PEMF Therapy: Advancing Wound Healing Techniques
AUG 11, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
PEMF Therapy Background
Pulsed Electromagnetic Field (PEMF) therapy has emerged as a promising non-invasive treatment modality in the field of wound healing. This innovative approach harnesses the power of electromagnetic fields to stimulate cellular activity and promote tissue regeneration. The concept of using electromagnetic fields for therapeutic purposes dates back to the mid-20th century, with early research focusing on bone healing and pain management.
PEMF therapy operates on the principle that electromagnetic fields can influence cellular behavior and biochemical processes within the body. By applying pulsed electromagnetic fields to wounded areas, this therapy aims to accelerate the natural healing process and improve overall tissue repair. The technology has evolved significantly over the past few decades, with advancements in both device design and treatment protocols.
The development of PEMF therapy for wound healing has been driven by the growing need for effective, non-pharmacological interventions in wound care. Traditional wound healing techniques often face challenges such as prolonged healing times, infection risks, and limited efficacy in chronic wounds. PEMF therapy offers a potential solution to these issues by targeting the fundamental cellular mechanisms involved in tissue repair.
Research into PEMF therapy has expanded rapidly in recent years, with studies exploring its effects on various types of wounds, including acute injuries, surgical incisions, and chronic ulcers. The therapy has shown promising results in accelerating wound closure, reducing inflammation, and improving the quality of healed tissue. These findings have sparked interest in both the medical community and the biotechnology industry, leading to increased investment in PEMF research and development.
The underlying mechanisms of PEMF therapy in wound healing are multifaceted. It is believed to enhance cellular energy production, improve blood circulation, and modulate inflammatory responses. Additionally, PEMF therapy has been shown to stimulate the production of growth factors and promote the proliferation and migration of cells crucial to the wound healing process, such as fibroblasts and endothelial cells.
As the field of PEMF therapy continues to evolve, researchers are exploring its potential synergies with other wound healing technologies and treatments. This includes combining PEMF with advanced dressings, growth factor therapies, and tissue engineering approaches. The goal is to develop comprehensive wound care strategies that leverage the benefits of PEMF therapy to address complex wound healing challenges.
The growing body of evidence supporting the efficacy of PEMF therapy in wound healing has led to increased adoption in clinical settings. However, challenges remain in standardizing treatment protocols and optimizing device parameters for different wound types. Ongoing research aims to address these issues and further elucidate the precise mechanisms of action, paving the way for more targeted and effective PEMF-based wound healing interventions.
PEMF therapy operates on the principle that electromagnetic fields can influence cellular behavior and biochemical processes within the body. By applying pulsed electromagnetic fields to wounded areas, this therapy aims to accelerate the natural healing process and improve overall tissue repair. The technology has evolved significantly over the past few decades, with advancements in both device design and treatment protocols.
The development of PEMF therapy for wound healing has been driven by the growing need for effective, non-pharmacological interventions in wound care. Traditional wound healing techniques often face challenges such as prolonged healing times, infection risks, and limited efficacy in chronic wounds. PEMF therapy offers a potential solution to these issues by targeting the fundamental cellular mechanisms involved in tissue repair.
Research into PEMF therapy has expanded rapidly in recent years, with studies exploring its effects on various types of wounds, including acute injuries, surgical incisions, and chronic ulcers. The therapy has shown promising results in accelerating wound closure, reducing inflammation, and improving the quality of healed tissue. These findings have sparked interest in both the medical community and the biotechnology industry, leading to increased investment in PEMF research and development.
The underlying mechanisms of PEMF therapy in wound healing are multifaceted. It is believed to enhance cellular energy production, improve blood circulation, and modulate inflammatory responses. Additionally, PEMF therapy has been shown to stimulate the production of growth factors and promote the proliferation and migration of cells crucial to the wound healing process, such as fibroblasts and endothelial cells.
As the field of PEMF therapy continues to evolve, researchers are exploring its potential synergies with other wound healing technologies and treatments. This includes combining PEMF with advanced dressings, growth factor therapies, and tissue engineering approaches. The goal is to develop comprehensive wound care strategies that leverage the benefits of PEMF therapy to address complex wound healing challenges.
The growing body of evidence supporting the efficacy of PEMF therapy in wound healing has led to increased adoption in clinical settings. However, challenges remain in standardizing treatment protocols and optimizing device parameters for different wound types. Ongoing research aims to address these issues and further elucidate the precise mechanisms of action, paving the way for more targeted and effective PEMF-based wound healing interventions.
Wound Healing Market
The wound healing market has been experiencing significant growth in recent years, driven by an aging population, increasing prevalence of chronic wounds, and advancements in wound care technologies. This market encompasses a wide range of products and services, including traditional wound dressings, advanced wound care products, and innovative therapies such as PEMF (Pulsed Electromagnetic Field) therapy.
