Analysis of Point-of-care Devices in Infectious Disease Diagnosis
SEP 19, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Point-of-care Testing Background and Objectives
Point-of-care testing (POCT) represents a paradigm shift in diagnostic medicine, evolving from traditional laboratory-based testing to rapid, decentralized testing at or near the patient's location. This evolution began in the 1980s with simple glucose meters and has since expanded to encompass a wide range of diagnostic capabilities. The fundamental principle of POCT is to deliver actionable diagnostic information within minutes rather than hours or days, enabling immediate clinical decision-making and intervention.
In the context of infectious disease diagnosis, POCT has gained significant momentum due to the global burden of infectious diseases and the critical need for rapid detection and containment. The COVID-19 pandemic dramatically accelerated both the development and adoption of POCT technologies, highlighting their essential role in public health emergencies and routine healthcare settings alike.
The primary objectives of POCT in infectious disease diagnosis are multifaceted. First, to reduce the time-to-result from hours or days to minutes, enabling prompt treatment decisions and infection control measures. Second, to extend diagnostic capabilities to resource-limited settings where traditional laboratory infrastructure is unavailable. Third, to improve patient outcomes through earlier intervention and appropriate antimicrobial stewardship.
Technologically, POCT devices for infectious diseases have progressed from simple lateral flow immunoassays to sophisticated molecular diagnostic platforms capable of detecting nucleic acids with high sensitivity and specificity. This progression reflects broader technological trends including miniaturization, automation, and integration of multiple analytical steps into self-contained systems.
The development trajectory of POCT is increasingly focused on multiplexed testing capabilities, allowing simultaneous detection of multiple pathogens from a single sample. Additionally, connectivity features enabling result transmission to electronic health records and public health surveillance systems represent a critical advancement in the field.
Looking forward, the technical goals for next-generation POCT devices include further improvements in sensitivity and specificity, reduced cost per test, simplified operation requiring minimal training, and enhanced durability for field deployment in challenging environments. The ultimate objective is to develop truly universal POCT platforms that can be rapidly adapted to emerging infectious threats through simple modifications rather than complete redesign.
The convergence of advances in microfluidics, biosensors, nanomaterials, and artificial intelligence is expected to drive the next wave of innovation in POCT for infectious diseases, potentially transforming our approach to disease surveillance, outbreak response, and routine clinical care.
In the context of infectious disease diagnosis, POCT has gained significant momentum due to the global burden of infectious diseases and the critical need for rapid detection and containment. The COVID-19 pandemic dramatically accelerated both the development and adoption of POCT technologies, highlighting their essential role in public health emergencies and routine healthcare settings alike.
The primary objectives of POCT in infectious disease diagnosis are multifaceted. First, to reduce the time-to-result from hours or days to minutes, enabling prompt treatment decisions and infection control measures. Second, to extend diagnostic capabilities to resource-limited settings where traditional laboratory infrastructure is unavailable. Third, to improve patient outcomes through earlier intervention and appropriate antimicrobial stewardship.
Technologically, POCT devices for infectious diseases have progressed from simple lateral flow immunoassays to sophisticated molecular diagnostic platforms capable of detecting nucleic acids with high sensitivity and specificity. This progression reflects broader technological trends including miniaturization, automation, and integration of multiple analytical steps into self-contained systems.
The development trajectory of POCT is increasingly focused on multiplexed testing capabilities, allowing simultaneous detection of multiple pathogens from a single sample. Additionally, connectivity features enabling result transmission to electronic health records and public health surveillance systems represent a critical advancement in the field.
Looking forward, the technical goals for next-generation POCT devices include further improvements in sensitivity and specificity, reduced cost per test, simplified operation requiring minimal training, and enhanced durability for field deployment in challenging environments. The ultimate objective is to develop truly universal POCT platforms that can be rapidly adapted to emerging infectious threats through simple modifications rather than complete redesign.
