Exploring Medical Polypropylene’s Non-Invasive Surgery Applications
JUL 21, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Medical PP Evolution
Medical polypropylene (PP) has undergone significant evolution in its applications for non-invasive surgery. Initially developed in the 1950s, PP quickly gained attention in the medical field due to its unique properties, including high chemical resistance, low density, and excellent processability.
In the 1960s and 1970s, medical PP saw its first applications in surgical sutures and basic medical devices. The material's biocompatibility and resistance to degradation made it an attractive option for implantable devices. However, its use in non-invasive surgery was limited during this period.
The 1980s marked a turning point for medical PP in non-invasive applications. With advancements in polymer science and processing techniques, manufacturers began producing PP-based products specifically designed for minimally invasive procedures. This decade saw the introduction of PP-based laparoscopic instruments and endoscopic devices.
Throughout the 1990s, the use of medical PP in non-invasive surgery expanded rapidly. Improved sterilization techniques and the development of specialized PP grades enhanced the material's suitability for a wider range of surgical applications. During this time, PP became a common material for disposable surgical instruments and components used in endoscopic procedures.
The early 2000s brought about a new era of innovation in medical PP for non-invasive surgery. Nanotechnology and surface modification techniques allowed for the creation of PP-based materials with enhanced properties, such as improved biocompatibility and reduced friction. These advancements led to the development of more sophisticated endoscopic tools and minimally invasive surgical instruments.
In recent years, the focus has shifted towards developing medical PP composites and blends tailored for specific non-invasive surgical applications. These materials offer improved mechanical properties, enhanced visualization under imaging techniques, and better integration with other surgical technologies.
The latest trend in medical PP evolution for non-invasive surgery involves the incorporation of smart materials and functionalities. Researchers are exploring PP-based materials that can change properties in response to external stimuli, potentially enabling more precise and adaptable surgical tools. Additionally, efforts are being made to develop PP-based materials with antimicrobial properties to reduce the risk of surgical site infections in minimally invasive procedures.
As we look to the future, the evolution of medical PP in non-invasive surgery is likely to continue, driven by advancements in material science, surgical techniques, and emerging technologies such as robotics and artificial intelligence. The ongoing research in this field promises to deliver even more innovative and effective solutions for minimally invasive surgical procedures.
In the 1960s and 1970s, medical PP saw its first applications in surgical sutures and basic medical devices. The material's biocompatibility and resistance to degradation made it an attractive option for implantable devices. However, its use in non-invasive surgery was limited during this period.
The 1980s marked a turning point for medical PP in non-invasive applications. With advancements in polymer science and processing techniques, manufacturers began producing PP-based products specifically designed for minimally invasive procedures. This decade saw the introduction of PP-based laparoscopic instruments and endoscopic devices.
Throughout the 1990s, the use of medical PP in non-invasive surgery expanded rapidly. Improved sterilization techniques and the development of specialized PP grades enhanced the material's suitability for a wider range of surgical applications. During this time, PP became a common material for disposable surgical instruments and components used in endoscopic procedures.
The early 2000s brought about a new era of innovation in medical PP for non-invasive surgery. Nanotechnology and surface modification techniques allowed for the creation of PP-based materials with enhanced properties, such as improved biocompatibility and reduced friction. These advancements led to the development of more sophisticated endoscopic tools and minimally invasive surgical instruments.
In recent years, the focus has shifted towards developing medical PP composites and blends tailored for specific non-invasive surgical applications. These materials offer improved mechanical properties, enhanced visualization under imaging techniques, and better integration with other surgical technologies.
The latest trend in medical PP evolution for non-invasive surgery involves the incorporation of smart materials and functionalities. Researchers are exploring PP-based materials that can change properties in response to external stimuli, potentially enabling more precise and adaptable surgical tools. Additionally, efforts are being made to develop PP-based materials with antimicrobial properties to reduce the risk of surgical site infections in minimally invasive procedures.