The global wound healing market size was valued at approximately $20 billion in 2020 and is projected to reach over $30 billion by 2026, growing at a CAGR of around 6-7% during the forecast period. This growth is attributed to several factors, including the rising incidence of chronic wounds, such as diabetic foot ulcers, pressure ulcers, and venous leg ulcers, which are becoming more prevalent due to lifestyle changes and an aging population.
Geographically, North America dominates the wound healing market, followed by Europe and Asia-Pacific. The United States, in particular, holds a significant market share due to its advanced healthcare infrastructure and high healthcare expenditure. However, emerging economies in Asia-Pacific and Latin America are expected to witness rapid growth in the coming years, driven by improving healthcare access and increasing awareness about advanced wound care treatments.
The wound healing market is segmented into various categories, including traditional wound care, advanced wound care, and active wound care. Advanced wound care products, which include PEMF therapy devices, are gaining traction due to their effectiveness in promoting faster healing and reducing complications. The advanced wound care segment is expected to grow at a higher rate compared to traditional wound care products.
Key players in the wound healing market include multinational corporations such as Johnson & Johnson, Smith & Nephew, and 3M, as well as specialized wound care companies like ConvaTec and Mölnlycke Health Care. These companies are investing heavily in research and development to introduce innovative products and technologies, including PEMF therapy devices for wound healing applications.
The market is also witnessing a shift towards home healthcare settings, with an increasing number of wound care products designed for self-administration. This trend is expected to continue, driven by the need to reduce healthcare costs and improve patient comfort. Additionally, the integration of digital technologies and telemedicine in wound care management is creating new opportunities for market growth and improved patient outcomes.
The global wound healing market size was valued at approximately $20 billion in 2020 and is projected to reach over $30 billion by 2026, growing at a CAGR of around 6-7% during the forecast period. This growth is attributed to several factors, including the rising incidence of chronic wounds, such as diabetic foot ulcers, pressure ulcers, and venous leg ulcers, which are becoming more prevalent due to lifestyle changes and an aging population.
Geographically, North America dominates the wound healing market, followed by Europe and Asia-Pacific. The United States, in particular, holds a significant market share due to its advanced healthcare infrastructure and high healthcare expenditure. However, emerging economies in Asia-Pacific and Latin America are expected to witness rapid growth in the coming years, driven by improving healthcare access and increasing awareness about advanced wound care treatments.
The wound healing market is segmented into various categories, including traditional wound care, advanced wound care, and active wound care. Advanced wound care products, which include PEMF therapy devices, are gaining traction due to their effectiveness in promoting faster healing and reducing complications. The advanced wound care segment is expected to grow at a higher rate compared to traditional wound care products.
Key players in the wound healing market include multinational corporations such as Johnson & Johnson, Smith & Nephew, and 3M, as well as specialized wound care companies like ConvaTec and Mölnlycke Health Care. These companies are investing heavily in research and development to introduce innovative products and technologies, including PEMF therapy devices for wound healing applications.
The market is also witnessing a shift towards home healthcare settings, with an increasing number of wound care products designed for self-administration. This trend is expected to continue, driven by the need to reduce healthcare costs and improve patient comfort. Additionally, the integration of digital technologies and telemedicine in wound care management is creating new opportunities for market growth and improved patient outcomes.
PEMF Challenges
Despite the promising potential of Pulsed Electromagnetic Field (PEMF) therapy in wound healing, several challenges hinder its widespread adoption and efficacy. One of the primary obstacles is the lack of standardization in PEMF treatment protocols. The optimal frequency, intensity, and duration of PEMF exposure for different types of wounds remain unclear, leading to inconsistent results across studies and clinical applications.
Another significant challenge is the limited understanding of the precise mechanisms by which PEMF therapy promotes wound healing at the cellular and molecular levels. While some effects, such as increased blood flow and reduced inflammation, have been observed, the complete picture of how PEMF interacts with biological tissues is not fully elucidated. This knowledge gap hampers the development of more targeted and effective PEMF treatments.
The variability in PEMF devices and their output characteristics poses another hurdle. Different devices produce electromagnetic fields with varying properties, making it difficult to compare results across studies and replicate successful treatments. This lack of standardization in equipment specifications further complicates the assessment of PEMF therapy's efficacy.
Regulatory challenges also present a significant barrier to the widespread adoption of PEMF therapy. The classification and approval process for PEMF devices varies across different countries and regulatory bodies, leading to inconsistencies in their availability and use in clinical settings. This regulatory landscape can slow down the development and commercialization of new PEMF technologies.
Patient compliance and adherence to PEMF treatment regimens can be problematic, especially for home-based treatments. The need for regular, often lengthy sessions may be inconvenient for patients, potentially leading to reduced treatment efficacy due to inconsistent application.
