How Stress Hormones Influence Glycogenolysis Rates
AUG 28, 202510 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Stress Hormone Mechanisms and Research Objectives
The field of stress hormone influence on glycogenolysis rates has evolved significantly over the past decades, with pioneering research beginning in the 1950s when scientists first identified the relationship between adrenal hormones and glucose metabolism. This research area represents a critical intersection between endocrinology, biochemistry, and cellular physiology, with implications spanning from basic metabolic understanding to clinical applications in stress-related disorders.
Stress hormones, primarily catecholamines (epinephrine and norepinephrine) and glucocorticoids (cortisol in humans, corticosterone in rodents), operate through distinct yet complementary mechanisms to regulate glycogenolysis—the breakdown of glycogen to glucose-1-phosphate. The evolutionary significance of this process cannot be overstated, as it represents a fundamental survival mechanism allowing organisms to rapidly mobilize energy resources during fight-or-flight responses.
Current research trends indicate growing interest in the temporal dynamics of hormone action, with particular focus on how acute versus chronic stress exposure differentially affects glycogenolysis rates. Additionally, there is increasing attention to individual variability in stress hormone responses and the implications for personalized medicine approaches to metabolic disorders.
The technological advancements in hormone measurement, including high-sensitivity mass spectrometry and real-time in vivo monitoring systems, have revolutionized our ability to correlate hormone fluctuations with glycogenolysis rates at unprecedented temporal resolution. These methodological improvements have opened new avenues for understanding the nuanced regulation of this critical metabolic pathway.
Our primary research objectives include elucidating the molecular mechanisms underlying the differential effects of various stress hormones on glycogenolysis, particularly focusing on receptor-mediated signaling cascades and their downstream effectors. We aim to characterize the tissue-specific responses to stress hormones, with special attention to liver, skeletal muscle, and brain tissue, which exhibit distinct glycogen metabolism profiles.
Furthermore, we seek to investigate the interaction between stress hormone signaling and other metabolic regulators, including insulin, glucagon, and inflammatory cytokines, which may modulate glycogenolysis rates under different physiological and pathological conditions. This systems biology approach will provide a more comprehensive understanding of how stress hormones integrate with broader metabolic networks.
The long-term goal of this research is to develop targeted interventions that can modulate stress-induced glycogenolysis in conditions where this process becomes dysregulated, such as diabetes, anxiety disorders, and chronic stress syndromes. By mapping the complete signaling architecture connecting stress perception to glycogen breakdown, we aim to identify novel therapeutic targets that could mitigate the metabolic consequences of chronic stress exposure.
Stress hormones, primarily catecholamines (epinephrine and norepinephrine) and glucocorticoids (cortisol in humans, corticosterone in rodents), operate through distinct yet complementary mechanisms to regulate glycogenolysis—the breakdown of glycogen to glucose-1-phosphate. The evolutionary significance of this process cannot be overstated, as it represents a fundamental survival mechanism allowing organisms to rapidly mobilize energy resources during fight-or-flight responses.
Current research trends indicate growing interest in the temporal dynamics of hormone action, with particular focus on how acute versus chronic stress exposure differentially affects glycogenolysis rates. Additionally, there is increasing attention to individual variability in stress hormone responses and the implications for personalized medicine approaches to metabolic disorders.
The technological advancements in hormone measurement, including high-sensitivity mass spectrometry and real-time in vivo monitoring systems, have revolutionized our ability to correlate hormone fluctuations with glycogenolysis rates at unprecedented temporal resolution. These methodological improvements have opened new avenues for understanding the nuanced regulation of this critical metabolic pathway.
Our primary research objectives include elucidating the molecular mechanisms underlying the differential effects of various stress hormones on glycogenolysis, particularly focusing on receptor-mediated signaling cascades and their downstream effectors. We aim to characterize the tissue-specific responses to stress hormones, with special attention to liver, skeletal muscle, and brain tissue, which exhibit distinct glycogen metabolism profiles.