The convergence of advances in microfluidics, biosensors, nanomaterials, and artificial intelligence is expected to drive the next wave of innovation in POCT for infectious diseases, potentially transforming our approach to disease surveillance, outbreak response, and routine clinical care.
Market Analysis for Infectious Disease POC Diagnostics
The global market for Point-of-Care (POC) diagnostic devices for infectious diseases has experienced significant growth in recent years, driven by increasing prevalence of infectious diseases, growing demand for rapid diagnostic solutions, and technological advancements. The market was valued at approximately $18.4 billion in 2021 and is projected to reach $30.9 billion by 2027, growing at a CAGR of 9.1% during the forecast period.
COVID-19 has substantially accelerated market expansion, creating unprecedented demand for rapid testing solutions. This pandemic-induced growth has attracted numerous new entrants to the market while prompting established players to expand their infectious disease diagnostic portfolios. The market has witnessed a paradigm shift from traditional laboratory-based testing to decentralized point-of-care testing.
Geographically, North America dominates the market with approximately 40% share, followed by Europe at 30% and Asia-Pacific at 20%. The Asia-Pacific region is expected to witness the highest growth rate due to increasing healthcare expenditure, growing awareness about early disease diagnosis, and improving healthcare infrastructure in countries like China and India.
By pathogen type, bacterial infection diagnostics currently hold the largest market share at 45%, followed by viral infection diagnostics at 35%. However, viral infection diagnostics segment is growing at a faster rate due to the ongoing pandemic and increasing prevalence of viral outbreaks globally.
The market is segmented by technology into immunoassays, molecular diagnostics, microfluidics, and others. Immunoassays currently dominate with 50% market share, but molecular diagnostic POC devices are experiencing the fastest growth due to their higher accuracy and ability to detect pathogens at lower concentrations.
End-user analysis reveals that hospitals and clinics remain the primary users of infectious disease POC diagnostics, accounting for 55% of the market. However, home care settings are emerging as a rapidly growing segment, expected to register a CAGR of 12% during the forecast period, driven by increasing preference for self-testing and remote patient monitoring.
Key market challenges include stringent regulatory requirements, reimbursement issues, and quality concerns with some POC tests. Opportunities lie in technological integration with digital health platforms, development of multiplexed assays capable of detecting multiple pathogens simultaneously, and expansion into underserved markets in developing regions where infectious diseases burden is high but access to diagnostic infrastructure is limited.
COVID-19 has substantially accelerated market expansion, creating unprecedented demand for rapid testing solutions. This pandemic-induced growth has attracted numerous new entrants to the market while prompting established players to expand their infectious disease diagnostic portfolios. The market has witnessed a paradigm shift from traditional laboratory-based testing to decentralized point-of-care testing.
Geographically, North America dominates the market with approximately 40% share, followed by Europe at 30% and Asia-Pacific at 20%. The Asia-Pacific region is expected to witness the highest growth rate due to increasing healthcare expenditure, growing awareness about early disease diagnosis, and improving healthcare infrastructure in countries like China and India.
By pathogen type, bacterial infection diagnostics currently hold the largest market share at 45%, followed by viral infection diagnostics at 35%. However, viral infection diagnostics segment is growing at a faster rate due to the ongoing pandemic and increasing prevalence of viral outbreaks globally.
The market is segmented by technology into immunoassays, molecular diagnostics, microfluidics, and others. Immunoassays currently dominate with 50% market share, but molecular diagnostic POC devices are experiencing the fastest growth due to their higher accuracy and ability to detect pathogens at lower concentrations.
End-user analysis reveals that hospitals and clinics remain the primary users of infectious disease POC diagnostics, accounting for 55% of the market. However, home care settings are emerging as a rapidly growing segment, expected to register a CAGR of 12% during the forecast period, driven by increasing preference for self-testing and remote patient monitoring.
