidence-based guidelines for integrated pain management approaches.
Additionally, there is a shortage of trained professionals who are well-versed in both PEMF therapy and other pain management modalities. This skills gap can lead to suboptimal treatment combinations and missed opportunities for synergistic effects. The interdisciplinary nature of pain management requires healthcare providers to have a comprehensive understanding of various treatment options, including PEMF, to effectively integrate them into patient care plans.
Furthermore, the integration of PEMF therapy faces challenges related to reimbursement and insurance coverage. Many insurance providers do not yet recognize PEMF as a standard treatment option, making it difficult for patients to access this therapy as part of a comprehensive pain management program. This financial barrier can limit the widespread adoption and integration of PEMF in clinical practice.
Lastly, there is a need for more robust clinical evidence demonstrating the efficacy of integrated PEMF approaches. While individual studies have shown promising results, large-scale, randomized controlled trials examining the combined effects of PEMF with other pain management modalities are still lacking. This paucity of high-quality evidence makes it challenging to convince skeptical healthcare providers and policymakers of the value of integrating PEMF into mainstream pain management protocols.
Another significant challenge is the limited understanding of potential interactions between PEMF and other pain management techniques. While PEMF has shown promising results in various studies, its synergistic or antagonistic effects when used alongside pharmaceutical interventions, physical therapy, or other non-invasive treatments remain largely unexplored. This knowledge gap hinders the development of comprehensive, multi-modal pain management strategies that incorporate PEMF effectively.
The variability in PEMF devices and treatment parameters further complicates integration efforts. Different devices may produce varying electromagnetic field strengths, frequencies, and waveforms, making it challenging to establish consistent treatment protocols across different clinical settings. This lack of standardization also impedes the comparison of research results and the development of evidence-based guidelines for integrated pain management approaches.
Additionally, there is a shortage of trained professionals who are well-versed in both PEMF therapy and other pain management modalities. This skills gap can lead to suboptimal treatment combinations and missed opportunities for synergistic effects. The interdisciplinary nature of pain management requires healthcare providers to have a comprehensive understanding of various treatment options, including PEMF, to effectively integrate them into patient care plans.
Furthermore, the integration of PEMF therapy faces challenges related to reimbursement and insurance coverage. Many insurance providers do not yet recognize PEMF as a standard treatment option, making it difficult for patients to access this therapy as part of a comprehensive pain management program. This financial barrier can limit the widespread adoption and integration of PEMF in clinical practice.
Lastly, there is a need for more robust clinical evidence demonstrating the efficacy of integrated PEMF approaches. While individual studies have shown promising results, large-scale, randomized controlled trials examining the combined effects of PEMF with other pain management modalities are still lacking. This paucity of high-quality evidence makes it challenging to convince skeptical healthcare providers and policymakers of the value of integrating PEMF into mainstream pain management protocols.
Existing PEMF Integration Approaches
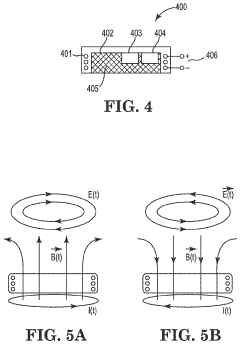
01 PEMF devices for pain management
Pulsed Electromagnetic Field (PEMF) therapy devices are designed specifically for pain management. These devices generate electromagnetic fields that penetrate the body, stimulating cellular activity and promoting healing. They can be used to treat various types of pain, including chronic pain, musculoskeletal pain, and post-operative pain.- PEMF devices for pain management: Pulsed Electromagnetic Field (PEMF) therapy devices are designed specifically for pain management. These devices generate electromagnetic fields that penetrate the body, stimulating cellular activity and promoting healing. They can be used to treat various types of pain, including chronic pain, musculoskeletal pain, and post-operative pain.
- Wearable PEMF devices for targeted pain relief: Wearable PEMF devices allow for targeted and continuous pain relief. These devices can be worn on specific body parts, providing localized electromagnetic therapy. They are designed for ease of use and mobility, allowing patients to receive treatment while going about their daily activities.
