How Photocatalytic Disinfection Reinforces Hospital Sanitation Protocols
OCT 21, 202510 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Photocatalytic Disinfection Background and Objectives
Photocatalytic disinfection technology has evolved significantly since its initial discovery in the 1970s when researchers first observed the antimicrobial properties of titanium dioxide (TiO2) under ultraviolet light. This phenomenon, based on the generation of reactive oxygen species (ROS) through semiconductor photocatalysis, has gradually transitioned from laboratory curiosity to practical application in various fields, with healthcare environments representing one of the most promising implementation areas.
The evolution of this technology has accelerated in recent decades, driven by increasing concerns about hospital-acquired infections (HAIs) and the emergence of antibiotic-resistant pathogens. Traditional disinfection methods in healthcare settings often face limitations including chemical residues, human error in application, and incomplete coverage of surfaces. Photocatalytic disinfection offers a potential solution by providing continuous antimicrobial activity without additional human intervention after initial application.
Current technological trends in this field include the development of visible light-responsive photocatalysts, nanostructured materials with enhanced surface area, and composite materials that combine multiple functional properties. These innovations aim to overcome the traditional limitations of first-generation photocatalysts, which typically required UV light activation and showed limited efficiency under indoor lighting conditions common in hospital environments.
The primary objective of photocatalytic disinfection in hospital settings is to establish a supplementary layer of continuous disinfection that works alongside conventional cleaning protocols. This approach aims to address the critical gap between scheduled cleaning sessions, during which recontamination frequently occurs. By maintaining antimicrobial activity on high-touch surfaces, photocatalytic technologies could significantly reduce pathogen transmission vectors.
Secondary objectives include reducing reliance on chemical disinfectants, which can contribute to antimicrobial resistance development and pose occupational health risks to healthcare workers through respiratory irritation and dermatological conditions. Additionally, photocatalytic systems aim to provide cost-effective solutions by extending the intervals between intensive manual cleaning, thereby optimizing resource allocation in healthcare facilities.
From a technical perspective, the field is working toward several specific goals: developing photocatalysts with high quantum efficiency under indoor lighting conditions; creating durable coatings that maintain activity for months or years rather than days; ensuring safety for human contact on treated surfaces; and establishing standardized testing protocols to verify efficacy against clinically relevant pathogens under realistic conditions.
The convergence of nanotechnology, materials science, and infection control principles has created a multidisciplinary approach to advancing this technology, with research contributions spanning academic institutions, healthcare systems, and commercial entities worldwide. This collaborative ecosystem continues to drive innovation toward practical implementations that can meaningfully impact hospital infection control strategies.
The evolution of this technology has accelerated in recent decades, driven by increasing concerns about hospital-acquired infections (HAIs) and the emergence of antibiotic-resistant pathogens. Traditional disinfection methods in healthcare settings often face limitations including chemical residues, human error in application, and incomplete coverage of surfaces. Photocatalytic disinfection offers a potential solution by providing continuous antimicrobial activity without additional human intervention after initial application.
Current technological trends in this field include the development of visible light-responsive photocatalysts, nanostructured materials with enhanced surface area, and composite materials that combine multiple functional properties. These innovations aim to overcome the traditional limitations of first-generation photocatalysts, which typically required UV light activation and showed limited efficiency under indoor lighting conditions common in hospital environments.
The primary objective of photocatalytic disinfection in hospital settings is to establish a supplementary layer of continuous disinfection that works alongside conventional cleaning protocols. This approach aims to address the critical gap between scheduled cleaning sessions, during which recontamination frequently occurs. By maintaining antimicrobial activity on high-touch surfaces, photocatalytic technologies could significantly reduce pathogen transmission vectors.
Secondary objectives include reducing reliance on chemical disinfectants, which can contribute to antimicrobial resistance development and pose occupational health risks to healthcare workers through respiratory irritation and dermatological conditions. Additionally, photocatalytic systems aim to provide cost-effective solutions by extending the intervals between intensive manual cleaning, thereby optimizing resource allocation in healthcare facilities.
