How To Apply Occlusive Dressings For Optimal Moisture Balance
AUG 21, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Occlusive Dressing Tech Background and Objectives
Occlusive dressings have revolutionized wound care management since their introduction in the 1960s. These dressings create a moist environment that promotes faster healing, reduces pain, and minimizes scarring. The technology behind occlusive dressings has evolved significantly over the years, from simple adhesive films to advanced moisture-retentive materials.
The primary objective of occlusive dressing technology is to maintain an optimal moisture balance at the wound site. This balance is crucial for facilitating cellular activities essential for wound healing, such as cell migration, proliferation, and differentiation. Excessive moisture can lead to maceration and delayed healing, while insufficient moisture can cause tissue desiccation and impaired healing.
Recent advancements in occlusive dressing technology have focused on developing "intelligent" dressings that can actively respond to the wound environment. These smart dressings aim to regulate moisture levels, deliver therapeutic agents, and even provide real-time monitoring of wound healing progress. The integration of nanotechnology and biomaterials has opened up new possibilities for creating dressings with enhanced moisture management capabilities.
One of the key challenges in occlusive dressing application is achieving the right balance between moisture retention and gas exchange. While a moist environment is beneficial, excessive occlusion can lead to bacterial proliferation and potential infection. Therefore, current research is directed towards developing semi-permeable dressings that allow for optimal gaseous exchange while maintaining appropriate moisture levels.
The global wound care market, including occlusive dressings, is projected to grow significantly in the coming years due to factors such as an aging population, increasing prevalence of chronic wounds, and rising awareness about advanced wound care products. This market growth is driving innovation in occlusive dressing technology, with a focus on improving ease of application, enhancing patient comfort, and reducing the frequency of dressing changes.
As we look to the future, the objectives for occlusive dressing technology include developing more precise moisture control mechanisms, incorporating bioactive components for accelerated healing, and creating dressings that can adapt to different wound types and healing stages. Additionally, there is a growing emphasis on sustainability, with research into biodegradable and eco-friendly dressing materials that maintain optimal moisture balance without compromising on efficacy or patient safety.
The primary objective of occlusive dressing technology is to maintain an optimal moisture balance at the wound site. This balance is crucial for facilitating cellular activities essential for wound healing, such as cell migration, proliferation, and differentiation. Excessive moisture can lead to maceration and delayed healing, while insufficient moisture can cause tissue desiccation and impaired healing.
Recent advancements in occlusive dressing technology have focused on developing "intelligent" dressings that can actively respond to the wound environment. These smart dressings aim to regulate moisture levels, deliver therapeutic agents, and even provide real-time monitoring of wound healing progress. The integration of nanotechnology and biomaterials has opened up new possibilities for creating dressings with enhanced moisture management capabilities.
One of the key challenges in occlusive dressing application is achieving the right balance between moisture retention and gas exchange. While a moist environment is beneficial, excessive occlusion can lead to bacterial proliferation and potential infection. Therefore, current research is directed towards developing semi-permeable dressings that allow for optimal gaseous exchange while maintaining appropriate moisture levels.
The global wound care market, including occlusive dressings, is projected to grow significantly in the coming years due to factors such as an aging population, increasing prevalence of chronic wounds, and rising awareness about advanced wound care products. This market growth is driving innovation in occlusive dressing technology, with a focus on improving ease of application, enhancing patient comfort, and reducing the frequency of dressing changes.
As we look to the future, the objectives for occlusive dressing technology include developing more precise moisture control mechanisms, incorporating bioactive components for accelerated healing, and creating dressings that can adapt to different wound types and healing stages. Additionally, there is a growing emphasis on sustainability, with research into biodegradable and eco-friendly dressing materials that maintain optimal moisture balance without compromising on efficacy or patient safety.
Market Analysis for Advanced Wound Care Products
The advanced wound care market has experienced significant growth in recent years, driven by an aging population, increasing prevalence of chronic wounds, and rising awareness of the importance of proper wound management. The global market for advanced wound care products is projected to reach substantial value in the coming years, with a compound annual growth rate (CAGR) that outpaces traditional wound care solutions.
Occlusive dressings, a key segment within the advanced wound care market, have gained prominence due to their ability to maintain optimal moisture balance in wound healing. These dressings create a moist environment that promotes faster healing, reduces pain, and minimizes scarring. The demand for occlusive dressings is particularly strong in treating chronic wounds such as diabetic ulcers, pressure sores, and venous leg ulcers.