- PEMF therapy combined with other treatment modalities: PEMF therapy can be combined with other treatment modalities to enhance pain management. This may include integration with physical therapy, medication, or other forms of electromagnetic stimulation. The combination approach aims to provide more comprehensive and effective pain relief.
- Customizable PEMF treatment protocols: Advanced PEMF devices offer customizable treatment protocols for pain management. These systems allow for adjustment of frequency, intensity, and duration of electromagnetic pulses based on the specific needs of the patient and the type of pain being treated. This personalization can lead to more effective pain relief outcomes.
- PEMF therapy for specific pain conditions: PEMF therapy can be tailored for specific pain conditions such as arthritis, fibromyalgia, or neuropathic pain. Research and development in this area focus on optimizing PEMF parameters and treatment protocols for targeted pain relief in these specific conditions, potentially offering more effective alternatives to traditional pain management approaches.
02 Wearable PEMF devices for continuous therapy
Wearable PEMF devices allow for continuous pain management therapy. These portable devices can be worn on specific body parts, providing targeted electromagnetic field therapy throughout the day. This approach enables patients to receive ongoing treatment while maintaining mobility and carrying out daily activities.Expand Specific Solutions03 Combination of PEMF with other therapies
PEMF therapy can be combined with other treatment modalities for enhanced pain management. This may include integration with physical therapy, medication, or other forms of electromagnetic stimulation. The synergistic effect of combined therapies can potentially provide more effective pain relief and improved patient outcomes.Expand Specific Solutions04 Customizable PEMF treatment protocols
Advanced PEMF devices offer customizable treatment protocols for pain management. These systems allow healthcare providers to adjust parameters such as frequency, intensity, and duration of electromagnetic pulses based on individual patient needs and specific pain conditions. This personalized approach aims to optimize treatment efficacy and patient comfort.Expand Specific Solutions05 PEMF therapy for specific pain conditions
PEMF therapy can be tailored to address specific pain conditions. Research and development efforts focus on optimizing PEMF parameters for targeted treatment of conditions such as arthritis, fibromyalgia, neuropathic pain, and sports-related injuries. This specialized approach aims to improve the effectiveness of PEMF therapy in managing diverse pain syndromes.Expand Specific Solutions
Key Players in PEMF and Pain Management
The integration of PEMF therapy with other pain management modalities is an emerging field in the healthcare industry, currently in its growth phase. The market size is expanding as more healthcare providers recognize the potential of combining PEMF with traditional pain management techniques. Technologically, the field is advancing rapidly, with companies like Regenesis Biomedical and SofPulse leading the way in developing innovative PEMF devices. Medtronic, a major player in medical technology, is also contributing to the field's maturation. The technology's integration with other modalities is still evolving, with research institutions like the National University of Singapore and the Swiss Federal Institute of Technology playing crucial roles in advancing the scientific understanding and clinical applications of combined therapies.
Regenesis Biomedical, Inc.
Technical Solution: Regenesis Biomedical has developed a PEMF therapy system that integrates seamlessly with other pain management modalities. Their Provant Therapy System utilizes a specific PEMF signal that has been shown to reduce pain and promote healing at the cellular level[7]. The company has focused on creating protocols that allow for the concurrent use of their PEMF technology with other treatments such as physical therapy, medication management, and cognitive behavioral therapy. Regenesis has also developed a portable PEMF device that can be used in conjunction with traditional pain management techniques, allowing for continuous treatment both in clinical settings and at home[8]. Their approach emphasizes patient education and engagement, with a comprehensive support system to ensure proper integration of PEMF therapy into overall pain management strategies[9].
Strengths: Portable and versatile PEMF system that complements existing pain management techniques. Strong focus on patient education and support. Weaknesses: May be less comprehensive than multi-modal systems offered by larger companies. Effectiveness may vary depending on the integration with other modalities.
SofPulse, Inc.
