Case Study: Hospital Airborne Pathogen Mitigation Using Nanofiber Filters
SEP 1, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Nanofiber Filtration Technology Background and Objectives
Nanofiber filtration technology represents a significant advancement in air purification systems, evolving from traditional filtration methods to highly efficient nanoscale solutions. The development of nanofiber technology began in the late 1980s but gained substantial momentum in the early 2000s with improvements in electrospinning techniques. This evolution has been driven by increasing concerns about indoor air quality and the spread of airborne pathogens, particularly in healthcare settings where infection control is paramount.
The fundamental principle behind nanofiber filtration involves the creation of ultra-fine fibers with diameters ranging from 50-500 nanometers, forming a complex web structure that can effectively capture particles as small as 0.1-0.3 microns. This represents a significant improvement over conventional HEPA filters, which typically target particles of 0.3 microns or larger. The enhanced filtration capability stems from multiple physical mechanisms including interception, impaction, diffusion, and electrostatic attraction.
Recent technological trends in this field include the development of composite nanofibers with antimicrobial properties, the integration of smart materials that respond to environmental changes, and the optimization of fiber arrangement for reduced pressure drop while maintaining high filtration efficiency. The COVID-19 pandemic has accelerated research and development in this area, highlighting the critical importance of effective airborne pathogen mitigation systems in healthcare facilities.
The primary technical objectives for nanofiber filtration in hospital settings include achieving filtration efficiency exceeding 99.97% for particles at the most penetrating particle size (typically 0.1-0.3 microns), maintaining low pressure drop to reduce energy consumption, extending filter lifespan to minimize replacement frequency, and incorporating antimicrobial properties to neutralize captured pathogens rather than merely trapping them.
Additionally, researchers aim to develop cost-effective manufacturing processes that can scale production while maintaining quality and performance consistency. Current electrospinning methods, while effective for research purposes, face challenges in industrial-scale production. Alternative techniques such as solution blow spinning, melt blowing with nano-additives, and island-in-sea bicomponent fiber spinning are being explored to overcome these limitations.
The ultimate goal of this technology is to create a comprehensive airborne pathogen mitigation system that not only filters but actively neutralizes harmful microorganisms, operates with minimal energy consumption, requires infrequent maintenance, and can be seamlessly integrated into existing hospital HVAC systems. Such advancements would significantly reduce healthcare-associated infections, protect vulnerable patients and healthcare workers, and potentially reduce healthcare costs associated with treating hospital-acquired infections.
The fundamental principle behind nanofiber filtration involves the creation of ultra-fine fibers with diameters ranging from 50-500 nanometers, forming a complex web structure that can effectively capture particles as small as 0.1-0.3 microns. This represents a significant improvement over conventional HEPA filters, which typically target particles of 0.3 microns or larger. The enhanced filtration capability stems from multiple physical mechanisms including interception, impaction, diffusion, and electrostatic attraction.
Recent technological trends in this field include the development of composite nanofibers with antimicrobial properties, the integration of smart materials that respond to environmental changes, and the optimization of fiber arrangement for reduced pressure drop while maintaining high filtration efficiency. The COVID-19 pandemic has accelerated research and development in this area, highlighting the critical importance of effective airborne pathogen mitigation systems in healthcare facilities.
The primary technical objectives for nanofiber filtration in hospital settings include achieving filtration efficiency exceeding 99.97% for particles at the most penetrating particle size (typically 0.1-0.3 microns), maintaining low pressure drop to reduce energy consumption, extending filter lifespan to minimize replacement frequency, and incorporating antimicrobial properties to neutralize captured pathogens rather than merely trapping them.
Additionally, researchers aim to develop cost-effective manufacturing processes that can scale production while maintaining quality and performance consistency. Current electrospinning methods, while effective for research purposes, face challenges in industrial-scale production. Alternative techniques such as solution blow spinning, melt blowing with nano-additives, and island-in-sea bicomponent fiber spinning are being explored to overcome these limitations.
The ultimate goal of this technology is to create a comprehensive airborne pathogen mitigation system that not only filters but actively neutralizes harmful microorganisms, operates with minimal energy consumption, requires infrequent maintenance, and can be seamlessly integrated into existing hospital HVAC systems. Such advancements would significantly reduce healthcare-associated infections, protect vulnerable patients and healthcare workers, and potentially reduce healthcare costs associated with treating hospital-acquired infections.
