Age-Related Muscimol Sensitivity in Neuromodulation
JUL 4, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Muscimol Neuromodulation Background and Objectives
Muscimol, a potent GABA-A receptor agonist, has been a subject of significant interest in the field of neuromodulation for decades. Its ability to selectively activate GABA-A receptors makes it a valuable tool for investigating inhibitory neurotransmission and its effects on various neurological processes. The study of age-related changes in muscimol sensitivity has emerged as a crucial area of research, given the increasing global aging population and the prevalence of age-related neurological disorders.
The primary objective of this research is to elucidate the complex relationship between aging and muscimol sensitivity in the context of neuromodulation. This involves exploring how the efficacy and impact of muscimol-induced neuromodulation may vary across different age groups, from young adults to the elderly. Understanding these age-related changes is essential for developing more effective and personalized neuromodulatory interventions for age-related neurological conditions.
Historically, muscimol research has evolved from basic pharmacological studies to more sophisticated investigations of its neuromodulatory effects. Early work focused on characterizing muscimol's binding properties and its acute effects on neural activity. As research progressed, scientists began to explore its potential therapeutic applications in various neurological and psychiatric disorders.
Recent technological advancements have enabled more precise and targeted delivery of muscimol, allowing researchers to study its effects on specific brain regions and neural circuits. This has led to a better understanding of how muscimol-induced neuromodulation can influence cognitive processes, motor function, and emotional regulation across different age groups.
The current research landscape is characterized by a growing interest in the intersection of aging neurobiology and neuromodulation techniques. This includes investigating how age-related changes in GABA-A receptor expression, distribution, and function may influence the effectiveness of muscimol-based interventions. Additionally, researchers are exploring the potential of muscimol as a tool for mitigating age-related cognitive decline and as a therapeutic agent for neurodegenerative diseases.
As we look towards future developments, the field aims to uncover the molecular and cellular mechanisms underlying age-related changes in muscimol sensitivity. This knowledge will be crucial for optimizing neuromodulatory strategies and developing age-specific interventions. Furthermore, there is a growing emphasis on translating these findings into clinical applications, with the ultimate goal of improving the quality of life for aging populations affected by neurological disorders.
The primary objective of this research is to elucidate the complex relationship between aging and muscimol sensitivity in the context of neuromodulation. This involves exploring how the efficacy and impact of muscimol-induced neuromodulation may vary across different age groups, from young adults to the elderly. Understanding these age-related changes is essential for developing more effective and personalized neuromodulatory interventions for age-related neurological conditions.
Historically, muscimol research has evolved from basic pharmacological studies to more sophisticated investigations of its neuromodulatory effects. Early work focused on characterizing muscimol's binding properties and its acute effects on neural activity. As research progressed, scientists began to explore its potential therapeutic applications in various neurological and psychiatric disorders.
Recent technological advancements have enabled more precise and targeted delivery of muscimol, allowing researchers to study its effects on specific brain regions and neural circuits. This has led to a better understanding of how muscimol-induced neuromodulation can influence cognitive processes, motor function, and emotional regulation across different age groups.
The current research landscape is characterized by a growing interest in the intersection of aging neurobiology and neuromodulation techniques. This includes investigating how age-related changes in GABA-A receptor expression, distribution, and function may influence the effectiveness of muscimol-based interventions. Additionally, researchers are exploring the potential of muscimol as a tool for mitigating age-related cognitive decline and as a therapeutic agent for neurodegenerative diseases.
As we look towards future developments, the field aims to uncover the molecular and cellular mechanisms underlying age-related changes in muscimol sensitivity. This knowledge will be crucial for optimizing neuromodulatory strategies and developing age-specific interventions. Furthermore, there is a growing emphasis on translating these findings into clinical applications, with the ultimate goal of improving the quality of life for aging populations affected by neurological disorders.
Market Analysis for Age-Specific Neuromodulation Therapies
The market for age-specific neuromodulation therapies is experiencing significant growth, driven by the increasing prevalence of age-related neurological disorders and the growing aging population worldwide. As the global population continues to age, there is a rising demand for innovative treatments that can address the unique neurological challenges faced by older adults.
