Neuromorphic Chips in Healthcare: Low-Power Wearable Monitoring and On-Device Alerts
AUG 20, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Neuromorphic Chips in Healthcare: Background and Objectives
Neuromorphic computing represents a paradigm shift in the field of artificial intelligence and computing, drawing inspiration from the structure and function of biological neural networks. In the context of healthcare, particularly in the realm of wearable monitoring and on-device alerts, neuromorphic chips offer unprecedented potential for low-power, high-efficiency data processing and analysis.
The evolution of neuromorphic technology can be traced back to the 1980s, with pioneering work by Carver Mead. However, it is only in recent years that significant advancements have been made, driven by the increasing demand for energy-efficient computing solutions in various domains, including healthcare.
The primary objective of integrating neuromorphic chips into healthcare wearables is to enable continuous, real-time monitoring of vital signs and physiological parameters while minimizing power consumption. This approach aims to overcome the limitations of traditional computing architectures, which often struggle with the energy demands of constant data processing and transmission in portable devices.
By mimicking the brain's neural networks, neuromorphic chips can process sensory data more efficiently, allowing for rapid pattern recognition and anomaly detection. This capability is crucial for generating timely alerts in response to changes in a patient's condition, potentially saving lives in critical situations.
Another key goal is to enhance the autonomy of wearable healthcare devices. By performing complex computations directly on the device, neuromorphic chips reduce the need for constant communication with external servers, thereby improving privacy and reducing latency in decision-making processes.
The development of neuromorphic chips for healthcare applications also aligns with the broader trend towards edge computing in the Internet of Things (IoT) ecosystem. This shift aims to bring computation closer to the data source, reducing bandwidth requirements and enhancing overall system responsiveness.
As we look towards the future, the objectives for neuromorphic chips in healthcare extend beyond mere monitoring. There is a growing interest in developing adaptive systems that can learn from individual patient data, potentially leading to personalized healthcare solutions that evolve with the user's needs over time.
In conclusion, the background and objectives of neuromorphic chips in healthcare, particularly for low-power wearable monitoring and on-device alerts, reflect a convergence of technological innovation and healthcare needs. The pursuit of energy-efficient, intelligent, and autonomous wearable devices promises to revolutionize patient care, enabling more proactive and personalized health management strategies.
The evolution of neuromorphic technology can be traced back to the 1980s, with pioneering work by Carver Mead. However, it is only in recent years that significant advancements have been made, driven by the increasing demand for energy-efficient computing solutions in various domains, including healthcare.
The primary objective of integrating neuromorphic chips into healthcare wearables is to enable continuous, real-time monitoring of vital signs and physiological parameters while minimizing power consumption. This approach aims to overcome the limitations of traditional computing architectures, which often struggle with the energy demands of constant data processing and transmission in portable devices.
By mimicking the brain's neural networks, neuromorphic chips can process sensory data more efficiently, allowing for rapid pattern recognition and anomaly detection. This capability is crucial for generating timely alerts in response to changes in a patient's condition, potentially saving lives in critical situations.
Another key goal is to enhance the autonomy of wearable healthcare devices. By performing complex computations directly on the device, neuromorphic chips reduce the need for constant communication with external servers, thereby improving privacy and reducing latency in decision-making processes.
The development of neuromorphic chips for healthcare applications also aligns with the broader trend towards edge computing in the Internet of Things (IoT) ecosystem. This shift aims to bring computation closer to the data source, reducing bandwidth requirements and enhancing overall system responsiveness.
As we look towards the future, the objectives for neuromorphic chips in healthcare extend beyond mere monitoring. There is a growing interest in developing adaptive systems that can learn from individual patient data, potentially leading to personalized healthcare solutions that evolve with the user's needs over time.
In conclusion, the background and objectives of neuromorphic chips in healthcare, particularly for low-power wearable monitoring and on-device alerts, reflect a convergence of technological innovation and healthcare needs. The pursuit of energy-efficient, intelligent, and autonomous wearable devices promises to revolutionize patient care, enabling more proactive and personalized health management strategies.
Market Demand for Low-Power Wearable Health Monitoring
The market demand for low-power wearable health monitoring devices has been experiencing significant growth in recent years, driven by several key factors. The aging global population, coupled with the increasing prevalence of chronic diseases, has created a pressing need for continuous health monitoring solutions that can provide real-time data and early warning signs of potential health issues.