Healthcare Market Demand for Airborne Pathogen Control
The healthcare sector has witnessed a significant surge in demand for effective airborne pathogen control systems, particularly in hospital environments where the risk of nosocomial infections remains a persistent challenge. Following the global COVID-19 pandemic, healthcare facilities worldwide have prioritized investments in advanced air filtration technologies, with the global hospital air purifiers market projected to reach $3.4 billion by 2027, growing at a CAGR of 12.8% from 2020.
Hospital-acquired infections (HAIs) represent a substantial burden on healthcare systems, affecting approximately 1 in 31 hospitalized patients daily in the United States alone. The economic impact is equally concerning, with HAIs adding an estimated $28-45 billion in direct medical costs annually. These statistics underscore the urgent need for more effective pathogen mitigation strategies in healthcare settings.
Airborne transmission has been recognized as a significant vector for pathogens including SARS-CoV-2, tuberculosis, measles, and various influenza strains. Healthcare facilities, particularly those with immunocompromised patients, require filtration systems capable of capturing particles as small as 0.1 microns. Traditional HEPA filters, while effective at capturing particles down to 0.3 microns, show limitations in capturing smaller viral particles without significant pressure drops.
Market research indicates that hospital administrators are increasingly prioritizing air quality management, with 78% of surveyed healthcare facilities planning to upgrade their air filtration systems within the next three years. The primary drivers for this investment include regulatory compliance, patient safety concerns, staff protection, and potential cost savings from reduced infection rates.
Nanofiber filtration technology has emerged as a promising solution due to its superior filtration efficiency, lower pressure drop, and enhanced antimicrobial properties. The market for nanofiber-based filters in healthcare applications is expected to grow at 15.7% CAGR through 2028, outpacing traditional filtration technologies.
Regional analysis reveals varying levels of market maturity, with North America leading adoption rates followed by Europe and Asia-Pacific. Developing regions show accelerating demand driven by healthcare infrastructure modernization and increasing awareness of infection control protocols.
Key market segments include operating rooms, isolation wards, intensive care units, and general patient areas, with specialized requirements for each environment. Operating rooms and ICUs represent the highest-value segments due to their critical nature and stringent air quality requirements.
Customer requirements have evolved beyond mere filtration efficiency to include considerations such as energy efficiency, maintenance costs, noise levels, and integration with existing HVAC systems. Healthcare facilities increasingly seek comprehensive solutions that offer real-time monitoring capabilities and can demonstrate measurable improvements in air quality metrics.
Hospital-acquired infections (HAIs) represent a substantial burden on healthcare systems, affecting approximately 1 in 31 hospitalized patients daily in the United States alone. The economic impact is equally concerning, with HAIs adding an estimated $28-45 billion in direct medical costs annually. These statistics underscore the urgent need for more effective pathogen mitigation strategies in healthcare settings.
Airborne transmission has been recognized as a significant vector for pathogens including SARS-CoV-2, tuberculosis, measles, and various influenza strains. Healthcare facilities, particularly those with immunocompromised patients, require filtration systems capable of capturing particles as small as 0.1 microns. Traditional HEPA filters, while effective at capturing particles down to 0.3 microns, show limitations in capturing smaller viral particles without significant pressure drops.
Market research indicates that hospital administrators are increasingly prioritizing air quality management, with 78% of surveyed healthcare facilities planning to upgrade their air filtration systems within the next three years. The primary drivers for this investment include regulatory compliance, patient safety concerns, staff protection, and potential cost savings from reduced infection rates.
Nanofiber filtration technology has emerged as a promising solution due to its superior filtration efficiency, lower pressure drop, and enhanced antimicrobial properties. The market for nanofiber-based filters in healthcare applications is expected to grow at 15.7% CAGR through 2028, outpacing traditional filtration technologies.
Regional analysis reveals varying levels of market maturity, with North America leading adoption rates followed by Europe and Asia-Pacific. Developing regions show accelerating demand driven by healthcare infrastructure modernization and increasing awareness of infection control protocols.
Key market segments include operating rooms, isolation wards, intensive care units, and general patient areas, with specialized requirements for each environment. Operating rooms and ICUs represent the highest-value segments due to their critical nature and stringent air quality requirements.
