How Point-of-care Devices Address Global Health Challenges
SEP 19, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Point-of-care Technology Evolution and Objectives
Point-of-care (POC) testing has evolved significantly over the past several decades, transforming from rudimentary diagnostic tools to sophisticated, integrated systems capable of delivering laboratory-quality results in diverse settings. The evolution began in the 1960s with simple glucose testing strips, progressing through the 1980s with the introduction of handheld blood analyzers, and accelerating in the 2000s with molecular diagnostic capabilities and smartphone integration.
The technological trajectory has been shaped by miniaturization advances in microfluidics, biosensors, and microelectronics, enabling increasingly complex diagnostic procedures to be performed on smaller, more portable platforms. Recent developments in nanotechnology and materials science have further enhanced sensitivity and specificity while reducing sample volume requirements and time-to-result metrics.
A pivotal shift occurred with the integration of digital connectivity, allowing POC devices to transmit results to healthcare information systems, facilitating remote monitoring and telehealth applications. This connectivity represents a fundamental advancement in addressing global health challenges by extending diagnostic capabilities to underserved regions while maintaining links to broader healthcare networks.
The primary objective of modern POC technology development is to democratize access to diagnostic testing across geographic, economic, and infrastructural barriers. This includes creating robust devices capable of operating in resource-limited settings with minimal infrastructure requirements, addressing the diagnostic gap that affects approximately 47% of the global population with limited access to basic laboratory services.
Technical objectives focus on developing multiplex testing capabilities that can simultaneously detect multiple conditions from a single sample, crucial for addressing comorbidities common in many global health challenges. Equally important is the pursuit of increased sensitivity and specificity to ensure accurate diagnosis of conditions at early stages when intervention is most effective.
Cost-effectiveness represents another critical objective, with efforts directed toward reducing both device and per-test costs to enable sustainable implementation in low-resource settings. This includes innovations in manufacturing processes and materials selection to optimize production economics while maintaining performance standards.
The evolution trajectory aims toward creating integrated diagnostic ecosystems that combine testing with treatment guidance and follow-up capabilities, transforming POC devices from isolated diagnostic tools into comprehensive healthcare management platforms. This holistic approach aligns with global health initiatives seeking to strengthen healthcare systems rather than implementing isolated technological solutions.
The technological trajectory has been shaped by miniaturization advances in microfluidics, biosensors, and microelectronics, enabling increasingly complex diagnostic procedures to be performed on smaller, more portable platforms. Recent developments in nanotechnology and materials science have further enhanced sensitivity and specificity while reducing sample volume requirements and time-to-result metrics.
A pivotal shift occurred with the integration of digital connectivity, allowing POC devices to transmit results to healthcare information systems, facilitating remote monitoring and telehealth applications. This connectivity represents a fundamental advancement in addressing global health challenges by extending diagnostic capabilities to underserved regions while maintaining links to broader healthcare networks.
The primary objective of modern POC technology development is to democratize access to diagnostic testing across geographic, economic, and infrastructural barriers. This includes creating robust devices capable of operating in resource-limited settings with minimal infrastructure requirements, addressing the diagnostic gap that affects approximately 47% of the global population with limited access to basic laboratory services.
Technical objectives focus on developing multiplex testing capabilities that can simultaneously detect multiple conditions from a single sample, crucial for addressing comorbidities common in many global health challenges. Equally important is the pursuit of increased sensitivity and specificity to ensure accurate diagnosis of conditions at early stages when intervention is most effective.
Cost-effectiveness represents another critical objective, with efforts directed toward reducing both device and per-test costs to enable sustainable implementation in low-resource settings. This includes innovations in manufacturing processes and materials selection to optimize production economics while maintaining performance standards.
The evolution trajectory aims toward creating integrated diagnostic ecosystems that combine testing with treatment guidance and follow-up capabilities, transforming POC devices from isolated diagnostic tools into comprehensive healthcare management platforms. This holistic approach aligns with global health initiatives seeking to strengthen healthcare systems rather than implementing isolated technological solutions.
