Analysis of Photocatalytic Disinfection's Role in Reducing Hospital Acquired Infections
OCT 21, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Photocatalytic Disinfection Background and Objectives
Photocatalytic disinfection technology has evolved significantly since its initial discovery in the 1970s when researchers observed the antimicrobial properties of titanium dioxide (TiO₂) under ultraviolet light. This phenomenon, based on the generation of reactive oxygen species (ROS) through semiconductor photocatalysis, has gradually developed from laboratory curiosity to practical application over the past five decades.
The evolution of this technology has been marked by several key milestones, including the development of visible light-responsive photocatalysts in the early 2000s, which expanded potential applications beyond UV-dependent systems. Recent advancements have focused on enhancing catalytic efficiency, reducing activation energy requirements, and developing novel composite materials with superior antimicrobial properties.
In healthcare settings, hospital-acquired infections (HAIs) represent a significant global challenge, affecting approximately 7% of patients in developed countries and over 10% in developing regions. These infections result in prolonged hospital stays, increased healthcare costs estimated at $28-45 billion annually in the US alone, and contribute to approximately 90,000 deaths per year in the United States.
Traditional disinfection methods in healthcare facilities rely heavily on chemical disinfectants and manual cleaning protocols, which present several limitations including human error, chemical resistance development, and potential toxicity concerns. The COVID-19 pandemic has further highlighted the urgent need for more effective, continuous, and passive disinfection technologies in healthcare environments.
Photocatalytic disinfection offers a promising alternative approach through its ability to provide continuous surface decontamination without manual intervention, broad-spectrum antimicrobial activity against bacteria, viruses, and fungi, and minimal development of microbial resistance due to its non-specific oxidative damage mechanism.
The primary objective of this technical research is to comprehensively evaluate the potential of photocatalytic disinfection technologies in reducing hospital-acquired infections. Specifically, we aim to assess the efficacy of various photocatalytic materials and systems against common nosocomial pathogens, analyze implementation challenges in healthcare settings, and identify optimal integration strategies for existing hospital infrastructure.
Additionally, this research seeks to quantify the potential impact of widespread photocatalytic disinfection implementation on HAI rates, patient outcomes, and healthcare economics. By establishing clear performance metrics and implementation guidelines, we intend to provide healthcare facilities with actionable insights for adopting this technology as part of comprehensive infection control strategies.
The evolution of this technology has been marked by several key milestones, including the development of visible light-responsive photocatalysts in the early 2000s, which expanded potential applications beyond UV-dependent systems. Recent advancements have focused on enhancing catalytic efficiency, reducing activation energy requirements, and developing novel composite materials with superior antimicrobial properties.
In healthcare settings, hospital-acquired infections (HAIs) represent a significant global challenge, affecting approximately 7% of patients in developed countries and over 10% in developing regions. These infections result in prolonged hospital stays, increased healthcare costs estimated at $28-45 billion annually in the US alone, and contribute to approximately 90,000 deaths per year in the United States.
Traditional disinfection methods in healthcare facilities rely heavily on chemical disinfectants and manual cleaning protocols, which present several limitations including human error, chemical resistance development, and potential toxicity concerns. The COVID-19 pandemic has further highlighted the urgent need for more effective, continuous, and passive disinfection technologies in healthcare environments.
Photocatalytic disinfection offers a promising alternative approach through its ability to provide continuous surface decontamination without manual intervention, broad-spectrum antimicrobial activity against bacteria, viruses, and fungi, and minimal development of microbial resistance due to its non-specific oxidative damage mechanism.
The primary objective of this technical research is to comprehensively evaluate the potential of photocatalytic disinfection technologies in reducing hospital-acquired infections. Specifically, we aim to assess the efficacy of various photocatalytic materials and systems against common nosocomial pathogens, analyze implementation challenges in healthcare settings, and identify optimal integration strategies for existing hospital infrastructure.
Additionally, this research seeks to quantify the potential impact of widespread photocatalytic disinfection implementation on HAI rates, patient outcomes, and healthcare economics. By establishing clear performance metrics and implementation guidelines, we intend to provide healthcare facilities with actionable insights for adopting this technology as part of comprehensive infection control strategies.