Customer requirements have evolved beyond mere filtration efficiency to include considerations such as energy efficiency, maintenance costs, noise levels, and integration with existing HVAC systems. Healthcare facilities increasingly seek comprehensive solutions that offer real-time monitoring capabilities and can demonstrate measurable improvements in air quality metrics.
Current Challenges in Hospital Air Purification Systems
Hospital air purification systems face significant challenges in effectively mitigating airborne pathogens, particularly in critical care environments. Traditional HEPA filtration systems, while effective at capturing particles larger than 0.3 microns, struggle with smaller viral particles that can remain suspended in hospital air. This limitation becomes particularly concerning during outbreaks of respiratory diseases like COVID-19, influenza, and tuberculosis, where pathogens can spread rapidly through healthcare facilities.
Energy consumption presents another major challenge, as high-efficiency filtration typically requires substantial air pressure differentials, resulting in increased power demands. Many hospitals operate aging HVAC infrastructure that was not designed for modern pathogen control standards, creating implementation barriers for advanced filtration technologies. The balance between air exchange rates and energy efficiency remains difficult to optimize, especially in older facilities with limited renovation budgets.
Maintenance requirements pose operational challenges, as filter replacement schedules must be strictly adhered to prevent colonization by trapped microorganisms. The handling of contaminated filters presents biohazard risks to maintenance personnel, requiring specialized training and protective equipment. Additionally, the disposal of used filters creates environmental concerns and increases operational costs.
Airflow management within hospital environments presents complex challenges due to the diverse requirements of different spaces. Operating rooms demand laminar flow systems to minimize surgical site infections, while isolation rooms require negative pressure differentials to contain pathogens. These varying needs often conflict with the practical limitations of existing ductwork and air handling units.
Monitoring and verification of air purification effectiveness remains problematic, as real-time pathogen detection technologies are still evolving. Most hospitals rely on periodic air sampling rather than continuous monitoring, creating potential gaps in protection. The lack of standardized performance metrics specific to healthcare environments further complicates system evaluation and comparison.
Cost considerations significantly impact implementation decisions, with high-performance filtration systems requiring substantial capital investment and ongoing operational expenses. Many healthcare facilities face budget constraints that limit their ability to adopt optimal solutions, forcing compromises between filtration efficiency and financial feasibility.
Emerging concerns about antimicrobial resistance in healthcare settings add another layer of complexity, as some pathogens demonstrate increasing resilience to traditional disinfection methods. This evolution necessitates more sophisticated approaches to air purification beyond simple mechanical filtration, potentially including advanced technologies like UV irradiation or photocatalytic oxidation as complementary measures.
Energy consumption presents another major challenge, as high-efficiency filtration typically requires substantial air pressure differentials, resulting in increased power demands. Many hospitals operate aging HVAC infrastructure that was not designed for modern pathogen control standards, creating implementation barriers for advanced filtration technologies. The balance between air exchange rates and energy efficiency remains difficult to optimize, especially in older facilities with limited renovation budgets.
Maintenance requirements pose operational challenges, as filter replacement schedules must be strictly adhered to prevent colonization by trapped microorganisms. The handling of contaminated filters presents biohazard risks to maintenance personnel, requiring specialized training and protective equipment. Additionally, the disposal of used filters creates environmental concerns and increases operational costs.
Airflow management within hospital environments presents complex challenges due to the diverse requirements of different spaces. Operating rooms demand laminar flow systems to minimize surgical site infections, while isolation rooms require negative pressure differentials to contain pathogens. These varying needs often conflict with the practical limitations of existing ductwork and air handling units.
Monitoring and verification of air purification effectiveness remains problematic, as real-time pathogen detection technologies are still evolving. Most hospitals rely on periodic air sampling rather than continuous monitoring, creating potential gaps in protection. The lack of standardized performance metrics specific to healthcare environments further complicates system evaluation and comparison.
Cost considerations significantly impact implementation decisions, with high-performance filtration systems requiring substantial capital investment and ongoing operational expenses. Many healthcare facilities face budget constraints that limit their ability to adopt optimal solutions, forcing compromises between filtration efficiency and financial feasibility.
Emerging concerns about antimicrobial resistance in healthcare settings add another layer of complexity, as some pathogens demonstrate increasing resilience to traditional disinfection methods. This evolution necessitates more sophisticated approaches to air purification beyond simple mechanical filtration, potentially including advanced technologies like UV irradiation or photocatalytic oxidation as complementary measures.