Key market challenges include stringent regulatory requirements, reimbursement issues, and quality concerns with some POC tests. Opportunities lie in technological integration with digital health platforms, development of multiplexed assays capable of detecting multiple pathogens simultaneously, and expansion into underserved markets in developing regions where infectious diseases burden is high but access to diagnostic infrastructure is limited.
Current Challenges in Infectious Disease POC Testing
Despite significant advancements in point-of-care (POC) testing for infectious diseases, several critical challenges continue to impede widespread implementation and optimal performance. One of the most persistent issues is the trade-off between sensitivity and specificity. Many current POC devices struggle to achieve the high sensitivity of laboratory-based molecular methods while maintaining adequate specificity, particularly in resource-limited settings where background contaminants may be prevalent.
Sample preparation remains a significant bottleneck in POC testing workflows. The complex nature of clinical specimens often requires multiple processing steps to isolate pathogens or their biomarkers, which contradicts the simplicity demanded of true POC applications. Current solutions often require trained personnel or additional equipment, limiting deployment in field conditions.
Technical limitations in detection methodologies present another challenge. While nucleic acid amplification techniques offer superior sensitivity, they typically require temperature cycling, precise reagent handling, and contamination control measures that are difficult to implement in portable devices. Immunoassay-based approaches, though simpler, frequently lack the sensitivity needed for early-stage infection detection.
The stability of reagents under varying environmental conditions poses a substantial hurdle for global deployment. Many POC tests require cold chain storage or have limited shelf life in tropical climates, restricting their utility in regions with the highest infectious disease burden. Current stabilization technologies add cost and complexity to device manufacturing.
Integration with data management systems represents an emerging challenge. The value of POC testing is maximized when results can be rapidly communicated to healthcare systems for surveillance and patient management. However, many current devices lack connectivity features or utilize proprietary systems that cannot interface with existing healthcare informatics infrastructure.
Regulatory pathways for POC infectious disease diagnostics remain complex and inconsistent across global markets. Manufacturers face significant barriers in navigating different approval processes, particularly for novel technologies or multiplex assays targeting emerging pathogens. This regulatory burden increases development costs and delays market entry.
Cost-effectiveness continues to be a critical concern, especially for implementation in low-resource settings. While individual test costs have decreased, the total cost of ownership—including quality control, training, and maintenance—often exceeds budgetary constraints of target healthcare systems. Current business models struggle to balance affordability with sustainable manufacturing and distribution.
Sample preparation remains a significant bottleneck in POC testing workflows. The complex nature of clinical specimens often requires multiple processing steps to isolate pathogens or their biomarkers, which contradicts the simplicity demanded of true POC applications. Current solutions often require trained personnel or additional equipment, limiting deployment in field conditions.
Technical limitations in detection methodologies present another challenge. While nucleic acid amplification techniques offer superior sensitivity, they typically require temperature cycling, precise reagent handling, and contamination control measures that are difficult to implement in portable devices. Immunoassay-based approaches, though simpler, frequently lack the sensitivity needed for early-stage infection detection.
The stability of reagents under varying environmental conditions poses a substantial hurdle for global deployment. Many POC tests require cold chain storage or have limited shelf life in tropical climates, restricting their utility in regions with the highest infectious disease burden. Current stabilization technologies add cost and complexity to device manufacturing.
Integration with data management systems represents an emerging challenge. The value of POC testing is maximized when results can be rapidly communicated to healthcare systems for surveillance and patient management. However, many current devices lack connectivity features or utilize proprietary systems that cannot interface with existing healthcare informatics infrastructure.
Regulatory pathways for POC infectious disease diagnostics remain complex and inconsistent across global markets. Manufacturers face significant barriers in navigating different approval processes, particularly for novel technologies or multiplex assays targeting emerging pathogens. This regulatory burden increases development costs and delays market entry.
Cost-effectiveness continues to be a critical concern, especially for implementation in low-resource settings. While individual test costs have decreased, the total cost of ownership—including quality control, training, and maintenance—often exceeds budgetary constraints of target healthcare systems. Current business models struggle to balance affordability with sustainable manufacturing and distribution.