Consumers are becoming increasingly health-conscious and are seeking ways to proactively manage their well-being. This trend has led to a surge in demand for wearable devices that can track various health metrics such as heart rate, blood pressure, oxygen saturation, and physical activity levels. The convenience and non-invasive nature of these devices make them particularly attractive to users who want to monitor their health without disrupting their daily routines.
The healthcare industry is also recognizing the potential of wearable health monitoring devices to improve patient care and reduce healthcare costs. Remote patient monitoring systems, enabled by low-power wearable devices, allow healthcare providers to track patients' vital signs and health status outside of traditional clinical settings. This capability is particularly valuable for managing chronic conditions, post-operative care, and elderly care, as it can help prevent hospital readmissions and enable early interventions.
The COVID-19 pandemic has further accelerated the adoption of wearable health monitoring devices. The need for remote health monitoring and the desire to track potential symptoms have led to increased interest in devices that can measure body temperature, respiratory rate, and other relevant health indicators.
Market research indicates that the global wearable medical devices market is expected to grow substantially in the coming years. Factors contributing to this growth include technological advancements in sensor technology, miniaturization of components, and improvements in battery life and power efficiency. The integration of artificial intelligence and machine learning algorithms into these devices is also enhancing their capabilities, allowing for more accurate health predictions and personalized insights.
However, challenges remain in the widespread adoption of low-power wearable health monitoring devices. Concerns about data privacy and security, as well as the accuracy and reliability of measurements, need to be addressed to gain consumer trust. Additionally, regulatory approval processes for medical-grade wearable devices can be lengthy and complex, potentially slowing market entry for some innovative products.
Despite these challenges, the market demand for low-power wearable health monitoring devices remains strong and is expected to continue growing. As technology advances and consumer awareness increases, these devices are poised to play an increasingly important role in preventive healthcare and personalized medicine.
Consumers are becoming increasingly health-conscious and are seeking ways to proactively manage their well-being. This trend has led to a surge in demand for wearable devices that can track various health metrics such as heart rate, blood pressure, oxygen saturation, and physical activity levels. The convenience and non-invasive nature of these devices make them particularly attractive to users who want to monitor their health without disrupting their daily routines.
The healthcare industry is also recognizing the potential of wearable health monitoring devices to improve patient care and reduce healthcare costs. Remote patient monitoring systems, enabled by low-power wearable devices, allow healthcare providers to track patients' vital signs and health status outside of traditional clinical settings. This capability is particularly valuable for managing chronic conditions, post-operative care, and elderly care, as it can help prevent hospital readmissions and enable early interventions.
The COVID-19 pandemic has further accelerated the adoption of wearable health monitoring devices. The need for remote health monitoring and the desire to track potential symptoms have led to increased interest in devices that can measure body temperature, respiratory rate, and other relevant health indicators.
Market research indicates that the global wearable medical devices market is expected to grow substantially in the coming years. Factors contributing to this growth include technological advancements in sensor technology, miniaturization of components, and improvements in battery life and power efficiency. The integration of artificial intelligence and machine learning algorithms into these devices is also enhancing their capabilities, allowing for more accurate health predictions and personalized insights.
However, challenges remain in the widespread adoption of low-power wearable health monitoring devices. Concerns about data privacy and security, as well as the accuracy and reliability of measurements, need to be addressed to gain consumer trust. Additionally, regulatory approval processes for medical-grade wearable devices can be lengthy and complex, potentially slowing market entry for some innovative products.
Despite these challenges, the market demand for low-power wearable health monitoring devices remains strong and is expected to continue growing. As technology advances and consumer awareness increases, these devices are poised to play an increasingly important role in preventive healthcare and personalized medicine.
Current State and Challenges of Neuromorphic Computing in Healthcare
Neuromorphic computing in healthcare has made significant strides in recent years, yet it still faces numerous challenges. The current state of this technology is characterized by a mix of promising advancements and persistent obstacles. One of the primary areas of progress is in the development of low-power, wearable monitoring devices that utilize neuromorphic chips. These devices have shown potential in continuous health monitoring, offering real-time data collection with minimal energy consumption.
However, the integration of neuromorphic computing into mainstream healthcare systems remains limited. While research prototypes have demonstrated impressive capabilities, the transition to commercially viable products has been slow. This is partly due to the complexity of neuromorphic architectures and the need for specialized programming paradigms, which differ significantly from traditional computing approaches.