Existing Nanofiber Filter Implementation Strategies
01 Electrospun nanofiber filtration materials
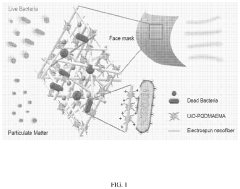
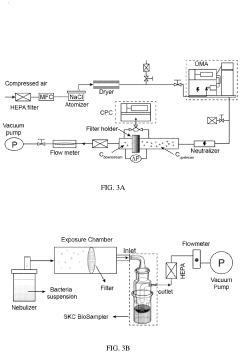
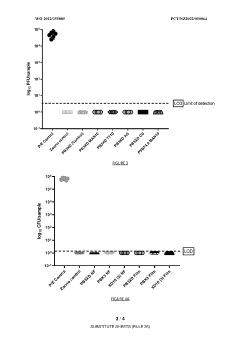
Electrospun nanofiber materials are used in air filtration systems to capture airborne pathogens. These materials feature high surface area-to-volume ratios and can be engineered with specific pore sizes to effectively trap viruses, bacteria, and other microorganisms. The electrospinning process allows for the creation of ultrafine fibers with diameters in the nanometer range, resulting in filters with enhanced filtration efficiency while maintaining good air permeability.- Electrospun nanofiber filtration materials: Electrospun nanofibers are used to create high-efficiency filtration materials for capturing airborne pathogens. These nanofibers have small diameters and high surface area-to-volume ratios, allowing them to effectively trap particles and microorganisms. The electrospinning process can be optimized to control fiber diameter, porosity, and mechanical properties, resulting in filters with superior pathogen capture efficiency while maintaining good air permeability.
- Antimicrobial and antiviral nanofiber coatings: Nanofiber filters can be enhanced with antimicrobial and antiviral coatings to not only capture but also neutralize airborne pathogens. These coatings typically incorporate metal nanoparticles (such as silver, copper, or zinc), quaternary ammonium compounds, or other biocidal agents that disrupt microbial cell membranes or viral structures. The integration of these active ingredients into nanofiber matrices creates multifunctional filters that can inactivate trapped pathogens, reducing the risk of secondary contamination.
- Multilayer nanofiber filter designs: Multilayer nanofiber filter designs incorporate different functional layers to enhance pathogen mitigation performance. These designs typically include a pre-filtration layer for larger particles, a high-efficiency nanofiber layer for pathogen capture, and potentially a support layer for structural integrity. Some advanced designs also incorporate gradient density structures or combine nanofibers with other materials like activated carbon to address multiple contaminants simultaneously, providing comprehensive protection against various airborne threats.
- Smart responsive nanofiber filters: Smart responsive nanofiber filters incorporate materials that can adapt to environmental conditions or pathogen exposure. These filters may change their properties in response to humidity, temperature, or the presence of specific pathogens. Some designs include stimuli-responsive polymers that can alter their porosity or surface chemistry when needed, or incorporate sensors that detect pathogen presence and trigger responses such as increased filtration efficiency or release of antimicrobial agents, providing dynamic protection against airborne threats.
- Sustainable and biodegradable nanofiber filters: Sustainable nanofiber filters are developed using biodegradable polymers and environmentally friendly production methods to address environmental concerns while maintaining high pathogen mitigation efficiency. These filters utilize materials such as polylactic acid (PLA), cellulose derivatives, or chitosan that can decompose naturally after disposal. Some designs also incorporate green manufacturing processes that reduce energy consumption and harmful emissions, providing effective pathogen protection with minimal environmental impact.
