Innovations in PEMF Therapy for Oncological Supportive Care
AUG 11, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
PEMF Therapy Evolution
Pulsed Electromagnetic Field (PEMF) therapy has undergone significant evolution since its inception in the mid-20th century. Initially developed for bone healing, PEMF therapy has expanded its applications to various medical fields, including oncological supportive care. The therapy's evolution can be traced through several key phases, each marked by technological advancements and broadening clinical applications.
In the 1950s and 1960s, researchers began exploring the effects of electromagnetic fields on biological systems. Early studies focused on bone healing, with pioneering work by Dr. Andrew Bassett demonstrating the potential of PEMF to stimulate bone formation. This laid the foundation for the first FDA-approved PEMF device for bone healing in 1979.
The 1980s and 1990s saw an expansion of PEMF research into other areas of medicine. Scientists began investigating its potential in pain management, wound healing, and neurological disorders. During this period, technological improvements led to more compact and user-friendly PEMF devices, making the therapy more accessible for clinical and home use.
The turn of the millennium marked a new era for PEMF therapy, with increased focus on its potential in cancer care. Researchers began exploring PEMF's effects on cancer cells, tumor growth, and treatment-related side effects. Studies indicated that PEMF could potentially enhance the efficacy of chemotherapy and radiation therapy while reducing their side effects.
In recent years, PEMF therapy has seen significant advancements in device technology and treatment protocols. Modern PEMF devices offer precise control over field strength, frequency, and waveform, allowing for more targeted and personalized treatments. The integration of digital technology has enabled better monitoring and adjustment of treatment parameters.
The application of PEMF in oncological supportive care has become a particular area of interest. Recent studies have investigated its potential in managing cancer-related fatigue, pain, and quality of life issues. Researchers are also exploring PEMF's role in enhancing immune function and reducing inflammation in cancer patients.
As PEMF therapy continues to evolve, there is growing interest in combining it with other treatment modalities. Ongoing research is exploring synergistic effects between PEMF and immunotherapy, targeted drug delivery, and other emerging cancer treatments. This integrative approach holds promise for enhancing overall treatment outcomes and patient well-being.
The evolution of PEMF therapy reflects a broader trend towards non-invasive, patient-friendly treatment options in oncology. As research progresses, PEMF therapy is poised to play an increasingly important role in comprehensive cancer care, offering new possibilities for improving treatment efficacy and quality of life for cancer patients.
In the 1950s and 1960s, researchers began exploring the effects of electromagnetic fields on biological systems. Early studies focused on bone healing, with pioneering work by Dr. Andrew Bassett demonstrating the potential of PEMF to stimulate bone formation. This laid the foundation for the first FDA-approved PEMF device for bone healing in 1979.
The 1980s and 1990s saw an expansion of PEMF research into other areas of medicine. Scientists began investigating its potential in pain management, wound healing, and neurological disorders. During this period, technological improvements led to more compact and user-friendly PEMF devices, making the therapy more accessible for clinical and home use.
The turn of the millennium marked a new era for PEMF therapy, with increased focus on its potential in cancer care. Researchers began exploring PEMF's effects on cancer cells, tumor growth, and treatment-related side effects. Studies indicated that PEMF could potentially enhance the efficacy of chemotherapy and radiation therapy while reducing their side effects.
In recent years, PEMF therapy has seen significant advancements in device technology and treatment protocols. Modern PEMF devices offer precise control over field strength, frequency, and waveform, allowing for more targeted and personalized treatments. The integration of digital technology has enabled better monitoring and adjustment of treatment parameters.
The application of PEMF in oncological supportive care has become a particular area of interest. Recent studies have investigated its potential in managing cancer-related fatigue, pain, and quality of life issues. Researchers are also exploring PEMF's role in enhancing immune function and reducing inflammation in cancer patients.
As PEMF therapy continues to evolve, there is growing interest in combining it with other treatment modalities. Ongoing research is exploring synergistic effects between PEMF and immunotherapy, targeted drug delivery, and other emerging cancer treatments. This integrative approach holds promise for enhancing overall treatment outcomes and patient well-being.