As we look to the future, the evolution of medical PP in non-invasive surgery is likely to continue, driven by advancements in material science, surgical techniques, and emerging technologies such as robotics and artificial intelligence. The ongoing research in this field promises to deliver even more innovative and effective solutions for minimally invasive surgical procedures.
Non-Invasive Surgery Demand
The demand for non-invasive surgery has been steadily increasing in recent years, driven by several factors that highlight the advantages of these procedures over traditional open surgeries. Patients are increasingly seeking less invasive treatment options that offer reduced pain, shorter recovery times, and minimal scarring. This trend is particularly evident in developed countries with aging populations, where there is a growing need for surgical interventions that pose lower risks for elderly patients.
Medical polypropylene, with its unique properties, is well-positioned to meet the rising demand for non-invasive surgical applications. The material's biocompatibility, durability, and versatility make it an ideal candidate for developing innovative medical devices and instruments used in minimally invasive procedures. As healthcare providers strive to improve patient outcomes and reduce healthcare costs, the adoption of non-invasive techniques utilizing medical polypropylene is expected to accelerate.
Market research indicates that the global non-invasive surgery market is experiencing robust growth. Key drivers include technological advancements in imaging and surgical techniques, increasing prevalence of chronic diseases, and a growing emphasis on patient-centered care. The demand for non-invasive procedures spans various medical specialties, including cardiology, orthopedics, gastroenterology, and neurology.
In the field of cardiology, there is a significant demand for non-invasive interventions such as transcatheter aortic valve replacement (TAVR) and minimally invasive coronary artery bypass grafting (CABG). These procedures often involve the use of medical polypropylene components in catheters, guidewires, and other surgical instruments. The orthopedic sector is witnessing a surge in demand for arthroscopic procedures, where medical polypropylene-based devices play a crucial role in joint repair and reconstruction.
Gastroenterology is another area experiencing rapid growth in non-invasive techniques, with endoscopic procedures becoming increasingly sophisticated. Medical polypropylene is utilized in the production of endoscopes and related accessories, contributing to improved diagnostic and therapeutic capabilities. In neurosurgery, the demand for minimally invasive approaches to treat conditions such as brain tumors and vascular malformations is driving innovation in surgical tools and implants, many of which incorporate medical polypropylene.
The COVID-19 pandemic has further accelerated the shift towards non-invasive surgeries, as healthcare systems seek to minimize hospital stays and reduce the risk of infection transmission. This has led to increased investment in outpatient surgical centers and the development of advanced non-invasive techniques that can be performed in these settings.
As the demand for non-invasive surgery continues to grow, there is a parallel increase in the need for specialized medical polypropylene formulations tailored to specific surgical applications. This presents significant opportunities for material scientists and medical device manufacturers to collaborate in developing next-generation solutions that enhance the safety, efficacy, and outcomes of non-invasive procedures.
Medical polypropylene, with its unique properties, is well-positioned to meet the rising demand for non-invasive surgical applications. The material's biocompatibility, durability, and versatility make it an ideal candidate for developing innovative medical devices and instruments used in minimally invasive procedures. As healthcare providers strive to improve patient outcomes and reduce healthcare costs, the adoption of non-invasive techniques utilizing medical polypropylene is expected to accelerate.
Market research indicates that the global non-invasive surgery market is experiencing robust growth. Key drivers include technological advancements in imaging and surgical techniques, increasing prevalence of chronic diseases, and a growing emphasis on patient-centered care. The demand for non-invasive procedures spans various medical specialties, including cardiology, orthopedics, gastroenterology, and neurology.
In the field of cardiology, there is a significant demand for non-invasive interventions such as transcatheter aortic valve replacement (TAVR) and minimally invasive coronary artery bypass grafting (CABG). These procedures often involve the use of medical polypropylene components in catheters, guidewires, and other surgical instruments. The orthopedic sector is witnessing a surge in demand for arthroscopic procedures, where medical polypropylene-based devices play a crucial role in joint repair and reconstruction.