Healthcare Market Demand for HAI Prevention Solutions
The healthcare sector is witnessing a significant surge in demand for effective Hospital Acquired Infection (HAI) prevention solutions, driven by alarming infection rates and their substantial economic impact. HAIs affect approximately 1.7 million patients annually in the United States alone, resulting in nearly 99,000 deaths and adding an estimated $20 billion in healthcare costs. This pressing issue has created a robust market for innovative disinfection technologies, with photocatalytic disinfection emerging as a promising solution.
Market research indicates that the global infection control market is projected to reach $52.7 billion by 2026, growing at a CAGR of 6.5% from 2021. Within this broader market, advanced disinfection technologies are experiencing particularly strong growth, with the hospital disinfection segment expanding at nearly 8% annually. Healthcare facilities are increasingly prioritizing investment in these technologies due to regulatory pressures, reimbursement policies tied to infection rates, and growing patient awareness of HAI risks.
The COVID-19 pandemic has dramatically accelerated this market trend, creating unprecedented demand for continuous disinfection solutions that can operate safely in occupied spaces. Hospital administrators report that patient perception of cleanliness and infection control measures now significantly influences healthcare facility selection, making investment in advanced disinfection technologies both a clinical and business imperative.
Key market drivers include stringent regulatory requirements from bodies like the CDC and Joint Commission, which have established increasingly strict guidelines for infection prevention. Additionally, the financial penalties imposed on healthcare facilities with high HAI rates through programs like Medicare's Hospital-Acquired Condition Reduction Program have created direct economic incentives for adoption of effective prevention technologies.
Market segmentation reveals particularly strong demand in high-risk areas such as operating rooms, intensive care units, and isolation wards, where the consequences of infections are most severe. There is also growing interest from outpatient facilities and ambulatory surgical centers seeking to differentiate themselves through superior infection control practices.
The value proposition of photocatalytic disinfection aligns well with current market needs, offering continuous rather than episodic disinfection, compatibility with occupied spaces, and reduced reliance on manual cleaning processes. Healthcare facilities are increasingly seeking solutions that address multiple pathogens simultaneously while minimizing disruption to clinical workflows and reducing dependence on chemical disinfectants that may contribute to antimicrobial resistance.
Market research indicates that the global infection control market is projected to reach $52.7 billion by 2026, growing at a CAGR of 6.5% from 2021. Within this broader market, advanced disinfection technologies are experiencing particularly strong growth, with the hospital disinfection segment expanding at nearly 8% annually. Healthcare facilities are increasingly prioritizing investment in these technologies due to regulatory pressures, reimbursement policies tied to infection rates, and growing patient awareness of HAI risks.
The COVID-19 pandemic has dramatically accelerated this market trend, creating unprecedented demand for continuous disinfection solutions that can operate safely in occupied spaces. Hospital administrators report that patient perception of cleanliness and infection control measures now significantly influences healthcare facility selection, making investment in advanced disinfection technologies both a clinical and business imperative.
Key market drivers include stringent regulatory requirements from bodies like the CDC and Joint Commission, which have established increasingly strict guidelines for infection prevention. Additionally, the financial penalties imposed on healthcare facilities with high HAI rates through programs like Medicare's Hospital-Acquired Condition Reduction Program have created direct economic incentives for adoption of effective prevention technologies.
Market segmentation reveals particularly strong demand in high-risk areas such as operating rooms, intensive care units, and isolation wards, where the consequences of infections are most severe. There is also growing interest from outpatient facilities and ambulatory surgical centers seeking to differentiate themselves through superior infection control practices.
The value proposition of photocatalytic disinfection aligns well with current market needs, offering continuous rather than episodic disinfection, compatibility with occupied spaces, and reduced reliance on manual cleaning processes. Healthcare facilities are increasingly seeking solutions that address multiple pathogens simultaneously while minimizing disruption to clinical workflows and reducing dependence on chemical disinfectants that may contribute to antimicrobial resistance.
Current Photocatalytic Technology Status and Barriers
Photocatalytic disinfection technology has emerged as a promising approach for reducing hospital-acquired infections (HAIs), with significant advancements in recent years. Currently, titanium dioxide (TiO2) remains the most widely studied and applied photocatalyst due to its chemical stability, non-toxicity, and cost-effectiveness. When activated by UV light, TiO2 generates reactive oxygen species (ROS) that can effectively destroy a broad spectrum of pathogens including bacteria, viruses, and fungi commonly found in healthcare settings.