Current POC Solutions for Infectious Disease Detection
01 Diagnostic and monitoring systems for point-of-care applications
Point-of-care diagnostic systems enable rapid testing and monitoring of patient conditions in various healthcare settings. These devices incorporate sensors, analyzers, and data processing capabilities to provide immediate results without requiring laboratory infrastructure. They support clinical decision-making by delivering real-time diagnostic information at the patient's location, improving treatment outcomes and reducing healthcare costs.- Diagnostic and monitoring systems for point-of-care applications: Point-of-care diagnostic systems enable rapid testing and monitoring of patient conditions in various healthcare settings. These systems incorporate sensors, analyzers, and data processing capabilities to provide immediate results without the need for laboratory facilities. They can be used for blood analysis, vital sign monitoring, and detection of specific biomarkers, allowing healthcare providers to make timely clinical decisions.
- Data management and integration for point-of-care devices: Point-of-care devices incorporate sophisticated data management systems that collect, process, and integrate patient information. These systems enable seamless communication between devices and electronic health records, ensuring that test results and patient data are properly documented and accessible to healthcare providers. The integration capabilities support clinical decision-making and improve workflow efficiency in healthcare settings.
- Mobile and portable point-of-care technologies: Mobile and portable point-of-care technologies are designed for use in diverse settings, including remote locations, emergency situations, and home care environments. These compact devices offer functionality comparable to traditional laboratory equipment while being lightweight, battery-operated, and user-friendly. They enable healthcare delivery in resource-limited settings and support telemedicine applications by providing diagnostic capabilities outside of conventional healthcare facilities.
- Healthcare management systems incorporating point-of-care devices: Healthcare management systems integrate point-of-care devices into broader clinical workflows and administrative processes. These systems coordinate patient care, resource allocation, and information flow across healthcare settings. By incorporating point-of-care testing results into comprehensive management platforms, healthcare providers can improve operational efficiency, reduce costs, and enhance patient outcomes through more coordinated and responsive care delivery.
- Novel sensing technologies for point-of-care applications: Advanced sensing technologies enhance the capabilities of point-of-care devices by enabling more accurate, sensitive, and diverse testing options. These innovations include microfluidic systems, biosensors, optical detection methods, and electrochemical sensors that can detect biomarkers, pathogens, and physiological parameters with laboratory-grade precision. The integration of these sensing technologies into portable formats allows for expanded diagnostic capabilities in point-of-care settings.
02 Healthcare data management and integration platforms
Integrated platforms for managing point-of-care device data enable seamless collection, storage, and analysis of patient information. These systems facilitate the integration of diagnostic results with electronic health records, supporting comprehensive patient care. The platforms incorporate security measures to protect sensitive medical information while allowing authorized healthcare providers to access relevant data for informed decision-making.Expand Specific Solutions03 Mobile and portable point-of-care technologies
Mobile point-of-care devices enable healthcare delivery in remote or resource-limited settings. These portable technologies include smartphone-based diagnostic tools, wearable monitors, and compact analyzers that can be easily transported and operated outside traditional healthcare facilities. They extend medical services to underserved populations and support telemedicine applications by enabling remote diagnostics and monitoring.Expand Specific Solutions04 AI and machine learning integration in point-of-care systems
Artificial intelligence and machine learning algorithms enhance the capabilities of point-of-care devices by improving diagnostic accuracy and providing decision support. These technologies analyze complex medical data patterns to assist healthcare providers in interpreting test results and recommending appropriate interventions. The integration of AI enables predictive analytics and personalized medicine approaches at the point of care.Expand Specific Solutions05 Regulatory compliance and quality control for point-of-care devices
Systems and methods for ensuring regulatory compliance and quality control in point-of-care testing environments are essential for maintaining accuracy and reliability. These approaches include automated calibration, performance monitoring, and documentation processes that meet healthcare standards and regulations. They address challenges related to operator training, device maintenance, and result verification to ensure consistent and reliable diagnostic performance.Expand Specific Solutions
Key Industry Players in POC Diagnostics
The point-of-care (POC) diagnostic device market for infectious diseases is currently in a growth phase, with increasing adoption across healthcare settings. The market is projected to expand significantly due to rising demand for rapid, on-site testing solutions. Key players like Becton, Dickinson & Co. and Convatec demonstrate advanced technological maturity in this space, while emerging companies such as Fluxergy and Osler Diagnostics are introducing innovative platforms. Academic institutions including Cornell University and University of Washington are contributing breakthrough research. The technology landscape shows varying degrees of maturity, with established companies offering commercialized solutions while newer entrants focus on novel approaches combining microfluidics, biosensors, and AI integration to enhance diagnostic capabilities and accessibility in resource-limited settings.