Gastroenterology is another area experiencing rapid growth in non-invasive techniques, with endoscopic procedures becoming increasingly sophisticated. Medical polypropylene is utilized in the production of endoscopes and related accessories, contributing to improved diagnostic and therapeutic capabilities. In neurosurgery, the demand for minimally invasive approaches to treat conditions such as brain tumors and vascular malformations is driving innovation in surgical tools and implants, many of which incorporate medical polypropylene.
The COVID-19 pandemic has further accelerated the shift towards non-invasive surgeries, as healthcare systems seek to minimize hospital stays and reduce the risk of infection transmission. This has led to increased investment in outpatient surgical centers and the development of advanced non-invasive techniques that can be performed in these settings.
As the demand for non-invasive surgery continues to grow, there is a parallel increase in the need for specialized medical polypropylene formulations tailored to specific surgical applications. This presents significant opportunities for material scientists and medical device manufacturers to collaborate in developing next-generation solutions that enhance the safety, efficacy, and outcomes of non-invasive procedures.
PP Tech Challenges
Polypropylene (PP) has gained significant attention in medical applications, particularly in non-invasive surgery. However, several technical challenges persist in fully realizing its potential. One of the primary obstacles is achieving optimal biocompatibility. While PP is generally considered biocompatible, long-term implantation can sometimes lead to inflammatory responses or tissue adhesion. Researchers are working on surface modifications and coatings to enhance its compatibility with human tissues and reduce adverse reactions.
Another challenge lies in the mechanical properties of PP. Although it offers good flexibility and strength, there's a need to fine-tune these properties for specific surgical applications. For instance, in hernia repair meshes, the material must be strong enough to provide support but flexible enough to conform to body contours. Balancing these requirements while maintaining the lightweight nature of PP remains a technical hurdle.
Sterilization presents another significant challenge. Traditional sterilization methods like ethylene oxide or gamma radiation can potentially degrade PP's properties. Developing sterilization techniques that effectively eliminate pathogens without compromising the material's integrity is crucial for its widespread adoption in surgical applications.
The long-term stability of PP in the human body is also a concern. While it is resistant to many chemicals, the complex biological environment can lead to gradual degradation over time. This degradation can result in the release of microparticles, potentially causing complications. Enhancing the material's long-term stability without sacrificing its beneficial properties is an ongoing research focus.
Additionally, there's a challenge in developing PP-based materials with controlled drug release capabilities. Incorporating pharmaceuticals into PP structures for localized, sustained drug delivery could significantly enhance its therapeutic potential. However, achieving controlled release profiles while maintaining the material's structural integrity poses technical difficulties.
Lastly, the processability of PP for specific medical applications presents challenges. While PP is generally easy to process, creating complex, precise structures required for certain surgical applications can be demanding. Developing advanced manufacturing techniques, such as 3D printing with medical-grade PP, to produce intricate, patient-specific devices is an area of active research and development.
Addressing these technical challenges is crucial for expanding the use of PP in non-invasive surgery. Ongoing research in material science, bioengineering, and manufacturing technologies is gradually overcoming these hurdles, paving the way for innovative PP-based solutions in medical applications.
Another challenge lies in the mechanical properties of PP. Although it offers good flexibility and strength, there's a need to fine-tune these properties for specific surgical applications. For instance, in hernia repair meshes, the material must be strong enough to provide support but flexible enough to conform to body contours. Balancing these requirements while maintaining the lightweight nature of PP remains a technical hurdle.
Sterilization presents another significant challenge. Traditional sterilization methods like ethylene oxide or gamma radiation can potentially degrade PP's properties. Developing sterilization techniques that effectively eliminate pathogens without compromising the material's integrity is crucial for its widespread adoption in surgical applications.
The long-term stability of PP in the human body is also a concern. While it is resistant to many chemicals, the complex biological environment can lead to gradual degradation over time. This degradation can result in the release of microparticles, potentially causing complications. Enhancing the material's long-term stability without sacrificing its beneficial properties is an ongoing research focus.
Additionally, there's a challenge in developing PP-based materials with controlled drug release capabilities. Incorporating pharmaceuticals into PP structures for localized, sustained drug delivery could significantly enhance its therapeutic potential. However, achieving controlled release profiles while maintaining the material's structural integrity poses technical difficulties.
