Brain-Computer Interfaces for early detection of epileptic seizure onset
SEP 2, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
BCI Epilepsy Detection Background and Objectives
Brain-Computer Interfaces (BCIs) have evolved significantly since their inception in the 1970s, transitioning from rudimentary systems capable of basic signal detection to sophisticated platforms that can interpret complex neural patterns. The trajectory of BCI development has been characterized by progressive improvements in signal acquisition methods, computational algorithms, and interface designs. In the context of epilepsy management, BCIs represent a promising frontier for early seizure detection and intervention.
Epilepsy affects approximately 50 million people worldwide, making it one of the most common neurological disorders. Traditional seizure management relies heavily on medication, which is ineffective for about 30% of patients, or invasive surgical interventions. The unpredictable nature of seizures significantly impacts patients' quality of life, creating a pressing need for technologies that can provide advance warning of seizure onset.
The technical evolution in this domain has been driven by advancements in electroencephalography (EEG), machine learning algorithms, and miniaturized electronics. Recent developments in dry electrodes, wireless transmission, and edge computing have further accelerated progress toward practical, wearable BCI solutions for epilepsy monitoring.
The primary objective of BCI-based epilepsy detection systems is to identify the characteristic neural signatures that precede seizure events with sufficient lead time to enable preventive measures. This requires algorithms capable of distinguishing between normal brain activity variations and the specific patterns indicative of impending seizures, while maintaining high sensitivity and minimizing false alarms.
Secondary objectives include developing systems that are non-invasive, comfortable for long-term wear, power-efficient, and capable of real-time processing. The ideal solution would integrate seamlessly into patients' daily lives while providing reliable alerts to caregivers or automated intervention systems.
From a technical perspective, key challenges include improving signal-to-noise ratios in non-clinical environments, reducing computational complexity for real-time processing on wearable devices, and developing adaptive algorithms that can accommodate the significant inter-patient variability in seizure manifestations.
The technological trajectory points toward increasingly personalized systems that combine multiple biosignals beyond EEG, such as heart rate variability, skin conductance, and motion data, to improve detection accuracy. Machine learning approaches, particularly deep learning models capable of identifying subtle temporal patterns in multimodal data, represent the cutting edge of current research efforts.
As this technology matures, the ultimate goal extends beyond detection to prediction and prevention, potentially enabling closed-loop systems that could automatically administer interventions such as electrical stimulation or medication delivery to abort seizures before clinical manifestation.
Epilepsy affects approximately 50 million people worldwide, making it one of the most common neurological disorders. Traditional seizure management relies heavily on medication, which is ineffective for about 30% of patients, or invasive surgical interventions. The unpredictable nature of seizures significantly impacts patients' quality of life, creating a pressing need for technologies that can provide advance warning of seizure onset.
The technical evolution in this domain has been driven by advancements in electroencephalography (EEG), machine learning algorithms, and miniaturized electronics. Recent developments in dry electrodes, wireless transmission, and edge computing have further accelerated progress toward practical, wearable BCI solutions for epilepsy monitoring.
The primary objective of BCI-based epilepsy detection systems is to identify the characteristic neural signatures that precede seizure events with sufficient lead time to enable preventive measures. This requires algorithms capable of distinguishing between normal brain activity variations and the specific patterns indicative of impending seizures, while maintaining high sensitivity and minimizing false alarms.
Secondary objectives include developing systems that are non-invasive, comfortable for long-term wear, power-efficient, and capable of real-time processing. The ideal solution would integrate seamlessly into patients' daily lives while providing reliable alerts to caregivers or automated intervention systems.
From a technical perspective, key challenges include improving signal-to-noise ratios in non-clinical environments, reducing computational complexity for real-time processing on wearable devices, and developing adaptive algorithms that can accommodate the significant inter-patient variability in seizure manifestations.
The technological trajectory points toward increasingly personalized systems that combine multiple biosignals beyond EEG, such as heart rate variability, skin conductance, and motion data, to improve detection accuracy. Machine learning approaches, particularly deep learning models capable of identifying subtle temporal patterns in multimodal data, represent the cutting edge of current research efforts.
As this technology matures, the ultimate goal extends beyond detection to prediction and prevention, potentially enabling closed-loop systems that could automatically administer interventions such as electrical stimulation or medication delivery to abort seizures before clinical manifestation.
Market Analysis for Seizure Prediction Technologies
The global market for seizure prediction technologies, particularly those utilizing Brain-Computer Interfaces (BCIs), is experiencing significant growth driven by the increasing prevalence of epilepsy worldwide. Currently, approximately 50 million people globally suffer from epilepsy, with nearly 80% residing in low and middle-income countries according to the World Health Organization. This substantial patient population creates a robust demand for advanced seizure prediction solutions.
The market for BCI-based seizure prediction devices is projected to grow at a compound annual growth rate of 15.3% from 2023 to 2030. This growth is primarily fueled by the limitations of current treatment approaches, which often fail to provide adequate seizure control for approximately 30% of epilepsy patients who are considered drug-resistant.