Neuromodulation therapies tailored to specific age groups, particularly those focusing on muscimol sensitivity, represent a promising segment within the broader neuromodulation market. These therapies aim to provide targeted interventions for age-related neurological conditions, such as cognitive decline, movement disorders, and chronic pain, which become more prevalent as individuals age.
The market for age-specific neuromodulation therapies is characterized by a diverse range of products and technologies, including deep brain stimulation devices, spinal cord stimulators, and transcranial magnetic stimulation systems. These technologies are being adapted and refined to address the specific needs of different age groups, with a particular focus on the elderly population.
Key market drivers include the increasing awareness of age-related neurological disorders, advancements in neuromodulation technologies, and the growing acceptance of non-pharmacological treatment options. Additionally, the potential for improved quality of life and reduced healthcare costs associated with successful neuromodulation therapies is attracting significant interest from healthcare providers and payers.
The market is segmented by age groups, with a particular emphasis on therapies designed for older adults. This segmentation allows for more targeted and effective treatments, as the neurological needs and responses to neuromodulation can vary significantly across different age groups.
Geographically, North America and Europe currently dominate the market for age-specific neuromodulation therapies, due to their advanced healthcare infrastructure and higher adoption rates of innovative medical technologies. However, the Asia-Pacific region is expected to witness rapid growth in the coming years, driven by improving healthcare access and rising disposable incomes in emerging economies.
Despite the promising outlook, the market faces several challenges, including high treatment costs, limited reimbursement policies, and the need for more extensive clinical evidence to support the efficacy of age-specific neuromodulation therapies. Overcoming these barriers will be crucial for the continued expansion and adoption of these innovative treatments.
As research on age-related muscimol sensitivity in neuromodulation advances, it is expected to open new avenues for targeted therapies and potentially expand the market further. This research could lead to the development of more precise and effective neuromodulation treatments tailored to the specific neurological needs of different age groups, particularly in addressing age-related changes in neurotransmitter sensitivity.
Neuromodulation therapies tailored to specific age groups, particularly those focusing on muscimol sensitivity, represent a promising segment within the broader neuromodulation market. These therapies aim to provide targeted interventions for age-related neurological conditions, such as cognitive decline, movement disorders, and chronic pain, which become more prevalent as individuals age.
The market for age-specific neuromodulation therapies is characterized by a diverse range of products and technologies, including deep brain stimulation devices, spinal cord stimulators, and transcranial magnetic stimulation systems. These technologies are being adapted and refined to address the specific needs of different age groups, with a particular focus on the elderly population.
Key market drivers include the increasing awareness of age-related neurological disorders, advancements in neuromodulation technologies, and the growing acceptance of non-pharmacological treatment options. Additionally, the potential for improved quality of life and reduced healthcare costs associated with successful neuromodulation therapies is attracting significant interest from healthcare providers and payers.
The market is segmented by age groups, with a particular emphasis on therapies designed for older adults. This segmentation allows for more targeted and effective treatments, as the neurological needs and responses to neuromodulation can vary significantly across different age groups.
Geographically, North America and Europe currently dominate the market for age-specific neuromodulation therapies, due to their advanced healthcare infrastructure and higher adoption rates of innovative medical technologies. However, the Asia-Pacific region is expected to witness rapid growth in the coming years, driven by improving healthcare access and rising disposable incomes in emerging economies.
Despite the promising outlook, the market faces several challenges, including high treatment costs, limited reimbursement policies, and the need for more extensive clinical evidence to support the efficacy of age-specific neuromodulation therapies. Overcoming these barriers will be crucial for the continued expansion and adoption of these innovative treatments.
As research on age-related muscimol sensitivity in neuromodulation advances, it is expected to open new avenues for targeted therapies and potentially expand the market further. This research could lead to the development of more precise and effective neuromodulation treatments tailored to the specific neurological needs of different age groups, particularly in addressing age-related changes in neurotransmitter sensitivity.
