Carbolic Acid Effects on Increasing Biocompatibility in Medical Devices
JUL 22, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Carbolic Acid Biocompatibility Background
Carbolic acid, also known as phenol, has a long and significant history in the field of medical devices and biocompatibility. Its journey began in the late 19th century when Joseph Lister, a British surgeon, pioneered its use as an antiseptic in surgical procedures. This marked a revolutionary step in reducing post-operative infections and mortality rates, setting the stage for modern surgical practices.
The concept of biocompatibility in medical devices emerged as a critical consideration in the mid-20th century, coinciding with the rapid advancement of biomaterials and implantable devices. Researchers began to recognize the importance of creating materials that could interact harmoniously with the human body, minimizing adverse reactions and promoting healing.
In this context, carbolic acid's role evolved from a purely antiseptic agent to a potential modifier of material surfaces. Scientists discovered that controlled application of carbolic acid could alter the surface properties of certain materials, potentially enhancing their biocompatibility. This finding opened up new avenues for research in the field of medical device development.
The mechanism by which carbolic acid influences biocompatibility is multifaceted. It can modify surface chemistry, altering the way proteins and cells interact with the material. Additionally, its ability to create micro-textures on surfaces can affect cell adhesion and proliferation, key factors in the integration of medical devices with surrounding tissues.
Over the years, researchers have explored various concentrations and application methods of carbolic acid to optimize its effects on different materials used in medical devices. These studies have ranged from investigating its impact on polymers and metals to examining its potential in enhancing the performance of implants, catheters, and other biomedical devices.
The goal of incorporating carbolic acid in medical device development is to create surfaces that are not only non-toxic and non-immunogenic but also promote positive biological responses. This includes improved cell adhesion, reduced inflammation, and enhanced tissue integration. Such advancements are crucial in developing medical devices that can function effectively over long periods without causing adverse reactions in the body.
As research in this field progresses, the focus has shifted towards understanding the long-term effects of carbolic acid-modified surfaces and developing standardized protocols for its application in medical device manufacturing. This ongoing work aims to harness the full potential of carbolic acid in creating the next generation of biocompatible medical devices, potentially revolutionizing patient care and treatment outcomes.
The concept of biocompatibility in medical devices emerged as a critical consideration in the mid-20th century, coinciding with the rapid advancement of biomaterials and implantable devices. Researchers began to recognize the importance of creating materials that could interact harmoniously with the human body, minimizing adverse reactions and promoting healing.
In this context, carbolic acid's role evolved from a purely antiseptic agent to a potential modifier of material surfaces. Scientists discovered that controlled application of carbolic acid could alter the surface properties of certain materials, potentially enhancing their biocompatibility. This finding opened up new avenues for research in the field of medical device development.
The mechanism by which carbolic acid influences biocompatibility is multifaceted. It can modify surface chemistry, altering the way proteins and cells interact with the material. Additionally, its ability to create micro-textures on surfaces can affect cell adhesion and proliferation, key factors in the integration of medical devices with surrounding tissues.
Over the years, researchers have explored various concentrations and application methods of carbolic acid to optimize its effects on different materials used in medical devices. These studies have ranged from investigating its impact on polymers and metals to examining its potential in enhancing the performance of implants, catheters, and other biomedical devices.
The goal of incorporating carbolic acid in medical device development is to create surfaces that are not only non-toxic and non-immunogenic but also promote positive biological responses. This includes improved cell adhesion, reduced inflammation, and enhanced tissue integration. Such advancements are crucial in developing medical devices that can function effectively over long periods without causing adverse reactions in the body.
As research in this field progresses, the focus has shifted towards understanding the long-term effects of carbolic acid-modified surfaces and developing standardized protocols for its application in medical device manufacturing. This ongoing work aims to harness the full potential of carbolic acid in creating the next generation of biocompatible medical devices, potentially revolutionizing patient care and treatment outcomes.