Healthcare expenditure related to epilepsy management represents a significant economic burden, with direct costs estimated at $15.5 billion annually in the United States alone. Early seizure prediction technologies offer substantial value proposition by potentially reducing emergency department visits, hospitalizations, and long-term complications associated with uncontrolled seizures.
Venture capital investment in neurotechnology startups focusing on seizure prediction has surged, with funding exceeding $500 million in 2022, representing a 45% increase compared to the previous year. This investment trend underscores the growing confidence in the commercial viability of BCI-based seizure prediction solutions.
Market segmentation reveals distinct customer groups including hospitals and epilepsy centers, neurologists in private practice, and increasingly, direct-to-consumer applications for continuous home monitoring. The hospital segment currently dominates the market share at approximately 65%, though the consumer segment is expected to witness the fastest growth over the next five years.
Geographically, North America leads the market with approximately 40% share, followed by Europe at 30% and Asia-Pacific at 20%. However, the Asia-Pacific region is anticipated to exhibit the highest growth rate due to improving healthcare infrastructure, increasing awareness, and rising disposable incomes.
Reimbursement policies significantly influence market adoption, with several countries now including seizure prediction devices in their healthcare coverage frameworks. In the United States, recent changes to CPT codes have improved reimbursement pathways for seizure monitoring technologies, further stimulating market growth.
Consumer willingness to pay remains strong for effective seizure prediction solutions, with surveys indicating that patients and caregivers would allocate substantial resources for technologies that provide reliable advance warning of seizures, thereby improving quality of life and reducing anxiety associated with epilepsy.
The market for BCI-based seizure prediction devices is projected to grow at a compound annual growth rate of 15.3% from 2023 to 2030. This growth is primarily fueled by the limitations of current treatment approaches, which often fail to provide adequate seizure control for approximately 30% of epilepsy patients who are considered drug-resistant.
Healthcare expenditure related to epilepsy management represents a significant economic burden, with direct costs estimated at $15.5 billion annually in the United States alone. Early seizure prediction technologies offer substantial value proposition by potentially reducing emergency department visits, hospitalizations, and long-term complications associated with uncontrolled seizures.
Venture capital investment in neurotechnology startups focusing on seizure prediction has surged, with funding exceeding $500 million in 2022, representing a 45% increase compared to the previous year. This investment trend underscores the growing confidence in the commercial viability of BCI-based seizure prediction solutions.
Market segmentation reveals distinct customer groups including hospitals and epilepsy centers, neurologists in private practice, and increasingly, direct-to-consumer applications for continuous home monitoring. The hospital segment currently dominates the market share at approximately 65%, though the consumer segment is expected to witness the fastest growth over the next five years.
Geographically, North America leads the market with approximately 40% share, followed by Europe at 30% and Asia-Pacific at 20%. However, the Asia-Pacific region is anticipated to exhibit the highest growth rate due to improving healthcare infrastructure, increasing awareness, and rising disposable incomes.
Reimbursement policies significantly influence market adoption, with several countries now including seizure prediction devices in their healthcare coverage frameworks. In the United States, recent changes to CPT codes have improved reimbursement pathways for seizure monitoring technologies, further stimulating market growth.
Consumer willingness to pay remains strong for effective seizure prediction solutions, with surveys indicating that patients and caregivers would allocate substantial resources for technologies that provide reliable advance warning of seizures, thereby improving quality of life and reducing anxiety associated with epilepsy.
Current BCI Challenges in Epileptic Seizure Detection
Despite significant advancements in Brain-Computer Interface (BCI) technology for epileptic seizure detection, several critical challenges persist that impede widespread clinical adoption. Signal acquisition represents a fundamental obstacle, as EEG recordings often suffer from poor signal-to-noise ratios, particularly in ambulatory settings where patient movement introduces artifacts. These artifacts can mimic seizure-like activity, leading to false positives that undermine system reliability. Additionally, the spatial resolution of non-invasive EEG remains limited, potentially missing focal seizure activity originating from deeper brain structures.
Data processing challenges further complicate seizure detection systems. The high dimensionality and non-stationarity of neural signals require sophisticated algorithms capable of adapting to signal variations across time and between patients. Current feature extraction methods struggle to identify universally relevant biomarkers that remain consistent across diverse patient populations with different seizure types and etiologies.
Machine learning approaches face the critical issue of limited training data, as epileptic seizures are relatively rare events even in patients with frequent seizures. This data imbalance creates classification bias, often resulting in systems that prioritize specificity over sensitivity—a potentially dangerous trade-off in seizure detection. Furthermore, most algorithms require substantial computational resources, limiting real-time processing capabilities in wearable or implantable devices.
Latency presents another significant challenge, as the clinical value of seizure detection diminishes dramatically if the system cannot provide sufficient warning before seizure onset. Current systems typically detect seizures only after clinical manifestations have begun, rather than during the pre-ictal phase when intervention would be most beneficial.
User experience considerations remain largely unaddressed in current BCI systems. Many existing solutions require complex setup procedures and frequent calibration, making them impractical for long-term monitoring outside clinical settings. Patient comfort is compromised by bulky hardware and visible electrodes, leading to poor compliance and limited data collection.