Lastly, the processability of PP for specific medical applications presents challenges. While PP is generally easy to process, creating complex, precise structures required for certain surgical applications can be demanding. Developing advanced manufacturing techniques, such as 3D printing with medical-grade PP, to produce intricate, patient-specific devices is an area of active research and development.
Addressing these technical challenges is crucial for expanding the use of PP in non-invasive surgery. Ongoing research in material science, bioengineering, and manufacturing technologies is gradually overcoming these hurdles, paving the way for innovative PP-based solutions in medical applications.
Current PP Applications
01 Medical grade polypropylene compositions
Development of specialized polypropylene compositions for medical applications, focusing on improved properties such as biocompatibility, sterilization resistance, and enhanced mechanical characteristics. These compositions are tailored to meet the specific requirements of medical devices and equipment.- Medical polypropylene compositions: Development of specialized polypropylene compositions for medical applications, focusing on improved properties such as biocompatibility, sterilization resistance, and enhanced mechanical characteristics. These compositions may include additives or modifications to meet specific medical requirements.
- Polypropylene-based medical devices: Creation of medical devices using polypropylene materials, including surgical instruments, implants, and disposable medical equipment. These devices leverage the material's properties such as chemical resistance, durability, and ease of sterilization.
- Sterilization-resistant polypropylene: Development of polypropylene formulations that can withstand various sterilization methods commonly used in medical settings, such as gamma radiation, ethylene oxide, or autoclave sterilization, without significant degradation of material properties.
- Polypropylene-based medical packaging: Utilization of polypropylene in medical packaging applications, including blister packs, vials, and containers for pharmaceuticals and medical devices. These packaging solutions focus on maintaining product sterility, barrier properties, and compatibility with the packaged medical items.
- Surface modification of medical polypropylene: Techniques for modifying the surface of polypropylene used in medical applications to enhance properties such as biocompatibility, antimicrobial activity, or improved adhesion for coatings. These modifications may involve plasma treatment, chemical grafting, or the application of specialized coatings.
02 Polypropylene-based medical textiles
Creation of medical textiles using polypropylene fibers or fabrics, designed for applications such as surgical gowns, masks, and wound dressings. These materials offer advantages like breathability, fluid resistance, and comfort for medical professionals and patients.Expand Specific Solutions03 Polypropylene medical packaging solutions
Development of polypropylene-based packaging materials for medical devices, pharmaceuticals, and sterile products. These packaging solutions provide protection, maintain sterility, and ensure the integrity of medical items during storage and transportation.Expand Specific Solutions04 Medical polypropylene with antimicrobial properties
Incorporation of antimicrobial agents or surface treatments to polypropylene materials used in medical applications. These modifications enhance the material's ability to resist bacterial growth and reduce the risk of infections in healthcare settings.Expand Specific Solutions05 Recycling and sustainability of medical polypropylene
Development of processes and technologies for recycling medical polypropylene products, as well as the creation of more sustainable and eco-friendly polypropylene formulations for medical applications. These efforts aim to reduce the environmental impact of medical plastics while maintaining their performance and safety standards.Expand Specific Solutions
Key Medical PP Players
The medical polypropylene market for non-invasive surgery applications is in a growth phase, driven by increasing demand for minimally invasive procedures. The global market size is expanding, with projections indicating significant growth in the coming years. Technologically, the field is advancing rapidly, with companies like Tepha, Inc. and Braskem America, Inc. leading innovation in biocompatible and high-performance materials. Established players such as ExxonMobil Chemical Patents, Inc. and Mitsui Chemicals, Inc. are leveraging their expertise in polymer science to develop specialized medical-grade polypropylene. Emerging companies like Jiangsu ProMed Medical Material Co., Ltd. are also contributing to the competitive landscape, focusing on niche applications and regional markets.