Medical Device Market Analysis
The medical device market has experienced significant growth in recent years, driven by technological advancements, an aging population, and increasing healthcare expenditure. The global medical device market was valued at approximately $456 billion in 2021 and is projected to reach $658 billion by 2028, growing at a CAGR of 5.4% during the forecast period.
Biocompatibility is a critical factor in the medical device industry, as it directly impacts patient safety and device efficacy. The market for biocompatible materials and coatings is expected to grow at a faster rate than the overall medical device market, with a CAGR of 7.8% from 2021 to 2028. This growth is primarily attributed to the increasing demand for implantable devices and the need for improved patient outcomes.
The use of carbolic acid (phenol) in medical devices to enhance biocompatibility represents a niche but growing segment within the broader biocompatible materials market. While specific market data for carbolic acid in medical devices is limited, the overall trend towards improved biocompatibility suggests a positive outlook for this application.
Key market drivers for biocompatible materials, including carbolic acid-based solutions, include the rising prevalence of chronic diseases, increasing surgical procedures, and growing awareness of healthcare-associated infections. Additionally, stringent regulatory requirements for medical device safety and performance are pushing manufacturers to invest in advanced biocompatible materials and surface treatments.
The medical device market is highly competitive, with major players such as Medtronic, Johnson & Johnson, and Abbott Laboratories dominating the industry. These companies are actively investing in research and development to improve device biocompatibility and reduce the risk of adverse reactions. Smaller, specialized companies focusing on biocompatible materials and surface treatments are also gaining traction in the market.
Geographically, North America holds the largest share of the medical device market, followed by Europe and Asia-Pacific. However, emerging markets in Asia-Pacific and Latin America are expected to grow at a faster rate due to improving healthcare infrastructure and increasing healthcare spending.
The COVID-19 pandemic has had a mixed impact on the medical device market. While elective procedures saw a decline, there was an increased demand for critical care devices and personal protective equipment. The pandemic has also accelerated the adoption of telemedicine and remote patient monitoring devices, creating new opportunities for biocompatible wearable and implantable technologies.
Biocompatibility is a critical factor in the medical device industry, as it directly impacts patient safety and device efficacy. The market for biocompatible materials and coatings is expected to grow at a faster rate than the overall medical device market, with a CAGR of 7.8% from 2021 to 2028. This growth is primarily attributed to the increasing demand for implantable devices and the need for improved patient outcomes.
The use of carbolic acid (phenol) in medical devices to enhance biocompatibility represents a niche but growing segment within the broader biocompatible materials market. While specific market data for carbolic acid in medical devices is limited, the overall trend towards improved biocompatibility suggests a positive outlook for this application.
Key market drivers for biocompatible materials, including carbolic acid-based solutions, include the rising prevalence of chronic diseases, increasing surgical procedures, and growing awareness of healthcare-associated infections. Additionally, stringent regulatory requirements for medical device safety and performance are pushing manufacturers to invest in advanced biocompatible materials and surface treatments.
The medical device market is highly competitive, with major players such as Medtronic, Johnson & Johnson, and Abbott Laboratories dominating the industry. These companies are actively investing in research and development to improve device biocompatibility and reduce the risk of adverse reactions. Smaller, specialized companies focusing on biocompatible materials and surface treatments are also gaining traction in the market.
Geographically, North America holds the largest share of the medical device market, followed by Europe and Asia-Pacific. However, emerging markets in Asia-Pacific and Latin America are expected to grow at a faster rate due to improving healthcare infrastructure and increasing healthcare spending.
The COVID-19 pandemic has had a mixed impact on the medical device market. While elective procedures saw a decline, there was an increased demand for critical care devices and personal protective equipment. The pandemic has also accelerated the adoption of telemedicine and remote patient monitoring devices, creating new opportunities for biocompatible wearable and implantable technologies.