Current Challenges in Age-Related Muscimol Sensitivity
The field of age-related muscimol sensitivity in neuromodulation faces several significant challenges that hinder progress and limit our understanding of this complex phenomenon. One of the primary obstacles is the lack of comprehensive longitudinal studies that track changes in muscimol sensitivity across the lifespan. Such studies are crucial for establishing a clear trajectory of how GABA receptor responses to muscimol evolve with age, but they are time-consuming and resource-intensive.
Another major challenge lies in the heterogeneity of aging processes among individuals. Factors such as genetics, lifestyle, and environmental exposures can significantly influence the rate and pattern of age-related changes in neural systems. This variability makes it difficult to establish standardized protocols for assessing muscimol sensitivity and complicates the interpretation of research findings across different populations.
The complexity of the aging brain itself presents a formidable challenge. As the brain ages, it undergoes numerous structural and functional changes, including alterations in neurotransmitter systems, synaptic plasticity, and neural network connectivity. Disentangling the specific effects of age on muscimol sensitivity from these broader neurological changes requires sophisticated experimental designs and advanced analytical techniques.
Furthermore, there is a notable gap in our understanding of the molecular mechanisms underlying age-related changes in muscimol sensitivity. While it is known that GABA receptor subunit composition and distribution change with age, the precise dynamics of these alterations and their functional consequences remain poorly understood. This knowledge gap hampers the development of targeted interventions to modulate muscimol sensitivity in aging populations.
Ethical considerations also pose challenges in this field of research. Studies involving the administration of neuroactive compounds to elderly populations must navigate complex ethical landscapes, balancing the potential benefits of research with the risks to vulnerable subjects. This often results in limitations on the types and extent of experiments that can be conducted, particularly in human studies.
Technological limitations present additional hurdles. Current neuroimaging and electrophysiological techniques may lack the resolution or sensitivity required to detect subtle age-related changes in muscimol binding and receptor function. Developing more advanced, non-invasive methods for assessing GABA receptor activity in vivo is crucial for advancing our understanding of age-related muscimol sensitivity.
Lastly, translating findings from animal models to human applications remains a significant challenge. While animal studies provide valuable insights, the complexity of the human brain and the unique aspects of human aging necessitate careful validation of animal-derived data in human subjects. Bridging this translational gap is essential for developing effective neuromodulation strategies based on age-related muscimol sensitivity research.
Another major challenge lies in the heterogeneity of aging processes among individuals. Factors such as genetics, lifestyle, and environmental exposures can significantly influence the rate and pattern of age-related changes in neural systems. This variability makes it difficult to establish standardized protocols for assessing muscimol sensitivity and complicates the interpretation of research findings across different populations.
The complexity of the aging brain itself presents a formidable challenge. As the brain ages, it undergoes numerous structural and functional changes, including alterations in neurotransmitter systems, synaptic plasticity, and neural network connectivity. Disentangling the specific effects of age on muscimol sensitivity from these broader neurological changes requires sophisticated experimental designs and advanced analytical techniques.
Furthermore, there is a notable gap in our understanding of the molecular mechanisms underlying age-related changes in muscimol sensitivity. While it is known that GABA receptor subunit composition and distribution change with age, the precise dynamics of these alterations and their functional consequences remain poorly understood. This knowledge gap hampers the development of targeted interventions to modulate muscimol sensitivity in aging populations.
Ethical considerations also pose challenges in this field of research. Studies involving the administration of neuroactive compounds to elderly populations must navigate complex ethical landscapes, balancing the potential benefits of research with the risks to vulnerable subjects. This often results in limitations on the types and extent of experiments that can be conducted, particularly in human studies.
Technological limitations present additional hurdles. Current neuroimaging and electrophysiological techniques may lack the resolution or sensitivity required to detect subtle age-related changes in muscimol binding and receptor function. Developing more advanced, non-invasive methods for assessing GABA receptor activity in vivo is crucial for advancing our understanding of age-related muscimol sensitivity.
Lastly, translating findings from animal models to human applications remains a significant challenge. While animal studies provide valuable insights, the complexity of the human brain and the unique aspects of human aging necessitate careful validation of animal-derived data in human subjects. Bridging this translational gap is essential for developing effective neuromodulation strategies based on age-related muscimol sensitivity research.