A major challenge lies in the scalability of neuromorphic systems for healthcare applications. Current neuromorphic chips often struggle to handle the diverse and complex data streams typical in medical environments. This limitation hinders their ability to process and analyze large-scale health data efficiently, a crucial requirement for comprehensive patient monitoring and diagnostics.
Another significant hurdle is the reliability and accuracy of neuromorphic systems in healthcare settings. The inherent variability in neuromorphic hardware can lead to inconsistencies in data processing and decision-making, which is particularly problematic in critical healthcare applications where precision is paramount. Addressing this challenge requires advancements in both hardware design and algorithmic approaches to ensure robust and dependable performance.
The development of on-device alerts and decision-making capabilities presents both opportunities and challenges. While neuromorphic chips show promise in rapid, low-power data processing for immediate health alerts, ensuring the accuracy and contextual relevance of these alerts remains a significant challenge. False positives or missed critical events could have serious consequences in healthcare scenarios.
Interoperability with existing healthcare IT infrastructure is another key challenge. Neuromorphic systems need to seamlessly integrate with traditional electronic health records and other medical devices, requiring standardized interfaces and data formats. This integration is crucial for the widespread adoption of neuromorphic technology in healthcare settings.
Lastly, regulatory hurdles pose a significant challenge to the adoption of neuromorphic computing in healthcare. The novel nature of these systems means that existing regulatory frameworks may not adequately address their unique characteristics, potentially slowing down approval processes and market entry.
However, the integration of neuromorphic computing into mainstream healthcare systems remains limited. While research prototypes have demonstrated impressive capabilities, the transition to commercially viable products has been slow. This is partly due to the complexity of neuromorphic architectures and the need for specialized programming paradigms, which differ significantly from traditional computing approaches.
A major challenge lies in the scalability of neuromorphic systems for healthcare applications. Current neuromorphic chips often struggle to handle the diverse and complex data streams typical in medical environments. This limitation hinders their ability to process and analyze large-scale health data efficiently, a crucial requirement for comprehensive patient monitoring and diagnostics.
Another significant hurdle is the reliability and accuracy of neuromorphic systems in healthcare settings. The inherent variability in neuromorphic hardware can lead to inconsistencies in data processing and decision-making, which is particularly problematic in critical healthcare applications where precision is paramount. Addressing this challenge requires advancements in both hardware design and algorithmic approaches to ensure robust and dependable performance.
The development of on-device alerts and decision-making capabilities presents both opportunities and challenges. While neuromorphic chips show promise in rapid, low-power data processing for immediate health alerts, ensuring the accuracy and contextual relevance of these alerts remains a significant challenge. False positives or missed critical events could have serious consequences in healthcare scenarios.
Interoperability with existing healthcare IT infrastructure is another key challenge. Neuromorphic systems need to seamlessly integrate with traditional electronic health records and other medical devices, requiring standardized interfaces and data formats. This integration is crucial for the widespread adoption of neuromorphic technology in healthcare settings.
Lastly, regulatory hurdles pose a significant challenge to the adoption of neuromorphic computing in healthcare. The novel nature of these systems means that existing regulatory frameworks may not adequately address their unique characteristics, potentially slowing down approval processes and market entry.
Existing Neuromorphic Solutions for Wearable Health Monitoring
01 Low-power neuromorphic chip design
Neuromorphic chips are designed with power-efficient architectures that mimic the human brain's neural networks. These designs incorporate techniques such as sparse coding, event-driven processing, and analog computing to significantly reduce power consumption compared to traditional digital processors.- Low-power neuromorphic chip design: Neuromorphic chips are designed with energy-efficient architectures that mimic the human brain's neural networks. These designs incorporate low-power consumption techniques such as event-driven processing, sparse coding, and analog computing to significantly reduce energy usage while maintaining high computational performance.
- Power-efficient synaptic devices: Advanced synaptic devices are developed for neuromorphic chips to minimize power consumption. These devices utilize novel materials and structures to achieve ultra-low power operation, including memristors, phase-change materials, and spintronic devices. They enable efficient weight storage and updates, reducing the overall energy requirements of neuromorphic systems.
- Dynamic power management techniques: Neuromorphic chips implement dynamic power management strategies to optimize energy consumption. These techniques include adaptive voltage scaling, clock gating, and power gating of inactive neural circuits. By dynamically adjusting power usage based on computational demands, these chips can achieve significant energy savings during operation.