Global Health Market Needs Analysis
The global health landscape faces unprecedented challenges, with disparities in healthcare access affecting billions worldwide. Point-of-care (POC) testing devices have emerged as critical tools to address these inequities, particularly in resource-limited settings where traditional healthcare infrastructure is inadequate. Market analysis reveals that approximately 3.8 billion people lack access to essential health services, creating substantial demand for decentralized diagnostic solutions that can function effectively outside conventional clinical environments.
The POC diagnostics market is experiencing robust growth, valued at $29.7 billion in 2022 and projected to reach $51.4 billion by 2027, representing a compound annual growth rate of 11.6%. This expansion is driven primarily by the increasing prevalence of infectious diseases in low and middle-income countries (LMICs), where traditional laboratory infrastructure remains insufficient to meet population needs.
Infectious disease diagnostics constitute the largest segment within the POC market, accounting for 37% of global demand. This is particularly relevant in sub-Saharan Africa and South Asia, where diseases like HIV, tuberculosis, and malaria continue to pose significant public health challenges. The COVID-19 pandemic has further accelerated market growth, highlighting the critical importance of rapid, accessible diagnostic capabilities during global health emergencies.
Demographic trends are also shaping market dynamics, with aging populations in developed economies driving demand for chronic disease management tools. Simultaneously, high birth rates in developing regions necessitate maternal and child health solutions that can function in low-resource settings. These divergent needs create distinct market segments with different technological requirements and price sensitivities.
Healthcare expenditure patterns reveal significant regional variations that impact market potential. While North America and Europe account for 67% of global healthcare spending, they represent only 25% of the global disease burden. Conversely, Africa bears 25% of the global disease burden while accounting for just 1% of healthcare expenditure, underscoring the need for cost-effective POC solutions tailored to economic realities in these regions.
Regulatory environments and reimbursement policies significantly influence market adoption rates. Countries with streamlined approval pathways for essential diagnostics show faster uptake of POC technologies. The World Health Organization's Essential Diagnostics List has become an important market driver, providing guidance for national health systems on priority diagnostic tools and creating more predictable demand for manufacturers.
AI and mobile connectivity are transforming user expectations, with growing demand for POC devices that integrate with digital health ecosystems. This trend is particularly pronounced in regions with high mobile penetration but limited healthcare infrastructure, creating opportunities for innovative business models that leverage existing telecommunications networks to extend diagnostic reach.
The POC diagnostics market is experiencing robust growth, valued at $29.7 billion in 2022 and projected to reach $51.4 billion by 2027, representing a compound annual growth rate of 11.6%. This expansion is driven primarily by the increasing prevalence of infectious diseases in low and middle-income countries (LMICs), where traditional laboratory infrastructure remains insufficient to meet population needs.
Infectious disease diagnostics constitute the largest segment within the POC market, accounting for 37% of global demand. This is particularly relevant in sub-Saharan Africa and South Asia, where diseases like HIV, tuberculosis, and malaria continue to pose significant public health challenges. The COVID-19 pandemic has further accelerated market growth, highlighting the critical importance of rapid, accessible diagnostic capabilities during global health emergencies.
Demographic trends are also shaping market dynamics, with aging populations in developed economies driving demand for chronic disease management tools. Simultaneously, high birth rates in developing regions necessitate maternal and child health solutions that can function in low-resource settings. These divergent needs create distinct market segments with different technological requirements and price sensitivities.
Healthcare expenditure patterns reveal significant regional variations that impact market potential. While North America and Europe account for 67% of global healthcare spending, they represent only 25% of the global disease burden. Conversely, Africa bears 25% of the global disease burden while accounting for just 1% of healthcare expenditure, underscoring the need for cost-effective POC solutions tailored to economic realities in these regions.
Regulatory environments and reimbursement policies significantly influence market adoption rates. Countries with streamlined approval pathways for essential diagnostics show faster uptake of POC technologies. The World Health Organization's Essential Diagnostics List has become an important market driver, providing guidance for national health systems on priority diagnostic tools and creating more predictable demand for manufacturers.
AI and mobile connectivity are transforming user expectations, with growing demand for POC devices that integrate with digital health ecosystems. This trend is particularly pronounced in regions with high mobile penetration but limited healthcare infrastructure, creating opportunities for innovative business models that leverage existing telecommunications networks to extend diagnostic reach.