The evolution of PEMF therapy reflects a broader trend towards non-invasive, patient-friendly treatment options in oncology. As research progresses, PEMF therapy is poised to play an increasingly important role in comprehensive cancer care, offering new possibilities for improving treatment efficacy and quality of life for cancer patients.
Oncology Support Needs
Cancer patients face numerous challenges during their treatment journey, necessitating comprehensive supportive care to address their physical, emotional, and psychological needs. Oncology support needs encompass a wide range of interventions aimed at improving quality of life, managing treatment side effects, and enhancing overall well-being.
Pain management is a critical aspect of oncological supportive care. Cancer-related pain can significantly impact a patient's daily activities and quality of life. Effective pain control strategies, including pharmacological and non-pharmacological approaches, are essential to alleviate suffering and improve functional status.
Fatigue is another prevalent issue among cancer patients, affecting up to 90% of individuals undergoing treatment. Addressing cancer-related fatigue requires a multifaceted approach, incorporating exercise interventions, energy conservation techniques, and psychological support to help patients cope with this debilitating symptom.
Nausea and vomiting, common side effects of chemotherapy and radiation therapy, can severely impact a patient's nutritional status and quality of life. Antiemetic medications, dietary modifications, and complementary therapies are crucial components of managing these symptoms effectively.
Emotional and psychological support is paramount in oncological care. Cancer diagnosis and treatment can lead to anxiety, depression, and other mental health challenges. Providing access to counseling services, support groups, and psychosocial interventions helps patients navigate the emotional complexities of their cancer journey.
Nutritional support plays a vital role in maintaining patients' strength and resilience during treatment. Cancer and its therapies can significantly impact appetite and nutritional status. Tailored dietary interventions, nutritional supplements, and feeding assistance may be necessary to prevent malnutrition and support optimal treatment outcomes.
Palliative care, focusing on symptom management and quality of life improvement, is an integral part of oncological supportive care. Early integration of palliative care services has been shown to enhance patient outcomes and satisfaction with care.
As cancer treatments advance, long-term survivorship care becomes increasingly important. Addressing the unique needs of cancer survivors, including managing late effects of treatment, surveillance for recurrence, and psychosocial support, is essential for comprehensive oncological care.
Innovations in supportive care technologies, such as PEMF therapy, offer promising avenues for addressing these multifaceted needs. By potentially alleviating pain, reducing fatigue, and improving overall well-being, novel interventions like PEMF therapy may complement existing supportive care strategies and enhance the quality of life for cancer patients throughout their treatment journey.
Pain management is a critical aspect of oncological supportive care. Cancer-related pain can significantly impact a patient's daily activities and quality of life. Effective pain control strategies, including pharmacological and non-pharmacological approaches, are essential to alleviate suffering and improve functional status.
Fatigue is another prevalent issue among cancer patients, affecting up to 90% of individuals undergoing treatment. Addressing cancer-related fatigue requires a multifaceted approach, incorporating exercise interventions, energy conservation techniques, and psychological support to help patients cope with this debilitating symptom.
Nausea and vomiting, common side effects of chemotherapy and radiation therapy, can severely impact a patient's nutritional status and quality of life. Antiemetic medications, dietary modifications, and complementary therapies are crucial components of managing these symptoms effectively.
Emotional and psychological support is paramount in oncological care. Cancer diagnosis and treatment can lead to anxiety, depression, and other mental health challenges. Providing access to counseling services, support groups, and psychosocial interventions helps patients navigate the emotional complexities of their cancer journey.
Nutritional support plays a vital role in maintaining patients' strength and resilience during treatment. Cancer and its therapies can significantly impact appetite and nutritional status. Tailored dietary interventions, nutritional supplements, and feeding assistance may be necessary to prevent malnutrition and support optimal treatment outcomes.
Palliative care, focusing on symptom management and quality of life improvement, is an integral part of oncological supportive care. Early integration of palliative care services has been shown to enhance patient outcomes and satisfaction with care.
As cancer treatments advance, long-term survivorship care becomes increasingly important. Addressing the unique needs of cancer survivors, including managing late effects of treatment, surveillance for recurrence, and psychosocial support, is essential for comprehensive oncological care.