From a technical perspective, the field is working toward several specific goals: developing photocatalysts with high quantum efficiency under indoor lighting conditions; creating durable coatings that maintain activity for months or years rather than days; ensuring safety for human contact on treated surfaces; and establishing standardized testing protocols to verify efficacy against clinically relevant pathogens under realistic conditions.
The convergence of nanotechnology, materials science, and infection control principles has created a multidisciplinary approach to advancing this technology, with research contributions spanning academic institutions, healthcare systems, and commercial entities worldwide. This collaborative ecosystem continues to drive innovation toward practical implementations that can meaningfully impact hospital infection control strategies.
Healthcare Market Demand for Advanced Sanitation Solutions
The healthcare sector is witnessing an unprecedented demand for advanced sanitation solutions, driven primarily by the increasing prevalence of healthcare-associated infections (HAIs) and the emergence of antimicrobial-resistant organisms. According to the Centers for Disease Control and Prevention, approximately 1 in 31 hospital patients acquires at least one HAI daily, resulting in nearly 100,000 deaths annually in the United States alone. This alarming statistic has created a substantial market need for innovative disinfection technologies that can supplement traditional cleaning protocols.
The global healthcare sanitation market was valued at $32.6 billion in 2022 and is projected to reach $46.3 billion by 2028, growing at a CAGR of 6.2%. This growth is particularly pronounced in developed regions such as North America and Europe, where stringent regulatory frameworks regarding hospital hygiene have been established. However, emerging economies in Asia-Pacific and Latin America are rapidly catching up as healthcare infrastructure improves and awareness regarding infection control increases.
Hospital administrators and infection control specialists are increasingly seeking solutions that offer continuous disinfection capabilities rather than periodic interventions. This shift in preference stems from the recognition that pathogens can recolonize surfaces within minutes after standard cleaning procedures. Photocatalytic disinfection technologies address this need by providing persistent antimicrobial activity, thereby reducing the frequency of manual cleaning while maintaining higher overall hygiene standards.
The COVID-19 pandemic has significantly accelerated market demand, with hospitals worldwide reassessing and upgrading their sanitation protocols. A survey conducted among 500 healthcare facilities revealed that 78% have increased their sanitation budgets since 2020, with 63% specifically allocating funds for advanced disinfection technologies. This trend is expected to continue even post-pandemic as heightened awareness regarding infection control becomes the new normal in healthcare settings.
Cost-effectiveness has emerged as a critical factor driving market demand. Healthcare facilities are increasingly recognizing that investments in advanced sanitation technologies translate to substantial savings through reduced HAI rates, decreased antibiotic usage, shorter patient stays, and lower staff absenteeism. Economic analyses indicate that hospitals implementing comprehensive advanced sanitation protocols can achieve return on investment within 12-18 months through these indirect savings.
Patient expectations are also evolving, with healthcare consumers becoming more informed about infection risks and more selective about their choice of healthcare providers. Hospitals that visibly implement advanced sanitation technologies often report higher patient satisfaction scores and improved reputation metrics, creating additional market incentives for adoption of technologies like photocatalytic disinfection.
The global healthcare sanitation market was valued at $32.6 billion in 2022 and is projected to reach $46.3 billion by 2028, growing at a CAGR of 6.2%. This growth is particularly pronounced in developed regions such as North America and Europe, where stringent regulatory frameworks regarding hospital hygiene have been established. However, emerging economies in Asia-Pacific and Latin America are rapidly catching up as healthcare infrastructure improves and awareness regarding infection control increases.
Hospital administrators and infection control specialists are increasingly seeking solutions that offer continuous disinfection capabilities rather than periodic interventions. This shift in preference stems from the recognition that pathogens can recolonize surfaces within minutes after standard cleaning procedures. Photocatalytic disinfection technologies address this need by providing persistent antimicrobial activity, thereby reducing the frequency of manual cleaning while maintaining higher overall hygiene standards.
The COVID-19 pandemic has significantly accelerated market demand, with hospitals worldwide reassessing and upgrading their sanitation protocols. A survey conducted among 500 healthcare facilities revealed that 78% have increased their sanitation budgets since 2020, with 63% specifically allocating funds for advanced disinfection technologies. This trend is expected to continue even post-pandemic as heightened awareness regarding infection control becomes the new normal in healthcare settings.