Carbolic Acid Application Challenges
The application of carbolic acid to enhance biocompatibility in medical devices faces several significant challenges. One of the primary obstacles is the precise control of carbolic acid concentration. While carbolic acid has shown potential in improving biocompatibility, its effectiveness is highly dependent on the exact dosage applied. Too little may not yield the desired biocompatibility improvements, while excessive amounts can lead to cytotoxicity and tissue damage.
Another challenge lies in the uniform distribution of carbolic acid across the surface of medical devices. Achieving a consistent and even layer is crucial for optimal biocompatibility enhancement. However, the complex geometries and varied materials used in medical devices can make this process difficult, potentially resulting in areas with inadequate coverage or excessive accumulation.
The long-term stability of carbolic acid treatments presents an additional hurdle. Medical devices often need to maintain their biocompatibility properties over extended periods, sometimes for years. Ensuring that the carbolic acid treatment remains effective and does not degrade or leach out over time is a significant challenge that requires extensive testing and validation.
Compatibility with sterilization processes is another critical issue. Many medical devices undergo rigorous sterilization procedures, such as autoclaving or gamma irradiation. These processes can potentially alter or degrade the carbolic acid treatment, compromising its biocompatibility-enhancing properties. Developing treatments that can withstand various sterilization methods without losing efficacy is essential.
Regulatory compliance and safety concerns also pose substantial challenges. Carbolic acid, despite its potential benefits, is known for its toxicity at higher concentrations. Demonstrating the safety and efficacy of carbolic acid treatments to regulatory bodies like the FDA requires extensive clinical trials and safety studies. This process can be time-consuming and costly, potentially slowing down the adoption of this technology in medical devices.
Furthermore, the interaction between carbolic acid and different biomaterials used in medical devices needs careful consideration. The acid may react differently with various polymers, metals, or ceramics commonly used in device fabrication. Understanding and optimizing these interactions to ensure both biocompatibility enhancement and material integrity is a complex task that requires extensive research and development efforts.
Lastly, the scalability of carbolic acid treatments for mass production of medical devices presents logistical and technical challenges. Developing processes that can efficiently and consistently apply carbolic acid treatments to large quantities of devices while maintaining quality control is crucial for widespread adoption in the medical device industry.
Another challenge lies in the uniform distribution of carbolic acid across the surface of medical devices. Achieving a consistent and even layer is crucial for optimal biocompatibility enhancement. However, the complex geometries and varied materials used in medical devices can make this process difficult, potentially resulting in areas with inadequate coverage or excessive accumulation.
The long-term stability of carbolic acid treatments presents an additional hurdle. Medical devices often need to maintain their biocompatibility properties over extended periods, sometimes for years. Ensuring that the carbolic acid treatment remains effective and does not degrade or leach out over time is a significant challenge that requires extensive testing and validation.
Compatibility with sterilization processes is another critical issue. Many medical devices undergo rigorous sterilization procedures, such as autoclaving or gamma irradiation. These processes can potentially alter or degrade the carbolic acid treatment, compromising its biocompatibility-enhancing properties. Developing treatments that can withstand various sterilization methods without losing efficacy is essential.
Regulatory compliance and safety concerns also pose substantial challenges. Carbolic acid, despite its potential benefits, is known for its toxicity at higher concentrations. Demonstrating the safety and efficacy of carbolic acid treatments to regulatory bodies like the FDA requires extensive clinical trials and safety studies. This process can be time-consuming and costly, potentially slowing down the adoption of this technology in medical devices.
Furthermore, the interaction between carbolic acid and different biomaterials used in medical devices needs careful consideration. The acid may react differently with various polymers, metals, or ceramics commonly used in device fabrication. Understanding and optimizing these interactions to ensure both biocompatibility enhancement and material integrity is a complex task that requires extensive research and development efforts.
Lastly, the scalability of carbolic acid treatments for mass production of medical devices presents logistical and technical challenges. Developing processes that can efficiently and consistently apply carbolic acid treatments to large quantities of devices while maintaining quality control is crucial for widespread adoption in the medical device industry.