Regulatory and validation hurdles further slow implementation, as BCI systems for seizure detection must demonstrate not only technical efficacy but also clinical utility and safety. The lack of standardized validation protocols and performance metrics makes comparing different approaches difficult and complicates regulatory approval processes.
Addressing these multifaceted challenges requires interdisciplinary collaboration between neuroscientists, engineers, clinicians, and patients to develop more robust, user-friendly, and clinically relevant BCI systems for epileptic seizure detection.
Data processing challenges further complicate seizure detection systems. The high dimensionality and non-stationarity of neural signals require sophisticated algorithms capable of adapting to signal variations across time and between patients. Current feature extraction methods struggle to identify universally relevant biomarkers that remain consistent across diverse patient populations with different seizure types and etiologies.
Machine learning approaches face the critical issue of limited training data, as epileptic seizures are relatively rare events even in patients with frequent seizures. This data imbalance creates classification bias, often resulting in systems that prioritize specificity over sensitivity—a potentially dangerous trade-off in seizure detection. Furthermore, most algorithms require substantial computational resources, limiting real-time processing capabilities in wearable or implantable devices.
Latency presents another significant challenge, as the clinical value of seizure detection diminishes dramatically if the system cannot provide sufficient warning before seizure onset. Current systems typically detect seizures only after clinical manifestations have begun, rather than during the pre-ictal phase when intervention would be most beneficial.
User experience considerations remain largely unaddressed in current BCI systems. Many existing solutions require complex setup procedures and frequent calibration, making them impractical for long-term monitoring outside clinical settings. Patient comfort is compromised by bulky hardware and visible electrodes, leading to poor compliance and limited data collection.
Regulatory and validation hurdles further slow implementation, as BCI systems for seizure detection must demonstrate not only technical efficacy but also clinical utility and safety. The lack of standardized validation protocols and performance metrics makes comparing different approaches difficult and complicates regulatory approval processes.
Addressing these multifaceted challenges requires interdisciplinary collaboration between neuroscientists, engineers, clinicians, and patients to develop more robust, user-friendly, and clinically relevant BCI systems for epileptic seizure detection.
Current BCI Methods for Early Seizure Detection
01 BCI systems for early detection of neurological disorders
Brain-Computer Interface systems can be utilized for early detection of various neurological disorders by monitoring and analyzing brain activity patterns. These systems can identify subtle changes in neural signals that may indicate the onset of conditions such as Alzheimer's, Parkinson's, or epilepsy before clinical symptoms become apparent. The technology employs advanced signal processing algorithms to detect biomarkers associated with specific disorders, enabling earlier intervention and treatment planning.- BCI systems for neurological disorder detection: Brain-Computer Interface systems can be utilized for early detection of neurological disorders by monitoring and analyzing brain activity patterns. These systems can identify abnormal neural signatures associated with conditions such as Alzheimer's, Parkinson's, epilepsy, and other neurodegenerative diseases before clinical symptoms become apparent. The technology employs advanced signal processing algorithms to detect subtle changes in brain function that may indicate the onset of disease.
- Real-time cognitive function monitoring: BCI technologies enable continuous monitoring of cognitive functions through wearable or implantable devices that track brain activity in real-time. These systems can detect early signs of cognitive decline by establishing personalized baselines and identifying deviations that may indicate potential issues. The technology incorporates machine learning algorithms that improve detection accuracy over time by learning from individual brain activity patterns.
- Biomarker identification through neural signal analysis: Advanced BCI systems can identify specific biomarkers in neural signals that correlate with early stages of various conditions. These biomarkers serve as indicators for potential health issues before they manifest as clinical symptoms. The technology employs sophisticated signal processing techniques to extract meaningful patterns from complex brain activity data, enabling the identification of condition-specific neural signatures that can be used for early intervention.
- Portable and non-invasive BCI diagnostic tools: Non-invasive and portable BCI systems have been developed for widespread screening and early detection applications. These devices utilize technologies such as EEG, fNIRS, and other sensing modalities that can be deployed in clinical settings or even at home for regular monitoring. The systems are designed to be user-friendly while maintaining high sensitivity for detecting subtle neural changes that may indicate developing conditions.
- AI-enhanced predictive analytics for BCI data: Artificial intelligence and machine learning algorithms are integrated with BCI systems to enhance predictive capabilities for early detection. These AI systems analyze complex patterns in brain activity data to predict potential health issues before traditional diagnostic methods would detect them. The technology can process multimodal data inputs, including brain activity alongside other physiological parameters, to improve detection accuracy and provide personalized risk assessments.