Cost-effectiveness has emerged as a critical factor driving market demand. Healthcare facilities are increasingly recognizing that investments in advanced sanitation technologies translate to substantial savings through reduced HAI rates, decreased antibiotic usage, shorter patient stays, and lower staff absenteeism. Economic analyses indicate that hospitals implementing comprehensive advanced sanitation protocols can achieve return on investment within 12-18 months through these indirect savings.
Patient expectations are also evolving, with healthcare consumers becoming more informed about infection risks and more selective about their choice of healthcare providers. Hospitals that visibly implement advanced sanitation technologies often report higher patient satisfaction scores and improved reputation metrics, creating additional market incentives for adoption of technologies like photocatalytic disinfection.
Current Status and Challenges in Hospital Disinfection Technologies
Hospital disinfection technologies have evolved significantly over the past decades, yet continue to face substantial challenges in effectively eliminating pathogens in healthcare environments. Traditional disinfection methods predominantly rely on chemical agents such as quaternary ammonium compounds, hydrogen peroxide, sodium hypochlorite, and alcohol-based solutions. While these methods have demonstrated efficacy against many pathogens, they present limitations including chemical residue concerns, potential material damage, and incomplete coverage of complex surfaces.
Manual cleaning and disinfection protocols remain the backbone of hospital sanitation globally, but suffer from inconsistent application, human error, and labor intensity. Studies indicate that up to 50% of high-touch surfaces may remain contaminated after standard cleaning procedures, creating reservoirs for healthcare-associated infections (HAIs).
Automated technologies have emerged to address these shortcomings, including ultraviolet (UV) light systems, hydrogen peroxide vapor, and electrostatic sprayers. UV-C disinfection systems have gained prominence for their ability to inactivate microorganisms without chemical residues, yet they require direct line-of-sight exposure and cannot penetrate shadows or covered surfaces. Hydrogen peroxide vapor systems offer excellent penetration but necessitate room sealing and extended contact times.
The geographic distribution of advanced disinfection technologies reveals significant disparities, with higher adoption rates in North America and Western Europe compared to developing regions. This disparity is primarily driven by cost barriers, infrastructure limitations, and varying regulatory frameworks.
A critical challenge facing current disinfection technologies is the rise of antimicrobial resistance (AMR). The World Health Organization has identified AMR as one of the top ten global public health threats, with hospital environments serving as potential breeding grounds for resistant organisms. Chemical disinfectants, when improperly used, may contribute to selective pressure favoring resistant strains.
Environmental concerns also present significant challenges, as many conventional disinfectants contain compounds harmful to ecosystems when discharged into wastewater systems. Additionally, occupational health risks for healthcare workers exposed to chemical disinfectants include respiratory irritation, dermatitis, and potential long-term health effects.
The COVID-19 pandemic has intensified focus on hospital disinfection protocols, highlighting both strengths and weaknesses in existing systems. While the pandemic accelerated adoption of advanced technologies like UV robots and electrostatic sprayers, it also exposed vulnerabilities in supply chains and standardization of protocols across different healthcare settings.
Photocatalytic disinfection represents an emerging technology addressing several of these challenges, offering continuous disinfection capabilities without the limitations of traditional methods. However, its integration into existing hospital protocols faces hurdles including initial implementation costs, staff training requirements, and the need for further validation studies in diverse healthcare settings.
Manual cleaning and disinfection protocols remain the backbone of hospital sanitation globally, but suffer from inconsistent application, human error, and labor intensity. Studies indicate that up to 50% of high-touch surfaces may remain contaminated after standard cleaning procedures, creating reservoirs for healthcare-associated infections (HAIs).
Automated technologies have emerged to address these shortcomings, including ultraviolet (UV) light systems, hydrogen peroxide vapor, and electrostatic sprayers. UV-C disinfection systems have gained prominence for their ability to inactivate microorganisms without chemical residues, yet they require direct line-of-sight exposure and cannot penetrate shadows or covered surfaces. Hydrogen peroxide vapor systems offer excellent penetration but necessitate room sealing and extended contact times.