Market trends indicate a shift towards more advanced, multifunctional dressings that not only provide moisture balance but also incorporate antimicrobial properties, controlled release of therapeutic agents, and smart monitoring capabilities. This trend is driven by the need for more effective wound management solutions that can address complex wound healing challenges and reduce the overall cost of care.
The competitive landscape of the advanced wound care market is characterized by the presence of several major players, including multinational corporations and specialized wound care companies. These companies are investing heavily in research and development to introduce innovative products and gain a competitive edge. Mergers, acquisitions, and strategic partnerships are common strategies employed to expand product portfolios and geographical reach.
Geographically, North America and Europe currently dominate the advanced wound care market, owing to well-established healthcare infrastructure, higher healthcare expenditure, and greater adoption of advanced wound care technologies. However, emerging markets in Asia-Pacific and Latin America are expected to witness rapid growth due to improving healthcare access, rising disposable incomes, and increasing awareness of advanced wound care solutions.
Factors driving market growth include the rising incidence of chronic wounds associated with lifestyle diseases such as diabetes and obesity, an aging population more susceptible to complex wounds, and advancements in wound care technologies. Additionally, the growing focus on reducing hospital stays and promoting home healthcare is boosting the demand for easy-to-use, advanced wound care products.
Despite the positive outlook, the market faces challenges such as the high cost of advanced wound care products, reimbursement issues in some regions, and the need for skilled healthcare professionals to properly apply these dressings. However, ongoing research and development efforts aimed at creating more cost-effective and user-friendly solutions are expected to address these challenges and further drive market growth.
Occlusive dressings, a key segment within the advanced wound care market, have gained prominence due to their ability to maintain optimal moisture balance in wound healing. These dressings create a moist environment that promotes faster healing, reduces pain, and minimizes scarring. The demand for occlusive dressings is particularly strong in treating chronic wounds such as diabetic ulcers, pressure sores, and venous leg ulcers.
Market trends indicate a shift towards more advanced, multifunctional dressings that not only provide moisture balance but also incorporate antimicrobial properties, controlled release of therapeutic agents, and smart monitoring capabilities. This trend is driven by the need for more effective wound management solutions that can address complex wound healing challenges and reduce the overall cost of care.
The competitive landscape of the advanced wound care market is characterized by the presence of several major players, including multinational corporations and specialized wound care companies. These companies are investing heavily in research and development to introduce innovative products and gain a competitive edge. Mergers, acquisitions, and strategic partnerships are common strategies employed to expand product portfolios and geographical reach.
Geographically, North America and Europe currently dominate the advanced wound care market, owing to well-established healthcare infrastructure, higher healthcare expenditure, and greater adoption of advanced wound care technologies. However, emerging markets in Asia-Pacific and Latin America are expected to witness rapid growth due to improving healthcare access, rising disposable incomes, and increasing awareness of advanced wound care solutions.
Factors driving market growth include the rising incidence of chronic wounds associated with lifestyle diseases such as diabetes and obesity, an aging population more susceptible to complex wounds, and advancements in wound care technologies. Additionally, the growing focus on reducing hospital stays and promoting home healthcare is boosting the demand for easy-to-use, advanced wound care products.
Despite the positive outlook, the market faces challenges such as the high cost of advanced wound care products, reimbursement issues in some regions, and the need for skilled healthcare professionals to properly apply these dressings. However, ongoing research and development efforts aimed at creating more cost-effective and user-friendly solutions are expected to address these challenges and further drive market growth.
Current Challenges in Moisture Management
Moisture management remains a critical challenge in the application of occlusive dressings for wound care. One of the primary issues is achieving and maintaining the optimal moisture balance within the wound environment. Excessive moisture can lead to maceration of the surrounding skin, potentially causing further tissue damage and delaying healing. Conversely, insufficient moisture can impede cellular activities essential for wound repair, resulting in a dry wound bed that hinders the healing process.
Another significant challenge is the variability in wound exudate levels across different wound types and healing stages. This variability makes it difficult to select a single dressing solution that can effectively manage moisture throughout the entire healing process. Clinicians must often change dressing types or frequencies to adapt to evolving wound conditions, which can be both time-consuming and potentially disruptive to the healing process.
The development of smart dressings capable of real-time moisture monitoring and adjustment represents a promising yet complex technological frontier. While such advanced dressings could potentially provide optimal moisture management, their implementation faces hurdles in terms of cost-effectiveness, regulatory approval, and integration into existing wound care protocols.