- Sparse coding and event-driven processing: Neuromorphic chips utilize sparse coding and event-driven processing to reduce power consumption. These approaches minimize data movement and computations by only processing relevant information when needed. This results in substantial energy savings compared to traditional computing architectures, especially for tasks involving sensory data processing and pattern recognition.
- 3D integration and advanced packaging: Advanced packaging and 3D integration techniques are employed to optimize power consumption in neuromorphic chips. These approaches include through-silicon vias (TSVs), interposer-based integration, and die stacking. By reducing interconnect lengths and improving thermal management, these techniques contribute to lower power consumption and enhanced overall system efficiency.
02 Dynamic power management in neuromorphic systems
Advanced power management techniques are implemented in neuromorphic chips to optimize energy usage. These include dynamic voltage and frequency scaling, selective activation of neural circuits, and adaptive power gating to minimize power consumption during idle periods or low computational demands.Expand Specific Solutions03 Energy-efficient synaptic operations
Neuromorphic chips employ novel materials and device structures to perform synaptic operations with minimal energy expenditure. This includes the use of memristive devices, phase-change materials, or spintronic elements that can efficiently store and process synaptic weights, reducing the overall power consumption of the chip.Expand Specific Solutions04 Optimized neural network architectures
Researchers develop specialized neural network architectures tailored for neuromorphic hardware to maximize energy efficiency. These architectures often involve sparse connectivity, reduced precision computations, and optimized data flow patterns that minimize unnecessary operations and data movement, thereby lowering power consumption.Expand Specific Solutions05 Integration of energy harvesting techniques
Some neuromorphic chip designs incorporate energy harvesting mechanisms to supplement or reduce their power requirements. These may include harvesting energy from ambient light, thermal gradients, or mechanical vibrations, allowing the chips to operate with minimal external power input in certain applications.Expand Specific Solutions
Key Players in Neuromorphic Computing and Healthcare Wearables
The neuromorphic chip market for healthcare wearables is in its early growth stage, with significant potential for expansion. The market size is projected to increase rapidly as demand for low-power, intelligent edge devices in healthcare monitoring grows. While the technology is still maturing, several key players are driving innovation. Companies like Sotera Wireless, VitalConnect, and CareBand are developing wearable biosensors, while semiconductor firms such as Syntiant, Renesas, and Huawei are advancing neuromorphic chip designs. Academic institutions like Tianjin University and Shanghai Jiao Tong University are also contributing to R&D efforts. As the technology progresses, we can expect increased adoption in applications like continuous patient monitoring and early disease detection.
Koninklijke Philips NV
Technical Solution: Philips has been developing neuromorphic computing solutions for healthcare applications, focusing on integrating these technologies into their existing medical devices and wearables. Their approach combines neuromorphic chips with advanced sensors for continuous patient monitoring. Philips' wearable biosensors use low-power processing to analyze multiple vital signs simultaneously, providing early warning scores for patient deterioration[7]. The company has also explored using neuromorphic computing for ECG analysis and arrhythmia detection, potentially enabling on-device processing of complex cardiac signals with minimal power consumption[8]. Philips' IntelliVue Guardian Solution, which incorporates some of these technologies, has been shown to reduce cardiac and respiratory arrests by up to 86%[9].
Strengths: Integration with existing medical device ecosystem, comprehensive vital sign monitoring capabilities. Weaknesses: May rely on a mix of traditional and neuromorphic computing, potentially limiting full power efficiency gains.
International Business Machines Corp.
Technical Solution: IBM has developed a neuromorphic chip called TrueNorth, which is designed for low-power, real-time sensory processing. For healthcare applications, TrueNorth can be used in wearable devices for continuous monitoring and on-device alerts. The chip's architecture mimics the human brain's neural networks, allowing for efficient processing of sensory data[1]. TrueNorth consumes only 70 milliwatts of power while performing 46 billion synaptic operations per second, making it ideal for battery-powered wearable devices[2]. IBM has demonstrated TrueNorth's capabilities in real-time speech recognition and image classification, which can be applied to healthcare monitoring scenarios[3].
Strengths: Extremely low power consumption, high-speed parallel processing, and scalability. Weaknesses: Requires specialized programming paradigms and may have limited compatibility with existing software ecosystems.