Current POC Diagnostic Capabilities and Barriers
Point-of-care (POC) diagnostic technologies have evolved significantly over the past decade, offering capabilities that range from basic lateral flow assays to sophisticated molecular diagnostics. Current POC devices can detect infectious diseases such as malaria, HIV, tuberculosis, and more recently COVID-19 with varying degrees of sensitivity and specificity. Many modern POC platforms utilize immunoassay techniques, nucleic acid amplification tests (NAATs), and microfluidic technologies to deliver results within minutes to hours, compared to traditional laboratory testing that may take days.
Despite these advancements, significant barriers persist in the widespread implementation of POC diagnostics, particularly in resource-limited settings. Technical challenges include limited sensitivity for certain conditions, especially at early disease stages when pathogen loads are low. Many POC tests still struggle to match the gold standard laboratory-based methods in terms of accuracy and reliability, creating hesitancy among healthcare providers to rely solely on POC results for critical clinical decisions.
Infrastructure limitations represent another major barrier, with many POC devices requiring stable electricity, temperature-controlled environments, or clean water—resources often unavailable in remote or underserved areas. Even "simple" lateral flow tests may require proper storage conditions to maintain reagent stability and test performance, conditions that cannot be guaranteed in many global health settings.
Cost remains a persistent obstacle, with many advanced POC platforms being prohibitively expensive for widespread deployment in low- and middle-income countries (LMICs). While the per-test cost may be reasonable, the initial capital investment for equipment often exceeds available budgets. Additionally, ongoing costs for quality control, maintenance, and consumables are frequently overlooked in implementation planning.
Regulatory and quality assurance frameworks present further challenges. Many countries lack robust regulatory systems for evaluating and approving POC diagnostics, leading to market penetration of substandard products. The absence of standardized quality control measures and external quality assessment programs undermines confidence in test results and hampers adoption.
Human resource constraints also limit POC implementation, as effective use requires trained personnel who understand proper sample collection, test procedures, result interpretation, and quality control measures. The shortage of healthcare workers in many regions, coupled with limited training opportunities, creates bottlenecks in POC testing programs.
Integration with existing healthcare systems presents another barrier, as many POC technologies operate in isolation rather than connecting with laboratory information systems or electronic health records. This disconnection limits the utility of test results for patient management, epidemiological surveillance, and health system planning.
Despite these advancements, significant barriers persist in the widespread implementation of POC diagnostics, particularly in resource-limited settings. Technical challenges include limited sensitivity for certain conditions, especially at early disease stages when pathogen loads are low. Many POC tests still struggle to match the gold standard laboratory-based methods in terms of accuracy and reliability, creating hesitancy among healthcare providers to rely solely on POC results for critical clinical decisions.
Infrastructure limitations represent another major barrier, with many POC devices requiring stable electricity, temperature-controlled environments, or clean water—resources often unavailable in remote or underserved areas. Even "simple" lateral flow tests may require proper storage conditions to maintain reagent stability and test performance, conditions that cannot be guaranteed in many global health settings.
Cost remains a persistent obstacle, with many advanced POC platforms being prohibitively expensive for widespread deployment in low- and middle-income countries (LMICs). While the per-test cost may be reasonable, the initial capital investment for equipment often exceeds available budgets. Additionally, ongoing costs for quality control, maintenance, and consumables are frequently overlooked in implementation planning.
Regulatory and quality assurance frameworks present further challenges. Many countries lack robust regulatory systems for evaluating and approving POC diagnostics, leading to market penetration of substandard products. The absence of standardized quality control measures and external quality assessment programs undermines confidence in test results and hampers adoption.
Human resource constraints also limit POC implementation, as effective use requires trained personnel who understand proper sample collection, test procedures, result interpretation, and quality control measures. The shortage of healthcare workers in many regions, coupled with limited training opportunities, creates bottlenecks in POC testing programs.
Integration with existing healthcare systems presents another barrier, as many POC technologies operate in isolation rather than connecting with laboratory information systems or electronic health records. This disconnection limits the utility of test results for patient management, epidemiological surveillance, and health system planning.