Despite these advantages, several technological barriers limit widespread implementation. The primary challenge is the UV light dependency of traditional photocatalysts, requiring specific lighting conditions that are not always practical in hospital environments. This limitation has driven research toward visible-light-responsive photocatalysts, including doped TiO2, graphene-based composites, and novel materials like g-C3N4, though these alternatives often demonstrate reduced efficiency compared to UV-activated systems.
Another significant barrier is the durability and longevity of photocatalytic coatings in high-traffic hospital environments. Current formulations show degradation under repeated cleaning protocols and mechanical abrasion, necessitating frequent reapplication. This maintenance requirement increases operational costs and creates implementation challenges for healthcare facilities with continuous occupancy.
The efficacy of photocatalytic disinfection against biofilms presents another technical hurdle. While the technology shows promising results against planktonic microorganisms, hospital pathogens often form biofilms that provide protection against antimicrobial agents. Current photocatalytic systems demonstrate limited penetration into these complex microbial communities, reducing their effectiveness against established infections.
Scalability and integration with existing hospital infrastructure remain problematic. Current application methods, including spray coatings, dip-coating, and physical vapor deposition, each present trade-offs between coverage uniformity, adhesion strength, and implementation cost. Additionally, the potential for nanoparticle leaching raises safety concerns that have not been fully addressed by current technology solutions.
Globally, research efforts are unevenly distributed, with significant advancements emerging from East Asia (particularly Japan and China), Europe, and North America. This geographical concentration has created disparities in technology access and implementation. Regulatory frameworks also vary considerably across regions, with some countries establishing clear guidelines for photocatalytic materials in healthcare settings while others lack specific standards.
The economic viability of photocatalytic disinfection technologies represents a final barrier, as initial implementation costs remain high relative to conventional disinfection methods, despite potential long-term savings through reduced infection rates and associated healthcare costs.
Despite these advantages, several technological barriers limit widespread implementation. The primary challenge is the UV light dependency of traditional photocatalysts, requiring specific lighting conditions that are not always practical in hospital environments. This limitation has driven research toward visible-light-responsive photocatalysts, including doped TiO2, graphene-based composites, and novel materials like g-C3N4, though these alternatives often demonstrate reduced efficiency compared to UV-activated systems.
Another significant barrier is the durability and longevity of photocatalytic coatings in high-traffic hospital environments. Current formulations show degradation under repeated cleaning protocols and mechanical abrasion, necessitating frequent reapplication. This maintenance requirement increases operational costs and creates implementation challenges for healthcare facilities with continuous occupancy.
The efficacy of photocatalytic disinfection against biofilms presents another technical hurdle. While the technology shows promising results against planktonic microorganisms, hospital pathogens often form biofilms that provide protection against antimicrobial agents. Current photocatalytic systems demonstrate limited penetration into these complex microbial communities, reducing their effectiveness against established infections.
Scalability and integration with existing hospital infrastructure remain problematic. Current application methods, including spray coatings, dip-coating, and physical vapor deposition, each present trade-offs between coverage uniformity, adhesion strength, and implementation cost. Additionally, the potential for nanoparticle leaching raises safety concerns that have not been fully addressed by current technology solutions.
Globally, research efforts are unevenly distributed, with significant advancements emerging from East Asia (particularly Japan and China), Europe, and North America. This geographical concentration has created disparities in technology access and implementation. Regulatory frameworks also vary considerably across regions, with some countries establishing clear guidelines for photocatalytic materials in healthcare settings while others lack specific standards.
The economic viability of photocatalytic disinfection technologies represents a final barrier, as initial implementation costs remain high relative to conventional disinfection methods, despite potential long-term savings through reduced infection rates and associated healthcare costs.