Innovations in supportive care technologies, such as PEMF therapy, offer promising avenues for addressing these multifaceted needs. By potentially alleviating pain, reducing fatigue, and improving overall well-being, novel interventions like PEMF therapy may complement existing supportive care strategies and enhance the quality of life for cancer patients throughout their treatment journey.
PEMF in Cancer Care
Pulsed Electromagnetic Field (PEMF) therapy has emerged as a promising complementary approach in cancer care, offering potential benefits for patients undergoing oncological treatments. This non-invasive technique utilizes low-frequency electromagnetic fields to stimulate cellular activity and promote healing processes. In the context of cancer care, PEMF therapy has shown potential in alleviating various side effects associated with conventional cancer treatments, such as chemotherapy and radiation therapy.
The application of PEMF in oncological supportive care is based on its ability to influence cellular processes at the molecular level. Research has demonstrated that PEMF can modulate cell membrane potential, enhance cellular energy production, and influence various signaling pathways involved in cell growth and differentiation. These mechanisms may contribute to the reduction of inflammation, improvement of tissue oxygenation, and enhancement of the body's natural healing processes.
One of the primary areas where PEMF therapy has shown promise in cancer care is in managing treatment-related side effects. Studies have reported potential benefits in reducing chemotherapy-induced nausea and vomiting, alleviating cancer-related fatigue, and improving overall quality of life for cancer patients. Additionally, PEMF therapy has been investigated for its potential to enhance the efficacy of conventional cancer treatments by increasing tumor oxygenation and sensitizing cancer cells to radiation and chemotherapy.
The integration of PEMF therapy into cancer care protocols is still in its early stages, with ongoing research aimed at optimizing treatment parameters and understanding the full spectrum of its effects. Clinical trials have explored various PEMF protocols, including different frequencies, intensities, and treatment durations, to determine the most effective approaches for specific cancer-related conditions. While results have been promising, more extensive studies are needed to establish standardized protocols and validate the long-term efficacy and safety of PEMF therapy in oncological settings.
It is important to note that PEMF therapy is not intended as a standalone treatment for cancer but rather as a complementary approach to support conventional therapies and improve patient outcomes. The potential of PEMF in cancer care extends beyond symptom management, with ongoing investigations into its possible role in enhancing immune function, promoting tissue repair, and even directly influencing tumor growth. As research in this field progresses, PEMF therapy may become an increasingly valuable tool in the comprehensive care of cancer patients, offering a non-pharmacological option to improve treatment outcomes and quality of life.
The application of PEMF in oncological supportive care is based on its ability to influence cellular processes at the molecular level. Research has demonstrated that PEMF can modulate cell membrane potential, enhance cellular energy production, and influence various signaling pathways involved in cell growth and differentiation. These mechanisms may contribute to the reduction of inflammation, improvement of tissue oxygenation, and enhancement of the body's natural healing processes.
One of the primary areas where PEMF therapy has shown promise in cancer care is in managing treatment-related side effects. Studies have reported potential benefits in reducing chemotherapy-induced nausea and vomiting, alleviating cancer-related fatigue, and improving overall quality of life for cancer patients. Additionally, PEMF therapy has been investigated for its potential to enhance the efficacy of conventional cancer treatments by increasing tumor oxygenation and sensitizing cancer cells to radiation and chemotherapy.
The integration of PEMF therapy into cancer care protocols is still in its early stages, with ongoing research aimed at optimizing treatment parameters and understanding the full spectrum of its effects. Clinical trials have explored various PEMF protocols, including different frequencies, intensities, and treatment durations, to determine the most effective approaches for specific cancer-related conditions. While results have been promising, more extensive studies are needed to establish standardized protocols and validate the long-term efficacy and safety of PEMF therapy in oncological settings.
It is important to note that PEMF therapy is not intended as a standalone treatment for cancer but rather as a complementary approach to support conventional therapies and improve patient outcomes. The potential of PEMF in cancer care extends beyond symptom management, with ongoing investigations into its possible role in enhancing immune function, promoting tissue repair, and even directly influencing tumor growth. As research in this field progresses, PEMF therapy may become an increasingly valuable tool in the comprehensive care of cancer patients, offering a non-pharmacological option to improve treatment outcomes and quality of life.