Existing Approaches to Age-Adjusted Muscimol Administration
01 Detection methods for muscimol sensitivity
Various detection methods have been developed to assess muscimol sensitivity in biological samples. These methods may include spectroscopic techniques, chromatography, or biosensors that can accurately measure the presence and concentration of muscimol. Such detection methods are crucial for research, medical diagnostics, and potential therapeutic applications related to muscimol and its effects on GABA receptors.- Detection methods for muscimol sensitivity: Various detection methods have been developed to assess muscimol sensitivity in biological samples. These methods may include spectroscopic techniques, chromatography, or biosensors that can accurately measure the presence and concentration of muscimol. Such detection methods are crucial for research, medical diagnostics, and potential therapeutic applications related to muscimol sensitivity.
- Pharmaceutical compositions targeting muscimol sensitivity: Researchers have formulated pharmaceutical compositions that specifically target muscimol sensitivity. These compositions may include muscimol analogs, antagonists, or other compounds that modulate GABA receptor activity. Such formulations aim to either enhance or mitigate the effects of muscimol, depending on the desired therapeutic outcome.
- Imaging techniques for muscimol-sensitive receptors: Advanced imaging techniques have been developed to visualize and study muscimol-sensitive receptors in the brain and other tissues. These methods may involve fluorescent labeling, positron emission tomography (PET), or other molecular imaging approaches that allow researchers to track the distribution and activity of muscimol-sensitive receptors in real-time.
- Genetic factors influencing muscimol sensitivity: Studies have identified genetic factors that may influence an individual's sensitivity to muscimol. This research involves analyzing genetic variations in GABA receptor subunits and other related genes to understand how they affect muscimol binding and receptor function. Such insights could lead to personalized approaches in treatments involving muscimol or related compounds.
- Applications of muscimol sensitivity in neuroscience research: Muscimol sensitivity has been utilized in various neuroscience research applications. These may include studying neural circuits, investigating the role of GABAergic signaling in brain function, and developing potential treatments for neurological disorders. Researchers have developed tools and protocols that leverage muscimol sensitivity to probe specific aspects of brain activity and behavior.
02 Pharmaceutical compositions targeting muscimol sensitivity
Researchers have developed pharmaceutical compositions that target muscimol sensitivity for potential therapeutic applications. These formulations may include muscimol analogs, GABA receptor modulators, or other compounds that interact with the GABAergic system. Such compositions aim to modulate neuronal activity and may have applications in treating various neurological and psychiatric disorders.Expand Specific Solutions03 Imaging techniques for visualizing muscimol activity
Advanced imaging techniques have been developed to visualize and analyze muscimol activity in the brain and other tissues. These methods may include fluorescence microscopy, PET scanning, or other molecular imaging approaches that allow researchers to track the distribution and effects of muscimol in real-time. Such techniques provide valuable insights into the mechanisms of muscimol action and its impact on neural circuits.Expand Specific Solutions04 Genetic factors influencing muscimol sensitivity
Studies have identified genetic factors that may influence an individual's sensitivity to muscimol. This research involves analyzing genetic variations in GABA receptor subunits, neurotransmitter transporters, or other related proteins. Understanding these genetic factors could help predict individual responses to muscimol and inform personalized treatment approaches in the future.Expand Specific Solutions05 Environmental and physiological factors affecting muscimol sensitivity
Research has explored various environmental and physiological factors that can affect an individual's sensitivity to muscimol. These factors may include age, diet, stress levels, or exposure to other substances that interact with the GABAergic system. Understanding these influences is crucial for accurately assessing muscimol sensitivity and developing appropriate dosing strategies for potential therapeutic applications.Expand Specific Solutions
Key Players in Neuromodulation Research and Development
The research on age-related muscimol sensitivity in neuromodulation is in an early developmental stage, with a growing market potential as the global population ages. The competitive landscape is characterized by a mix of established pharmaceutical companies, specialized neuromodulation firms, and academic institutions. Key players like AgeneBio, Saluda Medical, and Boston Scientific Neuromodulation are advancing the field with innovative approaches. The technology's maturity varies, with some companies focusing on drug development while others explore device-based solutions. As the understanding of age-related neural changes deepens, collaborations between industry and research institutions, such as Washington University in St. Louis and the University of Leiden, are likely to drive progress in this emerging field.