Current Photocatalytic Solutions for HAI Prevention
01 TiO2-based photocatalytic materials for hospital disinfection
Titanium dioxide (TiO2) is widely used as a photocatalyst for disinfection in hospital environments. When activated by light, particularly UV radiation, TiO2 generates reactive oxygen species that can effectively kill bacteria, viruses, and other pathogens responsible for hospital-acquired infections. These photocatalytic materials can be incorporated into coatings, films, or standalone devices for continuous disinfection of surfaces and air in healthcare settings.- TiO2-based photocatalytic materials for hospital disinfection: Titanium dioxide (TiO2) is widely used as a photocatalyst for disinfection in hospital environments. When activated by light, TiO2 generates reactive oxygen species that can effectively kill bacteria, viruses, and other pathogens responsible for hospital-acquired infections. These photocatalytic materials can be incorporated into coatings, films, or standalone devices for continuous disinfection of surfaces and air in healthcare settings.
- UV-activated photocatalytic disinfection systems: Ultraviolet light-activated photocatalytic systems provide enhanced disinfection capabilities in hospital environments. These systems combine UV light sources with photocatalytic materials to generate powerful oxidizing agents that destroy pathogens. The technology can be implemented in various forms including air purifiers, surface coatings, and standalone disinfection units, offering continuous protection against hospital-acquired infections even in hard-to-reach areas.
- Visible light-responsive photocatalysts for continuous disinfection: Advanced photocatalysts that can be activated by visible light rather than just UV radiation represent a significant advancement in hospital disinfection technology. These materials can function under normal indoor lighting conditions, providing continuous antimicrobial activity throughout the day. By incorporating metal dopants or creating composite materials, these photocatalysts offer enhanced efficiency in eliminating hospital-acquired infections while being safe for use in occupied spaces.
- Portable photocatalytic disinfection devices for healthcare settings: Portable photocatalytic disinfection devices provide flexible solutions for targeting hospital-acquired infections in various healthcare settings. These devices can be moved between patient rooms, operating theaters, and other critical areas to provide on-demand disinfection. The portable nature allows for strategic deployment in high-risk areas or during outbreak situations, complementing existing infection control protocols with photocatalytic technology that can inactivate a broad spectrum of pathogens.
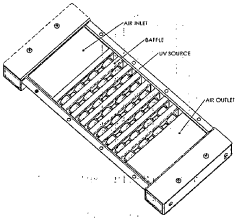
- Integration of photocatalytic technology in hospital ventilation systems: Photocatalytic technology integrated into hospital ventilation and air handling systems provides continuous air disinfection throughout healthcare facilities. These systems incorporate photocatalytic filters or reactor chambers that treat air as it circulates through the building, reducing airborne pathogens responsible for hospital-acquired infections. The integration with existing HVAC infrastructure offers a sustainable approach to infection control without disrupting normal hospital operations or requiring additional staff intervention.
02 UV-activated disinfection systems for healthcare facilities
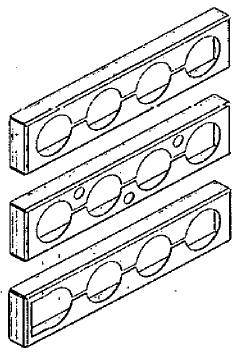
Specialized UV-activated disinfection systems have been developed specifically for healthcare environments. These systems utilize photocatalytic reactions triggered by UV light to eliminate pathogens on surfaces and in the air. The technology can be integrated into existing hospital infrastructure such as ventilation systems, lighting fixtures, or as standalone units. These systems provide continuous disinfection without manual intervention, reducing the risk of hospital-acquired infections in patient rooms, operating theaters, and other critical areas.Expand Specific Solutions03 Novel photocatalyst compositions for enhanced antimicrobial activity
Advanced photocatalyst compositions have been developed to enhance antimicrobial efficacy against hospital-acquired infections. These include doped photocatalysts, composite materials, and novel formulations that improve light absorption range, quantum efficiency, and antimicrobial activity. Some compositions incorporate metals like silver, copper, or zinc to provide synergistic disinfection effects. These enhanced photocatalysts can operate under visible light or low-intensity illumination, making them practical for continuous use in hospital environments.Expand Specific Solutions04 Photocatalytic surface coatings and materials for infection control
Specialized photocatalytic coatings and materials have been developed for application on high-touch surfaces in hospitals to prevent pathogen transmission. These coatings can be applied to walls, floors, door handles, bed rails, and medical equipment. The photocatalytic materials provide continuous disinfection when exposed to light, reducing bioburden and the risk of cross-contamination. Some formulations include self-cleaning properties that decompose organic matter, maintaining antimicrobial efficacy over extended periods without frequent reapplication.Expand Specific Solutions05 Portable and mobile photocatalytic disinfection devices