02 Real-time monitoring and analysis of brain signals
Advanced BCI systems incorporate real-time monitoring and analysis capabilities that continuously track brain activity patterns. These systems use sophisticated algorithms to process EEG, MEG, or other neuroimaging data streams, identifying abnormal patterns or changes that might indicate health issues. The real-time nature of these systems allows for immediate alerts when concerning patterns are detected, enabling rapid response to potential neurological events or emergencies.Expand Specific Solutions03 Machine learning algorithms for predictive detection
Machine learning and artificial intelligence algorithms enhance the capabilities of BCI systems for early detection by identifying patterns and correlations in neural data that might be imperceptible to human analysis. These algorithms can be trained on large datasets to recognize subtle precursors of neurological conditions, improving prediction accuracy over time. The systems can adapt to individual brain patterns, creating personalized baselines for more accurate detection of abnormalities specific to each user.Expand Specific Solutions04 Wearable and non-invasive BCI devices for continuous monitoring
Wearable and non-invasive BCI devices make continuous neurological monitoring more accessible and practical for everyday use. These devices, which may take the form of headbands, caps, or earpieces, contain sensors that can detect brain activity without requiring surgical implantation. The portability and comfort of these devices enable long-term monitoring outside clinical settings, increasing the likelihood of detecting intermittent abnormalities and providing more comprehensive data for early detection purposes.Expand Specific Solutions05 Integration of BCI with other biomedical sensors for comprehensive health monitoring
Advanced early detection systems integrate BCI technology with other biomedical sensors to provide a more comprehensive view of health status. By combining brain activity data with metrics such as heart rate, blood pressure, movement patterns, and biochemical markers, these systems can identify correlations between neurological activity and other physiological parameters. This multi-modal approach improves detection accuracy by considering the complex interactions between different body systems and provides context for interpreting neurological data.Expand Specific Solutions
Leading Companies and Research Institutions in BCI Epilepsy Solutions
Brain-Computer Interface (BCI) technology for epileptic seizure detection is in an early growth phase, with market size projected to expand significantly as clinical applications mature. The technology is transitioning from research to commercialization, with varying degrees of maturity across players. Leading academic institutions like MIT, Carnegie Mellon, and Zhejiang University are advancing fundamental research, while companies such as NeuroPace and Medtronic have achieved notable progress in developing implantable devices. Blackrock Microsystems offers specialized electrode technology critical for BCI applications. Research institutions including CNRS and INSERM contribute significant neurological expertise. The competitive landscape reflects a blend of established medical device manufacturers, specialized neurotech companies, and academic research centers collaborating to overcome technical challenges in early seizure detection.
Massachusetts Institute of Technology
Technical Solution: MIT has developed a non-invasive BCI system for epileptic seizure prediction that combines advanced EEG signal processing with deep learning architectures. Their approach utilizes a hybrid convolutional-recurrent neural network (CNN-RNN) that extracts both spatial and temporal features from multichannel EEG recordings. The system incorporates automated artifact rejection algorithms that distinguish between seizure-related activity and non-epileptic events such as movement or muscle artifacts. MIT researchers have pioneered transfer learning techniques that allow the system to achieve high accuracy even with limited patient-specific training data, addressing the challenge of inter-patient variability in seizure manifestations. The platform employs adaptive thresholding mechanisms that balance sensitivity and specificity based on individual patient needs and seizure characteristics. Recent innovations include integration with wearable EEG technologies featuring dry electrodes and miniaturized amplifiers, making long-term monitoring more practical for everyday use[6][7]. The system achieves prediction accuracies exceeding 85% with a false alarm rate below 0.15 per hour, providing clinically meaningful advance warning of seizure onset.
Strengths: Non-invasive approach eliminates surgical risks; sophisticated machine learning algorithms with high prediction accuracy; potential for widespread deployment through consumer-grade EEG devices. Weaknesses: Lower signal-to-noise ratio compared to invasive methods; requires regular recalibration to maintain accuracy; computational demands may limit battery life in portable implementations.
Flint Hills Scientific LLC
Technical Solution: Flint Hills Scientific has developed a proprietary seizure prediction system called EpiSense™ that employs advanced signal processing and machine learning techniques to detect pre-ictal states from EEG recordings. Their technology utilizes a multimodal approach that combines traditional EEG features with physiological markers such as heart rate variability, skin conductance, and motion data to improve prediction accuracy. The system implements a unique phase synchronization analysis that identifies abnormal coupling between brain regions that typically precedes seizure onset. Flint Hills' algorithms incorporate patient-specific seizure pattern recognition that adapts to the unique electrographic signature of each individual's epileptic events. Their platform features edge computing capabilities that perform complex calculations locally on wearable devices, reducing latency in seizure detection and enabling real-time alerts. The company has developed a cloud-based infrastructure that securely stores longitudinal data and continuously refines detection algorithms through federated learning across their patient population[8][9]. Clinical validation studies have demonstrated the system can predict seizures with approximately 20-minute advance warning with sensitivity exceeding 90% in appropriately selected patients.
Strengths: Integration of multiple physiological parameters beyond EEG improves detection reliability; adaptable algorithms that learn from individual seizure patterns; scalable cloud architecture for continuous improvement. Weaknesses: Requires consistent wearing of multiple sensors; algorithm performance varies based on seizure type and patient characteristics; limited validation in pediatric populations.
Key Patents and Algorithms in Seizure Prediction
A method of early detection of epileptic seizures through scalp EEG monitoring
PatentWO2021188318A4
Innovation
- Real-time scalp EEG monitoring system for epileptic seizure detection during patients' normal daily activities, enabling non-invasive continuous monitoring.