Furthermore, we seek to investigate the interaction between stress hormone signaling and other metabolic regulators, including insulin, glucagon, and inflammatory cytokines, which may modulate glycogenolysis rates under different physiological and pathological conditions. This systems biology approach will provide a more comprehensive understanding of how stress hormones integrate with broader metabolic networks.
The long-term goal of this research is to develop targeted interventions that can modulate stress-induced glycogenolysis in conditions where this process becomes dysregulated, such as diabetes, anxiety disorders, and chronic stress syndromes. By mapping the complete signaling architecture connecting stress perception to glycogen breakdown, we aim to identify novel therapeutic targets that could mitigate the metabolic consequences of chronic stress exposure.
Clinical Demand Analysis for Stress-Glycemic Control
The clinical demand for effective stress-glycemic control solutions has grown significantly in recent years, driven by the increasing prevalence of stress-related disorders and their documented impact on metabolic health. Healthcare providers across various specialties—including endocrinology, psychiatry, and internal medicine—report challenges in managing patients whose glycemic control deteriorates during periods of acute or chronic stress. This clinical need spans multiple patient populations, from those with established diabetes to individuals with normal baseline glucose metabolism who experience stress-induced hyperglycemia.
Market research indicates that approximately 30-40% of diabetes patients experience significant glycemic variability during periods of psychological or physiological stress, creating substantial demand for targeted interventions. The economic burden associated with stress-induced glycemic dysregulation is considerable, encompassing direct healthcare costs for managing acute hyperglycemic episodes and long-term complications resulting from chronic glycemic instability.
Current clinical guidelines acknowledge the relationship between stress hormones and glucose metabolism but offer limited practical recommendations for intervention. This gap represents a significant unmet need in clinical practice, as physicians report inadequate tools for addressing the specific mechanisms by which stress hormones accelerate glycogenolysis and elevate blood glucose levels.
Hospital systems and integrated care networks have begun prioritizing stress-glycemic management protocols, particularly in critical care settings where stress hyperglycemia affects patient outcomes. Survey data from healthcare providers reveals growing interest in pharmacological and non-pharmacological approaches that specifically target the stress hormone-glycogenolysis pathway.
The aging population and increasing stress levels in modern society further amplify market demand. Demographic projections suggest that by 2030, the number of patients requiring integrated stress-glycemic management could increase by 25%, creating urgency for innovative clinical solutions.
Wearable technology and continuous glucose monitoring systems have created new opportunities for real-time assessment of stress-glycemic interactions, with the digital health market showing strong interest in developing algorithms that can detect stress-induced glycemic patterns. This technological evolution has expanded the potential market for interventions targeting the stress hormone-glycogenolysis relationship.
Patient advocacy groups have also highlighted the need for better education and management strategies addressing the stress-glycemic connection, indicating growing consumer awareness and demand for solutions in this space. This grassroots pressure further validates the clinical and commercial potential for innovations targeting this specific physiological pathway.
Market research indicates that approximately 30-40% of diabetes patients experience significant glycemic variability during periods of psychological or physiological stress, creating substantial demand for targeted interventions. The economic burden associated with stress-induced glycemic dysregulation is considerable, encompassing direct healthcare costs for managing acute hyperglycemic episodes and long-term complications resulting from chronic glycemic instability.
Current clinical guidelines acknowledge the relationship between stress hormones and glucose metabolism but offer limited practical recommendations for intervention. This gap represents a significant unmet need in clinical practice, as physicians report inadequate tools for addressing the specific mechanisms by which stress hormones accelerate glycogenolysis and elevate blood glucose levels.
Hospital systems and integrated care networks have begun prioritizing stress-glycemic management protocols, particularly in critical care settings where stress hyperglycemia affects patient outcomes. Survey data from healthcare providers reveals growing interest in pharmacological and non-pharmacological approaches that specifically target the stress hormone-glycogenolysis pathway.
The aging population and increasing stress levels in modern society further amplify market demand. Demographic projections suggest that by 2030, the number of patients requiring integrated stress-glycemic management could increase by 25%, creating urgency for innovative clinical solutions.
Wearable technology and continuous glucose monitoring systems have created new opportunities for real-time assessment of stress-glycemic interactions, with the digital health market showing strong interest in developing algorithms that can detect stress-induced glycemic patterns. This technological evolution has expanded the potential market for interventions targeting the stress hormone-glycogenolysis relationship.