Existing POC Solutions for Resource-Limited Settings
01 Diagnostic and monitoring systems for point-of-care applications
Point-of-care diagnostic systems enable rapid testing and monitoring of patient conditions in various healthcare settings. These devices incorporate sensors, analyzers, and data processing capabilities to provide immediate results without requiring laboratory infrastructure. They support various testing methodologies including blood analysis, vital signs monitoring, and disease-specific diagnostics, allowing healthcare providers to make timely clinical decisions at the patient's location.- Diagnostic and monitoring systems for point-of-care applications: Point-of-care diagnostic systems enable rapid testing and monitoring of patient conditions in various healthcare settings. These systems incorporate sensors, analyzers, and data processing capabilities to provide immediate results without requiring laboratory facilities. They can detect biomarkers, measure vital signs, and analyze biological samples, allowing healthcare providers to make timely clinical decisions at the patient's location.
- Healthcare data management and integration platforms: These platforms facilitate the collection, storage, and analysis of patient data from point-of-care devices. They integrate with electronic health records (EHR) systems and enable secure data sharing between healthcare providers. The platforms support clinical decision-making by providing access to patient information, treatment guidelines, and diagnostic tools at the point of care, improving coordination and continuity of care.
- Mobile and portable point-of-care technologies: Mobile point-of-care technologies leverage smartphones, tablets, and portable devices to deliver healthcare services outside traditional clinical settings. These solutions include wearable sensors, handheld diagnostic tools, and mobile applications that enable remote monitoring, telemedicine consultations, and home-based care. They enhance accessibility to healthcare services, particularly in remote or underserved areas, and support patient self-management.
- Point-of-care testing for infectious diseases and emergency situations: Specialized point-of-care devices designed for rapid detection of infectious agents and emergency medical conditions. These systems provide quick results for time-sensitive conditions, enabling immediate treatment decisions. They incorporate technologies such as immunoassays, molecular diagnostics, and microfluidics to detect pathogens, biomarkers, and critical health parameters in emergency departments, field hospitals, and disaster response scenarios.
- AI and machine learning integration in point-of-care systems: Integration of artificial intelligence and machine learning algorithms into point-of-care devices enhances diagnostic accuracy and clinical decision support. These technologies analyze complex medical data, identify patterns, and generate predictive insights to assist healthcare providers. AI-powered point-of-care systems can interpret diagnostic images, recommend treatment options, and identify high-risk patients, improving efficiency and reducing diagnostic errors at the point of care.
02 Healthcare data management and integration platforms
These platforms facilitate the collection, storage, and integration of patient data from point-of-care devices into healthcare information systems. They enable seamless data flow between diagnostic devices and electronic health records, supporting clinical decision-making and care coordination. These systems incorporate security features to protect sensitive patient information while allowing authorized healthcare providers to access relevant data across different care settings.Expand Specific Solutions03 Mobile and portable point-of-care technologies
Mobile point-of-care technologies leverage portable devices and wireless connectivity to extend healthcare delivery beyond traditional settings. These solutions include smartphone-compatible diagnostic tools, wearable monitors, and portable analyzers that can be used in remote locations, home care settings, or during emergency responses. The mobility of these devices enables healthcare providers to deliver services in underserved areas and supports telemedicine applications.Expand Specific Solutions04 AI and machine learning integration in point-of-care systems
Artificial intelligence and machine learning technologies are being integrated into point-of-care devices to enhance diagnostic accuracy and provide decision support. These systems can analyze complex medical data, identify patterns, and suggest potential diagnoses or treatment options. The AI components can learn from new data, continuously improving their performance and adapting to different patient populations and clinical scenarios.Expand Specific Solutions05 Patient-centered point-of-care solutions
Patient-centered point-of-care solutions focus on improving the patient experience while delivering effective care. These technologies include user-friendly interfaces, personalized testing protocols, and systems designed for self-administration. They empower patients to participate in their own healthcare management through features like simplified operation, clear result interpretation, and integration with personal health tracking applications.Expand Specific Solutions
Leading POC Device Manufacturers and Startups
Point-of-care (POC) devices are revolutionizing global healthcare by addressing accessibility challenges in resource-limited settings. The market is in a growth phase, with an estimated value exceeding $30 billion and projected annual growth of 7-10%. Major players like Abbott Point of Care, Roche, and Siemens Healthineers lead with established technologies, while innovative companies such as T2 Biosystems, Hemex Health, and iAssay are developing next-generation solutions. Academic institutions including Brigham & Women's Hospital and Cornell University contribute significant research. The technology is maturing rapidly, with advancements in miniaturization, connectivity, and AI integration driving adoption across diverse healthcare settings, from remote clinics to emergency response scenarios.