Current Carbolic Acid Solutions
01 Biocompatible carbolic acid formulations
Development of biocompatible formulations containing carbolic acid for medical and pharmaceutical applications. These formulations aim to reduce the toxicity and irritation associated with carbolic acid while maintaining its therapeutic properties. Various excipients and delivery systems are used to enhance biocompatibility and control release.- Biocompatible carbolic acid formulations: Development of biocompatible formulations containing carbolic acid for medical and pharmaceutical applications. These formulations aim to reduce the toxicity and irritation associated with carbolic acid while maintaining its antimicrobial properties. Various excipients and delivery systems are used to improve the biocompatibility of carbolic acid-based products.
- Carbolic acid in medical devices: Incorporation of carbolic acid into medical devices to enhance their antimicrobial properties while ensuring biocompatibility. This includes the development of coatings, materials, and structures that can safely release carbolic acid in controlled amounts, reducing the risk of infection without causing harm to surrounding tissues.
- Carbolic acid derivatives with improved biocompatibility: Synthesis and evaluation of carbolic acid derivatives that maintain the desired antimicrobial activity while exhibiting enhanced biocompatibility. These modified compounds are designed to reduce toxicity and improve tissue tolerance, making them suitable for various medical and pharmaceutical applications.
- Biocompatible delivery systems for carbolic acid: Development of novel delivery systems that improve the biocompatibility of carbolic acid. These systems may include encapsulation technologies, controlled release mechanisms, and targeted delivery approaches to minimize systemic exposure and localize the antimicrobial effects of carbolic acid.
- Evaluation methods for carbolic acid biocompatibility: Development and standardization of methods to assess the biocompatibility of carbolic acid and its formulations. This includes in vitro and in vivo testing protocols, cytotoxicity assays, and long-term safety studies to ensure the safe use of carbolic acid in various applications while complying with regulatory requirements.
02 Carbolic acid in medical devices
Incorporation of carbolic acid in medical devices to provide antimicrobial properties. The biocompatibility of these devices is improved through careful material selection and surface modifications. This approach allows for the controlled release of carbolic acid to prevent infections while minimizing adverse effects on surrounding tissues.Expand Specific Solutions03 Carbolic acid derivatives with enhanced biocompatibility
Synthesis and evaluation of carbolic acid derivatives designed to have improved biocompatibility profiles. These modified compounds retain the desired therapeutic effects of carbolic acid while reducing toxicity and increasing tissue compatibility. Structure-activity relationships are studied to optimize biocompatibility.Expand Specific Solutions04 Biocompatible coatings containing carbolic acid
Development of biocompatible coatings that incorporate carbolic acid for various applications, including medical implants and wound dressings. These coatings are designed to provide controlled release of carbolic acid while maintaining compatibility with biological tissues. Different coating materials and techniques are explored to optimize biocompatibility and efficacy.Expand Specific Solutions05 Biocompatibility testing methods for carbolic acid products
Establishment and optimization of biocompatibility testing methods specifically tailored for carbolic acid-containing products. These methods assess various aspects of biocompatibility, including cytotoxicity, irritation, sensitization, and systemic toxicity. Standardized protocols are developed to ensure consistent evaluation of carbolic acid formulations across different applications.Expand Specific Solutions
Key Medical Device Manufacturers
The competitive landscape for carbolic acid effects on increasing biocompatibility in medical devices is in a growth phase, with a expanding market size driven by the increasing demand for advanced medical devices. The technology is reaching maturity, with several key players making significant advancements. Companies like Surmodics, Inc., BioInteractions Ltd, and Toray Industries, Inc. are leading the field with innovative surface modification technologies. Bausch & Lomb, Inc. and Medtronic Vascular, Inc. are leveraging their expertise in medical devices to enhance biocompatibility. Research institutions such as Shanghai Jiao Tong University and Massachusetts Institute of Technology are contributing to the scientific advancements, fostering collaborations between academia and industry.
Surmodics, Inc.