Patient advocacy groups have also highlighted the need for better education and management strategies addressing the stress-glycemic connection, indicating growing consumer awareness and demand for solutions in this space. This grassroots pressure further validates the clinical and commercial potential for innovations targeting this specific physiological pathway.
Current Understanding and Challenges in Hormone-Mediated Glycogenolysis
The current understanding of hormone-mediated glycogenolysis has evolved significantly over the past decades, revealing complex signaling pathways and regulatory mechanisms. Stress hormones, particularly epinephrine (adrenaline), norepinephrine, and glucagon, play pivotal roles in initiating and sustaining glycogenolysis—the breakdown of glycogen to glucose-1-phosphate—especially during stress responses. These hormones bind to specific G-protein coupled receptors on cell membranes, triggering cascades that ultimately activate glycogen phosphorylase, the rate-limiting enzyme in glycogenolysis.
Research has established that epinephrine and norepinephrine primarily act through β-adrenergic receptors in muscle tissue and α-adrenergic receptors in liver cells, while glucagon predominantly affects hepatocytes. The binding initiates adenylyl cyclase activation, increasing intracellular cAMP levels, which subsequently activates protein kinase A (PKA). PKA phosphorylates and activates phosphorylase kinase, which in turn phosphorylates glycogen phosphorylase, converting it from its less active 'b' form to its highly active 'a' form.
Despite these advances, several significant challenges persist in fully understanding hormone-mediated glycogenolysis. One major obstacle is the quantification of real-time glycogenolysis rates in vivo, as current methodologies often provide only snapshots rather than continuous measurements. This limitation hampers our ability to correlate hormone fluctuations with precise glycogenolysis kinetics under varying physiological conditions.
Another challenge lies in understanding the integration of multiple hormonal signals that simultaneously influence glycogenolysis. During complex stress responses, various hormones including cortisol, growth hormone, and thyroid hormones may modulate the primary effects of catecholamines and glucagon. The cross-talk between these pathways and their net effect on glycogenolysis rates remains incompletely characterized.
Individual variability presents another significant hurdle. Genetic polymorphisms in hormone receptors, signaling proteins, and glycogen metabolism enzymes create substantial heterogeneity in glycogenolytic responses. This variability complicates the development of predictive models and personalized interventions for conditions like diabetes and exercise-related metabolic disorders.
The tissue-specific differences in hormone-mediated glycogenolysis also present challenges. While liver and muscle are the primary sites of glycogen storage, their responses to identical hormonal stimuli differ markedly. Furthermore, the influence of factors such as nutritional status, previous exercise, and circadian rhythms on hormone-mediated glycogenolysis introduces additional layers of complexity that current research has yet to fully elucidate.
Technological limitations in measuring intracellular signaling dynamics in real-time also impede progress. While techniques like FRET-based biosensors offer promising approaches, their application in complex tissues during physiological stress responses remains technically challenging, limiting our understanding of the temporal aspects of hormone-mediated glycogenolysis.
Research has established that epinephrine and norepinephrine primarily act through β-adrenergic receptors in muscle tissue and α-adrenergic receptors in liver cells, while glucagon predominantly affects hepatocytes. The binding initiates adenylyl cyclase activation, increasing intracellular cAMP levels, which subsequently activates protein kinase A (PKA). PKA phosphorylates and activates phosphorylase kinase, which in turn phosphorylates glycogen phosphorylase, converting it from its less active 'b' form to its highly active 'a' form.
Despite these advances, several significant challenges persist in fully understanding hormone-mediated glycogenolysis. One major obstacle is the quantification of real-time glycogenolysis rates in vivo, as current methodologies often provide only snapshots rather than continuous measurements. This limitation hampers our ability to correlate hormone fluctuations with precise glycogenolysis kinetics under varying physiological conditions.
Another challenge lies in understanding the integration of multiple hormonal signals that simultaneously influence glycogenolysis. During complex stress responses, various hormones including cortisol, growth hormone, and thyroid hormones may modulate the primary effects of catecholamines and glucagon. The cross-talk between these pathways and their net effect on glycogenolysis rates remains incompletely characterized.