The geographic distribution of advanced disinfection technologies reveals significant disparities, with higher adoption rates in North America and Western Europe compared to developing regions. This disparity is primarily driven by cost barriers, infrastructure limitations, and varying regulatory frameworks.
A critical challenge facing current disinfection technologies is the rise of antimicrobial resistance (AMR). The World Health Organization has identified AMR as one of the top ten global public health threats, with hospital environments serving as potential breeding grounds for resistant organisms. Chemical disinfectants, when improperly used, may contribute to selective pressure favoring resistant strains.
Environmental concerns also present significant challenges, as many conventional disinfectants contain compounds harmful to ecosystems when discharged into wastewater systems. Additionally, occupational health risks for healthcare workers exposed to chemical disinfectants include respiratory irritation, dermatitis, and potential long-term health effects.
The COVID-19 pandemic has intensified focus on hospital disinfection protocols, highlighting both strengths and weaknesses in existing systems. While the pandemic accelerated adoption of advanced technologies like UV robots and electrostatic sprayers, it also exposed vulnerabilities in supply chains and standardization of protocols across different healthcare settings.
Photocatalytic disinfection represents an emerging technology addressing several of these challenges, offering continuous disinfection capabilities without the limitations of traditional methods. However, its integration into existing hospital protocols faces hurdles including initial implementation costs, staff training requirements, and the need for further validation studies in diverse healthcare settings.
Current Photocatalytic Implementation Strategies for Hospital Settings
01 TiO2-based photocatalytic disinfection systems
Titanium dioxide (TiO2) is widely used as a photocatalyst in disinfection systems due to its ability to generate reactive oxygen species when exposed to UV light. These systems can effectively inactivate bacteria, viruses, and other pathogens on surfaces and in water. The photocatalytic reaction occurs when TiO2 absorbs UV radiation, creating electron-hole pairs that produce hydroxyl radicals and superoxide ions, which destroy microorganisms by oxidizing their cell components.- TiO2-based photocatalytic disinfection systems: Titanium dioxide (TiO2) is widely used as a photocatalyst in disinfection systems due to its ability to generate reactive oxygen species when exposed to UV light. These systems can effectively eliminate bacteria, viruses, and other pathogens from surfaces, water, and air. The protocols typically involve coating surfaces with TiO2 or incorporating it into filtration systems, followed by UV light exposure to activate the photocatalytic process. This approach offers a chemical-free disinfection method with long-lasting antimicrobial effects.
- UV-activated photocatalytic sanitation devices: Specialized devices that combine UV light sources with photocatalytic materials for enhanced disinfection performance. These devices are designed for various applications including water purification, air cleaning, and surface sterilization. The protocols involve positioning the device appropriately, activating the UV light source, and allowing sufficient exposure time for complete disinfection. Some advanced systems incorporate sensors to monitor disinfection effectiveness and automatically adjust parameters for optimal performance.
- Portable photocatalytic disinfection solutions: Compact and mobile photocatalytic systems designed for on-the-go disinfection needs. These solutions typically utilize small UV-LED light sources combined with photocatalytic materials in handheld devices, wands, or portable units. The protocols involve bringing the device in close proximity to the target surface, activating the light source, and maintaining exposure for a specified duration. These systems are particularly useful for travel, emergency situations, or areas with limited access to traditional disinfection infrastructure.
- Advanced photocatalytic materials for enhanced disinfection: Novel photocatalytic materials and composites developed to improve disinfection efficiency and expand the spectrum of light activation. These include doped titanium dioxide, zinc oxide nanoparticles, graphene-based composites, and hybrid materials. The protocols involve applying these advanced materials as coatings or incorporating them into disinfection systems, followed by exposure to appropriate light sources. These materials often enable visible light activation, reducing energy requirements and allowing for continuous disinfection under ambient lighting conditions.
- Automated photocatalytic disinfection systems: Integrated systems that combine photocatalytic technology with automation for continuous or scheduled disinfection of spaces and surfaces. These systems typically include programmable light sources, photocatalytic materials, sensors, and control mechanisms. The protocols involve setting up the system, programming disinfection schedules, and monitoring performance through connected interfaces. Some advanced systems incorporate artificial intelligence to optimize disinfection parameters based on usage patterns, contamination levels, and environmental conditions.