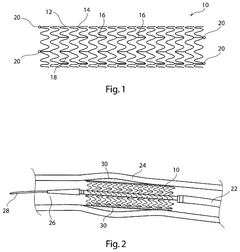
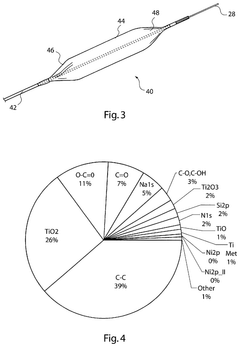
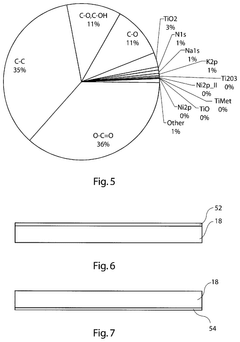
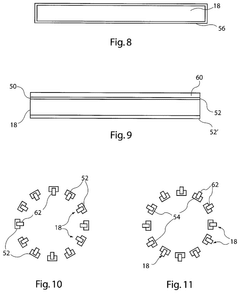
Technical Solution: Surmodics has developed a proprietary PhotoLink coating technology that utilizes carbolic acid derivatives to enhance biocompatibility of medical devices. This process involves the photochemical attachment of biocompatible molecules to device surfaces, creating a durable and uniform coating. The company's approach incorporates phenolic compounds, which are structurally similar to carbolic acid, to form a stable interfacial layer between the device surface and the biocompatible coating[1][3]. This technology has been successfully applied to various medical devices, including catheters, guidewires, and stents, demonstrating improved hemocompatibility and reduced thrombogenicity[2].
Strengths: Versatile application across various medical devices, proven efficacy in reducing thrombogenicity. Weaknesses: May require specialized equipment for coating application, potential for batch-to-batch variability in coating performance.
BioInteractions Ltd
Technical Solution: BioInteractions Ltd has developed a novel approach utilizing carbolic acid derivatives in their Astute Advanced coating technology. This proprietary coating incorporates modified phenolic compounds to create a highly biocompatible surface on medical devices. The company's method involves a multi-layer coating process, where carbolic acid-based molecules are strategically integrated to enhance cell adhesion and promote tissue integration[4]. The coating has been shown to significantly reduce protein adsorption and platelet activation, leading to improved long-term performance of implantable devices[5]. BioInteractions' technology has been particularly effective in cardiovascular applications, such as stents and heart valves.
Strengths: Highly effective in reducing protein adsorption and platelet activation, particularly beneficial for cardiovascular devices. Weaknesses: Complex multi-layer coating process may increase production costs and time.
Innovative Carbolic Acid Research
Coated medical device and method of coating such a device
PatentActiveUS12115288B2
Innovation
- A medical device with a surface coated by a layer of saturated carboxylic acid or its derivative, which acts as an outermost non-porous, non-polymerized layer to mask the device from the body, promoting endothelialization and reducing thrombosis, preferably using citric acid to enhance biocompatibility and adhesion of bioactive agents.
Biopassivating membrane stabilization by means of nitrocarboxylic acid-containing phospholipids in preparations and coatings
PatentInactiveEP2717864A1
Innovation
- The use of nitrocarboxylic acid-containing phospholipids in coatings for medical devices to create a biopassivating surface that reduces cellular reactions like matrix protein production, cell migration, and apoptosis by at least 10-70% compared to uncoated surfaces.
Regulatory Framework for Medical Devices
The regulatory framework for medical devices plays a crucial role in ensuring the safety and efficacy of products that incorporate carbolic acid to enhance biocompatibility. In the United States, the Food and Drug Administration (FDA) oversees the regulation of medical devices through the Center for Devices and Radiological Health (CDRH). The FDA classifies medical devices into three categories based on their risk level and intended use, with Class III devices being subject to the most stringent controls.