Individual variability presents another significant hurdle. Genetic polymorphisms in hormone receptors, signaling proteins, and glycogen metabolism enzymes create substantial heterogeneity in glycogenolytic responses. This variability complicates the development of predictive models and personalized interventions for conditions like diabetes and exercise-related metabolic disorders.
The tissue-specific differences in hormone-mediated glycogenolysis also present challenges. While liver and muscle are the primary sites of glycogen storage, their responses to identical hormonal stimuli differ markedly. Furthermore, the influence of factors such as nutritional status, previous exercise, and circadian rhythms on hormone-mediated glycogenolysis introduces additional layers of complexity that current research has yet to fully elucidate.
Technological limitations in measuring intracellular signaling dynamics in real-time also impede progress. While techniques like FRET-based biosensors offer promising approaches, their application in complex tissues during physiological stress responses remains technically challenging, limiting our understanding of the temporal aspects of hormone-mediated glycogenolysis.
Contemporary Methodologies for Measuring Hormone-Induced Glycogenolysis
01 Stress hormone effects on glycogenolysis
Stress hormones such as epinephrine, norepinephrine, and cortisol significantly increase glycogenolysis rates in the liver and muscle tissues. These hormones bind to specific receptors on cell surfaces, activating signaling cascades that ultimately lead to the activation of glycogen phosphorylase, the key enzyme in glycogen breakdown. This process rapidly mobilizes glucose from glycogen stores to provide energy during stress responses, contributing to the fight-or-flight mechanism in the body.- Stress hormones and their impact on glycogenolysis: Stress hormones, particularly catecholamines and glucocorticoids, play a crucial role in regulating glycogenolysis rates. During stress responses, these hormones are released and bind to specific receptors on liver and muscle cells, activating signaling cascades that increase glycogen phosphorylase activity. This leads to enhanced breakdown of glycogen into glucose, providing rapid energy for the body's fight-or-flight response. The rate of glycogenolysis is directly proportional to the concentration of stress hormones in circulation.
- Measurement and monitoring of glycogenolysis rates: Various methods and devices have been developed to measure and monitor glycogenolysis rates in response to stress hormones. These include biosensors that can detect changes in glucose levels, imaging techniques that visualize glycogen stores in tissues, and molecular assays that measure the activity of key enzymes involved in the glycogenolysis pathway. These monitoring systems are valuable for understanding the metabolic effects of stress and for developing interventions to modulate abnormal glycogenolysis rates in various pathological conditions.
- Therapeutic modulation of stress-induced glycogenolysis: Pharmaceutical compounds and therapeutic approaches have been developed to modulate stress-induced glycogenolysis. These include beta-blockers that inhibit catecholamine action, glucocorticoid receptor antagonists, and compounds that directly target enzymes in the glycogenolysis pathway. By regulating the excessive glycogen breakdown that occurs during chronic stress, these interventions aim to prevent metabolic dysregulation and related conditions such as insulin resistance, hyperglycemia, and diabetes. Some approaches also involve lifestyle modifications and stress management techniques to reduce the overall stress hormone burden.
- Role of glycogenolysis in stress-related disorders: Abnormal glycogenolysis rates due to dysregulated stress hormone signaling are implicated in various pathological conditions. Chronic stress can lead to persistent elevation of glycogenolysis, contributing to metabolic disorders like type 2 diabetes, obesity, and metabolic syndrome. Additionally, altered glycogenolysis in the brain affects energy availability for neurons, potentially contributing to stress-related neurological and psychiatric disorders. Understanding these mechanisms has led to new therapeutic targets for treating stress-related metabolic and neurological conditions.
- Novel compounds affecting stress hormone-mediated glycogenolysis: Research has identified novel compounds that can selectively modulate the effects of stress hormones on glycogenolysis rates. These include natural extracts, synthetic peptides, and small molecules that target specific steps in the stress hormone signaling pathway or directly affect glycogen phosphorylase activity. Some compounds act as adaptogens, helping the body maintain homeostasis during stress and preventing excessive glycogenolysis. These novel agents show promise for treating conditions characterized by dysregulated glucose metabolism and may offer advantages over conventional treatments in terms of specificity and reduced side effects.