Current PEMF Solutions
01 PEMF devices for therapeutic applications
Pulsed Electromagnetic Field (PEMF) therapy devices are designed for various therapeutic applications. These devices generate electromagnetic fields to stimulate cellular activity and promote healing. They can be used for pain management, tissue repair, and improving overall well-being.- PEMF devices for therapeutic applications: Pulsed Electromagnetic Field (PEMF) therapy devices are designed for various therapeutic applications. These devices generate electromagnetic fields to stimulate cellular repair and improve overall health. They can be used for pain management, tissue healing, and treating various medical conditions.
- PEMF therapy for specific medical conditions: PEMF therapy is utilized to treat specific medical conditions such as osteoarthritis, bone fractures, and neurological disorders. The therapy aims to reduce inflammation, promote tissue regeneration, and alleviate symptoms associated with these conditions. Specialized PEMF devices are developed to target specific areas of the body or particular health issues.
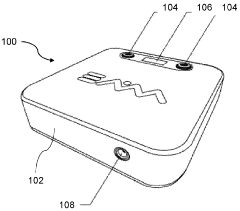
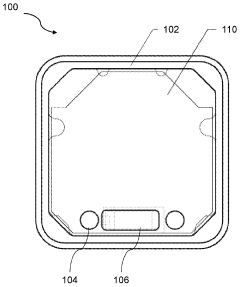
- Wearable PEMF devices: Wearable PEMF devices are designed for convenient and continuous therapy. These devices can be worn on various parts of the body, allowing for targeted treatment while the user goes about their daily activities. Wearable PEMF devices often incorporate flexible materials and compact designs for improved comfort and usability.
- PEMF therapy combined with other treatments: PEMF therapy is often combined with other treatment modalities to enhance therapeutic effects. This may include integration with light therapy, heat therapy, or other forms of electromagnetic stimulation. The combination of treatments aims to provide synergistic benefits and improve overall treatment outcomes.
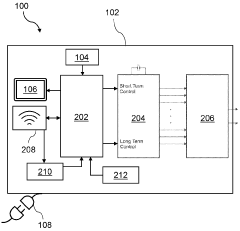
- Advanced PEMF control systems: Advanced control systems are developed for PEMF devices to optimize treatment parameters. These systems may include programmable settings, real-time monitoring, and adaptive algorithms to adjust the electromagnetic field based on the patient's response or specific treatment requirements. Such advancements aim to improve the efficacy and personalization of PEMF therapy.
02 PEMF therapy for specific medical conditions
PEMF therapy is utilized to treat specific medical conditions. It has shown efficacy in addressing issues such as musculoskeletal disorders, neurological conditions, and wound healing. The therapy can be tailored to target particular areas of the body or specific health concerns.Expand Specific Solutions03 Advancements in PEMF technology
Recent advancements in PEMF technology have led to more sophisticated and efficient devices. These improvements include better control over field intensity, frequency modulation, and treatment protocols. New designs also focus on portability and ease of use for home-based treatments.Expand Specific Solutions04 Combination of PEMF with other therapies
PEMF therapy is often combined with other treatment modalities to enhance therapeutic outcomes. This may include integration with physical therapy, acupuncture, or other forms of electromagnetic therapies. The synergistic effects can potentially improve treatment efficacy for various conditions.Expand Specific Solutions05 PEMF applications in non-medical fields
PEMF technology has found applications beyond medical treatments. It is being explored in areas such as agriculture for plant growth stimulation, animal husbandry for livestock health, and even in certain industrial processes. These diverse applications showcase the versatility of PEMF technology.Expand Specific Solutions
PEMF Device Manufacturers
The competitive landscape for innovations in PEMF therapy for oncological supportive care is in an early growth stage, with increasing market potential as cancer prevalence rises globally. The market size is expanding, driven by growing awareness of PEMF's benefits in managing cancer-related symptoms. Technologically, the field is evolving rapidly, with companies like Venus Concept Ltd. and Regenesis Biomedical leading in device development. Academic institutions such as Northwestern University and Fudan University are contributing to research advancements. Pharmaceutical giants like Boehringer Ingelheim and Novartis are exploring PEMF applications in oncology, indicating growing industry interest. Overall, the sector shows promise but requires further clinical validation and regulatory approvals to reach maturity.