02 UV-activated photocatalytic sanitation devices
Specialized devices incorporating UV light sources and photocatalytic materials have been developed for sanitation purposes. These devices can be designed as portable units, fixed installations, or integrated systems for various applications including air purification, water treatment, and surface disinfection. The protocols for using these devices typically involve controlled exposure times, specific light wavelengths, and strategic placement to maximize disinfection efficacy while ensuring safety for users.Expand Specific Solutions03 Advanced photocatalytic materials for enhanced disinfection
Research has led to the development of advanced photocatalytic materials with improved disinfection capabilities. These include doped photocatalysts, composite materials, and nanostructured catalysts that can operate under visible light rather than just UV radiation. Such innovations allow for more energy-efficient disinfection protocols and broader application scenarios. The enhanced photocatalytic materials demonstrate higher quantum efficiency and faster pathogen inactivation rates compared to traditional photocatalysts.Expand Specific Solutions04 Photocatalytic disinfection for water treatment systems
Specialized protocols have been developed for implementing photocatalytic disinfection in water treatment applications. These protocols address factors such as water turbidity, flow rate, contact time, and catalyst configuration to ensure effective pathogen removal. The systems can be designed for various scales, from point-of-use devices to municipal water treatment facilities. Photocatalytic water treatment offers advantages including minimal chemical input, reduction of disinfection byproducts, and effectiveness against chlorine-resistant microorganisms.Expand Specific Solutions05 Integrated photocatalytic sanitation protocols for public spaces
Comprehensive sanitation protocols combining photocatalytic technology with other disinfection methods have been developed for public spaces such as hospitals, schools, and transportation hubs. These integrated approaches include surface coating with photocatalytic materials, scheduled UV exposure, and monitoring systems to verify disinfection efficacy. The protocols typically specify implementation procedures, maintenance requirements, and performance validation methods to ensure consistent pathogen reduction in high-traffic environments.Expand Specific Solutions
Leading Manufacturers and Research Institutions in Photocatalytic Technology
Photocatalytic disinfection technology is emerging as a significant advancement in hospital sanitation protocols, currently in the growth phase with an estimated market size of $1.2-1.5 billion and projected annual growth of 8-10%. The competitive landscape features established healthcare companies like Fresenius Medical Care and FUJIFILM alongside specialized disinfection technology providers such as Synexis LLC and Aleddra. Academic institutions including University of Florida and Arizona State University are driving fundamental research, while companies like Signify Holding and Current Lighting Solutions are integrating photocatalytic technology into lighting systems. The technology is approaching maturity with commercial applications becoming more widespread, though ongoing research continues to enhance efficacy and reduce implementation costs.
Signify Holding BV
Technical Solution: Signify (formerly Philips Lighting) has developed advanced UV-C based photocatalytic disinfection systems specifically designed for healthcare environments. Their technology combines UV-C light with titanium dioxide (TiO2) photocatalysts to create powerful oxidizing agents that destroy bacteria, viruses, and other pathogens on surfaces and in air. The system works by activating the photocatalyst with specific wavelengths of UV light, generating reactive oxygen species (ROS) including hydroxyl radicals and hydrogen peroxide that break down organic contaminants and microbial cell structures. Signify's solutions include both fixed installation systems for operating rooms and patient rooms, as well as mobile units that can be deployed for targeted disinfection. Their systems incorporate safety features that prevent human exposure to UV radiation while maximizing disinfection efficacy. Clinical studies have demonstrated up to 99.9999% reduction in pathogens including MRSA, C. difficile, and coronaviruses in hospital settings when using their photocatalytic technology.
Strengths: Industry-leading expertise in lighting and UV technology; global distribution network; comprehensive safety features; proven efficacy against healthcare-associated pathogens. Weaknesses: Higher initial investment compared to conventional chemical disinfection; requires professional installation; effectiveness can be reduced in areas with physical shadows or obstructions.
Ondine International Holdings Ltd.