Technical Solution: SofPulse has developed a unique approach to integrating PEMF therapy with other pain management modalities, focusing on post-operative pain and recovery. Their system utilizes a targeted PEMF signal that is specifically calibrated to reduce inflammation and accelerate healing in surgical sites[10]. SofPulse's technology is designed to be used in conjunction with standard post-operative care, including medication management and physical therapy. The company has developed protocols for integrating their PEMF devices with patient-controlled analgesia (PCA) systems, allowing for a synergistic approach to pain management[11]. SofPulse's devices are compact and wearable, enabling continuous treatment during the critical post-operative period, both in hospital settings and during home recovery[12].
Strengths: Specialized focus on post-operative pain management. Easily integrates with existing post-operative care protocols. Weaknesses: May have limited application outside of surgical recovery contexts. Effectiveness may depend on proper integration with other post-operative care elements.
Core PEMF Integration Technologies
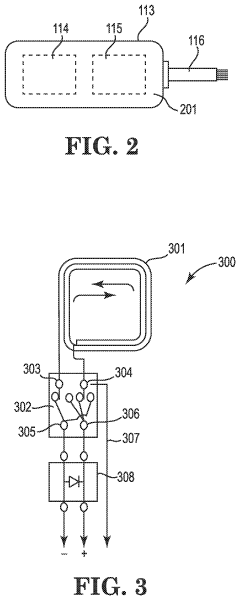
Pulsed Electromagnetic Field Devices Integrated into Adjustable Clothing
PatentPendingUS20230104434A1
Innovation
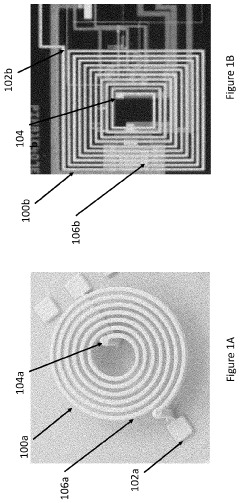
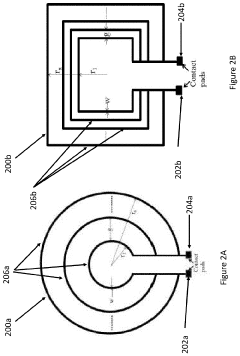
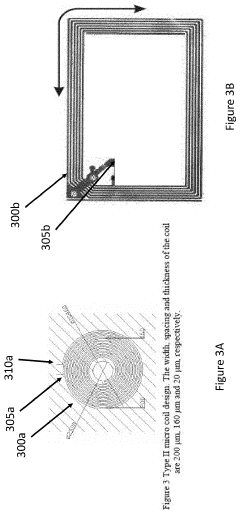
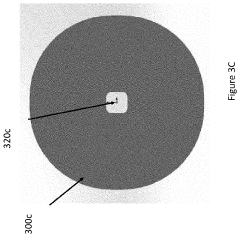
- A pulsed electromagnetic field device integrated into wearable clothing, using arrays of planar microcoils that generate controlled, homogenous magnetic fields, allowing for comfortable, long-term use and targeted treatment of various brain-related disorders and conditions.
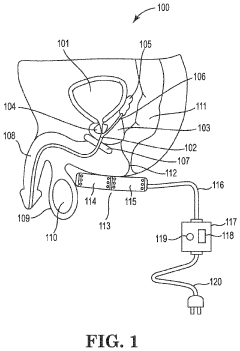
Method and apparatus for treatment of benign prostatic hyperplasia (BPH)
PatentInactiveUS20230398368A1
Innovation
- A non-invasive method utilizing pulsed electromagnetic field (PEMF) stimulation to increase the number of A2a receptors on cell membranes, enhancing the anti-inflammatory effects of adenosine and providing immunosuppressive action to reduce chronic inflammation and tissue damage in the prostate.
Safety and Efficacy Considerations
When integrating PEMF therapy with other pain management modalities, safety and efficacy considerations are paramount. The combination of PEMF with traditional pain management techniques requires careful evaluation to ensure optimal patient outcomes and minimize potential risks.