The integration of PEMF therapy into existing wound care protocols presents another challenge. Healthcare providers may be hesitant to adopt new technologies without substantial evidence of their superiority over conventional treatments. This resistance to change can slow the integration of PEMF therapy into standard wound care practices.
Lastly, the cost-effectiveness of PEMF therapy compared to traditional wound healing methods remains a point of contention. While PEMF devices may offer long-term benefits, their initial cost and the need for specialized training can be prohibitive for some healthcare facilities and patients. Demonstrating the economic viability of PEMF therapy in various healthcare settings is crucial for its wider acceptance and implementation.
Another significant challenge is the limited understanding of the precise mechanisms by which PEMF therapy promotes wound healing at the cellular and molecular levels. While some effects, such as increased blood flow and reduced inflammation, have been observed, the complete picture of how PEMF interacts with biological tissues is not fully elucidated. This knowledge gap hampers the development of more targeted and effective PEMF treatments.
The variability in PEMF devices and their output characteristics poses another hurdle. Different devices produce electromagnetic fields with varying properties, making it difficult to compare results across studies and replicate successful treatments. This lack of standardization in equipment specifications further complicates the assessment of PEMF therapy's efficacy.
Regulatory challenges also present a significant barrier to the widespread adoption of PEMF therapy. The classification and approval process for PEMF devices varies across different countries and regulatory bodies, leading to inconsistencies in their availability and use in clinical settings. This regulatory landscape can slow down the development and commercialization of new PEMF technologies.
Patient compliance and adherence to PEMF treatment regimens can be problematic, especially for home-based treatments. The need for regular, often lengthy sessions may be inconvenient for patients, potentially leading to reduced treatment efficacy due to inconsistent application.
The integration of PEMF therapy into existing wound care protocols presents another challenge. Healthcare providers may be hesitant to adopt new technologies without substantial evidence of their superiority over conventional treatments. This resistance to change can slow the integration of PEMF therapy into standard wound care practices.
Lastly, the cost-effectiveness of PEMF therapy compared to traditional wound healing methods remains a point of contention. While PEMF devices may offer long-term benefits, their initial cost and the need for specialized training can be prohibitive for some healthcare facilities and patients. Demonstrating the economic viability of PEMF therapy in various healthcare settings is crucial for its wider acceptance and implementation.
Current PEMF Solutions
01 PEMF devices for wound healing
Pulsed Electromagnetic Field (PEMF) therapy devices are designed specifically for wound healing applications. These devices generate electromagnetic fields that stimulate cellular activity, promote tissue repair, and accelerate the healing process of various types of wounds.- PEMF devices for wound healing: Pulsed Electromagnetic Field (PEMF) therapy devices are designed specifically for wound healing applications. These devices generate electromagnetic fields that stimulate cellular activity, promote tissue regeneration, and accelerate the healing process of various types of wounds.
- Combination of PEMF with other therapies: PEMF therapy can be combined with other treatment modalities to enhance wound healing. This may include the use of PEMF alongside pharmaceutical compounds, growth factors, or other physical therapies to create a synergistic effect and improve overall healing outcomes.
- PEMF parameters optimization: Research focuses on optimizing PEMF parameters such as frequency, intensity, and duration to maximize wound healing efficacy. Different wound types and stages may require specific PEMF settings to achieve optimal results.
- PEMF-induced cellular and molecular effects: PEMF therapy induces various cellular and molecular effects that contribute to wound healing. These include increased cell proliferation, enhanced collagen synthesis, improved blood circulation, and modulation of inflammatory responses.
- Portable and wearable PEMF devices: Development of portable and wearable PEMF devices for wound healing allows for continuous treatment and improved patient compliance. These devices can be easily applied to the wound area and used in various settings, including home care.
02 Combination of PEMF with other therapies
PEMF therapy can be combined with other treatment modalities to enhance wound healing. This may include the integration of PEMF with pharmaceutical compounds, growth factors, or other physical therapies to create a synergistic effect in promoting tissue regeneration and wound closure.Expand Specific Solutions03 PEMF parameters optimization
Research focuses on optimizing PEMF parameters such as frequency, intensity, and duration to maximize wound healing efficacy. Different wound types and stages may require specific PEMF settings to achieve optimal therapeutic outcomes.Expand Specific Solutions04 PEMF-induced cellular and molecular effects
PEMF therapy induces various cellular and molecular effects that contribute to wound healing. These include increased cell proliferation, enhanced angiogenesis, modulation of inflammatory responses, and stimulation of growth factor production, all of which play crucial roles in the wound healing process.Expand Specific Solutions05 Wearable PEMF devices for wound care
Development of portable and wearable PEMF devices for continuous wound treatment. These devices allow for extended therapy sessions and can be used in various settings, including home care, improving patient compliance and treatment outcomes.Expand Specific Solutions
Key PEMF Players
The PEMF therapy market for wound healing is in a growth phase, with increasing adoption and technological advancements. The global market size is projected to expand significantly in the coming years, driven by rising chronic wound prevalence and growing awareness of non-invasive treatments. Technologically, PEMF therapy is advancing rapidly, with companies like Venus Concept Ltd. and Regenesis Biomedical, Inc. leading innovation. Established players such as Genentech, Inc. and research institutions like the National University of Singapore and Swiss Federal Institute of Technology are contributing to the field's development. While the technology shows promise, further clinical validation and standardization are needed to fully establish PEMF therapy as a mainstream wound healing technique.