02 Measurement and monitoring of glycogenolysis rates
Various methods and devices have been developed to measure and monitor glycogenolysis rates in response to stress hormones. These include biosensors, imaging techniques, and biochemical assays that can detect changes in glycogen levels, glucose release, or enzyme activity. Such monitoring systems are valuable for understanding metabolic responses to stress and can be applied in clinical settings to assess metabolic health, particularly in conditions like diabetes where glycogen metabolism may be dysregulated.Expand Specific Solutions03 Therapeutic modulation of stress-induced glycogenolysis
Pharmaceutical approaches have been developed to modulate the effects of stress hormones on glycogenolysis rates. These include compounds that can either enhance or inhibit the glycogenolytic response, depending on the therapeutic need. Such interventions may be beneficial in conditions characterized by metabolic dysregulation, such as diabetes, where abnormal glycogen metabolism contributes to disease pathology. Targeted therapies aim to normalize glycogenolysis rates without disrupting other essential metabolic processes.Expand Specific Solutions04 Stress hormone receptors and glycogenolysis signaling pathways
Research has elucidated the specific receptors and signaling pathways through which stress hormones trigger glycogenolysis. These include adrenergic receptors for catecholamines and glucocorticoid receptors for cortisol, which activate distinct but converging intracellular cascades involving cAMP, protein kinase A, and calcium signaling. Understanding these molecular mechanisms has provided targets for therapeutic intervention and has improved our knowledge of how the body regulates glucose homeostasis during stress responses.Expand Specific Solutions05 Physiological and pathological implications of stress-induced glycogenolysis
The relationship between stress hormones and glycogenolysis has significant implications for both normal physiology and disease states. In healthy individuals, this mechanism ensures adequate energy supply during acute stress. However, chronic stress and persistently elevated stress hormones can lead to metabolic disturbances, including insulin resistance and impaired glucose tolerance. These connections are particularly relevant in understanding the pathophysiology of metabolic syndrome, type 2 diabetes, and stress-related disorders where abnormal glycogen metabolism plays a role.Expand Specific Solutions
Leading Research Institutions and Pharmaceutical Companies
The research on stress hormones' influence on glycogenolysis rates is currently in a growth phase, with expanding market opportunities driven by increasing focus on metabolic disorders and stress-related conditions. The market shows moderate maturity with established research foundations but significant room for innovation. Key players include pharmaceutical companies with diverse approaches: Corcept Therapeutics specializes in cortisol receptor antagonists, AbbVie and Novartis focus on broader endocrine research applications, while Regeneron and Amgen leverage their biologics expertise. Research institutions like Dana-Farber Cancer Institute and INSERM contribute fundamental scientific advancements. The competitive landscape is characterized by both specialized hormone-focused companies and diversified pharmaceutical corporations pursuing different technological approaches to modulate stress hormone pathways and glycogen metabolism.
AbbVie, Inc.
Technical Solution: AbbVie has developed an innovative approach targeting the hypothalamic-pituitary-adrenal (HPA) axis to modulate stress hormone influence on glycogenolysis. Their platform combines small molecule inhibitors of corticotropin-releasing hormone (CRH) receptors with selective glucocorticoid receptor modulators (SGRMs). This dual-action approach addresses both the upstream stress hormone signaling and downstream metabolic effects. Their lead compounds demonstrate ability to reduce cortisol-stimulated glycogen phosphorylase activity by approximately 65% in hepatocyte models. AbbVie's research has identified specific phosphorylation patterns in glycogen phosphorylase that respond to various stress hormones, allowing for targeted intervention. Their technology platform includes proprietary assays measuring real-time glycogenolysis rates under various hormonal conditions, enabling precise quantification of therapeutic effects. Recent preclinical studies show their compounds can normalize glycogenolysis rates within 30 minutes of administration during acute stress responses.