Portable and mobile photocatalytic disinfection devices have been designed for flexible deployment in healthcare settings. These devices can be moved between patient rooms, operating theaters, and other areas requiring enhanced disinfection. Some designs incorporate air purification capabilities alongside surface disinfection functions. The mobility of these systems allows hospitals to target disinfection efforts where needed most, particularly in areas with high infection risk or during outbreak situations. These devices typically combine photocatalytic materials with appropriate light sources to activate the disinfection process.Expand Specific Solutions
Key Industry Players in Photocatalytic Disinfection
Photocatalytic disinfection technology for reducing hospital-acquired infections is in an emerging growth phase, with the global market expected to reach significant expansion due to increasing healthcare concerns. The technology is advancing from experimental to commercial applications, with varying degrees of maturity across implementations. Key players demonstrate diverse approaches: Signify Holding BV and Current Lighting Solutions focus on integrated lighting systems; UV Partners and Synexis LLC specialize in automated disinfection technologies; while academic institutions like University of Florida and Northwestern University drive fundamental research. Companies such as Ecolab and B Braun Avitum bring healthcare expertise, while technology firms like Nikon and Canon contribute optical engineering capabilities. This competitive landscape reflects a technology transitioning from niche applications toward mainstream healthcare adoption.
Signify Holding BV
Technical Solution: Signify (formerly Philips Lighting) has developed advanced UV-C based photocatalytic disinfection systems specifically designed for healthcare environments. Their technology combines UV-C light with titanium dioxide (TiO2) photocatalysts to create powerful oxidizing agents that destroy pathogens. The system works by activating the photocatalyst with UV-C light, generating reactive oxygen species (ROS) including hydroxyl radicals and hydrogen peroxide that break down bacterial cell walls, viral envelopes, and microbial DNA. Signify's solutions include both fixed installations for continuous environmental disinfection and mobile units for targeted decontamination. Their systems have demonstrated up to 99.9% efficacy against common hospital pathogens including MRSA, C. difficile, and various coronaviruses in controlled studies. The technology is designed to operate safely in occupied spaces through strategic placement and shielding mechanisms.
Strengths: Established global presence with extensive distribution networks; comprehensive R&D capabilities; integration with smart building systems for automated operation. Weaknesses: Higher initial implementation costs compared to conventional disinfection methods; requires professional installation and maintenance; effectiveness can be reduced in areas with poor air circulation.
Synexis LLC
Technical Solution: Synexis has pioneered Dry Hydrogen Peroxide (DHP) technology that utilizes photocatalytic processes to create a continuous flow of hydrogen peroxide molecules from ambient humidity and oxygen. Their proprietary system employs a photocatalyst activated by specific wavelengths of light to generate low concentrations (1-3 parts per billion) of hydrogen peroxide gas that circulates throughout indoor spaces. This approach allows for continuous microbial reduction in occupied areas without disrupting normal hospital operations. Clinical studies in healthcare settings have shown Synexis systems can reduce surface bacterial counts by up to 94% and airborne microorganisms by up to 96%. The technology has been particularly effective against biofilm-forming bacteria that are often resistant to traditional cleaning methods. Synexis systems have been implemented in numerous hospitals across the United States with documented reductions in HAI rates, particularly for surgical site infections and C. difficile cases.
Strengths: Continuous operation providing 24/7 protection; safe for use in occupied spaces; requires minimal maintenance; addresses both airborne and surface contamination simultaneously. Weaknesses: Less effective against certain spore-forming bacteria compared to higher-concentration disinfection methods; optimal performance requires controlled humidity levels; relatively new technology with still-growing clinical evidence base.
Critical Photocatalytic Mechanisms and Materials Analysis
Chemical free disinfection and deodourization equipment
PatentInactiveIN201741009265A
Innovation
- A UV disinfection equipment with Aluminium baffle plates coated with titanium dioxide photocatalyst, designed to enhance photocatalysis by guiding UV light and air flow, ensuring uniform UV dosage and increased surface area for effective microbial inactivation and deodorization, using multiple UV lamps and a chamber made of UV reflective material.