One primary safety concern is the potential interaction between PEMF devices and other medical implants or devices. Patients with pacemakers, defibrillators, or other electronic implants should be thoroughly assessed before undergoing PEMF therapy in conjunction with their existing treatments. Healthcare providers must conduct comprehensive screenings to identify any contraindications and adjust treatment plans accordingly.
Efficacy considerations involve determining the most beneficial combination of PEMF therapy with other pain management modalities. This requires a thorough understanding of the mechanisms of action for both PEMF and the complementary treatments. For instance, when combining PEMF with pharmacological interventions, practitioners must consider potential synergistic effects or interactions that could enhance or diminish the overall therapeutic impact.
The dosage and timing of PEMF therapy in relation to other treatments are critical factors affecting both safety and efficacy. Establishing optimal treatment protocols that integrate PEMF with modalities such as physical therapy, acupuncture, or medication regimens is essential. This may involve adjusting the frequency, intensity, and duration of PEMF sessions to complement the effects of concurrent therapies.
Long-term safety monitoring is crucial when implementing integrated pain management approaches. Regular follow-ups and assessments should be conducted to evaluate the cumulative effects of combined treatments and identify any adverse reactions or unexpected outcomes. This ongoing monitoring allows for timely adjustments to the treatment plan and ensures patient safety throughout the course of therapy.
Efficacy evaluation in integrated pain management approaches presents unique challenges. Developing standardized assessment tools and protocols that can accurately measure the combined effects of PEMF and other modalities is essential. This may involve utilizing a combination of objective pain scales, functional assessments, and patient-reported outcomes to comprehensively evaluate treatment efficacy.
Patient education plays a vital role in ensuring both safety and efficacy when integrating PEMF therapy. Providing clear instructions on proper use of PEMF devices, potential side effects, and expected outcomes helps patients actively participate in their treatment and report any concerns promptly. This collaborative approach enhances treatment adherence and allows for more accurate monitoring of safety and efficacy.
One primary safety concern is the potential interaction between PEMF devices and other medical implants or devices. Patients with pacemakers, defibrillators, or other electronic implants should be thoroughly assessed before undergoing PEMF therapy in conjunction with their existing treatments. Healthcare providers must conduct comprehensive screenings to identify any contraindications and adjust treatment plans accordingly.
Efficacy considerations involve determining the most beneficial combination of PEMF therapy with other pain management modalities. This requires a thorough understanding of the mechanisms of action for both PEMF and the complementary treatments. For instance, when combining PEMF with pharmacological interventions, practitioners must consider potential synergistic effects or interactions that could enhance or diminish the overall therapeutic impact.
The dosage and timing of PEMF therapy in relation to other treatments are critical factors affecting both safety and efficacy. Establishing optimal treatment protocols that integrate PEMF with modalities such as physical therapy, acupuncture, or medication regimens is essential. This may involve adjusting the frequency, intensity, and duration of PEMF sessions to complement the effects of concurrent therapies.
Long-term safety monitoring is crucial when implementing integrated pain management approaches. Regular follow-ups and assessments should be conducted to evaluate the cumulative effects of combined treatments and identify any adverse reactions or unexpected outcomes. This ongoing monitoring allows for timely adjustments to the treatment plan and ensures patient safety throughout the course of therapy.
Efficacy evaluation in integrated pain management approaches presents unique challenges. Developing standardized assessment tools and protocols that can accurately measure the combined effects of PEMF and other modalities is essential. This may involve utilizing a combination of objective pain scales, functional assessments, and patient-reported outcomes to comprehensively evaluate treatment efficacy.
Patient education plays a vital role in ensuring both safety and efficacy when integrating PEMF therapy. Providing clear instructions on proper use of PEMF devices, potential side effects, and expected outcomes helps patients actively participate in their treatment and report any concerns promptly. This collaborative approach enhances treatment adherence and allows for more accurate monitoring of safety and efficacy.
Reimbursement Landscape for Integrated Therapies
The reimbursement landscape for integrated therapies combining PEMF (Pulsed Electromagnetic Field) therapy with other pain management modalities is complex and evolving. Currently, most insurance providers do not offer comprehensive coverage for PEMF therapy as a standalone treatment, let alone in combination with other modalities. This is primarily due to the lack of widespread recognition of PEMF as a standard medical treatment by regulatory bodies.