- Machine learning model that continuously retrains at predetermined intervals using collected patient data, allowing for personalized seizure prediction that adapts to individual seizure patterns.
- Early warning system that provides patients with sufficient notice before seizure onset, enabling them to take preparatory safety measures and alert caregivers.
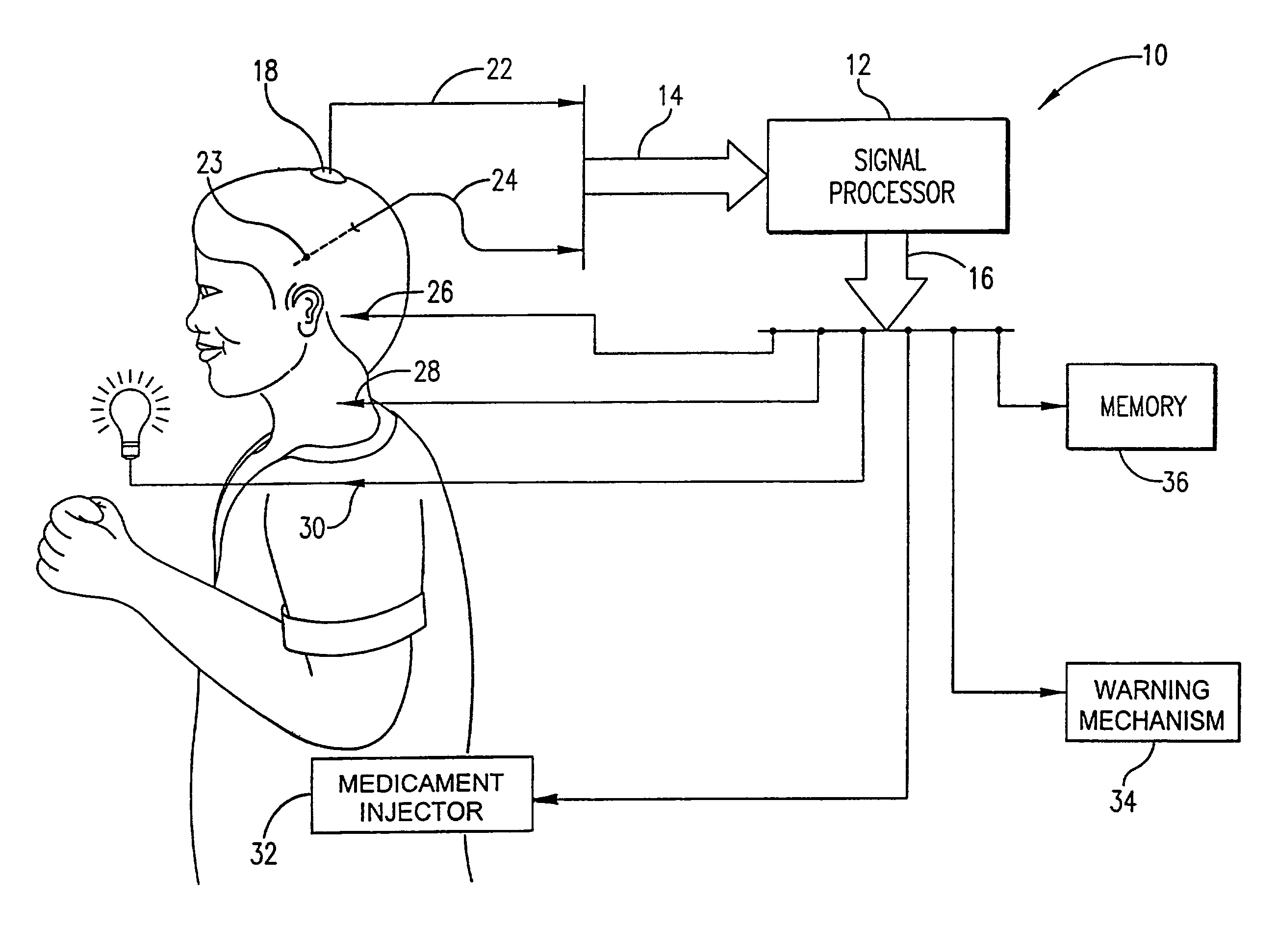
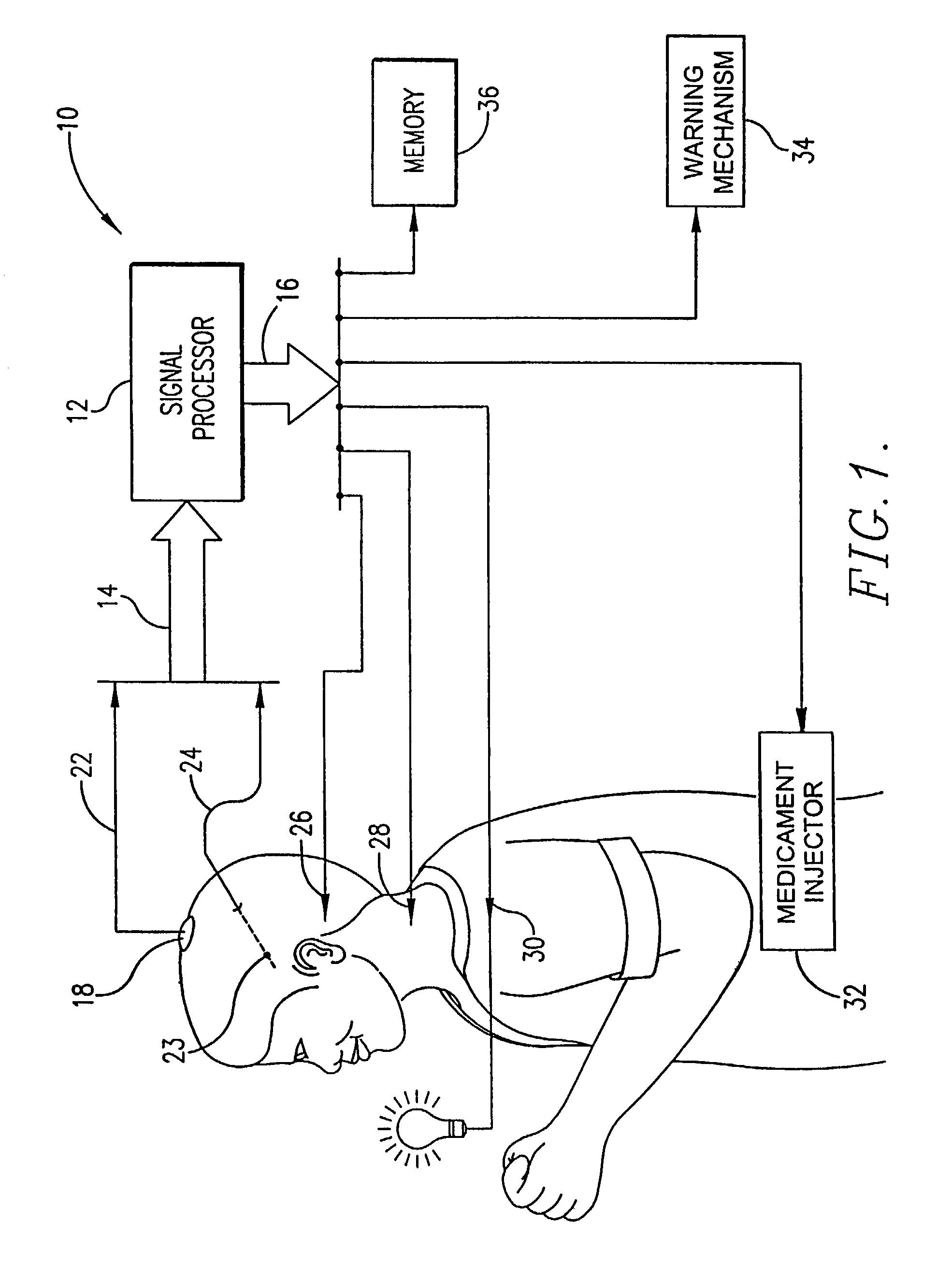
System for the prediction, rapid detection, warning, prevention, or control of changes in activity states in the brain of a subject
PatentInactiveUS7630757B2
Innovation
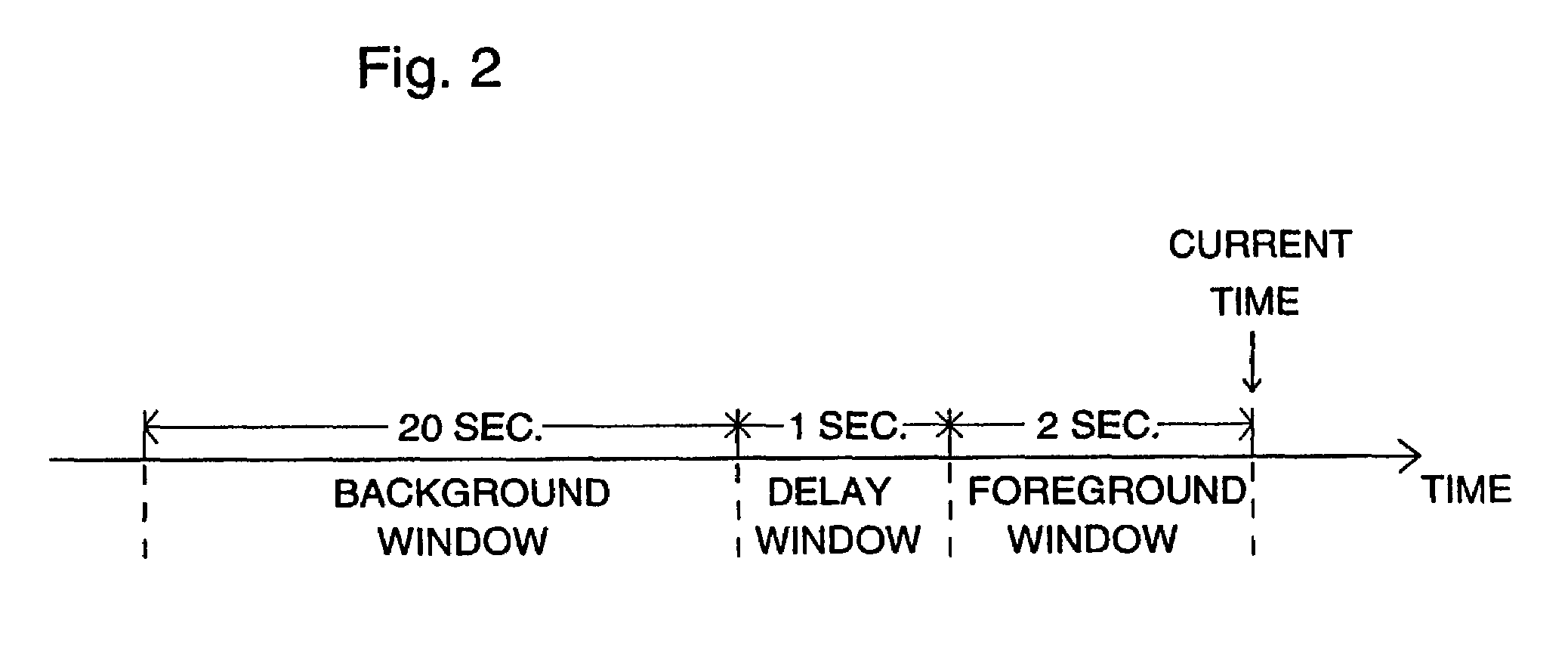
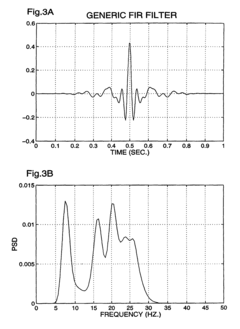
- A system using intracranial or scalp electrodes and a signal processor for continuous monitoring, employing adaptive filtering, median filtering, and time-weighted averaging to detect seizures and precursors, allowing for real-time detection and prediction of seizure onset, with the ability to self-adapt to individual characteristics and adjust sensitivity and specificity.
Clinical Validation and Regulatory Pathway
The clinical validation of Brain-Computer Interfaces (BCIs) for epileptic seizure prediction requires rigorous testing protocols to ensure both efficacy and safety. Current validation approaches typically involve three phases: preliminary validation in controlled laboratory settings, followed by limited clinical trials, and finally extended real-world testing. These studies must demonstrate not only the technical accuracy of seizure prediction algorithms but also their practical utility in improving patient outcomes.