Technical Solution: Ondine has pioneered Photodisinfection Technology (PDT) specifically for healthcare applications, utilizing a proprietary approach that combines non-toxic photosensitizers with specific wavelengths of visible light. Their technology differs from traditional photocatalysis by employing photosensitizer molecules that selectively bind to microbial cell structures. When activated by specific wavelengths (typically 630-670nm red light), these photosensitizers generate singlet oxygen and other reactive species that rapidly destroy pathogens without damaging human tissues. Ondine's MRSAid system specifically targets hospital-acquired infections by treating patient nares and other colonization sites to reduce pathogen reservoirs. Clinical studies in multiple hospitals have demonstrated that implementation of Ondine's photodisinfection protocols reduced surgical site infections by up to 84% and ventilator-associated pneumonia by 56%. The technology is particularly valuable for disinfecting complex medical devices and surfaces that cannot be effectively treated with traditional methods. Ondine's systems are designed for integration into existing hospital workflows with minimal disruption to clinical operations.
Strengths: Highly selective antimicrobial action; effective against drug-resistant pathogens; non-toxic to human tissues; can be used in presence of patients; no development of microbial resistance. Weaknesses: Requires direct light exposure to target areas; more suitable for targeted applications than whole-room disinfection; higher operational costs compared to basic UV systems.
Key Photocatalytic Materials and Mechanisms for Pathogen Elimination
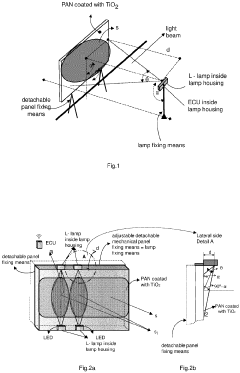
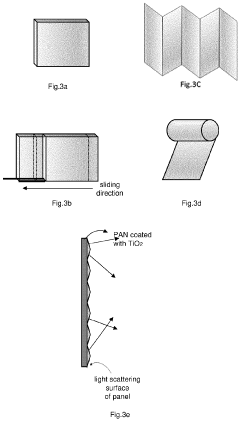
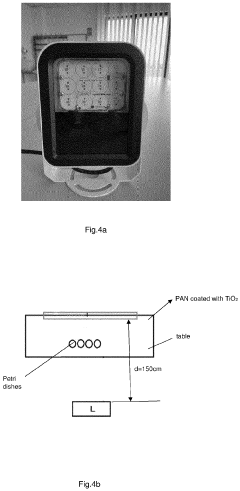
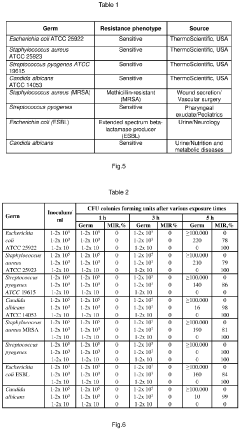
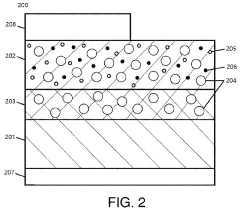
Medical device for disinfecting a volume of a hospital indoor environment and method for said disinfection
PatentPendingEP4389159A1
Innovation
- A portable medical device with a titanium dioxide TiO2 nanoparticle-coated panel and an LED irradiating lamp, controlled by an electronic unit, which adjusts power and duration based on environment volume and type, allowing flexible placement and low-energy operation, ensuring effective photocatalytic disinfection.
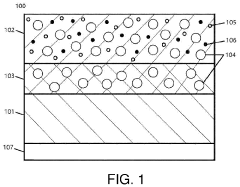
Self-Disinfecting Photocatalyst Sheet
PatentInactiveUS20220089912A1
Innovation
- A self-disinfecting photocatalyst sheet with a covalent bond between a metal oxide primary photocatalyst and substrate, activated by visible light, featuring a secondary metallic photocatalyst for enhanced disinfection and an optional adhesive layer for attachment, along with a color-changing dye for wear-indication.
Antimicrobial Resistance Considerations in Photocatalytic Applications
The emergence of antimicrobial resistance (AMR) represents one of the most significant challenges in modern healthcare settings. As conventional disinfection methods face increasing limitations due to resistant pathogens, photocatalytic disinfection technologies offer a promising alternative approach that may help address these concerns. Understanding the relationship between photocatalytic applications and antimicrobial resistance is crucial for developing effective hospital sanitation protocols.