Becton, Dickinson & Co.
Technical Solution: Becton, Dickinson & Co. (BD) has developed advanced point-of-care (POC) diagnostic platforms for infectious disease detection, including the BD Veritor™ System and BD MAX™ System. The BD Veritor™ System utilizes digital immunoassay technology to provide rapid results (approximately 15 minutes) for various infectious diseases including influenza, RSV, and SARS-CoV-2. The platform incorporates proprietary optical reading technology that reduces user interpretation errors and improves sensitivity compared to traditional lateral flow assays. BD's MAX™ System employs real-time PCR technology in a modular, scalable format that allows for multiplexed detection of various pathogens from a single sample. The company has also integrated connectivity solutions that enable test results to be automatically transmitted to electronic health records and public health surveillance systems, facilitating improved patient management and epidemiological monitoring.
Strengths: BD's platforms offer high sensitivity and specificity with rapid turnaround times. Their systems feature user-friendly interfaces reducing training requirements and error rates. The connectivity capabilities enhance data management and reporting efficiency. Weaknesses: The equipment requires significant initial capital investment compared to simpler POC tests. Some of their systems require stable power supply and controlled environmental conditions, limiting deployment in resource-constrained settings.
Osler Diagnostics Ltd.
Technical Solution: Osler Diagnostics has developed the Osler Origin™ platform, a revolutionary point-of-care diagnostic system designed to transform infectious disease diagnosis at the point of care. The technology integrates advanced microfluidics, electrochemical sensing, and machine learning algorithms to deliver laboratory-quality results within minutes from a small blood sample. Their proprietary "lab-on-chip" technology miniaturizes complex laboratory processes onto a single disposable cartridge, enabling simultaneous detection of multiple pathogens and biomarkers. The system can identify bacterial, viral, and fungal infections while simultaneously determining antimicrobial susceptibility, addressing the critical need for appropriate antibiotic stewardship. Osler's platform incorporates cloud connectivity for real-time data analysis and remote monitoring capabilities, allowing for integration with healthcare systems and epidemiological surveillance networks. The company has focused on making their technology accessible in diverse healthcare settings, from sophisticated hospitals to resource-limited environments.
Strengths: The platform offers comprehensive multiplex testing capabilities with laboratory-grade accuracy in a portable format. The system provides antimicrobial resistance information, supporting appropriate treatment selection. The technology requires minimal training and maintenance. Weaknesses: As a relatively newer entrant, the platform has less extensive clinical validation data compared to established competitors. The sophisticated technology may result in higher per-test costs compared to simpler diagnostic methods.