Venus Concept Ltd.
Technical Solution: Venus Concept has developed innovative PEMF therapy devices for oncological supportive care. Their technology utilizes precise electromagnetic pulses to stimulate cellular repair and reduce inflammation in cancer patients. The company's PEMF devices are designed to deliver targeted therapy to specific areas affected by cancer treatments, potentially reducing side effects and improving quality of life. Venus Concept's PEMF systems incorporate advanced frequency modulation techniques to optimize energy delivery and enhance therapeutic outcomes[1]. The devices are equipped with user-friendly interfaces and customizable treatment protocols to address individual patient needs in oncology settings[3].
Strengths: Targeted therapy for cancer-related symptoms, customizable protocols, and user-friendly design. Weaknesses: Limited long-term clinical data specific to oncology applications, potential for electromagnetic interference with other medical devices.
Regenesis Biomedical, Inc.
Technical Solution: Regenesis Biomedical has developed a proprietary PEMF technology called Provant Therapy System for oncological supportive care. Their approach focuses on using specific pulsed electromagnetic fields to promote tissue repair and reduce pain in cancer patients. The Provant system delivers non-invasive PEMF therapy through a wearable applicator, allowing for convenient at-home use. Regenesis' technology is based on a unique waveform that has been shown to stimulate cellular activity and enhance the body's natural healing processes[2]. The company has conducted clinical studies demonstrating the efficacy of their PEMF therapy in managing cancer-related symptoms, particularly in reducing pain and improving function in patients undergoing cancer treatments[4].
Strengths: Portable and user-friendly design for at-home use, specific waveform technology tailored for tissue repair. Weaknesses: May require longer treatment sessions compared to some other PEMF devices, limited coverage area per applicator.
Key PEMF Innovations
Pulsed Electromagnetic Field (PEMF) Therapy Whole Body Wellness Device to increase cells energy, strengthen immune system and promote cell regeneration
PatentInactiveUS20190054308A1
Innovation
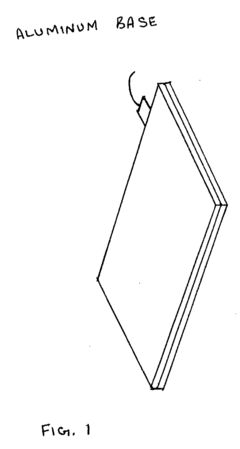
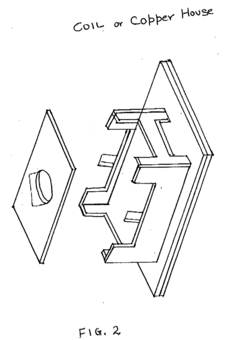
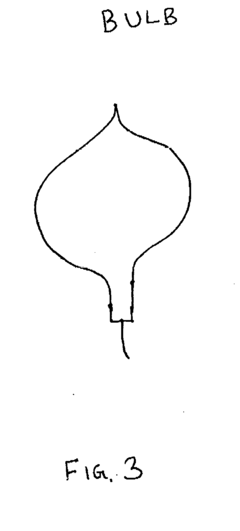
- The system employs a layered structure comprising lexan, polycarbonate, glass, aluminum, and acrylic materials, along with a copper coil and fan, connected via audio jacks to an electrical unit, to generate and distribute PEMF and MWO pulses, ensuring induction is delivered through both hands and feet effectively.
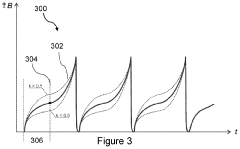
A pulsed electromagnetic field apparatus and method for generating frequencies
PatentWO2024127242A1
Innovation
- A PEMF apparatus with a pulse generator and electromagnetic field generation means that uses modified sawtooth waveforms with pre-stress and relaxation periods, and quasi-sine signals with pulse width modulation, along with a feedback circuit for frequency stability and precision, and a bifilar antenna for scalar wave generation.