Borealis AG
Technical Solution: Borealis AG has developed innovative polypropylene solutions for medical applications, including non-invasive surgical devices. Their Bormed™ portfolio includes advanced polypropylene grades specifically designed for healthcare applications. These materials offer high purity, excellent transparency, and good sterilization resistance, making them suitable for a wide range of non-invasive medical devices[11]. Borealis has focused on creating polypropylene formulations that meet stringent regulatory requirements while providing enhanced performance characteristics such as improved impact resistance and flow properties. Their technology has been applied in the development of diagnostic devices, drug delivery systems, and minimally invasive surgical instruments[12]. Additionally, Borealis has explored the use of their polypropylene grades in 3D printing applications for personalized medical devices, potentially revolutionizing the production of custom surgical tools and implants[13].
Strengths: Wide range of medical-grade polypropylene formulations; Focus on regulatory compliance and material purity. Weaknesses: Less specialized in specific surgical applications; Relies on partnerships for end-product development.
Abbott Cardiovascular Systems, Inc.
Technical Solution: Abbott Cardiovascular Systems has made significant advancements in utilizing medical-grade polypropylene for non-invasive cardiovascular interventions. Their technology centers on developing polypropylene-based catheters and delivery systems for minimally invasive cardiac procedures. Abbott's XIENCE Sierra™ stent delivery system, for instance, incorporates a polypropylene-based shaft that offers excellent pushability and trackability through tortuous vessels[8]. The company has also explored the use of polypropylene in creating advanced guidewires and microcatheters for complex coronary and peripheral interventions, allowing for more precise navigation and reduced procedural trauma[9]. Additionally, Abbott has invested in developing polypropylene-based heart valve repair devices that can be delivered through small incisions, significantly reducing the invasiveness of traditional open-heart surgeries[10].
Strengths: Specialized cardiovascular applications; Advanced delivery systems for minimally invasive procedures. Weaknesses: Narrow focus on cardiovascular field; May face regulatory challenges for novel devices.
PP Material Innovations
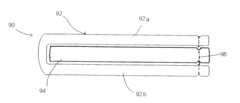
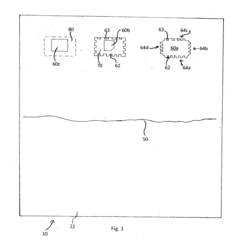
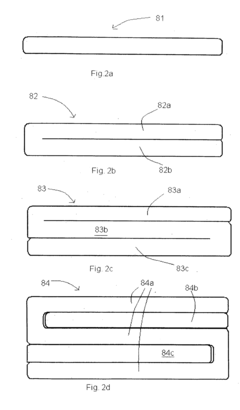
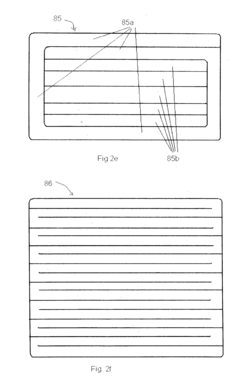
Surgical product
PatentInactiveUS20120259302A1
Innovation
- A nonwoven surgical product comprising multiple layers of wood pulp and polyester fibers with an X-ray or radio-detectable element, such as barium sulphate-coated thread, which is strong, hypoallergenic, and resistant to fiber separation, allowing for accurate counting and detection if inadvertently left in a patient.
Non-invasive and invasive health, surgical and implantable means based on polymers and silicon and fabric based on polyester and polymer-based sanitary means
PatentUndeterminedCZ20060354A3
Innovation
- Incorporation of biostatic additives containing biogenic silver ions and/or mixtures of biogenic silver and gold ions into polymer-based medical devices.
- Use of polymers and silicone-based materials for both non-invasive and invasive medical applications, providing versatility in device design.
- Integration of metallic silver and/or mixtures of metallic silver and gold into the material structure of medical devices.
Regulatory Compliance
Regulatory compliance is a critical aspect of introducing medical polypropylene for non-invasive surgery applications. The use of this material in medical devices and surgical instruments must adhere to stringent regulations set by various health authorities worldwide to ensure patient safety and product efficacy.