Core Innovations in Low-Power On-Device Alert Systems
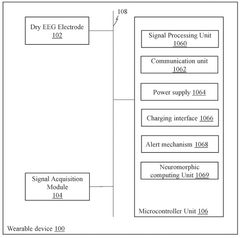
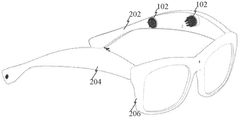
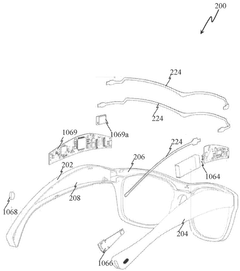
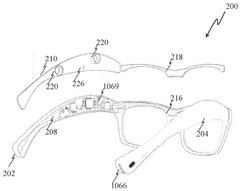
Wearable epileptic seizure prediction and alert glasses based on neuromorphic computing
PatentWO2025133790A1
Innovation
- A wearable device equipped with dry EEG electrodes and a neuromorphic computing unit that analyzes EEG signals in real-time using neural network models trained on seizure data, enabling detection of preictal phase abnormalities and providing timely alerts.
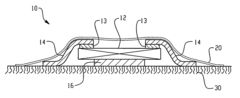
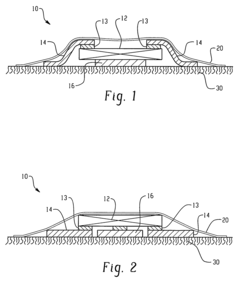
Wearable wireless device for monitoring, analyzing and communicating physiological status
PatentActiveUS7904133B2
Innovation
- A compact, lightweight, non-invasive wearable device with a unified system of electrodes and an electronics module covered by a single adhesive membrane, including a wireless transmitter for alarm status communication, allowing for adhesion to the body without interfering with motion and providing local alarms.
Regulatory Landscape for AI-Powered Medical Devices
The regulatory landscape for AI-powered medical devices, including neuromorphic chips for healthcare applications, is rapidly evolving to keep pace with technological advancements. In the United States, the Food and Drug Administration (FDA) has taken proactive steps to address the unique challenges posed by these innovative technologies.
The FDA has established a Digital Health Center of Excellence to streamline the regulatory process for AI-based medical devices. This initiative aims to provide clarity on regulatory requirements while fostering innovation in the field. The agency has also released guidance documents specifically addressing AI/ML-based Software as a Medical Device (SaMD), outlining a framework for assessing and monitoring these products throughout their lifecycle.
In Europe, the Medical Device Regulation (MDR) and In Vitro Diagnostic Regulation (IVDR) have introduced more stringent requirements for AI-powered medical devices. These regulations emphasize the importance of clinical evidence, post-market surveillance, and risk management for such devices. The European Commission has also proposed an Artificial Intelligence Act, which would establish a risk-based regulatory framework for AI applications, including those in healthcare.
Internationally, the International Medical Device Regulators Forum (IMDRF) has been working on harmonizing regulatory approaches for AI-based medical devices. Their efforts focus on developing common principles for evaluating the safety and performance of these technologies across different jurisdictions.
Key regulatory considerations for neuromorphic chips in healthcare applications include data privacy, cybersecurity, and the interpretability of AI algorithms. Regulators are particularly concerned with ensuring the transparency and explainability of AI-driven decision-making processes in medical devices.
As the field of neuromorphic computing in healthcare continues to advance, regulatory bodies are likely to refine their approaches. This may include developing specific guidelines for low-power wearable monitoring devices and on-device alert systems powered by neuromorphic chips. Manufacturers and developers in this space must stay informed about evolving regulatory requirements and engage proactively with regulatory agencies to ensure compliance and facilitate market access for their innovative products.
The FDA has established a Digital Health Center of Excellence to streamline the regulatory process for AI-based medical devices. This initiative aims to provide clarity on regulatory requirements while fostering innovation in the field. The agency has also released guidance documents specifically addressing AI/ML-based Software as a Medical Device (SaMD), outlining a framework for assessing and monitoring these products throughout their lifecycle.
In Europe, the Medical Device Regulation (MDR) and In Vitro Diagnostic Regulation (IVDR) have introduced more stringent requirements for AI-powered medical devices. These regulations emphasize the importance of clinical evidence, post-market surveillance, and risk management for such devices. The European Commission has also proposed an Artificial Intelligence Act, which would establish a risk-based regulatory framework for AI applications, including those in healthcare.
Internationally, the International Medical Device Regulators Forum (IMDRF) has been working on harmonizing regulatory approaches for AI-based medical devices. Their efforts focus on developing common principles for evaluating the safety and performance of these technologies across different jurisdictions.