Implementation Challenges in Healthcare Settings
The implementation of photocatalytic disinfection technology in healthcare settings faces several significant challenges that must be addressed for successful adoption. Healthcare facilities operate under strict regulatory frameworks that demand rigorous validation of any new infection control measures. Current photocatalytic systems often lack standardized testing protocols and certification pathways specifically designed for healthcare applications, creating uncertainty for hospital administrators considering implementation.
Physical integration presents another substantial hurdle. Many hospitals, particularly older facilities, have complex architectural layouts and established HVAC systems that were not designed to accommodate photocatalytic technology. Retrofitting these environments requires careful planning to ensure optimal placement of photocatalytic surfaces or devices without disrupting critical healthcare operations or creating maintenance difficulties.
Cost considerations significantly impact adoption decisions. The initial capital expenditure for photocatalytic systems can be substantial, particularly for large-scale implementation across an entire healthcare facility. Hospital financial decision-makers require clear return-on-investment analyses that demonstrate cost savings through reduced infection rates, decreased antibiotic usage, shorter patient stays, and lower staff absenteeism. However, these economic benefits often materialize over extended periods, creating budgetary challenges for institutions operating under tight financial constraints.
Staff acceptance and training requirements represent another implementation barrier. Healthcare workers already manage complex protocols and heavy workloads, making the introduction of new technologies potentially disruptive. Effective implementation requires comprehensive training programs and clear communication about how photocatalytic systems integrate with existing infection control practices. Without proper education, staff may view these systems as unnecessary additions rather than valuable tools for patient safety.
Technical performance limitations also present challenges in the dynamic healthcare environment. Photocatalytic efficiency can be affected by ambient lighting conditions, humidity levels, air flow patterns, and surface contamination. Hospitals must consider how these variables might impact performance across different departments with varying environmental conditions. Additionally, the technology must demonstrate effectiveness against the specific pathogens of greatest concern in healthcare settings, including drug-resistant organisms and emerging infectious agents.
Maintenance requirements pose ongoing operational challenges. Photocatalytic surfaces may require periodic cleaning, reactivation, or replacement to maintain optimal performance. These maintenance protocols must be integrated into existing facility management systems without creating excessive additional workload or disrupting patient care activities.
Physical integration presents another substantial hurdle. Many hospitals, particularly older facilities, have complex architectural layouts and established HVAC systems that were not designed to accommodate photocatalytic technology. Retrofitting these environments requires careful planning to ensure optimal placement of photocatalytic surfaces or devices without disrupting critical healthcare operations or creating maintenance difficulties.
Cost considerations significantly impact adoption decisions. The initial capital expenditure for photocatalytic systems can be substantial, particularly for large-scale implementation across an entire healthcare facility. Hospital financial decision-makers require clear return-on-investment analyses that demonstrate cost savings through reduced infection rates, decreased antibiotic usage, shorter patient stays, and lower staff absenteeism. However, these economic benefits often materialize over extended periods, creating budgetary challenges for institutions operating under tight financial constraints.
Staff acceptance and training requirements represent another implementation barrier. Healthcare workers already manage complex protocols and heavy workloads, making the introduction of new technologies potentially disruptive. Effective implementation requires comprehensive training programs and clear communication about how photocatalytic systems integrate with existing infection control practices. Without proper education, staff may view these systems as unnecessary additions rather than valuable tools for patient safety.
Technical performance limitations also present challenges in the dynamic healthcare environment. Photocatalytic efficiency can be affected by ambient lighting conditions, humidity levels, air flow patterns, and surface contamination. Hospitals must consider how these variables might impact performance across different departments with varying environmental conditions. Additionally, the technology must demonstrate effectiveness against the specific pathogens of greatest concern in healthcare settings, including drug-resistant organisms and emerging infectious agents.
Maintenance requirements pose ongoing operational challenges. Photocatalytic surfaces may require periodic cleaning, reactivation, or replacement to maintain optimal performance. These maintenance protocols must be integrated into existing facility management systems without creating excessive additional workload or disrupting patient care activities.