However, there is a growing trend towards more holistic and integrative approaches to pain management, which may eventually lead to changes in reimbursement policies. Some insurance companies are beginning to recognize the potential cost-effectiveness of integrated therapies in reducing long-term healthcare expenses associated with chronic pain management.
For integrated therapies involving PEMF, reimbursement is often handled on a case-by-case basis. Patients may need to obtain pre-authorization from their insurance provider, demonstrating medical necessity through documented failure of conventional treatments. In some instances, coverage may be provided under broader categories such as physical therapy or pain management services, rather than specifically for PEMF therapy.
Medicare and Medicaid generally do not cover PEMF therapy for pain management, except in specific cases such as bone healing. Private insurers vary widely in their coverage policies, with some offering limited reimbursement for PEMF devices when prescribed by a licensed healthcare provider for specific conditions.
To improve the reimbursement landscape, ongoing clinical research is crucial. Studies demonstrating the efficacy and cost-effectiveness of integrated therapies involving PEMF could potentially influence policy changes. Healthcare providers and medical device manufacturers are actively engaging with insurance companies and policymakers to advocate for expanded coverage.
Some innovative reimbursement models are emerging, such as value-based care arrangements, where providers are reimbursed based on patient outcomes rather than specific treatments. This approach could potentially benefit integrated therapies that demonstrate improved patient outcomes and reduced overall healthcare costs.
For patients, out-of-pocket expenses remain a significant consideration. Many turn to flexible spending accounts (FSAs) or health savings accounts (HSAs) to cover the costs of integrated therapies not fully reimbursed by insurance. Some providers offer payment plans or package deals for combined treatment modalities to make them more accessible.
As the field of integrative medicine continues to grow, it is likely that the reimbursement landscape for combined therapies including PEMF will evolve. Stakeholders in the healthcare industry are working towards creating more comprehensive and flexible reimbursement models that can accommodate innovative, multi-modal approaches to pain management.
However, there is a growing trend towards more holistic and integrative approaches to pain management, which may eventually lead to changes in reimbursement policies. Some insurance companies are beginning to recognize the potential cost-effectiveness of integrated therapies in reducing long-term healthcare expenses associated with chronic pain management.
For integrated therapies involving PEMF, reimbursement is often handled on a case-by-case basis. Patients may need to obtain pre-authorization from their insurance provider, demonstrating medical necessity through documented failure of conventional treatments. In some instances, coverage may be provided under broader categories such as physical therapy or pain management services, rather than specifically for PEMF therapy.
Medicare and Medicaid generally do not cover PEMF therapy for pain management, except in specific cases such as bone healing. Private insurers vary widely in their coverage policies, with some offering limited reimbursement for PEMF devices when prescribed by a licensed healthcare provider for specific conditions.
To improve the reimbursement landscape, ongoing clinical research is crucial. Studies demonstrating the efficacy and cost-effectiveness of integrated therapies involving PEMF could potentially influence policy changes. Healthcare providers and medical device manufacturers are actively engaging with insurance companies and policymakers to advocate for expanded coverage.
Some innovative reimbursement models are emerging, such as value-based care arrangements, where providers are reimbursed based on patient outcomes rather than specific treatments. This approach could potentially benefit integrated therapies that demonstrate improved patient outcomes and reduced overall healthcare costs.
For patients, out-of-pocket expenses remain a significant consideration. Many turn to flexible spending accounts (FSAs) or health savings accounts (HSAs) to cover the costs of integrated therapies not fully reimbursed by insurance. Some providers offer payment plans or package deals for combined treatment modalities to make them more accessible.
As the field of integrative medicine continues to grow, it is likely that the reimbursement landscape for combined therapies including PEMF will evolve. Stakeholders in the healthcare industry are working towards creating more comprehensive and flexible reimbursement models that can accommodate innovative, multi-modal approaches to pain management.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!