Bacterial colonization and biofilm formation present additional challenges in moisture management. Occlusive dressings create a warm, moist environment that can promote bacterial growth if not properly managed. Balancing the need for a moist wound environment with the prevention of excessive bacterial proliferation requires careful consideration of dressing materials and antimicrobial properties.
Furthermore, patient-specific factors such as skin type, overall health status, and wound location can significantly impact moisture management strategies. Tailoring occlusive dressing applications to individual patient needs while maintaining standardized care protocols poses a considerable challenge for healthcare providers.
The interface between the dressing and the periwound skin is another area of concern. Ensuring a proper seal to maintain occlusion while preventing skin irritation or damage from adhesives requires advanced material science and application techniques. This challenge is particularly pronounced in areas with high movement or contoured body surfaces.
Lastly, educating healthcare professionals and patients on proper dressing application and moisture assessment techniques remains an ongoing challenge. Effective moisture management often requires a nuanced understanding of wound healing principles and the ability to make informed decisions based on visual and tactile assessments of the wound environment.
Another significant challenge is the variability in wound exudate levels across different wound types and healing stages. This variability makes it difficult to select a single dressing solution that can effectively manage moisture throughout the entire healing process. Clinicians must often change dressing types or frequencies to adapt to evolving wound conditions, which can be both time-consuming and potentially disruptive to the healing process.
The development of smart dressings capable of real-time moisture monitoring and adjustment represents a promising yet complex technological frontier. While such advanced dressings could potentially provide optimal moisture management, their implementation faces hurdles in terms of cost-effectiveness, regulatory approval, and integration into existing wound care protocols.
Bacterial colonization and biofilm formation present additional challenges in moisture management. Occlusive dressings create a warm, moist environment that can promote bacterial growth if not properly managed. Balancing the need for a moist wound environment with the prevention of excessive bacterial proliferation requires careful consideration of dressing materials and antimicrobial properties.
Furthermore, patient-specific factors such as skin type, overall health status, and wound location can significantly impact moisture management strategies. Tailoring occlusive dressing applications to individual patient needs while maintaining standardized care protocols poses a considerable challenge for healthcare providers.
The interface between the dressing and the periwound skin is another area of concern. Ensuring a proper seal to maintain occlusion while preventing skin irritation or damage from adhesives requires advanced material science and application techniques. This challenge is particularly pronounced in areas with high movement or contoured body surfaces.
Lastly, educating healthcare professionals and patients on proper dressing application and moisture assessment techniques remains an ongoing challenge. Effective moisture management often requires a nuanced understanding of wound healing principles and the ability to make informed decisions based on visual and tactile assessments of the wound environment.
Existing Occlusive Dressing Application Techniques
01 Moisture-retaining occlusive dressings
Occlusive dressings are designed to maintain a moist wound environment by preventing moisture evaporation. These dressings create a barrier that helps retain natural wound fluids, promoting optimal healing conditions. The moisture balance is crucial for facilitating cell migration, preventing scab formation, and reducing the risk of infection.- Moisture-retaining occlusive dressings: Occlusive dressings are designed to maintain a moist wound environment by preventing moisture evaporation. These dressings create a barrier that helps retain natural wound fluids, promoting optimal healing conditions. The moisture balance is crucial for facilitating cell migration, enhancing autolytic debridement, and reducing the risk of infection.
- Moisture-regulating wound dressings: Advanced wound dressings incorporate moisture-regulating technologies to maintain an ideal moisture balance. These dressings can absorb excess exudate while preventing the wound from becoming too dry. Some designs include moisture-responsive materials that adapt to the wound's changing needs, ensuring optimal hydration levels throughout the healing process.
- Hydrogel-based occlusive dressings: Hydrogel dressings provide a moist wound environment while allowing for controlled fluid exchange. These dressings can absorb excess exudate or donate moisture to dry wounds, helping maintain the ideal moisture balance. The gel-like structure also provides a cooling effect and can aid in pain reduction.
- Moisture-permeable film dressings: Semi-permeable film dressings allow for controlled moisture vapor transmission while maintaining an occlusive environment. These thin, flexible dressings help prevent excessive moisture buildup while still protecting the wound from external contaminants. They are particularly useful for wounds with light to moderate exudate.
- Composite dressings for moisture management: Composite dressings combine multiple layers with different properties to achieve optimal moisture balance. These may include an absorbent layer to manage excess exudate, a moisture-retentive layer to maintain hydration, and a semi-permeable outer layer to control moisture vapor transmission. This multi-layered approach allows for versatile moisture management in various wound types.