Abbott Point of Care, Inc.
Technical Solution: Abbott Point of Care has developed the i-STAT system, a handheld blood analyzer that provides real-time, lab-quality results within minutes at the patient's bedside. The device uses cartridge-based technology with microfluidics and biosensor technology to perform multiple tests from a single blood sample. Their platform can test for blood gases, electrolytes, cardiac markers, and other critical care parameters. The i-STAT system has been deployed in over 50 countries and has been particularly impactful in resource-limited settings where laboratory infrastructure is lacking. Abbott has also developed the ID NOW platform for rapid molecular testing, which can detect infectious diseases like COVID-19, influenza, and strep A in under 15 minutes, enabling immediate treatment decisions in remote locations. Their NAVICA mobile app pairs with these devices to help manage and share test results, enhancing disease surveillance capabilities in global health contexts.
Strengths: Provides laboratory-quality results in minutes rather than hours or days; highly portable and battery-operated for use in remote settings; requires minimal training for healthcare workers; comprehensive test menu addressing multiple health conditions. Weaknesses: Initial device cost may be prohibitive for some low-resource settings; ongoing need for proprietary test cartridges creates supply chain dependencies; some tests still require refrigeration of reagents.
Hemex Health, Inc.
Technical Solution: Hemex Health has developed the Gazelle platform, a portable diagnostic device specifically designed to address neglected tropical diseases and hematological disorders in resource-limited settings. The system combines microfluidics and miniaturized electrochemical detection to diagnose malaria and sickle cell disease at the point of care within minutes, using only a drop of blood. Their technology employs magneto-optical detection for malaria parasites and hemoglobin electrophoresis for sickle cell diagnosis, both integrated into a single, battery-operated device that can function in challenging environmental conditions. The Gazelle platform features a touchscreen interface with simplified workflows requiring minimal training, making it accessible to community health workers. Their cloud-based data management system enables remote monitoring of disease prevalence and treatment outcomes, supporting public health surveillance in regions with limited infrastructure. Hemex has implemented a sustainable business model with tiered pricing based on country income levels, ensuring accessibility while maintaining operational viability. The company has established partnerships with local organizations in Africa and South Asia to ensure appropriate implementation and support of their technology in high-burden regions.
Strengths: Purpose-built for neglected diseases that disproportionately affect low-resource regions; extremely portable and durable design suitable for field use; low cost per test compared to traditional laboratory methods; minimal training requirements for operators. Weaknesses: More limited test menu compared to larger diagnostic companies; smaller global support network may affect maintenance and repair capabilities; early-stage company with less established supply chains compared to multinational corporations.
Key Innovations in Rapid Diagnostic Technologies
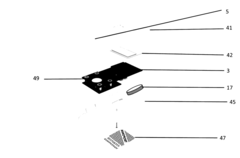
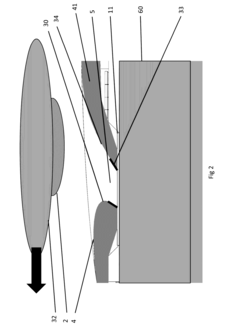
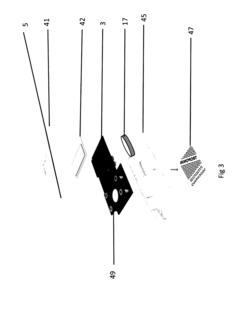
Industrial design of stand-alone assay system
PatentInactiveUS20170102378A1
Innovation
- A stand-alone assay system using magnetic particles as assay labels that react with target analytes, allowing for rapid sample preparation through a simple finger swipe mechanism, integrating a membrane filter and capillary system for unprocessed sample analysis, and enabling wireless result transmission, reducing the need for external components and minimizing biological contamination risks.