Regulatory Framework for Hospital Disinfection Technologies
The regulatory landscape governing hospital disinfection technologies is complex and multifaceted, with significant implications for the adoption of photocatalytic disinfection systems. In the United States, the Environmental Protection Agency (EPA) regulates disinfectants under the Federal Insecticide, Fungicide, and Rodenticide Act (FIFRA), requiring manufacturers to demonstrate both efficacy and safety before market approval. For photocatalytic technologies specifically, manufacturers must provide substantial evidence of antimicrobial claims through standardized testing protocols.
The Food and Drug Administration (FDA) maintains oversight of medical devices incorporating disinfection technologies, classifying them based on risk levels. Photocatalytic surfaces and systems may fall under Class II medical devices, requiring premarket notification (510(k)) or potentially more rigorous premarket approval depending on their specific applications and claims.
Internationally, regulatory frameworks vary significantly. The European Union operates under the Biocidal Products Regulation (BPR), which has established specific provisions for surface-active disinfectants. Japan's regulatory system has been particularly progressive regarding photocatalytic technologies, having established JIS standards specifically for photocatalytic materials and their antimicrobial properties.
Healthcare accreditation bodies such as The Joint Commission (TJC) and DNV GL Healthcare have established infection control standards that indirectly impact the adoption of novel disinfection technologies. These standards increasingly emphasize evidence-based approaches to infection prevention, creating pathways for innovative technologies with demonstrated efficacy.
Recent regulatory developments show a trend toward performance-based standards rather than prescriptive requirements, potentially accelerating the adoption of photocatalytic disinfection. The COVID-19 pandemic has prompted regulatory agencies worldwide to implement expedited review processes for disinfection technologies, though these pathways typically maintain rigorous efficacy requirements.
Compliance challenges for photocatalytic disinfection include the lack of standardized testing protocols specifically designed for persistent antimicrobial surfaces, creating uncertainty in the regulatory approval process. Additionally, varying international standards create complexity for global deployment of these technologies, requiring manufacturers to navigate multiple regulatory frameworks simultaneously.
Looking forward, regulatory harmonization efforts through organizations like the International Organization for Standardization (ISO) may streamline approval processes for photocatalytic disinfection technologies. The development of specific standards for continuous disinfection technologies represents a significant opportunity to accelerate market adoption while ensuring appropriate safety and efficacy verification.
The Food and Drug Administration (FDA) maintains oversight of medical devices incorporating disinfection technologies, classifying them based on risk levels. Photocatalytic surfaces and systems may fall under Class II medical devices, requiring premarket notification (510(k)) or potentially more rigorous premarket approval depending on their specific applications and claims.
Internationally, regulatory frameworks vary significantly. The European Union operates under the Biocidal Products Regulation (BPR), which has established specific provisions for surface-active disinfectants. Japan's regulatory system has been particularly progressive regarding photocatalytic technologies, having established JIS standards specifically for photocatalytic materials and their antimicrobial properties.
Healthcare accreditation bodies such as The Joint Commission (TJC) and DNV GL Healthcare have established infection control standards that indirectly impact the adoption of novel disinfection technologies. These standards increasingly emphasize evidence-based approaches to infection prevention, creating pathways for innovative technologies with demonstrated efficacy.
Recent regulatory developments show a trend toward performance-based standards rather than prescriptive requirements, potentially accelerating the adoption of photocatalytic disinfection. The COVID-19 pandemic has prompted regulatory agencies worldwide to implement expedited review processes for disinfection technologies, though these pathways typically maintain rigorous efficacy requirements.
Compliance challenges for photocatalytic disinfection include the lack of standardized testing protocols specifically designed for persistent antimicrobial surfaces, creating uncertainty in the regulatory approval process. Additionally, varying international standards create complexity for global deployment of these technologies, requiring manufacturers to navigate multiple regulatory frameworks simultaneously.
Looking forward, regulatory harmonization efforts through organizations like the International Organization for Standardization (ISO) may streamline approval processes for photocatalytic disinfection technologies. The development of specific standards for continuous disinfection technologies represents a significant opportunity to accelerate market adoption while ensuring appropriate safety and efficacy verification.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!