For devices utilizing carbolic acid to improve biocompatibility, manufacturers must comply with the premarket approval (PMA) process or the 510(k) clearance pathway, depending on the device classification. The PMA process is typically required for Class III devices and involves comprehensive clinical trials to demonstrate safety and effectiveness. The 510(k) pathway, generally applicable to Class II devices, requires manufacturers to demonstrate substantial equivalence to a predicate device already on the market.
In the European Union, the regulatory landscape for medical devices has undergone significant changes with the implementation of the Medical Device Regulation (MDR) in 2021. The MDR introduces more stringent requirements for clinical evidence, post-market surveillance, and traceability. Devices incorporating carbolic acid for biocompatibility purposes must comply with the Essential Requirements outlined in the MDR, including demonstrating that the benefits outweigh any potential risks associated with the use of the substance.
Globally, the International Organization for Standardization (ISO) provides standards that are widely recognized and adopted by regulatory bodies. ISO 10993 series, particularly ISO 10993-1, is essential for evaluating the biocompatibility of medical devices. Manufacturers must conduct appropriate biological evaluation tests to assess the potential risks associated with the use of carbolic acid in their devices.
Regulatory bodies also require manufacturers to implement and maintain a quality management system (QMS) that complies with standards such as ISO 13485. This ensures consistent production and monitoring of devices throughout their lifecycle. Additionally, post-market surveillance requirements mandate ongoing monitoring and reporting of adverse events related to the use of carbolic acid in medical devices.
As the understanding of biocompatibility and the effects of carbolic acid evolve, regulatory frameworks continue to adapt. Manufacturers must stay informed about changes in regulations and guidelines to ensure ongoing compliance and market access for their devices. This may involve periodic reassessment of the risk-benefit profile of carbolic acid use in medical devices and updating documentation and clinical evidence as required by regulatory authorities.
For devices utilizing carbolic acid to improve biocompatibility, manufacturers must comply with the premarket approval (PMA) process or the 510(k) clearance pathway, depending on the device classification. The PMA process is typically required for Class III devices and involves comprehensive clinical trials to demonstrate safety and effectiveness. The 510(k) pathway, generally applicable to Class II devices, requires manufacturers to demonstrate substantial equivalence to a predicate device already on the market.
In the European Union, the regulatory landscape for medical devices has undergone significant changes with the implementation of the Medical Device Regulation (MDR) in 2021. The MDR introduces more stringent requirements for clinical evidence, post-market surveillance, and traceability. Devices incorporating carbolic acid for biocompatibility purposes must comply with the Essential Requirements outlined in the MDR, including demonstrating that the benefits outweigh any potential risks associated with the use of the substance.
Globally, the International Organization for Standardization (ISO) provides standards that are widely recognized and adopted by regulatory bodies. ISO 10993 series, particularly ISO 10993-1, is essential for evaluating the biocompatibility of medical devices. Manufacturers must conduct appropriate biological evaluation tests to assess the potential risks associated with the use of carbolic acid in their devices.
Regulatory bodies also require manufacturers to implement and maintain a quality management system (QMS) that complies with standards such as ISO 13485. This ensures consistent production and monitoring of devices throughout their lifecycle. Additionally, post-market surveillance requirements mandate ongoing monitoring and reporting of adverse events related to the use of carbolic acid in medical devices.
As the understanding of biocompatibility and the effects of carbolic acid evolve, regulatory frameworks continue to adapt. Manufacturers must stay informed about changes in regulations and guidelines to ensure ongoing compliance and market access for their devices. This may involve periodic reassessment of the risk-benefit profile of carbolic acid use in medical devices and updating documentation and clinical evidence as required by regulatory authorities.
Safety and Toxicity Considerations
Carbolic acid, also known as phenol, has been extensively studied for its potential to enhance biocompatibility in medical devices. However, its use raises significant safety and toxicity concerns that must be carefully addressed. Phenol is a known corrosive and toxic substance, capable of causing severe burns and systemic poisoning upon contact with skin or mucous membranes. Its toxicity profile necessitates a thorough evaluation of potential risks associated with its incorporation into medical devices.