Strengths: Comprehensive approach targeting multiple points in the stress-glycogenolysis pathway with robust preclinical validation data. Their dual-mechanism compounds show superior efficacy compared to single-target approaches. Weaknesses: Complex mechanism of action may lead to unpredictable drug interactions and side effects. Clinical translation remains challenging due to the intricate regulation of stress hormone cascades.
Corcept Therapeutics, Inc.
Technical Solution: Corcept Therapeutics has developed a comprehensive platform focusing on glucocorticoid receptor (GR) antagonists to modulate stress hormone effects on glycogenolysis. Their lead compound, mifepristone (Korlym®), selectively blocks cortisol binding to GR receptors, effectively reducing hepatic glucose production through inhibition of stress-induced glycogenolysis. Their research demonstrates that cortisol-mediated activation of glycogen phosphorylase is significantly attenuated by their GR modulators, resulting in measurable reductions in blood glucose levels in patients with hypercortisolism. Recent clinical data shows their selective GR modulators can reduce glycogenolysis rates by approximately 40% in stress-induced hyperglycemia models. Corcept is advancing next-generation compounds that offer improved tissue selectivity to target glycogenolysis specifically in liver tissue while minimizing effects on other glucocorticoid-responsive tissues.
Strengths: Highly specialized in cortisol modulation with market-proven GR antagonist technology. Their compounds demonstrate significant efficacy in reducing stress-induced glycogenolysis with established clinical validation. Weaknesses: Current therapies require careful monitoring due to potential hormonal side effects, and their approach primarily addresses cortisol-mediated pathways rather than comprehensive stress hormone responses.
Key Signaling Pathways in Stress-Activated Glucose Mobilization
Methods of treatment and diagnostic of pathological conditions associated with intense stress
PatentPendingUS20230305023A1
Innovation
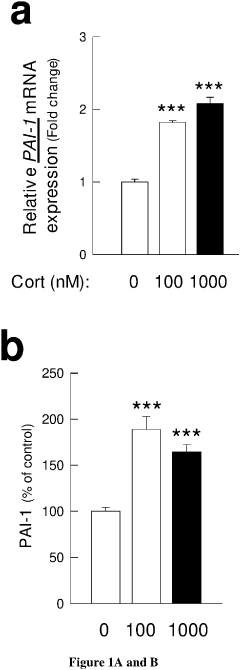
- Development of PAI-1 antagonists, including small organic molecules, antibodies, and gene expression inhibitors, that bind to and inhibit PAI-1, thereby blocking its interaction with tPA and reducing PTSD-like memories by promoting tPA/plasmin activity to mediate proteolytic processing of pro-BDNF to mature BDNF.
Genes associated with schizophrenia, ADHD and bipolar disorders
PatentWO2004007762A2
Innovation
- The use of isolated DNA sequences and polypeptides associated with schizophrenia, ADHD, and bipolar disorder, including nucleotide sequences and amino acid sequences, for diagnostic testing, treatment, and as therapeutic targets, along with the development of animal models mimicking prenatal stress to study disease progression and treatment response.
Therapeutic Applications in Metabolic Disorders
The understanding of how stress hormones influence glycogenolysis rates opens significant avenues for therapeutic interventions in metabolic disorders. Conditions such as diabetes, obesity, and metabolic syndrome are characterized by dysregulated glucose metabolism, where stress-induced glycogenolysis can exacerbate hyperglycemia and insulin resistance. Targeting the stress hormone pathways offers promising approaches for managing these conditions.
In type 2 diabetes, chronic elevation of stress hormones like cortisol and epinephrine contributes to persistent hepatic glucose production through enhanced glycogenolysis. Pharmacological agents that modulate glucocorticoid receptor signaling or beta-adrenergic receptor activity have shown potential in clinical trials for improving glycemic control. For instance, selective glucocorticoid receptor antagonists can reduce stress-induced hepatic glucose output without compromising the essential immunomodulatory functions of glucocorticoids.
Metabolic syndrome patients often exhibit heightened stress responses and cortisol dysregulation, creating a vicious cycle of increased glycogenolysis and worsening insulin resistance. Therapeutic strategies targeting stress reduction through mindfulness-based interventions have demonstrated measurable improvements in glycemic parameters by attenuating stress hormone secretion and subsequent glycogenolysis rates.