In the United States, the Food and Drug Administration (FDA) oversees the approval process for medical devices, including those made from medical polypropylene. Manufacturers must comply with the FDA's Quality System Regulation (QSR) and obtain premarket approval (PMA) or 510(k) clearance, depending on the device classification. The FDA also requires extensive documentation, including clinical trial data and risk assessments, to demonstrate the safety and effectiveness of the medical polypropylene devices.
In the European Union, medical devices must conform to the Medical Device Regulation (MDR) or In Vitro Diagnostic Regulation (IVDR). These regulations mandate CE marking, which involves a conformity assessment procedure and the implementation of a quality management system. Manufacturers must also appoint a qualified person responsible for regulatory compliance and maintain post-market surveillance systems.
Japan's Pharmaceuticals and Medical Devices Agency (PMDA) regulates medical devices through the Pharmaceutical and Medical Device Act. This law requires manufacturers to obtain marketing authorization and comply with Good Manufacturing Practice (GMP) standards. Similarly, China's National Medical Products Administration (NMPA) enforces regulations that necessitate product registration and quality management system certification.
International standards play a crucial role in regulatory compliance for medical polypropylene applications. ISO 13485, which specifies requirements for quality management systems in the medical device industry, is widely recognized and often required by regulatory bodies. Additionally, ISO 10993 series standards for biocompatibility testing are essential for evaluating the safety of medical polypropylene in contact with human tissues.
Manufacturers must also consider specific regulations related to sterilization methods, as medical polypropylene devices often require sterilization before use in non-invasive surgeries. Compliance with standards such as ISO 11137 for radiation sterilization or ISO 11135 for ethylene oxide sterilization is crucial to ensure the safety and efficacy of the sterilized products.
Environmental regulations are increasingly important in the medical device industry. Manufacturers must consider regulations such as the EU's Restriction of Hazardous Substances (RoHS) directive and the Registration, Evaluation, Authorization, and Restriction of Chemicals (REACH) regulation when developing medical polypropylene products. These regulations aim to reduce the environmental impact of medical devices and ensure the safety of materials used in their production.
In the United States, the Food and Drug Administration (FDA) oversees the approval process for medical devices, including those made from medical polypropylene. Manufacturers must comply with the FDA's Quality System Regulation (QSR) and obtain premarket approval (PMA) or 510(k) clearance, depending on the device classification. The FDA also requires extensive documentation, including clinical trial data and risk assessments, to demonstrate the safety and effectiveness of the medical polypropylene devices.
In the European Union, medical devices must conform to the Medical Device Regulation (MDR) or In Vitro Diagnostic Regulation (IVDR). These regulations mandate CE marking, which involves a conformity assessment procedure and the implementation of a quality management system. Manufacturers must also appoint a qualified person responsible for regulatory compliance and maintain post-market surveillance systems.
Japan's Pharmaceuticals and Medical Devices Agency (PMDA) regulates medical devices through the Pharmaceutical and Medical Device Act. This law requires manufacturers to obtain marketing authorization and comply with Good Manufacturing Practice (GMP) standards. Similarly, China's National Medical Products Administration (NMPA) enforces regulations that necessitate product registration and quality management system certification.
International standards play a crucial role in regulatory compliance for medical polypropylene applications. ISO 13485, which specifies requirements for quality management systems in the medical device industry, is widely recognized and often required by regulatory bodies. Additionally, ISO 10993 series standards for biocompatibility testing are essential for evaluating the safety of medical polypropylene in contact with human tissues.
Manufacturers must also consider specific regulations related to sterilization methods, as medical polypropylene devices often require sterilization before use in non-invasive surgeries. Compliance with standards such as ISO 11137 for radiation sterilization or ISO 11135 for ethylene oxide sterilization is crucial to ensure the safety and efficacy of the sterilized products.
Environmental regulations are increasingly important in the medical device industry. Manufacturers must consider regulations such as the EU's Restriction of Hazardous Substances (RoHS) directive and the Registration, Evaluation, Authorization, and Restriction of Chemicals (REACH) regulation when developing medical polypropylene products. These regulations aim to reduce the environmental impact of medical devices and ensure the safety of materials used in their production.