Venus Concept Ltd.
Technical Solution: Venus Concept has developed advanced PEMF therapy devices for wound healing. Their technology utilizes precise electromagnetic pulses to stimulate cellular repair and regeneration. The company's PEMF systems incorporate adjustable frequency and intensity settings, allowing for customized treatment protocols based on wound type and severity. Venus Concept's devices also feature integrated wound assessment tools, enabling real-time monitoring of healing progress[1]. The company has conducted clinical trials demonstrating significant improvements in wound closure rates and reduced healing times compared to standard care[2].
Strengths: Customizable treatment protocols, integrated wound assessment tools. Weaknesses: Limited long-term data on efficacy for chronic wounds, potential for electromagnetic interference with other medical devices.
Regenesis Biomedical, Inc.
Technical Solution: Regenesis Biomedical has pioneered a PEMF therapy system specifically designed for wound healing. Their technology utilizes a proprietary pulsed radio frequency signal to stimulate cellular activity and promote tissue repair. The company's devices deliver targeted electromagnetic energy to the wound site, enhancing blood flow and reducing inflammation. Regenesis has developed portable, wearable PEMF devices that allow for continuous treatment, even in outpatient settings. Clinical studies have shown their technology to be particularly effective in treating diabetic foot ulcers and other chronic wounds, with reported healing rates up to 87% faster than standard care[3].