The primary safety concern with carbolic acid is its potential for local tissue damage. Even at low concentrations, phenol can cause irritation, inflammation, and necrosis of tissues it comes into contact with. This is particularly problematic for implantable devices or those in prolonged contact with bodily tissues. The risk of tissue damage must be weighed against any potential biocompatibility benefits, and strategies to mitigate this risk, such as controlled release mechanisms or protective coatings, should be explored.
Systemic toxicity is another critical consideration. If phenol leaches from medical devices into the bloodstream, it can lead to serious health complications. Acute exposure to high levels of phenol can result in central nervous system depression, cardiovascular collapse, and even death. Chronic exposure, even at lower levels, has been associated with liver and kidney damage, as well as potential carcinogenic effects. Therefore, rigorous testing must be conducted to ensure that phenol-containing medical devices do not release harmful amounts of the substance over their intended lifespan.
The potential for allergic reactions and sensitization is also a significant concern. Some individuals may develop hypersensitivity to phenol, leading to allergic contact dermatitis or more severe systemic allergic responses. This risk necessitates careful patient screening and monitoring when using phenol-enhanced medical devices, particularly for long-term implants or frequently used external devices.
Environmental safety is another aspect that cannot be overlooked. The disposal of phenol-containing medical devices must be carefully managed to prevent environmental contamination. Phenol is known to be toxic to aquatic life and can persist in the environment, potentially entering the food chain. Proper disposal protocols and end-of-life management strategies for these devices must be developed and implemented to mitigate environmental risks.
To address these safety and toxicity concerns, comprehensive risk assessment and management strategies are essential. This includes extensive in vitro and in vivo testing to evaluate both short-term and long-term effects of phenol exposure from medical devices. Advanced analytical techniques should be employed to accurately measure phenol release rates and degradation products. Additionally, the development of safer alternatives or modified forms of phenol with reduced toxicity should be a priority in research efforts aimed at improving biocompatibility in medical devices.
The primary safety concern with carbolic acid is its potential for local tissue damage. Even at low concentrations, phenol can cause irritation, inflammation, and necrosis of tissues it comes into contact with. This is particularly problematic for implantable devices or those in prolonged contact with bodily tissues. The risk of tissue damage must be weighed against any potential biocompatibility benefits, and strategies to mitigate this risk, such as controlled release mechanisms or protective coatings, should be explored.
Systemic toxicity is another critical consideration. If phenol leaches from medical devices into the bloodstream, it can lead to serious health complications. Acute exposure to high levels of phenol can result in central nervous system depression, cardiovascular collapse, and even death. Chronic exposure, even at lower levels, has been associated with liver and kidney damage, as well as potential carcinogenic effects. Therefore, rigorous testing must be conducted to ensure that phenol-containing medical devices do not release harmful amounts of the substance over their intended lifespan.
The potential for allergic reactions and sensitization is also a significant concern. Some individuals may develop hypersensitivity to phenol, leading to allergic contact dermatitis or more severe systemic allergic responses. This risk necessitates careful patient screening and monitoring when using phenol-enhanced medical devices, particularly for long-term implants or frequently used external devices.
Environmental safety is another aspect that cannot be overlooked. The disposal of phenol-containing medical devices must be carefully managed to prevent environmental contamination. Phenol is known to be toxic to aquatic life and can persist in the environment, potentially entering the food chain. Proper disposal protocols and end-of-life management strategies for these devices must be developed and implemented to mitigate environmental risks.
To address these safety and toxicity concerns, comprehensive risk assessment and management strategies are essential. This includes extensive in vitro and in vivo testing to evaluate both short-term and long-term effects of phenol exposure from medical devices. Advanced analytical techniques should be employed to accurately measure phenol release rates and degradation products. Additionally, the development of safer alternatives or modified forms of phenol with reduced toxicity should be a priority in research efforts aimed at improving biocompatibility in medical devices.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!