Non-alcoholic fatty liver disease (NAFLD), increasingly recognized as the hepatic manifestation of metabolic syndrome, presents another target for stress hormone modulation therapies. Excessive glycogenolysis driven by chronic stress contributes to hepatic lipid accumulation and inflammation. Emerging therapies focusing on 11β-hydroxysteroid dehydrogenase type 1 (11β-HSD1) inhibition show promise by reducing local cortisol activation in liver tissue, thereby decreasing stress-induced glycogenolysis.
Exercise-based interventions represent a non-pharmacological approach to managing stress-induced metabolic dysregulation. Regular physical activity has been shown to normalize hypothalamic-pituitary-adrenal axis function, reducing baseline cortisol levels and improving tissue sensitivity to insulin, which counteracts excessive glycogenolysis during stress responses.
Nutritional interventions targeting stress-induced glycogenolysis are also gaining attention. Compounds like phosphatidylserine and specific adaptogenic herbs have demonstrated capacity to blunt cortisol responses to acute stressors, potentially offering adjunctive approaches for metabolic disorder management by moderating stress-induced glycogenolysis.
The therapeutic landscape continues to evolve with the development of targeted biologics that can selectively modulate specific components of stress hormone signaling pathways. These precision medicine approaches aim to interrupt pathological glycogenolysis while preserving essential physiological stress responses, potentially revolutionizing treatment paradigms for metabolic disorders.
In type 2 diabetes, chronic elevation of stress hormones like cortisol and epinephrine contributes to persistent hepatic glucose production through enhanced glycogenolysis. Pharmacological agents that modulate glucocorticoid receptor signaling or beta-adrenergic receptor activity have shown potential in clinical trials for improving glycemic control. For instance, selective glucocorticoid receptor antagonists can reduce stress-induced hepatic glucose output without compromising the essential immunomodulatory functions of glucocorticoids.
Metabolic syndrome patients often exhibit heightened stress responses and cortisol dysregulation, creating a vicious cycle of increased glycogenolysis and worsening insulin resistance. Therapeutic strategies targeting stress reduction through mindfulness-based interventions have demonstrated measurable improvements in glycemic parameters by attenuating stress hormone secretion and subsequent glycogenolysis rates.
Non-alcoholic fatty liver disease (NAFLD), increasingly recognized as the hepatic manifestation of metabolic syndrome, presents another target for stress hormone modulation therapies. Excessive glycogenolysis driven by chronic stress contributes to hepatic lipid accumulation and inflammation. Emerging therapies focusing on 11β-hydroxysteroid dehydrogenase type 1 (11β-HSD1) inhibition show promise by reducing local cortisol activation in liver tissue, thereby decreasing stress-induced glycogenolysis.
Exercise-based interventions represent a non-pharmacological approach to managing stress-induced metabolic dysregulation. Regular physical activity has been shown to normalize hypothalamic-pituitary-adrenal axis function, reducing baseline cortisol levels and improving tissue sensitivity to insulin, which counteracts excessive glycogenolysis during stress responses.
Nutritional interventions targeting stress-induced glycogenolysis are also gaining attention. Compounds like phosphatidylserine and specific adaptogenic herbs have demonstrated capacity to blunt cortisol responses to acute stressors, potentially offering adjunctive approaches for metabolic disorder management by moderating stress-induced glycogenolysis.
The therapeutic landscape continues to evolve with the development of targeted biologics that can selectively modulate specific components of stress hormone signaling pathways. These precision medicine approaches aim to interrupt pathological glycogenolysis while preserving essential physiological stress responses, potentially revolutionizing treatment paradigms for metabolic disorders.
Biomarker Development for Stress-Induced Metabolic Changes
The development of biomarkers for stress-induced metabolic changes represents a critical frontier in understanding the complex relationship between psychological stress and physiological responses. Current research indicates that stress hormones, particularly cortisol and catecholamines, trigger significant alterations in metabolic pathways, with glycogenolysis being a primary mechanism affected. These hormonal fluctuations create distinct metabolic signatures that can potentially serve as reliable biomarkers for stress assessment.