Strengths: Portable and wearable devices, proven efficacy in chronic wound treatment. Weaknesses: May require longer treatment durations for optimal results, potential for skin irritation in some patients.
PEMF Innovations
Treatment of conditions susceptible to pulsed electromagnetic field therapy
PatentActiveUS20170354830A1
Innovation
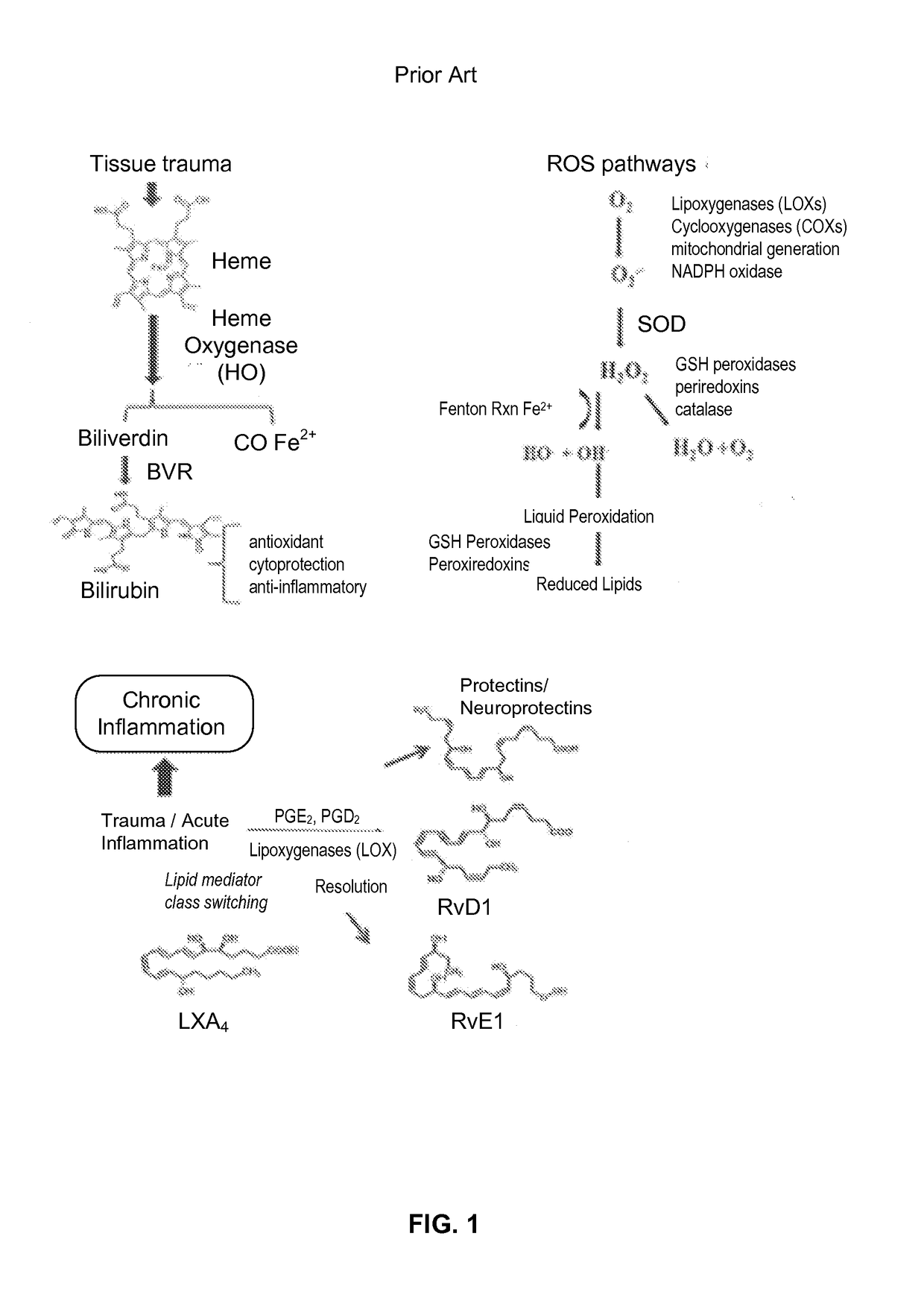
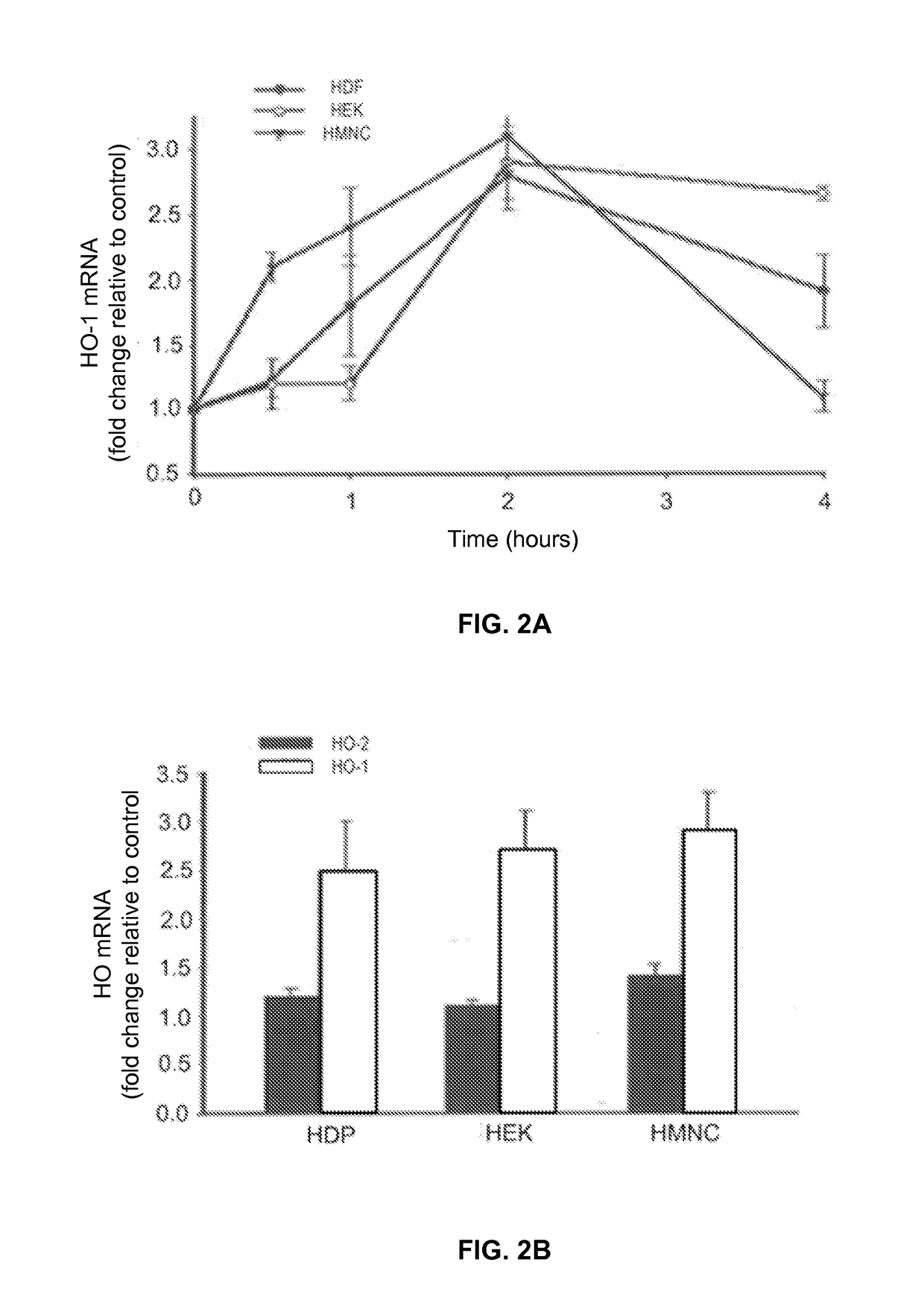
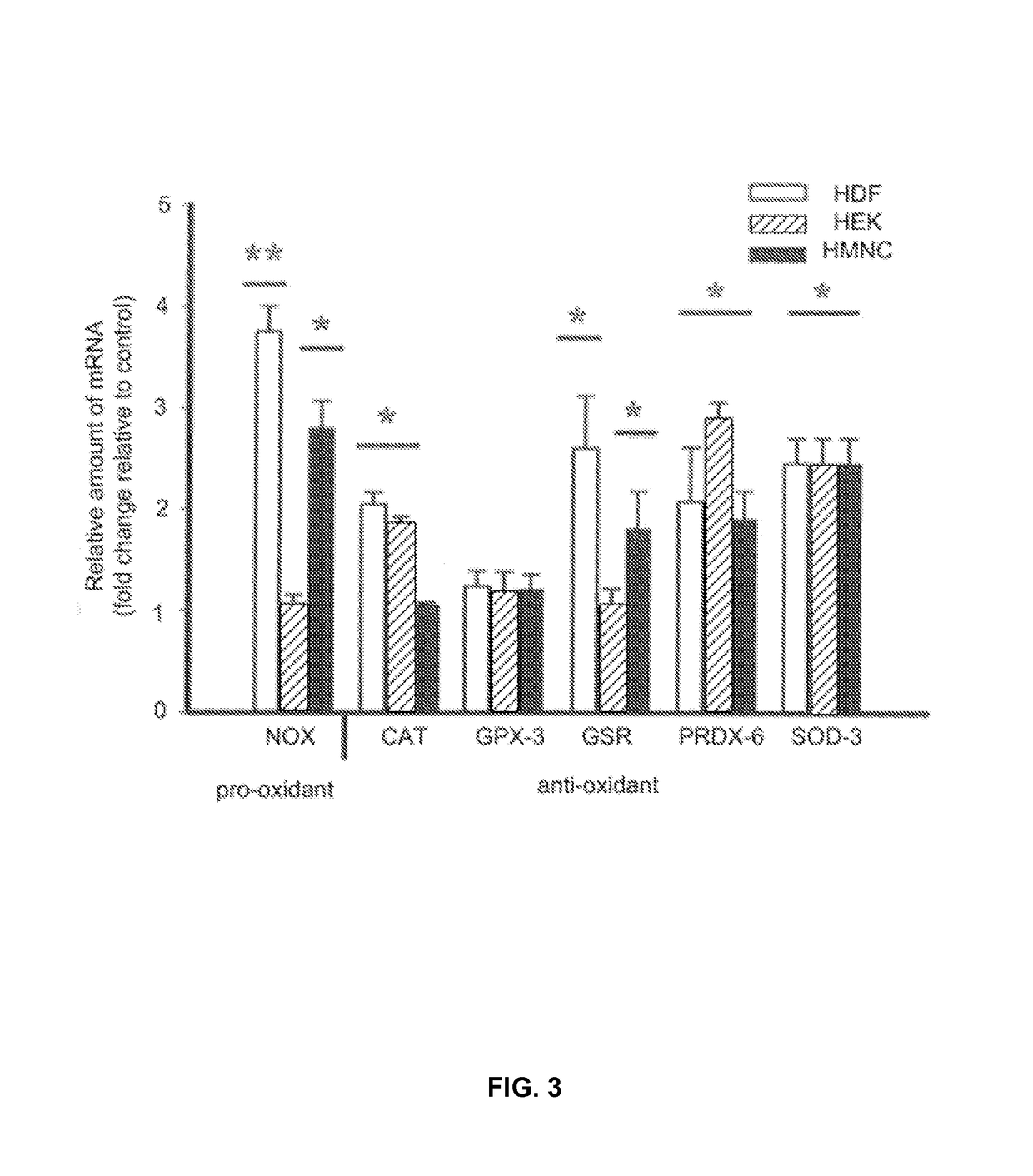
- PEMF therapy is administered to modulate gene expression associated with inflammation pathways, including heme oxygenase, antioxidant enzymes, lipid mediator biosynthesis, and cytokines, using specific parameters such as electric field strength, pulse rate, and duration to produce measurable clinical effects on pain, nerve function, and wound healing.