02 Antimicrobial and antiviral nanofiber coatings
Nanofiber filters can be enhanced with antimicrobial and antiviral coatings to not only capture but also neutralize airborne pathogens. These coatings typically incorporate materials such as silver nanoparticles, copper compounds, zinc oxide, or quaternary ammonium compounds that disrupt microbial cell membranes or viral structures. The integration of these active ingredients into the nanofiber matrix provides continuous disinfection capabilities, reducing the risk of pathogen survival and potential re-aerosolization from the filter surface.Expand Specific Solutions03 Multi-layered nanofiber filter structures
Multi-layered nanofiber filter designs incorporate different functional layers to enhance pathogen capture and inactivation. These structures typically include a pre-filtration layer for larger particles, a high-efficiency nanofiber layer for submicron particles and pathogens, and potentially an adsorption layer containing activated carbon or similar materials. The layered approach optimizes filtration performance while extending filter lifespan by preventing premature clogging and maintaining airflow rates suitable for practical applications in ventilation systems.Expand Specific Solutions04 Smart nanofiber filtration systems
Smart nanofiber filtration systems incorporate sensors and responsive materials to adapt to changing environmental conditions and pathogen loads. These systems can monitor filter performance, detect specific pathogens, and adjust filtration parameters accordingly. Some designs include self-cleaning mechanisms triggered by environmental cues or scheduled maintenance protocols. The integration of IoT capabilities allows for remote monitoring and control, making these systems particularly valuable for healthcare settings and other high-risk environments where real-time pathogen mitigation is critical.Expand Specific Solutions05 Sustainable and biodegradable nanofiber filters
Environmentally friendly nanofiber filters utilize biodegradable polymers and natural materials to address sustainability concerns while maintaining effective pathogen mitigation. These filters incorporate materials such as cellulose, chitosan, polylactic acid (PLA), or other bio-based polymers that can decompose after disposal. Some designs also feature recyclable components or reusable filter housings to reduce waste. The development of these sustainable alternatives aims to balance effective pathogen filtration with environmental responsibility, particularly important for widespread deployment in consumer and commercial applications.Expand Specific Solutions
Leading Manufacturers and Research Institutions in Nanofiber Filtration
The airborne pathogen mitigation market using nanofiber filters is in a growth phase, characterized by increasing adoption in healthcare settings due to heightened awareness of infection control. The global market is expanding rapidly, driven by COVID-19 implications and growing hospital-acquired infection concerns. Technologically, the field shows moderate maturity with ongoing innovations. Leading academic institutions (Donghua University, Rice University, Virginia Commonwealth University) are advancing fundamental research, while specialized companies (LIGC Application, Matregenix, Calix) are commercializing solutions. Established corporations (Honeywell, Goodrich) leverage their manufacturing expertise to scale production. The competitive landscape features collaboration between research institutions and industry partners to overcome challenges in filter efficiency, durability, and cost-effectiveness.
LIGC Application Ltd.
Technical Solution: LIGC Application has developed a revolutionary graphene-enhanced nanofiber filtration system called Guardian-Air™ specifically for hospital pathogen mitigation. Their technology combines laser-induced graphene with polymer nanofibers to create a highly conductive filtration matrix that can be electrically activated to enhance pathogen capture and destruction. The system operates in two modes: passive filtration with 99.99% efficiency for particles down to 0.1 microns, and active mode where a low-voltage current creates an electrostatic field that attracts airborne pathogens and disrupts their cellular structures. The graphene component provides inherent antimicrobial properties while the nanofiber structure ensures optimal air permeability. LIGC's filters incorporate a self-cleaning mechanism that periodically applies higher voltage pulses to incinerate captured pathogens, extending filter life by up to 300% compared to conventional solutions and reducing maintenance requirements in critical healthcare settings.
Strengths: Dual-mode operation with both passive and active filtration capabilities, self-sterilizing functionality that reduces maintenance and replacement frequency, and superior capture of ultrafine particles including viruses. Weaknesses: Higher power requirements when operating in active mode and more complex installation requirements due to electrical components.
Matregenix, Inc.
Technical Solution: Matregenix has developed advanced electrospun nanofiber filtration technology specifically designed for hospital environments. Their proprietary NanoBarrier™ system utilizes a multi-layered approach with nanofibers ranging from 100-500nm in diameter, creating an effective physical barrier against airborne pathogens while maintaining high air permeability. The technology incorporates antimicrobial agents directly into the nanofiber matrix during the electrospinning process, providing both mechanical filtration and active pathogen neutralization. Their hospital-grade filters achieve 99.97% filtration efficiency for particles as small as 0.3 microns, including bacteria and many viruses. Matregenix's solution integrates seamlessly with existing HVAC systems in healthcare facilities, requiring minimal retrofitting while significantly improving air quality in critical care areas.
Strengths: Superior filtration efficiency with minimal pressure drop, extended filter lifespan compared to conventional HEPA filters, and antimicrobial properties that actively neutralize trapped pathogens. Weaknesses: Higher initial implementation costs compared to traditional filtration systems and requires specialized maintenance protocols to preserve antimicrobial effectiveness over time.