Photocatalytic disinfection operates through fundamentally different mechanisms than traditional antimicrobial agents. While conventional antibiotics and disinfectants typically target specific cellular components or metabolic pathways, photocatalytic processes generate reactive oxygen species (ROS) that attack multiple cellular targets simultaneously. This multi-target approach significantly reduces the likelihood of resistance development, as microorganisms would need to evolve multiple defensive mechanisms concurrently.
Research indicates that titanium dioxide (TiO₂) and other photocatalysts demonstrate consistent efficacy against resistant bacterial strains, including methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant Enterococci (VRE). Studies have shown that these resistant pathogens exhibit similar susceptibility to photocatalytic treatment as their non-resistant counterparts, suggesting no cross-resistance between conventional antimicrobials and photocatalytic processes.
Long-term investigations into potential resistance development against photocatalytic treatments have yielded encouraging results. Even after repeated sub-lethal exposures to photocatalytic disinfection, microorganisms show minimal adaptation or resistance development. This contrasts sharply with conventional disinfectants, where resistance can emerge relatively quickly through selective pressure and genetic adaptation.
The integration of photocatalytic technologies into hospital environments may also reduce the overall use of conventional antimicrobial agents, thereby decreasing selective pressure that drives resistance development. Self-disinfecting surfaces incorporating photocatalysts can maintain continuous antimicrobial activity without requiring repeated application of chemical disinfectants, potentially slowing the emergence of resistant strains in healthcare settings.
However, challenges remain in optimizing photocatalytic systems to ensure complete microbial elimination. Incomplete inactivation could potentially create selective pressure for more resistant subpopulations. Therefore, careful design and implementation of photocatalytic systems are essential to maximize efficacy and minimize resistance risks.
From a public health perspective, photocatalytic disinfection represents a valuable tool in the broader antimicrobial stewardship strategy. By providing an alternative mechanism for pathogen control that does not contribute to conventional resistance patterns, these technologies may help preserve the efficacy of critical antimicrobial agents while maintaining effective infection control in healthcare environments.
Photocatalytic disinfection operates through fundamentally different mechanisms than traditional antimicrobial agents. While conventional antibiotics and disinfectants typically target specific cellular components or metabolic pathways, photocatalytic processes generate reactive oxygen species (ROS) that attack multiple cellular targets simultaneously. This multi-target approach significantly reduces the likelihood of resistance development, as microorganisms would need to evolve multiple defensive mechanisms concurrently.
Research indicates that titanium dioxide (TiO₂) and other photocatalysts demonstrate consistent efficacy against resistant bacterial strains, including methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant Enterococci (VRE). Studies have shown that these resistant pathogens exhibit similar susceptibility to photocatalytic treatment as their non-resistant counterparts, suggesting no cross-resistance between conventional antimicrobials and photocatalytic processes.
Long-term investigations into potential resistance development against photocatalytic treatments have yielded encouraging results. Even after repeated sub-lethal exposures to photocatalytic disinfection, microorganisms show minimal adaptation or resistance development. This contrasts sharply with conventional disinfectants, where resistance can emerge relatively quickly through selective pressure and genetic adaptation.
The integration of photocatalytic technologies into hospital environments may also reduce the overall use of conventional antimicrobial agents, thereby decreasing selective pressure that drives resistance development. Self-disinfecting surfaces incorporating photocatalysts can maintain continuous antimicrobial activity without requiring repeated application of chemical disinfectants, potentially slowing the emergence of resistant strains in healthcare settings.
However, challenges remain in optimizing photocatalytic systems to ensure complete microbial elimination. Incomplete inactivation could potentially create selective pressure for more resistant subpopulations. Therefore, careful design and implementation of photocatalytic systems are essential to maximize efficacy and minimize resistance risks.
From a public health perspective, photocatalytic disinfection represents a valuable tool in the broader antimicrobial stewardship strategy. By providing an alternative mechanism for pathogen control that does not contribute to conventional resistance patterns, these technologies may help preserve the efficacy of critical antimicrobial agents while maintaining effective infection control in healthcare environments.