Critical Technologies in Rapid Pathogen Detection
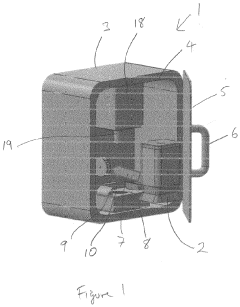
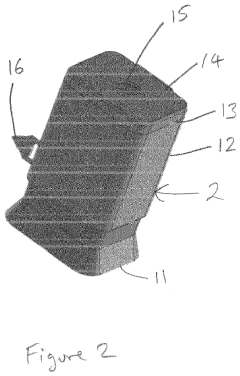
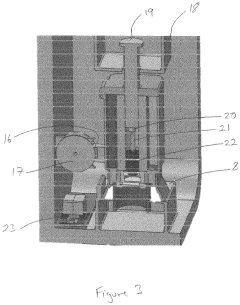
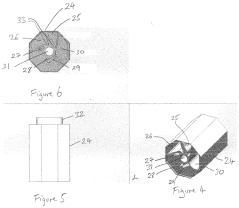
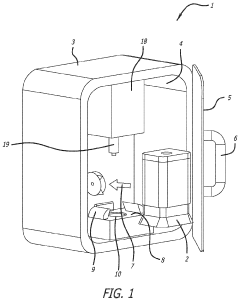
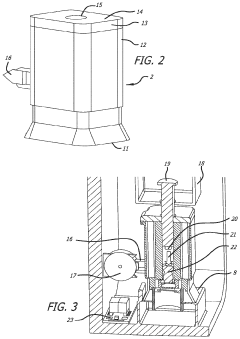
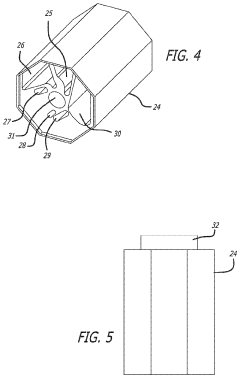
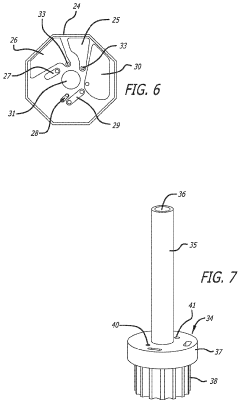
Systems and devices for infectious disease screening
PatentInactiveEP3919175A1
Innovation
- A system utilizing an ultrasonic transducer to lyse cells in a biological sample, coupled with a PCR arrangement and detection mechanism, which includes a frequency control module to optimize ultrasonic frequencies for cell lysis, a heating arrangement for thermal cycling, and a fluorescence detection system for rapid DNA amplification and detection, allowing for rapid result generation within 10 minutes or less.
Systems and devices for infectious disease screening
PatentActiveUS11440012B2
Innovation
- A system incorporating an ultrasonic transducer for cell lysis, a frequency control module to optimize ultrasonic frequencies for efficient DNA release, and a PCR arrangement with real-time fluorescence detection for rapid DNA amplification and detection, enabling rapid PCR processes that can provide results within 10 minutes.
Regulatory Framework for POC Diagnostic Devices
The regulatory landscape for Point-of-Care (POC) diagnostic devices represents a complex framework that varies significantly across global jurisdictions. In the United States, the Food and Drug Administration (FDA) classifies POC diagnostic devices for infectious diseases primarily under Class II or Class III medical devices, requiring either 510(k) clearance or Premarket Approval (PMA). The FDA has established specific guidelines for rapid diagnostic tests, including requirements for analytical validity, clinical validity, and quality system regulations.
The European Union implements the In Vitro Diagnostic Regulation (IVDR 2017/746), which replaced the previous In Vitro Diagnostic Directive (IVDD) with a transition period ending in 2022. This regulation introduces more stringent requirements for clinical evidence, post-market surveillance, and risk classification. POC devices for infectious disease diagnosis typically fall under higher risk categories, necessitating conformity assessment by notified bodies.
In emerging markets, regulatory frameworks often present significant variations. China's National Medical Products Administration (NMPA) has implemented specific pathways for POC diagnostics, while India's Central Drugs Standard Control Organization (CDSCO) continues to evolve its regulatory approach for these technologies. These regional differences create challenges for global manufacturers seeking multi-market approvals.