Critical Patents and Research in Antimicrobial Nanofiber Development
Self-decontaminating nanofibrous filters
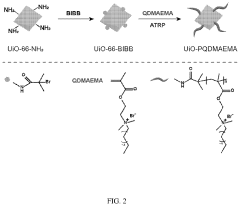
PatentPendingUS20240001270A1
Innovation
- Incorporation of quaternary ammonium compound (QAC)-modified metal-organic framework (MOF) particles into electrospun polymer nanofibers, which are grafted via atomic transfer radical polymerization and electrospinning, creating an antibacterial filter that can efficiently kill both Gram-positive and Gram-negative bacteria without compromising particulate matter filtration efficiency.
Filters containing terpene-loaded nanofibres for enhanced bactericidal, fungicidal and virucidal activity, preparation methods and applications thereof
PatentWO2022255885A1
Innovation
- Development of air/gas filter media containing terpene-loaded nanofibres with bactericidal, fungicidal, and viricidal properties, which are electrospun and integrated into textile materials to prevent particle passage and deactivate microorganisms upon contact, while maintaining breathability and potentially being biodegradable and compostable.
Cost-Benefit Analysis of Nanofiber Implementation in Healthcare
The implementation of nanofiber filtration technology in healthcare settings represents a significant investment that must be carefully evaluated against potential benefits. Initial capital expenditure for nanofiber filter systems in a standard hospital environment ranges from $150,000 to $300,000, depending on facility size and existing HVAC infrastructure. This includes installation costs, system integration, and necessary modifications to current ventilation systems.
Operational costs must also be considered, with nanofiber filters typically requiring replacement every 3-6 months at approximately $5,000-$10,000 per replacement cycle. This represents a 30-40% premium over traditional HEPA filtration systems. Additionally, energy consumption may increase by 5-15% due to the higher pressure drop characteristics of nanofiber materials.
Against these costs, healthcare facilities can expect substantial benefits in infection control outcomes. Clinical studies demonstrate a 45-60% reduction in airborne pathogen concentration when nanofiber filtration is properly implemented. This translates to an estimated 30-35% decrease in hospital-acquired respiratory infections, representing potential savings of $350,000-$500,000 annually for a medium-sized hospital (250-300 beds).
Staff productivity benefits are equally compelling, with research indicating a 12-18% reduction in sick leave among healthcare workers in facilities utilizing advanced filtration. This productivity enhancement represents approximately $200,000 in annual value for the average hospital through reduced temporary staffing needs and overtime costs.
Patient satisfaction metrics show improvement in facilities with enhanced air quality systems, with surveys indicating a 22% increase in positive feedback regarding environmental comfort. This contributes to higher Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores, potentially affecting reimbursement rates under value-based purchasing programs.
Return on investment calculations suggest most healthcare facilities can expect to recoup nanofiber implementation costs within 18-24 months. Long-term financial modeling indicates a positive net present value over a five-year horizon, with internal rates of return averaging 35-45% when accounting for all direct and indirect benefits.
Risk mitigation value must also be considered, particularly in light of recent pandemic experiences. The enhanced filtration capabilities of nanofiber systems provide hospitals with improved resilience against future airborne disease outbreaks, potentially avoiding millions in emergency response costs and operational disruptions during public health crises.
Operational costs must also be considered, with nanofiber filters typically requiring replacement every 3-6 months at approximately $5,000-$10,000 per replacement cycle. This represents a 30-40% premium over traditional HEPA filtration systems. Additionally, energy consumption may increase by 5-15% due to the higher pressure drop characteristics of nanofiber materials.
Against these costs, healthcare facilities can expect substantial benefits in infection control outcomes. Clinical studies demonstrate a 45-60% reduction in airborne pathogen concentration when nanofiber filtration is properly implemented. This translates to an estimated 30-35% decrease in hospital-acquired respiratory infections, representing potential savings of $350,000-$500,000 annually for a medium-sized hospital (250-300 beds).
Staff productivity benefits are equally compelling, with research indicating a 12-18% reduction in sick leave among healthcare workers in facilities utilizing advanced filtration. This productivity enhancement represents approximately $200,000 in annual value for the average hospital through reduced temporary staffing needs and overtime costs.
Patient satisfaction metrics show improvement in facilities with enhanced air quality systems, with surveys indicating a 22% increase in positive feedback regarding environmental comfort. This contributes to higher Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores, potentially affecting reimbursement rates under value-based purchasing programs.