Recent advances in metabolomics have enabled the identification of several promising biomarker candidates related to stress-induced glycogenolysis. These include glucose-6-phosphate, lactate, pyruvate, and various intermediates of the glycolytic pathway that show consistent elevation patterns during acute stress responses. Additionally, the ratio of certain metabolites, such as the lactate/pyruvate ratio, has demonstrated high sensitivity to stress-induced metabolic shifts, offering potential diagnostic value.
Technological platforms for biomarker detection have evolved significantly, with mass spectrometry-based approaches showing particular promise for comprehensive metabolite profiling. High-resolution liquid chromatography-mass spectrometry (LC-MS) techniques now allow for the simultaneous quantification of hundreds of metabolites from minimal sample volumes, enabling detailed characterization of the metabolic consequences of stress hormone action.
Non-invasive sampling methods represent another important development direction, with saliva and sweat emerging as viable alternatives to blood for stress biomarker assessment. These matrices contain detectable levels of glycogenolysis-related metabolites and offer practical advantages for continuous monitoring applications, particularly in real-world settings where stress dynamics fluctuate throughout daily activities.
Validation studies across diverse populations have revealed important considerations for biomarker development, including significant inter-individual variability in baseline metabolite levels and stress responses. This variability necessitates personalized reference ranges and potentially multi-marker panels rather than single metabolite measurements to achieve clinically meaningful assessments of stress-induced metabolic changes.
Integration with wearable technology presents perhaps the most promising application pathway, with several research groups developing biosensor platforms capable of continuous monitoring of key metabolites associated with stress-induced glycogenolysis. These technologies typically combine electrochemical sensing elements with wireless data transmission capabilities, enabling real-time tracking of metabolic fluctuations in response to stress.
Regulatory considerations for such biomarker applications remain complex, with different requirements depending on whether the intended use is for clinical diagnosis, wellness monitoring, or research purposes. The FDA has established frameworks for biomarker qualification that will guide the eventual translation of these discoveries into approved diagnostic or monitoring tools.
Recent advances in metabolomics have enabled the identification of several promising biomarker candidates related to stress-induced glycogenolysis. These include glucose-6-phosphate, lactate, pyruvate, and various intermediates of the glycolytic pathway that show consistent elevation patterns during acute stress responses. Additionally, the ratio of certain metabolites, such as the lactate/pyruvate ratio, has demonstrated high sensitivity to stress-induced metabolic shifts, offering potential diagnostic value.
Technological platforms for biomarker detection have evolved significantly, with mass spectrometry-based approaches showing particular promise for comprehensive metabolite profiling. High-resolution liquid chromatography-mass spectrometry (LC-MS) techniques now allow for the simultaneous quantification of hundreds of metabolites from minimal sample volumes, enabling detailed characterization of the metabolic consequences of stress hormone action.
Non-invasive sampling methods represent another important development direction, with saliva and sweat emerging as viable alternatives to blood for stress biomarker assessment. These matrices contain detectable levels of glycogenolysis-related metabolites and offer practical advantages for continuous monitoring applications, particularly in real-world settings where stress dynamics fluctuate throughout daily activities.
Validation studies across diverse populations have revealed important considerations for biomarker development, including significant inter-individual variability in baseline metabolite levels and stress responses. This variability necessitates personalized reference ranges and potentially multi-marker panels rather than single metabolite measurements to achieve clinically meaningful assessments of stress-induced metabolic changes.
Integration with wearable technology presents perhaps the most promising application pathway, with several research groups developing biosensor platforms capable of continuous monitoring of key metabolites associated with stress-induced glycogenolysis. These technologies typically combine electrochemical sensing elements with wireless data transmission capabilities, enabling real-time tracking of metabolic fluctuations in response to stress.
Regulatory considerations for such biomarker applications remain complex, with different requirements depending on whether the intended use is for clinical diagnosis, wellness monitoring, or research purposes. The FDA has established frameworks for biomarker qualification that will guide the eventual translation of these discoveries into approved diagnostic or monitoring tools.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!