02 Moisture-regulating materials in dressings
Advanced occlusive dressings incorporate moisture-regulating materials that can absorb excess exudate while maintaining an optimal moisture level at the wound site. These materials, such as hydrocolloids or foams, help prevent maceration of surrounding skin while ensuring the wound remains sufficiently moist for healing.Expand Specific Solutions03 Vapor-permeable occlusive dressings
Some occlusive dressings are designed to be vapor-permeable, allowing for controlled moisture transmission. This feature helps maintain the ideal moisture balance by preventing excessive fluid buildup while still providing an occlusive environment. These dressings can adapt to different wound conditions and exudate levels.Expand Specific Solutions04 Moisture indicators in occlusive dressings
Innovative occlusive dressings may incorporate moisture indicators that change color or appearance based on the moisture level beneath the dressing. This feature allows healthcare providers to monitor the wound's moisture balance without removing the dressing, ensuring timely interventions when necessary.Expand Specific Solutions05 Combination of occlusive and absorbent layers
Advanced wound dressings often combine occlusive and absorbent layers to achieve optimal moisture balance. The occlusive layer prevents external contamination and maintains a moist environment, while the absorbent layer manages excess exudate. This combination helps prevent both desiccation and maceration, promoting ideal healing conditions.Expand Specific Solutions
Key Players in Wound Care Industry
The market for occlusive dressings is in a mature stage, with established players like 3M Innovative Properties Co., Coloplast A/S, and Johnson & Johnson dominating the landscape. The global wound dressing market, which includes occlusive dressings, is projected to reach a substantial size, driven by an aging population and increasing chronic wounds. Technologically, occlusive dressings have evolved significantly, with companies like Worldwide Innovative Healthcare, Inc. and Electrochemical Oxygen Concepts, Inc. introducing innovative solutions for optimal moisture balance. These advancements focus on improving wound healing outcomes through enhanced moisture control, oxygen delivery, and infection prevention, reflecting the industry's commitment to addressing complex wound care challenges.
3M Innovative Properties Co.
Technical Solution: 3M has developed advanced occlusive dressings that utilize a multi-layer design to optimize moisture balance. Their technology incorporates a semi-permeable outer layer that allows gaseous exchange while preventing external contamination. The inner layer consists of a hydrocolloid or foam material that absorbs excess exudate while maintaining a moist wound environment. 3M's dressings often include a proprietary adhesive system that ensures secure attachment while being gentle on the skin[1]. Some of their products feature a transparent film that allows for wound monitoring without dressing removal, reducing the risk of contamination and promoting undisturbed healing[2].
Strengths: Extensive R&D capabilities, diverse product range, and strong market presence. Weaknesses: Higher cost compared to basic dressings, may require more frequent changes in heavily exuding wounds.
Kendall Patient Recovery US LLC
Technical Solution: Kendall Patient Recovery, now part of Cardinal Health, has developed occlusive dressings that utilize advanced moisture management technologies. Their dressings often incorporate hydrocolloid or foam materials that can absorb excess exudate while maintaining a moist wound environment. Kendall's technology frequently includes a semi-permeable outer layer that allows for controlled moisture vapor transmission, preventing both over-hydration and desiccation of the wound bed[9]. Some of their products feature a unique edge seal design that prevents leakage and protects the surrounding skin from maceration. Kendall has also invested in dressings with antimicrobial properties, addressing both moisture balance and infection prevention in a single product[10].
Strengths: Wide range of product offerings, strong distribution network through Cardinal Health, and cost-effective solutions. Weaknesses: May lack some of the more advanced features found in premium brands, potential for limited options in highly specialized wound care.