A device to measure vital parameters for remote diagnostics
PatentInactiveIN202221072417A
Innovation
- A portable, non-invasive single-point health care device that measures vital parameters like ECG, Heart Rate, SpO2, PPG, and Blood Pressure, using a camera for visual assessments, connected via a mobile app for real-time data collection and analysis, enabling first-hand diagnosis by medical professionals.
Regulatory Frameworks for POC Medical Devices
The regulatory landscape for Point-of-Care (POC) medical devices varies significantly across global regions, creating a complex environment for manufacturers and healthcare providers. In the United States, the Food and Drug Administration (FDA) classifies POC devices into three risk categories, with Class I devices facing minimal regulation while Class III devices undergo rigorous premarket approval processes. The FDA's recent Digital Health Innovation Action Plan has created pathways for expedited review of certain POC technologies, particularly those addressing public health emergencies.
The European Union implements the Medical Device Regulation (MDR) and In Vitro Diagnostic Regulation (IVDR), which enforce stricter requirements for clinical evidence, post-market surveillance, and unique device identification compared to previous directives. These regulations have significantly impacted POC device development timelines and costs, though they aim to enhance patient safety and device effectiveness.
Low and middle-income countries (LMICs) face distinct regulatory challenges, often lacking robust frameworks specifically designed for POC technologies. The World Health Organization's Prequalification of In Vitro Diagnostics program has become a critical pathway for ensuring quality POC diagnostics in these regions, serving as a reference point for national regulatory bodies with limited resources.
Harmonization efforts, such as the International Medical Device Regulators Forum (IMDRF), are working to align regulatory approaches globally. Their Medical Device Single Audit Program (MDSAP) allows manufacturers to undergo a single audit acceptable across multiple jurisdictions, reducing redundant inspections and accelerating market access.
Emerging regulatory considerations for POC devices include data privacy and cybersecurity requirements, particularly for connected devices that transmit patient information. The FDA's guidance on cybersecurity for medical devices and the EU's General Data Protection Regulation (GDPR) have established frameworks that manufacturers must navigate when developing networked POC solutions.
Regulatory pathways for emergency use authorization have gained prominence following the COVID-19 pandemic, with many jurisdictions implementing accelerated review processes for POC diagnostics addressing public health emergencies. These mechanisms balance the need for rapid deployment against safety considerations, often requiring robust post-market surveillance.
The regulatory burden remains a significant barrier to POC innovation, particularly for startups and smaller companies. Collaborative regulatory science initiatives between industry, academia, and regulatory bodies are emerging to develop evidence-based approaches that maintain safety standards while enabling technological advancement in this critical healthcare sector.
The European Union implements the Medical Device Regulation (MDR) and In Vitro Diagnostic Regulation (IVDR), which enforce stricter requirements for clinical evidence, post-market surveillance, and unique device identification compared to previous directives. These regulations have significantly impacted POC device development timelines and costs, though they aim to enhance patient safety and device effectiveness.
Low and middle-income countries (LMICs) face distinct regulatory challenges, often lacking robust frameworks specifically designed for POC technologies. The World Health Organization's Prequalification of In Vitro Diagnostics program has become a critical pathway for ensuring quality POC diagnostics in these regions, serving as a reference point for national regulatory bodies with limited resources.
Harmonization efforts, such as the International Medical Device Regulators Forum (IMDRF), are working to align regulatory approaches globally. Their Medical Device Single Audit Program (MDSAP) allows manufacturers to undergo a single audit acceptable across multiple jurisdictions, reducing redundant inspections and accelerating market access.
Emerging regulatory considerations for POC devices include data privacy and cybersecurity requirements, particularly for connected devices that transmit patient information. The FDA's guidance on cybersecurity for medical devices and the EU's General Data Protection Regulation (GDPR) have established frameworks that manufacturers must navigate when developing networked POC solutions.
Regulatory pathways for emergency use authorization have gained prominence following the COVID-19 pandemic, with many jurisdictions implementing accelerated review processes for POC diagnostics addressing public health emergencies. These mechanisms balance the need for rapid deployment against safety considerations, often requiring robust post-market surveillance.