Biocompatibility Aspects
Biocompatibility is a critical aspect of medical polypropylene's application in non-invasive surgery. The material's ability to interact safely with living tissues and biological systems is paramount for its successful implementation in medical devices and surgical instruments. Polypropylene has demonstrated excellent biocompatibility properties, making it a preferred choice for various medical applications.
One of the key factors contributing to polypropylene's biocompatibility is its chemical inertness. The material does not readily react with bodily fluids or tissues, reducing the risk of adverse reactions or inflammatory responses. This characteristic is particularly important in non-invasive surgical procedures, where the material may come into contact with sensitive internal organs or blood vessels.
Furthermore, polypropylene exhibits low toxicity and does not leach harmful substances into the surrounding tissues. This property ensures that the material remains stable and does not compromise patient safety during and after surgical procedures. The absence of toxic byproducts also contributes to faster healing and reduced risk of complications.
The material's resistance to degradation in biological environments is another crucial biocompatibility aspect. Polypropylene maintains its structural integrity and mechanical properties when exposed to bodily fluids and enzymes, ensuring the longevity and reliability of medical devices and implants. This stability is essential for applications such as surgical meshes or sutures used in non-invasive procedures.
Polypropylene's surface properties also play a significant role in its biocompatibility. The material's smooth surface reduces the risk of bacterial adhesion and biofilm formation, which can lead to infections. Additionally, the hydrophobic nature of polypropylene helps prevent the accumulation of proteins and other biological molecules on its surface, further enhancing its biocompatibility.
In terms of immune response, polypropylene generally elicits minimal reactions from the body's immune system. This characteristic is crucial for preventing inflammation, tissue rejection, or other adverse immune responses that could compromise the success of non-invasive surgical procedures. The material's ability to integrate with surrounding tissues without triggering significant immune reactions contributes to its widespread use in medical applications.
Sterilization compatibility is another important aspect of polypropylene's biocompatibility profile. The material can withstand common sterilization methods, including ethylene oxide treatment, gamma radiation, and steam autoclaving, without compromising its physical or chemical properties. This ensures that medical devices and instruments made from polypropylene can be effectively sterilized, maintaining their biocompatibility and safety for use in non-invasive surgical procedures.
One of the key factors contributing to polypropylene's biocompatibility is its chemical inertness. The material does not readily react with bodily fluids or tissues, reducing the risk of adverse reactions or inflammatory responses. This characteristic is particularly important in non-invasive surgical procedures, where the material may come into contact with sensitive internal organs or blood vessels.
Furthermore, polypropylene exhibits low toxicity and does not leach harmful substances into the surrounding tissues. This property ensures that the material remains stable and does not compromise patient safety during and after surgical procedures. The absence of toxic byproducts also contributes to faster healing and reduced risk of complications.
The material's resistance to degradation in biological environments is another crucial biocompatibility aspect. Polypropylene maintains its structural integrity and mechanical properties when exposed to bodily fluids and enzymes, ensuring the longevity and reliability of medical devices and implants. This stability is essential for applications such as surgical meshes or sutures used in non-invasive procedures.
Polypropylene's surface properties also play a significant role in its biocompatibility. The material's smooth surface reduces the risk of bacterial adhesion and biofilm formation, which can lead to infections. Additionally, the hydrophobic nature of polypropylene helps prevent the accumulation of proteins and other biological molecules on its surface, further enhancing its biocompatibility.
In terms of immune response, polypropylene generally elicits minimal reactions from the body's immune system. This characteristic is crucial for preventing inflammation, tissue rejection, or other adverse immune responses that could compromise the success of non-invasive surgical procedures. The material's ability to integrate with surrounding tissues without triggering significant immune reactions contributes to its widespread use in medical applications.
Sterilization compatibility is another important aspect of polypropylene's biocompatibility profile. The material can withstand common sterilization methods, including ethylene oxide treatment, gamma radiation, and steam autoclaving, without compromising its physical or chemical properties. This ensures that medical devices and instruments made from polypropylene can be effectively sterilized, maintaining their biocompatibility and safety for use in non-invasive surgical procedures.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!