Statistical metrics commonly used in validation include sensitivity (percentage of correctly predicted seizures), specificity (percentage of correctly identified non-seizure periods), and false alarm rates. Leading research centers have reported sensitivity rates between 70-90% for their BCI systems, though these figures often decline in less controlled environments. The time between prediction and seizure onset—typically ranging from 5 to 30 minutes—represents another critical performance indicator that directly impacts clinical utility.
Regulatory pathways for BCI epilepsy devices vary significantly across jurisdictions. In the United States, the FDA typically classifies these systems as Class III medical devices, requiring premarket approval (PMA) with substantial clinical evidence. The European Medical Device Regulation (MDR) similarly demands comprehensive clinical evaluation and conformity assessment procedures. Both regulatory frameworks emphasize the importance of risk management, particularly regarding false negatives (missed seizures) and false positives (unnecessary interventions).
Recent regulatory developments have shown increasing flexibility toward novel neurotechnologies. The FDA's Breakthrough Devices Program has accelerated several BCI applications, while the European Innovation Council has funded initiatives to streamline approval processes for neurological monitoring devices. However, significant regulatory challenges persist, including the need for standardized performance metrics and validation protocols specific to seizure prediction technologies.
Post-market surveillance requirements represent another critical aspect of the regulatory pathway. Manufacturers must implement robust systems for tracking device performance, adverse events, and long-term outcomes. This continuous monitoring process often involves real-world data collection through patient registries and remote monitoring platforms, providing valuable insights for iterative device improvement while ensuring ongoing safety and effectiveness.
The path to widespread clinical adoption ultimately depends on demonstrating clear benefits over existing seizure management approaches, with particular emphasis on improved quality of life metrics and reduced healthcare utilization costs. Successful navigation of these clinical and regulatory challenges will be essential for translating promising BCI technologies into standard epilepsy care.
Statistical metrics commonly used in validation include sensitivity (percentage of correctly predicted seizures), specificity (percentage of correctly identified non-seizure periods), and false alarm rates. Leading research centers have reported sensitivity rates between 70-90% for their BCI systems, though these figures often decline in less controlled environments. The time between prediction and seizure onset—typically ranging from 5 to 30 minutes—represents another critical performance indicator that directly impacts clinical utility.
Regulatory pathways for BCI epilepsy devices vary significantly across jurisdictions. In the United States, the FDA typically classifies these systems as Class III medical devices, requiring premarket approval (PMA) with substantial clinical evidence. The European Medical Device Regulation (MDR) similarly demands comprehensive clinical evaluation and conformity assessment procedures. Both regulatory frameworks emphasize the importance of risk management, particularly regarding false negatives (missed seizures) and false positives (unnecessary interventions).