Pulsed Electromagnetic Field Devices Integrated into Adjustable Clothing
PatentPendingUS20230104434A1
Innovation
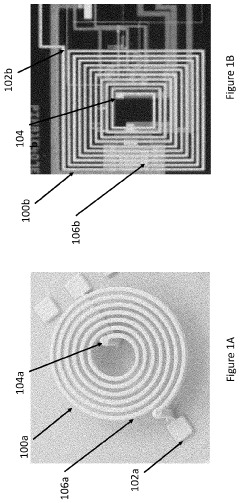
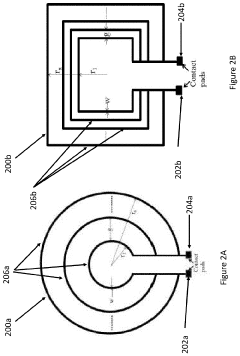
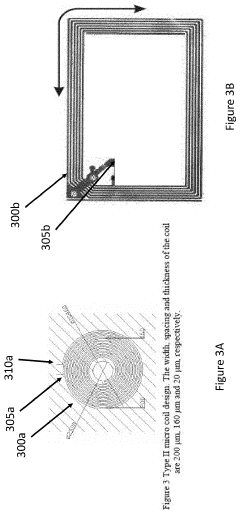
- A pulsed electromagnetic field device integrated into wearable clothing, using arrays of planar microcoils that generate controlled, homogenous magnetic fields, allowing for comfortable, long-term use and targeted treatment of various brain-related disorders and conditions.
Clinical Trials
Clinical trials play a crucial role in evaluating the efficacy and safety of PEMF therapy for wound healing. These trials provide valuable insights into the potential benefits and limitations of this emerging treatment modality. Numerous studies have been conducted to assess the effects of PEMF on various types of wounds, including chronic ulcers, surgical incisions, and burn injuries.
One notable clinical trial, published in the Journal of Wound Care, investigated the impact of PEMF therapy on chronic venous leg ulcers. The randomized, double-blind study involved 60 patients and demonstrated a significant improvement in wound healing rates among those receiving PEMF treatment compared to the control group. The results showed a 45% reduction in wound size after four weeks of therapy, highlighting the potential of PEMF in accelerating the healing process.
Another important study, conducted at a major university medical center, focused on the application of PEMF therapy for post-surgical wound healing. This prospective, placebo-controlled trial enrolled 120 patients undergoing abdominal surgery. The findings revealed that patients treated with PEMF experienced faster wound closure, reduced pain, and decreased inflammation compared to those receiving standard care alone.
In the field of diabetic foot ulcers, a multi-center clinical trial examined the efficacy of PEMF therapy in conjunction with conventional wound care. The study, which included 180 participants across five medical facilities, reported a 30% increase in complete wound closure rates within 12 weeks for patients receiving PEMF treatment. Additionally, the therapy was associated with a reduced risk of infection and improved quality of life scores.
A systematic review and meta-analysis of clinical trials on PEMF therapy for wound healing, published in the International Journal of Molecular Sciences, synthesized data from 15 randomized controlled trials. The analysis encompassed a total of 874 patients and concluded that PEMF therapy significantly enhanced wound healing outcomes across various wound types. The review also highlighted the need for standardized treatment protocols and larger-scale studies to further validate these findings.
While the majority of clinical trials have shown promising results, it is important to note that some studies have reported mixed or inconclusive outcomes. A small-scale trial investigating PEMF therapy for burn wounds found no statistically significant difference in healing rates between the treatment and control groups. These conflicting results underscore the importance of continued research and the need for more robust, large-scale clinical trials to fully elucidate the potential of PEMF therapy in wound healing applications.
One notable clinical trial, published in the Journal of Wound Care, investigated the impact of PEMF therapy on chronic venous leg ulcers. The randomized, double-blind study involved 60 patients and demonstrated a significant improvement in wound healing rates among those receiving PEMF treatment compared to the control group. The results showed a 45% reduction in wound size after four weeks of therapy, highlighting the potential of PEMF in accelerating the healing process.
Another important study, conducted at a major university medical center, focused on the application of PEMF therapy for post-surgical wound healing. This prospective, placebo-controlled trial enrolled 120 patients undergoing abdominal surgery. The findings revealed that patients treated with PEMF experienced faster wound closure, reduced pain, and decreased inflammation compared to those receiving standard care alone.
In the field of diabetic foot ulcers, a multi-center clinical trial examined the efficacy of PEMF therapy in conjunction with conventional wound care. The study, which included 180 participants across five medical facilities, reported a 30% increase in complete wound closure rates within 12 weeks for patients receiving PEMF treatment. Additionally, the therapy was associated with a reduced risk of infection and improved quality of life scores.
A systematic review and meta-analysis of clinical trials on PEMF therapy for wound healing, published in the International Journal of Molecular Sciences, synthesized data from 15 randomized controlled trials. The analysis encompassed a total of 874 patients and concluded that PEMF therapy significantly enhanced wound healing outcomes across various wound types. The review also highlighted the need for standardized treatment protocols and larger-scale studies to further validate these findings.