Return on investment calculations suggest most healthcare facilities can expect to recoup nanofiber implementation costs within 18-24 months. Long-term financial modeling indicates a positive net present value over a five-year horizon, with internal rates of return averaging 35-45% when accounting for all direct and indirect benefits.
Risk mitigation value must also be considered, particularly in light of recent pandemic experiences. The enhanced filtration capabilities of nanofiber systems provide hospitals with improved resilience against future airborne disease outbreaks, potentially avoiding millions in emergency response costs and operational disruptions during public health crises.
Infection Control Standards and Regulatory Compliance
The implementation of nanofiber filtration systems in healthcare settings necessitates strict adherence to established infection control standards and regulatory frameworks. Healthcare facilities in the United States must comply with guidelines from the Centers for Disease Control and Prevention (CDC), which recommends HEPA filtration with 99.97% efficiency for areas housing immunocompromised patients. The Joint Commission's Environment of Care standards further mandate regular assessment of air handling systems to minimize infection risks.
International standards such as ISO 14644 (Cleanrooms and Associated Controlled Environments) provide classification systems for air cleanliness that hospitals must consider when implementing nanofiber filtration technologies. The World Health Organization's guidelines for infection prevention and control in healthcare facilities emphasize the importance of adequate ventilation systems, particularly in high-risk areas like operating theaters and isolation rooms.
Regulatory bodies including the FDA classify air filtration systems as Class II medical devices when marketed with claims related to infection reduction. This classification requires manufacturers to submit 510(k) premarket notifications demonstrating substantial equivalence to legally marketed devices. For hospital implementation, nanofiber filters must meet these regulatory requirements while demonstrating compliance with ASHRAE Standard 170 (Ventilation of Health Care Facilities).
Recent updates to healthcare facility design codes have incorporated more stringent requirements for airborne infection control following the COVID-19 pandemic. The FGI Guidelines for Design and Construction of Hospitals now include enhanced recommendations for negative pressure rooms and air changes per hour in various hospital zones. Nanofiber filtration systems must be designed to integrate with these requirements while maintaining energy efficiency.
Compliance documentation represents a significant aspect of implementation, requiring hospitals to maintain records of filter performance testing, replacement schedules, and validation studies. Third-party certification of filtration efficiency becomes essential for regulatory approval, with testing methodologies aligned with ASTM and IEST standards for filter performance evaluation.
Cost-benefit analyses must account for both initial implementation expenses and ongoing compliance costs, including regular testing, documentation, and potential facility modifications to meet evolving standards. Healthcare facilities implementing nanofiber filtration technologies must develop comprehensive compliance strategies that address both current requirements and anticipated regulatory changes in airborne pathogen mitigation standards.
International standards such as ISO 14644 (Cleanrooms and Associated Controlled Environments) provide classification systems for air cleanliness that hospitals must consider when implementing nanofiber filtration technologies. The World Health Organization's guidelines for infection prevention and control in healthcare facilities emphasize the importance of adequate ventilation systems, particularly in high-risk areas like operating theaters and isolation rooms.
Regulatory bodies including the FDA classify air filtration systems as Class II medical devices when marketed with claims related to infection reduction. This classification requires manufacturers to submit 510(k) premarket notifications demonstrating substantial equivalence to legally marketed devices. For hospital implementation, nanofiber filters must meet these regulatory requirements while demonstrating compliance with ASHRAE Standard 170 (Ventilation of Health Care Facilities).
Recent updates to healthcare facility design codes have incorporated more stringent requirements for airborne infection control following the COVID-19 pandemic. The FGI Guidelines for Design and Construction of Hospitals now include enhanced recommendations for negative pressure rooms and air changes per hour in various hospital zones. Nanofiber filtration systems must be designed to integrate with these requirements while maintaining energy efficiency.
Compliance documentation represents a significant aspect of implementation, requiring hospitals to maintain records of filter performance testing, replacement schedules, and validation studies. Third-party certification of filtration efficiency becomes essential for regulatory approval, with testing methodologies aligned with ASTM and IEST standards for filter performance evaluation.
Cost-benefit analyses must account for both initial implementation expenses and ongoing compliance costs, including regular testing, documentation, and potential facility modifications to meet evolving standards. Healthcare facilities implementing nanofiber filtration technologies must develop comprehensive compliance strategies that address both current requirements and anticipated regulatory changes in airborne pathogen mitigation standards.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!