Clinical Trial Landscape
The clinical trial landscape for Pulsed Electromagnetic Field (PEMF) therapy in oncological supportive care has been evolving rapidly in recent years. A growing number of studies are exploring the potential benefits of PEMF in managing cancer-related symptoms and improving quality of life for patients undergoing cancer treatment.
Several ongoing clinical trials are investigating the efficacy of PEMF therapy in reducing chemotherapy-induced peripheral neuropathy (CIPN), a common and debilitating side effect of cancer treatment. These studies aim to determine optimal PEMF parameters, treatment duration, and long-term outcomes in alleviating CIPN symptoms.
Another area of focus in clinical trials is the use of PEMF therapy for cancer-related fatigue. Researchers are examining the potential of PEMF to enhance energy levels, improve physical function, and reduce fatigue in cancer patients undergoing various treatments. These trials are exploring different PEMF protocols and their impact on patient-reported outcomes.
Clinical studies are also investigating the role of PEMF therapy in managing cancer-related pain. Trials are assessing the effectiveness of PEMF in reducing pain intensity, improving pain management, and potentially reducing the need for analgesic medications in cancer patients.
Furthermore, several ongoing trials are exploring the potential of PEMF therapy in enhancing the efficacy of conventional cancer treatments. These studies aim to determine whether PEMF can sensitize cancer cells to chemotherapy or radiation therapy, potentially improving treatment outcomes while minimizing side effects.
The clinical trial landscape also includes studies investigating the safety profile of PEMF therapy in cancer patients. These trials are crucial in establishing the long-term safety and potential contraindications of PEMF use in oncological supportive care.
Multi-center, randomized controlled trials are becoming more prevalent in the PEMF clinical trial landscape. These larger-scale studies aim to provide more robust evidence on the efficacy and safety of PEMF therapy in various aspects of cancer supportive care.
Lastly, there is a growing interest in personalized PEMF therapy approaches. Clinical trials are exploring how individual patient characteristics, cancer types, and treatment regimens may influence the effectiveness of PEMF therapy, paving the way for more tailored supportive care strategies in oncology.
Several ongoing clinical trials are investigating the efficacy of PEMF therapy in reducing chemotherapy-induced peripheral neuropathy (CIPN), a common and debilitating side effect of cancer treatment. These studies aim to determine optimal PEMF parameters, treatment duration, and long-term outcomes in alleviating CIPN symptoms.
Another area of focus in clinical trials is the use of PEMF therapy for cancer-related fatigue. Researchers are examining the potential of PEMF to enhance energy levels, improve physical function, and reduce fatigue in cancer patients undergoing various treatments. These trials are exploring different PEMF protocols and their impact on patient-reported outcomes.
Clinical studies are also investigating the role of PEMF therapy in managing cancer-related pain. Trials are assessing the effectiveness of PEMF in reducing pain intensity, improving pain management, and potentially reducing the need for analgesic medications in cancer patients.
Furthermore, several ongoing trials are exploring the potential of PEMF therapy in enhancing the efficacy of conventional cancer treatments. These studies aim to determine whether PEMF can sensitize cancer cells to chemotherapy or radiation therapy, potentially improving treatment outcomes while minimizing side effects.
The clinical trial landscape also includes studies investigating the safety profile of PEMF therapy in cancer patients. These trials are crucial in establishing the long-term safety and potential contraindications of PEMF use in oncological supportive care.
Multi-center, randomized controlled trials are becoming more prevalent in the PEMF clinical trial landscape. These larger-scale studies aim to provide more robust evidence on the efficacy and safety of PEMF therapy in various aspects of cancer supportive care.
Lastly, there is a growing interest in personalized PEMF therapy approaches. Clinical trials are exploring how individual patient characteristics, cancer types, and treatment regimens may influence the effectiveness of PEMF therapy, paving the way for more tailored supportive care strategies in oncology.
Safety and Regulations
The safety and regulatory landscape surrounding Pulsed Electromagnetic Field (PEMF) therapy in oncological supportive care is complex and evolving. As PEMF technology advances and its applications in cancer treatment expand, regulatory bodies worldwide are closely monitoring its development to ensure patient safety and efficacy.