Key regulatory considerations for neuromorphic chips in healthcare applications include data privacy, cybersecurity, and the interpretability of AI algorithms. Regulators are particularly concerned with ensuring the transparency and explainability of AI-driven decision-making processes in medical devices.
As the field of neuromorphic computing in healthcare continues to advance, regulatory bodies are likely to refine their approaches. This may include developing specific guidelines for low-power wearable monitoring devices and on-device alert systems powered by neuromorphic chips. Manufacturers and developers in this space must stay informed about evolving regulatory requirements and engage proactively with regulatory agencies to ensure compliance and facilitate market access for their innovative products.
Energy Efficiency and Battery Life Considerations
Energy efficiency and battery life are critical considerations in the development and implementation of neuromorphic chips for healthcare applications, particularly in wearable monitoring devices and on-device alert systems. The low-power nature of neuromorphic computing offers significant advantages in this domain, potentially revolutionizing the longevity and functionality of healthcare wearables.
Neuromorphic chips, designed to mimic the human brain's neural networks, inherently consume less power than traditional von Neumann architectures. This efficiency stems from their event-driven processing and distributed memory, which allows for selective activation of only the necessary components. In healthcare wearables, this translates to extended battery life and reduced charging frequency, enhancing user experience and compliance.
The energy efficiency of neuromorphic chips enables continuous monitoring of vital signs and health parameters without frequent battery replacements or recharging. This is particularly crucial for patients with chronic conditions or those requiring round-the-clock monitoring. The ability to process data locally on the device further reduces power consumption by minimizing the need for constant data transmission to external servers.
On-device alerts powered by neuromorphic chips can operate with minimal energy overhead. These chips can efficiently analyze incoming data streams in real-time, triggering alerts only when necessary. This selective activation conserves energy while maintaining the device's ability to respond promptly to critical health events.
The low-power characteristics of neuromorphic chips also facilitate the integration of energy harvesting technologies. Wearable devices equipped with these chips can potentially harness energy from body heat, motion, or ambient light, further extending their operational lifespan. This synergy between neuromorphic computing and energy harvesting could lead to self-sustaining healthcare monitoring devices.
As battery technology continues to evolve, the combination of advanced energy storage solutions with neuromorphic chips promises to push the boundaries of wearable device longevity. This could enable the development of implantable monitoring devices with extended lifespans, reducing the need for invasive replacement procedures and improving patient outcomes.
However, challenges remain in optimizing the energy efficiency of neuromorphic chips for healthcare applications. Balancing computational power with energy consumption requires careful design considerations. Additionally, ensuring the reliability and accuracy of low-power neuromorphic systems in critical healthcare monitoring scenarios is paramount.
Neuromorphic chips, designed to mimic the human brain's neural networks, inherently consume less power than traditional von Neumann architectures. This efficiency stems from their event-driven processing and distributed memory, which allows for selective activation of only the necessary components. In healthcare wearables, this translates to extended battery life and reduced charging frequency, enhancing user experience and compliance.
The energy efficiency of neuromorphic chips enables continuous monitoring of vital signs and health parameters without frequent battery replacements or recharging. This is particularly crucial for patients with chronic conditions or those requiring round-the-clock monitoring. The ability to process data locally on the device further reduces power consumption by minimizing the need for constant data transmission to external servers.
On-device alerts powered by neuromorphic chips can operate with minimal energy overhead. These chips can efficiently analyze incoming data streams in real-time, triggering alerts only when necessary. This selective activation conserves energy while maintaining the device's ability to respond promptly to critical health events.
The low-power characteristics of neuromorphic chips also facilitate the integration of energy harvesting technologies. Wearable devices equipped with these chips can potentially harness energy from body heat, motion, or ambient light, further extending their operational lifespan. This synergy between neuromorphic computing and energy harvesting could lead to self-sustaining healthcare monitoring devices.
As battery technology continues to evolve, the combination of advanced energy storage solutions with neuromorphic chips promises to push the boundaries of wearable device longevity. This could enable the development of implantable monitoring devices with extended lifespans, reducing the need for invasive replacement procedures and improving patient outcomes.
However, challenges remain in optimizing the energy efficiency of neuromorphic chips for healthcare applications. Balancing computational power with energy consumption requires careful design considerations. Additionally, ensuring the reliability and accuracy of low-power neuromorphic systems in critical healthcare monitoring scenarios is paramount.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!