The regulatory burden remains a significant barrier to POC innovation, particularly for startups and smaller companies. Collaborative regulatory science initiatives between industry, academia, and regulatory bodies are emerging to develop evidence-based approaches that maintain safety standards while enabling technological advancement in this critical healthcare sector.
Cost-Effectiveness and Accessibility Considerations
Cost-effectiveness represents a critical factor in the widespread adoption of point-of-care (POC) devices for addressing global health challenges. Traditional laboratory testing often involves substantial infrastructure costs, specialized personnel, and expensive equipment, creating significant barriers to healthcare access in resource-limited settings. POC devices offer a compelling alternative by dramatically reducing per-test costs through simplified workflows and elimination of complex laboratory infrastructure requirements.
Economic analyses demonstrate that POC testing can reduce overall healthcare expenditures by enabling earlier diagnosis and treatment, thereby preventing disease progression to more costly advanced stages. For example, rapid HIV testing at the point of care has shown cost savings of 27-33% compared to conventional laboratory testing when accounting for comprehensive healthcare system costs and patient outcomes.
Accessibility considerations extend beyond mere affordability to encompass geographical, cultural, and infrastructural dimensions. POC devices designed for low-resource settings incorporate features that address these multifaceted accessibility challenges. Battery operation with low power consumption accommodates unreliable electricity supplies, while ruggedized designs withstand harsh environmental conditions including extreme temperatures, humidity, and dust exposure.
User interface simplification represents another crucial accessibility enhancement, with intuitive operation requiring minimal training and multilingual interfaces overcoming language barriers. These design considerations enable effective deployment even in settings with limited healthcare workforce capacity or technical expertise.
Supply chain optimization further enhances accessibility through extended reagent shelf-life at ambient temperatures, reducing cold chain dependencies that often fail in remote locations. Modular designs allowing for field maintenance and calibration minimize downtime and dependence on specialized technical support.
The economic sustainability of POC implementation requires consideration of total cost of ownership beyond initial device acquisition. This includes ongoing costs for consumables, maintenance, quality control, and operator training. Successful implementation models often incorporate innovative financing mechanisms such as volume-based pricing, public-private partnerships, and technology transfer arrangements to ensure long-term affordability.
Recent technological innovations are progressively driving down costs while improving performance, with smartphone-integrated diagnostics and paper-based microfluidic platforms emerging as particularly promising approaches for ultra-low-cost testing solutions that maintain clinical utility in challenging environments.
Economic analyses demonstrate that POC testing can reduce overall healthcare expenditures by enabling earlier diagnosis and treatment, thereby preventing disease progression to more costly advanced stages. For example, rapid HIV testing at the point of care has shown cost savings of 27-33% compared to conventional laboratory testing when accounting for comprehensive healthcare system costs and patient outcomes.
Accessibility considerations extend beyond mere affordability to encompass geographical, cultural, and infrastructural dimensions. POC devices designed for low-resource settings incorporate features that address these multifaceted accessibility challenges. Battery operation with low power consumption accommodates unreliable electricity supplies, while ruggedized designs withstand harsh environmental conditions including extreme temperatures, humidity, and dust exposure.
User interface simplification represents another crucial accessibility enhancement, with intuitive operation requiring minimal training and multilingual interfaces overcoming language barriers. These design considerations enable effective deployment even in settings with limited healthcare workforce capacity or technical expertise.
Supply chain optimization further enhances accessibility through extended reagent shelf-life at ambient temperatures, reducing cold chain dependencies that often fail in remote locations. Modular designs allowing for field maintenance and calibration minimize downtime and dependence on specialized technical support.
The economic sustainability of POC implementation requires consideration of total cost of ownership beyond initial device acquisition. This includes ongoing costs for consumables, maintenance, quality control, and operator training. Successful implementation models often incorporate innovative financing mechanisms such as volume-based pricing, public-private partnerships, and technology transfer arrangements to ensure long-term affordability.
Recent technological innovations are progressively driving down costs while improving performance, with smartphone-integrated diagnostics and paper-based microfluidic platforms emerging as particularly promising approaches for ultra-low-cost testing solutions that maintain clinical utility in challenging environments.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!