AgeneBio, Inc.
Technical Solution: AgeneBio has developed a novel approach to address age-related cognitive decline by targeting hippocampal overactivity. Their lead compound, AGB101, is a low-dose formulation of levetiracetam that aims to reduce excess hippocampal activity[1]. While not directly using muscimol, their research on age-related neural hyperactivity provides valuable insights into neuromodulation sensitivity changes with age. They have conducted clinical trials showing that reducing hippocampal overactivity can improve memory performance in elderly patients with amnestic mild cognitive impairment (aMCI)[2]. This approach demonstrates the potential for age-specific neuromodulation strategies.
Strengths: Targeted approach to age-related cognitive decline, clinical trial evidence supporting efficacy. Weaknesses: Limited to specific neurotransmitter systems, may not address all aspects of age-related changes in neuromodulation sensitivity.
Washington University in St. Louis
Technical Solution: Researchers at Washington University in St. Louis have made significant contributions to understanding age-related changes in neurotransmitter systems, including GABA receptors which are the primary target of muscimol. They have conducted studies using advanced neuroimaging techniques to examine how GABAergic neurotransmission changes with age[3]. Their research has shown that GABA levels in the frontal and parietal cortices decrease with age, which may contribute to cognitive decline[4]. While not specifically focused on muscimol, their work provides crucial insights into how the aging brain's response to GABAergic compounds may change, informing potential neuromodulation strategies for older adults.
Strengths: Comprehensive neuroimaging studies, focus on age-related changes in neurotransmitter systems. Weaknesses: Research is primarily observational, may require further translation to therapeutic applications.
Innovative Techniques in Age-Specific Neuromodulation
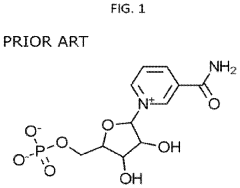
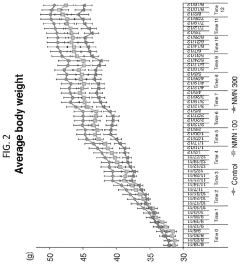
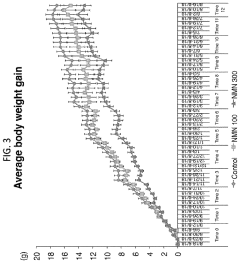
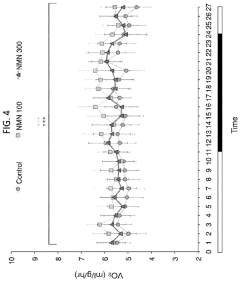
Administration of nicotinamide mononucleotide in the treatment of disease
PatentActiveUS20240009222A1
Innovation
- Administration of nicotinamide mononucleotide (NMN) through various compositions and routes, including oral and intraocular administration, to treat and prevent age-associated degenerative changes by enhancing NAD+ levels and promoting cellular health.
Adaptation of Neurostimulation Therapy to Age-Related Physiological Changes
PatentActiveUS20230014405A1
Innovation
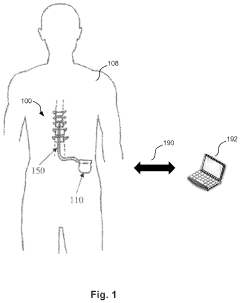
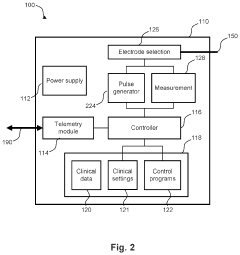
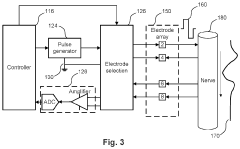
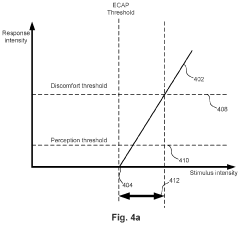
- Implantable devices and methods that enable self-reprogramming to adapt therapy parameters, such as stimulus intensity and ECAP targets, over time based on measured age-related physiological characteristics, using predefined schedules that can be altered in response to changes in patient physiology.