Integration with Existing Hospital Infection Control Protocols
The integration of photocatalytic disinfection technology into existing hospital infection control protocols represents a critical step in enhancing healthcare facility sanitation. Current hospital protocols typically involve manual cleaning with chemical disinfectants, UV light treatments, and hydrogen peroxide vapor systems. Photocatalytic disinfection offers complementary benefits that can strengthen these established practices without disrupting workflow.
Successful integration requires a multi-phase implementation approach. Initially, hospitals should conduct a comprehensive assessment of current infection control protocols, identifying specific areas where photocatalytic technology can provide maximum benefit. High-touch surfaces and areas with persistent contamination challenges present prime opportunities for implementation. The technology's continuous disinfection capability makes it particularly valuable in high-traffic zones where traditional cleaning intervals may be insufficient.
Protocol modification must address the coexistence of photocatalytic systems with traditional chemical cleaning agents. Some chemical compounds may interfere with photocatalytic reactions, necessitating careful selection of compatible cleaning products. Standard operating procedures should be updated to include maintenance requirements for photocatalytic surfaces and devices, ensuring sustained antimicrobial efficacy over time.
Staff training represents another crucial integration component. Healthcare workers must understand the principles of photocatalytic disinfection, its limitations, and how it complements rather than replaces existing hygiene practices. This educational component helps prevent the "hygiene relaxation effect" where staff might reduce manual cleaning efforts due to overreliance on new technology.
Monitoring and validation protocols require adaptation to incorporate photocatalytic disinfection metrics. Traditional surface sampling and ATP testing can verify immediate disinfection efficacy, while environmental monitoring should track long-term impacts on hospital-acquired infection rates. Integration of these measurements into existing infection control dashboards provides administrators with comprehensive sanitation performance data.
Regulatory compliance presents another integration consideration. Hospital infection control committees must ensure photocatalytic technologies meet relevant healthcare standards and are appropriately documented in facility infection prevention plans. This documentation should address how the technology supports existing protocols in meeting regulatory requirements from organizations such as the CDC, WHO, and national healthcare authorities.
Cost-effective implementation strategies can include phased deployment, beginning with high-risk areas such as operating rooms, intensive care units, and isolation rooms before expanding to general patient care areas. This approach allows for evaluation of real-world performance and refinement of integration protocols before facility-wide adoption.
Successful integration requires a multi-phase implementation approach. Initially, hospitals should conduct a comprehensive assessment of current infection control protocols, identifying specific areas where photocatalytic technology can provide maximum benefit. High-touch surfaces and areas with persistent contamination challenges present prime opportunities for implementation. The technology's continuous disinfection capability makes it particularly valuable in high-traffic zones where traditional cleaning intervals may be insufficient.
Protocol modification must address the coexistence of photocatalytic systems with traditional chemical cleaning agents. Some chemical compounds may interfere with photocatalytic reactions, necessitating careful selection of compatible cleaning products. Standard operating procedures should be updated to include maintenance requirements for photocatalytic surfaces and devices, ensuring sustained antimicrobial efficacy over time.
Staff training represents another crucial integration component. Healthcare workers must understand the principles of photocatalytic disinfection, its limitations, and how it complements rather than replaces existing hygiene practices. This educational component helps prevent the "hygiene relaxation effect" where staff might reduce manual cleaning efforts due to overreliance on new technology.
Monitoring and validation protocols require adaptation to incorporate photocatalytic disinfection metrics. Traditional surface sampling and ATP testing can verify immediate disinfection efficacy, while environmental monitoring should track long-term impacts on hospital-acquired infection rates. Integration of these measurements into existing infection control dashboards provides administrators with comprehensive sanitation performance data.
Regulatory compliance presents another integration consideration. Hospital infection control committees must ensure photocatalytic technologies meet relevant healthcare standards and are appropriately documented in facility infection prevention plans. This documentation should address how the technology supports existing protocols in meeting regulatory requirements from organizations such as the CDC, WHO, and national healthcare authorities.
Cost-effective implementation strategies can include phased deployment, beginning with high-risk areas such as operating rooms, intensive care units, and isolation rooms before expanding to general patient care areas. This approach allows for evaluation of real-world performance and refinement of integration protocols before facility-wide adoption.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!