The COVID-19 pandemic has catalyzed regulatory adaptations worldwide, with many authorities implementing Emergency Use Authorization (EUA) pathways to expedite POC diagnostic device approvals. These temporary measures have demonstrated the potential for accelerated regulatory processes while maintaining essential safety and efficacy standards. The pandemic experience has prompted ongoing discussions about permanent regulatory reforms to balance innovation speed with patient safety.
International harmonization efforts, including the Medical Device Single Audit Program (MDSAP) and the International Medical Device Regulators Forum (IMDRF), aim to streamline regulatory processes across borders. These initiatives seek to establish common standards and reduce duplicative requirements, potentially decreasing time-to-market for innovative POC diagnostic solutions.
Data privacy and cybersecurity regulations increasingly impact POC devices, particularly as connectivity features become standard. Regulations such as GDPR in Europe and HIPAA in the US impose strict requirements on patient data handling, necessitating robust data protection measures in modern POC systems. Manufacturers must navigate these requirements alongside traditional medical device regulations.
Reimbursement pathways represent another critical regulatory consideration, with significant variation in how different healthcare systems evaluate and cover POC diagnostic technologies. The demonstration of both clinical utility and cost-effectiveness has become essential for successful market access and adoption of these technologies in clinical practice.
The European Union implements the In Vitro Diagnostic Regulation (IVDR 2017/746), which replaced the previous In Vitro Diagnostic Directive (IVDD) with a transition period ending in 2022. This regulation introduces more stringent requirements for clinical evidence, post-market surveillance, and risk classification. POC devices for infectious disease diagnosis typically fall under higher risk categories, necessitating conformity assessment by notified bodies.
In emerging markets, regulatory frameworks often present significant variations. China's National Medical Products Administration (NMPA) has implemented specific pathways for POC diagnostics, while India's Central Drugs Standard Control Organization (CDSCO) continues to evolve its regulatory approach for these technologies. These regional differences create challenges for global manufacturers seeking multi-market approvals.
The COVID-19 pandemic has catalyzed regulatory adaptations worldwide, with many authorities implementing Emergency Use Authorization (EUA) pathways to expedite POC diagnostic device approvals. These temporary measures have demonstrated the potential for accelerated regulatory processes while maintaining essential safety and efficacy standards. The pandemic experience has prompted ongoing discussions about permanent regulatory reforms to balance innovation speed with patient safety.
International harmonization efforts, including the Medical Device Single Audit Program (MDSAP) and the International Medical Device Regulators Forum (IMDRF), aim to streamline regulatory processes across borders. These initiatives seek to establish common standards and reduce duplicative requirements, potentially decreasing time-to-market for innovative POC diagnostic solutions.
Data privacy and cybersecurity regulations increasingly impact POC devices, particularly as connectivity features become standard. Regulations such as GDPR in Europe and HIPAA in the US impose strict requirements on patient data handling, necessitating robust data protection measures in modern POC systems. Manufacturers must navigate these requirements alongside traditional medical device regulations.
Reimbursement pathways represent another critical regulatory consideration, with significant variation in how different healthcare systems evaluate and cover POC diagnostic technologies. The demonstration of both clinical utility and cost-effectiveness has become essential for successful market access and adoption of these technologies in clinical practice.
Global Health Impact and Accessibility Considerations
Point-of-care (POC) diagnostic devices for infectious diseases represent a transformative approach to global health management, particularly in resource-limited settings where traditional laboratory infrastructure is scarce. These technologies have demonstrated significant potential to democratize healthcare access across geographical and socioeconomic divides, enabling timely diagnosis and treatment initiation in regions most burdened by infectious disease.
The global health impact of POC devices extends beyond individual patient outcomes to population-level benefits. By facilitating early detection and appropriate treatment, these technologies help reduce transmission rates and contain outbreaks before they escalate to epidemic proportions. This preventive capability is especially crucial for high-burden diseases like tuberculosis, malaria, and HIV, which collectively account for millions of deaths annually in low and middle-income countries (LMICs).