Regulatory Framework for Age-Specific Neuromodulation
The regulatory framework for age-specific neuromodulation is a critical aspect of research on age-related muscimol sensitivity. As the field of neuromodulation advances, it becomes increasingly important to establish comprehensive guidelines that address the unique considerations associated with different age groups.
Current regulations primarily focus on general safety and efficacy standards for neuromodulation devices and treatments. However, the growing body of evidence suggesting age-related differences in muscimol sensitivity necessitates a more nuanced approach. Regulatory bodies, such as the FDA in the United States and the EMA in Europe, are beginning to recognize the need for age-specific guidelines in neuromodulation.
One key area of focus is the development of age-appropriate dosing protocols. As muscimol sensitivity can vary significantly between younger and older populations, regulators are working to establish guidelines that account for these differences. This includes recommendations for initial dosing, titration schedules, and maximum dosage limits based on age groups.
Safety monitoring requirements are also being tailored to address age-specific concerns. For instance, older adults may require more frequent follow-ups and assessments to monitor for potential adverse effects related to altered muscimol sensitivity. Regulators are considering mandating specialized protocols for geriatric patients undergoing neuromodulation treatments.
The ethical implications of age-specific neuromodulation are another crucial aspect of the regulatory framework. Guidelines are being developed to ensure informed consent processes adequately address age-related risks and benefits. This includes requirements for clear communication of potential age-specific side effects and treatment outcomes.
Regulatory bodies are also focusing on the standardization of clinical trial designs for age-related neuromodulation research. This includes guidelines for age-stratified participant recruitment, appropriate outcome measures for different age groups, and long-term follow-up requirements to assess the durability of treatment effects across the lifespan.
As the field continues to evolve, regulators are working to establish a flexible framework that can adapt to new findings in age-related muscimol sensitivity research. This includes provisions for regular review and updates to guidelines based on emerging scientific evidence. The goal is to create a regulatory environment that promotes innovation while ensuring the safety and efficacy of neuromodulation treatments across all age groups.
Current regulations primarily focus on general safety and efficacy standards for neuromodulation devices and treatments. However, the growing body of evidence suggesting age-related differences in muscimol sensitivity necessitates a more nuanced approach. Regulatory bodies, such as the FDA in the United States and the EMA in Europe, are beginning to recognize the need for age-specific guidelines in neuromodulation.
One key area of focus is the development of age-appropriate dosing protocols. As muscimol sensitivity can vary significantly between younger and older populations, regulators are working to establish guidelines that account for these differences. This includes recommendations for initial dosing, titration schedules, and maximum dosage limits based on age groups.
Safety monitoring requirements are also being tailored to address age-specific concerns. For instance, older adults may require more frequent follow-ups and assessments to monitor for potential adverse effects related to altered muscimol sensitivity. Regulators are considering mandating specialized protocols for geriatric patients undergoing neuromodulation treatments.
The ethical implications of age-specific neuromodulation are another crucial aspect of the regulatory framework. Guidelines are being developed to ensure informed consent processes adequately address age-related risks and benefits. This includes requirements for clear communication of potential age-specific side effects and treatment outcomes.
Regulatory bodies are also focusing on the standardization of clinical trial designs for age-related neuromodulation research. This includes guidelines for age-stratified participant recruitment, appropriate outcome measures for different age groups, and long-term follow-up requirements to assess the durability of treatment effects across the lifespan.
As the field continues to evolve, regulators are working to establish a flexible framework that can adapt to new findings in age-related muscimol sensitivity research. This includes provisions for regular review and updates to guidelines based on emerging scientific evidence. The goal is to create a regulatory environment that promotes innovation while ensuring the safety and efficacy of neuromodulation treatments across all age groups.