In the United States, the Food and Drug Administration (FDA) has classified PEMF devices into different categories based on their intended use and potential risks. For oncological supportive care, PEMF devices are typically classified as Class II medical devices, requiring premarket notification (510(k)) clearance. This process involves demonstrating substantial equivalence to a legally marketed predicate device, ensuring that new PEMF devices meet established safety and effectiveness standards.
The European Union has implemented the Medical Device Regulation (MDR), which came into full effect in May 2021. Under this framework, PEMF devices for oncological supportive care are subject to rigorous conformity assessment procedures. Manufacturers must demonstrate compliance with essential safety and performance requirements, conduct clinical evaluations, and implement a comprehensive quality management system.
Safety considerations for PEMF therapy in oncological care include potential interactions with other medical devices, such as pacemakers or implanted defibrillators. Regulatory bodies require manufacturers to provide clear contraindications and warnings in device labeling and user manuals. Additionally, there is ongoing research to establish optimal dosage and treatment protocols for different cancer types and stages, which may influence future regulatory guidelines.
Electromagnetic field exposure limits are another crucial aspect of PEMF safety regulations. The International Commission on Non-Ionizing Radiation Protection (ICNIRP) provides guidelines for limiting exposure to electromagnetic fields, which many countries adopt as the basis for their national standards. PEMF device manufacturers must ensure their products comply with these exposure limits to obtain regulatory approval.
As the field of PEMF therapy in oncology advances, regulatory bodies are adapting their approaches to keep pace with technological innovations. This includes developing new testing methodologies and safety standards specific to PEMF devices used in cancer care. Regulatory agencies are also encouraging post-market surveillance and real-world evidence collection to monitor long-term safety and effectiveness.
Collaboration between regulatory bodies, researchers, and industry stakeholders is essential for developing appropriate safety guidelines and regulations. International harmonization efforts, such as the Medical Device Single Audit Program (MDSAP), aim to streamline regulatory processes across multiple jurisdictions, facilitating global access to innovative PEMF therapies while maintaining high safety standards.
In the United States, the Food and Drug Administration (FDA) has classified PEMF devices into different categories based on their intended use and potential risks. For oncological supportive care, PEMF devices are typically classified as Class II medical devices, requiring premarket notification (510(k)) clearance. This process involves demonstrating substantial equivalence to a legally marketed predicate device, ensuring that new PEMF devices meet established safety and effectiveness standards.
The European Union has implemented the Medical Device Regulation (MDR), which came into full effect in May 2021. Under this framework, PEMF devices for oncological supportive care are subject to rigorous conformity assessment procedures. Manufacturers must demonstrate compliance with essential safety and performance requirements, conduct clinical evaluations, and implement a comprehensive quality management system.
Safety considerations for PEMF therapy in oncological care include potential interactions with other medical devices, such as pacemakers or implanted defibrillators. Regulatory bodies require manufacturers to provide clear contraindications and warnings in device labeling and user manuals. Additionally, there is ongoing research to establish optimal dosage and treatment protocols for different cancer types and stages, which may influence future regulatory guidelines.
Electromagnetic field exposure limits are another crucial aspect of PEMF safety regulations. The International Commission on Non-Ionizing Radiation Protection (ICNIRP) provides guidelines for limiting exposure to electromagnetic fields, which many countries adopt as the basis for their national standards. PEMF device manufacturers must ensure their products comply with these exposure limits to obtain regulatory approval.
As the field of PEMF therapy in oncology advances, regulatory bodies are adapting their approaches to keep pace with technological innovations. This includes developing new testing methodologies and safety standards specific to PEMF devices used in cancer care. Regulatory agencies are also encouraging post-market surveillance and real-world evidence collection to monitor long-term safety and effectiveness.
Collaboration between regulatory bodies, researchers, and industry stakeholders is essential for developing appropriate safety guidelines and regulations. International harmonization efforts, such as the Medical Device Single Audit Program (MDSAP), aim to streamline regulatory processes across multiple jurisdictions, facilitating global access to innovative PEMF therapies while maintaining high safety standards.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!