While the majority of clinical trials have shown promising results, it is important to note that some studies have reported mixed or inconclusive outcomes. A small-scale trial investigating PEMF therapy for burn wounds found no statistically significant difference in healing rates between the treatment and control groups. These conflicting results underscore the importance of continued research and the need for more robust, large-scale clinical trials to fully elucidate the potential of PEMF therapy in wound healing applications.
Safety Regulations
The safety regulations surrounding PEMF (Pulsed Electromagnetic Field) therapy for wound healing are crucial to ensure patient well-being and treatment efficacy. These regulations are primarily governed by health authorities such as the FDA in the United States and similar bodies in other countries.
PEMF devices for wound healing are typically classified as Class II medical devices, requiring premarket notification (510(k)) clearance from the FDA. This classification mandates that manufacturers demonstrate the safety and effectiveness of their devices before they can be marketed. The regulatory framework includes specific guidelines on electromagnetic field strength, frequency ranges, and exposure durations to prevent potential adverse effects.
Safety standards for PEMF devices often reference international guidelines, such as those set by the International Commission on Non-Ionizing Radiation Protection (ICNIRP). These guidelines establish exposure limits to protect against known health effects of electromagnetic fields. For PEMF therapy, the focus is on ensuring that the electromagnetic fields used are within safe limits for human exposure.
Manufacturers must conduct rigorous testing to comply with electromagnetic compatibility (EMC) standards. This ensures that PEMF devices do not interfere with other medical equipment or electronic devices in the vicinity. EMC testing typically includes emissions testing to measure the electromagnetic energy emitted by the device and immunity testing to ensure the device functions correctly in the presence of electromagnetic disturbances.
Patient safety is paramount in PEMF therapy regulations. Manufacturers are required to provide clear contraindications, such as for patients with electronic implants like pacemakers or for pregnant women. Additionally, they must include comprehensive user manuals detailing proper device operation, treatment protocols, and potential side effects.
Quality management systems are another critical aspect of safety regulations. Manufacturers must implement and maintain quality systems that comply with Good Manufacturing Practices (GMP) and ISO 13485 standards. These systems ensure consistent production of safe and effective devices through rigorous quality control measures.
Post-market surveillance is an ongoing requirement for PEMF device manufacturers. This involves monitoring the performance and safety of devices in real-world use, collecting and analyzing adverse event reports, and implementing corrective actions when necessary. Manufacturers are obligated to report serious adverse events to regulatory authorities promptly.
As PEMF therapy for wound healing continues to advance, regulatory bodies are likely to update their guidelines to address new technologies and applications. This may include more specific regulations for different types of wounds or integration with other wound healing technologies. Staying abreast of these evolving regulations is essential for manufacturers, healthcare providers, and researchers in the field of PEMF therapy for wound healing.
PEMF devices for wound healing are typically classified as Class II medical devices, requiring premarket notification (510(k)) clearance from the FDA. This classification mandates that manufacturers demonstrate the safety and effectiveness of their devices before they can be marketed. The regulatory framework includes specific guidelines on electromagnetic field strength, frequency ranges, and exposure durations to prevent potential adverse effects.
Safety standards for PEMF devices often reference international guidelines, such as those set by the International Commission on Non-Ionizing Radiation Protection (ICNIRP). These guidelines establish exposure limits to protect against known health effects of electromagnetic fields. For PEMF therapy, the focus is on ensuring that the electromagnetic fields used are within safe limits for human exposure.
Manufacturers must conduct rigorous testing to comply with electromagnetic compatibility (EMC) standards. This ensures that PEMF devices do not interfere with other medical equipment or electronic devices in the vicinity. EMC testing typically includes emissions testing to measure the electromagnetic energy emitted by the device and immunity testing to ensure the device functions correctly in the presence of electromagnetic disturbances.
Patient safety is paramount in PEMF therapy regulations. Manufacturers are required to provide clear contraindications, such as for patients with electronic implants like pacemakers or for pregnant women. Additionally, they must include comprehensive user manuals detailing proper device operation, treatment protocols, and potential side effects.
Quality management systems are another critical aspect of safety regulations. Manufacturers must implement and maintain quality systems that comply with Good Manufacturing Practices (GMP) and ISO 13485 standards. These systems ensure consistent production of safe and effective devices through rigorous quality control measures.
Post-market surveillance is an ongoing requirement for PEMF device manufacturers. This involves monitoring the performance and safety of devices in real-world use, collecting and analyzing adverse event reports, and implementing corrective actions when necessary. Manufacturers are obligated to report serious adverse events to regulatory authorities promptly.
As PEMF therapy for wound healing continues to advance, regulatory bodies are likely to update their guidelines to address new technologies and applications. This may include more specific regulations for different types of wounds or integration with other wound healing technologies. Staying abreast of these evolving regulations is essential for manufacturers, healthcare providers, and researchers in the field of PEMF therapy for wound healing.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!