Ethical Implications of Age-Based Neuromodulation Treatments
The ethical implications of age-based neuromodulation treatments raise significant concerns that require careful consideration. As research on age-related muscimol sensitivity in neuromodulation advances, it becomes crucial to address the ethical challenges associated with tailoring treatments based on age.
One primary ethical concern is the potential for age discrimination in healthcare. If neuromodulation treatments are found to be more effective or safer for certain age groups, it may lead to unequal access to care. This could result in older or younger individuals being denied potentially beneficial treatments solely based on their age, which raises questions of fairness and equity in healthcare provision.
Another ethical consideration is the impact on personal autonomy and informed consent. Age-related differences in treatment efficacy may complicate the decision-making process for patients and healthcare providers. Ensuring that patients of all ages can make fully informed decisions about their treatment options becomes increasingly challenging when age is a significant factor in determining outcomes.
Privacy and data protection also emerge as critical ethical issues. As research in this field progresses, it may require extensive collection and analysis of age-related health data. Safeguarding this sensitive information and preventing its misuse or unauthorized access is paramount to protect individuals' rights and maintain public trust in age-based neuromodulation research and treatments.
The potential for age-based treatments to exacerbate existing health disparities is another ethical concern. If certain age groups benefit more from these advanced treatments, it could widen the gap in health outcomes between different generations, potentially leading to social and economic implications that extend beyond individual health.
Furthermore, the long-term effects of age-specific neuromodulation treatments remain uncertain. Ethical questions arise regarding the responsibility of researchers and healthcare providers in monitoring and managing potential unforeseen consequences that may manifest differently across age groups over time.
The allocation of research resources and funding also presents ethical challenges. Prioritizing research on age-related muscimol sensitivity may divert attention and resources from other important areas of neuroscience and healthcare, potentially disadvantaging certain patient populations or neglecting other promising avenues of treatment.
In conclusion, while age-based neuromodulation treatments hold promise for improving patient outcomes, they also introduce complex ethical dilemmas. Addressing these challenges requires a multidisciplinary approach, involving ethicists, policymakers, healthcare professionals, and patient advocates to develop guidelines and frameworks that ensure equitable, responsible, and ethically sound implementation of these emerging technologies.
One primary ethical concern is the potential for age discrimination in healthcare. If neuromodulation treatments are found to be more effective or safer for certain age groups, it may lead to unequal access to care. This could result in older or younger individuals being denied potentially beneficial treatments solely based on their age, which raises questions of fairness and equity in healthcare provision.
Another ethical consideration is the impact on personal autonomy and informed consent. Age-related differences in treatment efficacy may complicate the decision-making process for patients and healthcare providers. Ensuring that patients of all ages can make fully informed decisions about their treatment options becomes increasingly challenging when age is a significant factor in determining outcomes.
Privacy and data protection also emerge as critical ethical issues. As research in this field progresses, it may require extensive collection and analysis of age-related health data. Safeguarding this sensitive information and preventing its misuse or unauthorized access is paramount to protect individuals' rights and maintain public trust in age-based neuromodulation research and treatments.
The potential for age-based treatments to exacerbate existing health disparities is another ethical concern. If certain age groups benefit more from these advanced treatments, it could widen the gap in health outcomes between different generations, potentially leading to social and economic implications that extend beyond individual health.
Furthermore, the long-term effects of age-specific neuromodulation treatments remain uncertain. Ethical questions arise regarding the responsibility of researchers and healthcare providers in monitoring and managing potential unforeseen consequences that may manifest differently across age groups over time.
The allocation of research resources and funding also presents ethical challenges. Prioritizing research on age-related muscimol sensitivity may divert attention and resources from other important areas of neuroscience and healthcare, potentially disadvantaging certain patient populations or neglecting other promising avenues of treatment.
In conclusion, while age-based neuromodulation treatments hold promise for improving patient outcomes, they also introduce complex ethical dilemmas. Addressing these challenges requires a multidisciplinary approach, involving ethicists, policymakers, healthcare professionals, and patient advocates to develop guidelines and frameworks that ensure equitable, responsible, and ethically sound implementation of these emerging technologies.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!