Accessibility considerations for POC devices encompass multiple dimensions beyond mere physical availability. Cost remains a primary barrier, with many advanced diagnostic technologies priced beyond the reach of health systems in LMICs. The total cost of ownership must account for not only the initial device acquisition but also ongoing expenses for consumables, maintenance, and operator training. Sustainable implementation requires business models that align with local economic realities while ensuring consistent supply chains.
Technical accessibility presents another challenge, as many POC devices require specific environmental conditions, stable power supplies, or technical expertise that may be limited in remote settings. Successful deployment necessitates designs that accommodate infrastructure constraints such as intermittent electricity, limited refrigeration, and harsh environmental conditions. The ASSURED criteria (Affordable, Sensitive, Specific, User-friendly, Rapid and robust, Equipment-free, and Deliverable) established by the World Health Organization provide a framework for evaluating POC technologies' suitability for resource-constrained environments.
Cultural and linguistic accessibility factors also influence adoption rates and effective utilization. Diagnostic devices must be designed with consideration for local languages, literacy levels, and cultural perceptions of disease and testing. User interfaces that rely heavily on text instructions may present barriers in regions with low literacy rates, while community stigma around certain diseases may impact willingness to seek diagnosis.
Regulatory pathways represent another accessibility consideration, as lengthy approval processes and divergent requirements across countries can delay the introduction of innovative technologies where they are most needed. Harmonized regulatory frameworks and expedited review processes for essential diagnostics could accelerate deployment in high-burden regions.
Addressing these multifaceted accessibility challenges requires collaborative approaches involving technology developers, public health agencies, funders, and local stakeholders to ensure POC diagnostic innovations translate into meaningful health improvements for vulnerable populations worldwide.
The global health impact of POC devices extends beyond individual patient outcomes to population-level benefits. By facilitating early detection and appropriate treatment, these technologies help reduce transmission rates and contain outbreaks before they escalate to epidemic proportions. This preventive capability is especially crucial for high-burden diseases like tuberculosis, malaria, and HIV, which collectively account for millions of deaths annually in low and middle-income countries (LMICs).
Accessibility considerations for POC devices encompass multiple dimensions beyond mere physical availability. Cost remains a primary barrier, with many advanced diagnostic technologies priced beyond the reach of health systems in LMICs. The total cost of ownership must account for not only the initial device acquisition but also ongoing expenses for consumables, maintenance, and operator training. Sustainable implementation requires business models that align with local economic realities while ensuring consistent supply chains.
Technical accessibility presents another challenge, as many POC devices require specific environmental conditions, stable power supplies, or technical expertise that may be limited in remote settings. Successful deployment necessitates designs that accommodate infrastructure constraints such as intermittent electricity, limited refrigeration, and harsh environmental conditions. The ASSURED criteria (Affordable, Sensitive, Specific, User-friendly, Rapid and robust, Equipment-free, and Deliverable) established by the World Health Organization provide a framework for evaluating POC technologies' suitability for resource-constrained environments.
Cultural and linguistic accessibility factors also influence adoption rates and effective utilization. Diagnostic devices must be designed with consideration for local languages, literacy levels, and cultural perceptions of disease and testing. User interfaces that rely heavily on text instructions may present barriers in regions with low literacy rates, while community stigma around certain diseases may impact willingness to seek diagnosis.
Regulatory pathways represent another accessibility consideration, as lengthy approval processes and divergent requirements across countries can delay the introduction of innovative technologies where they are most needed. Harmonized regulatory frameworks and expedited review processes for essential diagnostics could accelerate deployment in high-burden regions.
Addressing these multifaceted accessibility challenges requires collaborative approaches involving technology developers, public health agencies, funders, and local stakeholders to ensure POC diagnostic innovations translate into meaningful health improvements for vulnerable populations worldwide.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!