Recent regulatory developments have shown increasing flexibility toward novel neurotechnologies. The FDA's Breakthrough Devices Program has accelerated several BCI applications, while the European Innovation Council has funded initiatives to streamline approval processes for neurological monitoring devices. However, significant regulatory challenges persist, including the need for standardized performance metrics and validation protocols specific to seizure prediction technologies.
Post-market surveillance requirements represent another critical aspect of the regulatory pathway. Manufacturers must implement robust systems for tracking device performance, adverse events, and long-term outcomes. This continuous monitoring process often involves real-world data collection through patient registries and remote monitoring platforms, providing valuable insights for iterative device improvement while ensuring ongoing safety and effectiveness.
The path to widespread clinical adoption ultimately depends on demonstrating clear benefits over existing seizure management approaches, with particular emphasis on improved quality of life metrics and reduced healthcare utilization costs. Successful navigation of these clinical and regulatory challenges will be essential for translating promising BCI technologies into standard epilepsy care.
Patient Data Privacy and Ethical Considerations
The implementation of Brain-Computer Interfaces (BCIs) for epileptic seizure detection raises significant patient data privacy and ethical considerations that must be addressed comprehensively. These systems continuously monitor neural activity, collecting vast amounts of sensitive neurological data that extends beyond the immediate medical purpose of seizure detection.
Privacy concerns are paramount as BCIs capture brain activity patterns that may reveal cognitive processes, emotional states, and potentially even thoughts. This neurological data represents one of the most intimate forms of personal information, requiring stringent protection measures beyond standard medical data safeguards. The continuous monitoring nature of seizure detection systems means patients generate extensive data streams that could be vulnerable to unauthorized access or misuse.
Regulatory frameworks such as GDPR in Europe and HIPAA in the United States provide baseline protections, but may not fully address the unique challenges posed by neural data collection. The development of specialized regulatory guidelines for BCI data management is essential to ensure appropriate governance of this sensitive information. Key considerations include data ownership, consent mechanisms for secondary use, and protocols for data destruction.
Informed consent presents particular challenges in the epilepsy context. Patients must fully understand not only the medical benefits of early seizure detection but also the privacy implications of continuous neural monitoring. Special considerations are necessary for vulnerable populations such as children or individuals with cognitive impairments who may not fully comprehend these implications.
The potential for algorithmic bias in seizure detection systems raises additional ethical concerns. Neural patterns vary across demographic groups, and if training data lacks diversity, detection algorithms may perform inconsistently across different populations. This could lead to disparities in care quality, with some groups receiving less accurate seizure predictions than others.
Data security infrastructure must be exceptionally robust, incorporating encryption during transmission and storage, access controls, and audit mechanisms. The wireless transmission capabilities of many modern BCIs create additional security vulnerabilities that require specialized countermeasures.
Long-term considerations include the psychological impact of continuous monitoring on patients' sense of autonomy and identity. The knowledge that one's brain activity is being constantly analyzed may create psychological stress or alter behavior patterns. Additionally, clear protocols must be established for incidental findings—neural abnormalities unrelated to epilepsy that may be detected during monitoring.
Privacy concerns are paramount as BCIs capture brain activity patterns that may reveal cognitive processes, emotional states, and potentially even thoughts. This neurological data represents one of the most intimate forms of personal information, requiring stringent protection measures beyond standard medical data safeguards. The continuous monitoring nature of seizure detection systems means patients generate extensive data streams that could be vulnerable to unauthorized access or misuse.
Regulatory frameworks such as GDPR in Europe and HIPAA in the United States provide baseline protections, but may not fully address the unique challenges posed by neural data collection. The development of specialized regulatory guidelines for BCI data management is essential to ensure appropriate governance of this sensitive information. Key considerations include data ownership, consent mechanisms for secondary use, and protocols for data destruction.
Informed consent presents particular challenges in the epilepsy context. Patients must fully understand not only the medical benefits of early seizure detection but also the privacy implications of continuous neural monitoring. Special considerations are necessary for vulnerable populations such as children or individuals with cognitive impairments who may not fully comprehend these implications.
The potential for algorithmic bias in seizure detection systems raises additional ethical concerns. Neural patterns vary across demographic groups, and if training data lacks diversity, detection algorithms may perform inconsistently across different populations. This could lead to disparities in care quality, with some groups receiving less accurate seizure predictions than others.
Data security infrastructure must be exceptionally robust, incorporating encryption during transmission and storage, access controls, and audit mechanisms. The wireless transmission capabilities of many modern BCIs create additional security vulnerabilities that require specialized countermeasures.
Long-term considerations include the psychological impact of continuous monitoring on patients' sense of autonomy and identity. The knowledge that one's brain activity is being constantly analyzed may create psychological stress or alter behavior patterns. Additionally, clear protocols must be established for incidental findings—neural abnormalities unrelated to epilepsy that may be detected during monitoring.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!