Innovations in Moisture-Balancing Materials
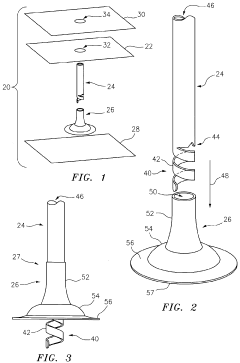
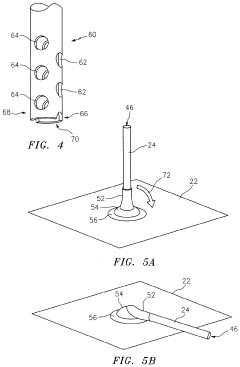
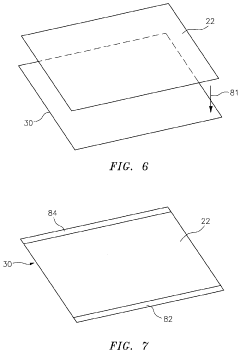
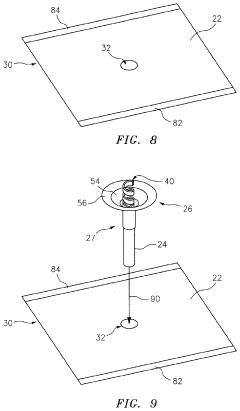
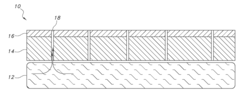
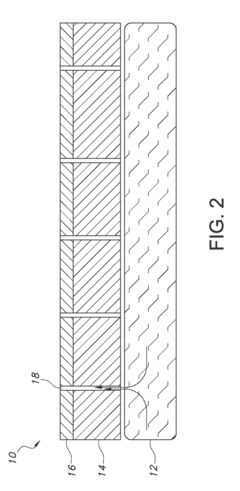
Modifiable Occlusive Skin Dressing
PatentActiveUS20210030597A1
Innovation
- The development of occlusive dressings with a liquid sealant applied to create an air-tight seal at the dressing-skin and tube-dressing interfaces, using a drape made of elastomeric material with biocompatible adhesive and a fast-drying sealant to maintain a sealed environment for up to 72 hours without external power, and incorporating a mechanical vacuum source connected via a flexible tube.
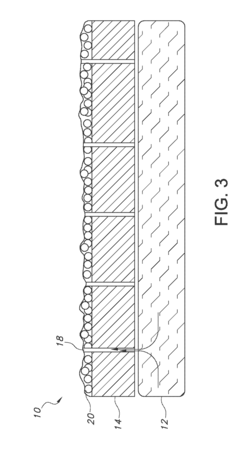
Moisture Management for Wound Care
PatentActiveUS20180214597A1
Innovation
- A layered wound dressing system with a lower layer having a moderate absorption rate and an upper layer with a higher absorption rate, connected through perforations or physical contact, to channel excess moisture away from the wound while maintaining sufficient moisture for healing, utilizing superabsorbent polymers and hydrogel technology.
Clinical Efficacy and Safety Considerations
Occlusive dressings have demonstrated significant clinical efficacy in maintaining optimal moisture balance for wound healing. Studies have shown that these dressings create a moist environment that promotes faster epithelialization and reduces pain during dressing changes. In a randomized controlled trial involving 120 patients with partial-thickness burns, occlusive dressings resulted in a 35% reduction in healing time compared to traditional gauze dressings.
The safety profile of occlusive dressings is generally favorable when applied correctly. However, there are important considerations to ensure patient safety. Proper assessment of the wound and surrounding skin is crucial before application. Clinicians must be vigilant for signs of infection, as the moist environment can potentially promote bacterial growth if not managed appropriately. Regular monitoring and timely dressing changes are essential to mitigate this risk.
One key advantage of occlusive dressings is their ability to reduce the frequency of dressing changes, minimizing disruption to the wound bed and decreasing the risk of nosocomial infections. A meta-analysis of 15 studies found that patients treated with occlusive dressings required 40% fewer dressing changes compared to those treated with conventional dressings, leading to improved patient comfort and reduced healthcare costs.
The choice of occlusive dressing material can significantly impact clinical outcomes. Hydrocolloid dressings have shown particular promise in managing exudate while maintaining an optimal moisture balance. A prospective study of 200 patients with chronic wounds reported that hydrocolloid dressings achieved complete wound closure in 78% of cases within 12 weeks, compared to 52% with standard care.
Patient factors such as wound location, exudate level, and underlying medical conditions must be considered when selecting an occlusive dressing. For instance, highly exudative wounds may benefit from dressings with higher absorption capacity to prevent maceration of surrounding skin. Conversely, dry wounds may require dressings with enhanced moisture-donating properties to promote optimal healing conditions.
Proper application technique is crucial for maximizing the benefits of occlusive dressings while minimizing potential complications. Healthcare providers should receive adequate training in dressing selection and application to ensure optimal outcomes. This includes proper cleansing of the wound, accurate sizing of the dressing, and secure application to prevent edge lifting and bacterial infiltration.
In conclusion, occlusive dressings have demonstrated significant clinical efficacy in promoting wound healing through optimal moisture balance. While generally safe, their use requires careful consideration of patient factors, wound characteristics, and proper application techniques to maximize benefits and minimize risks.
The safety profile of occlusive dressings is generally favorable when applied correctly. However, there are important considerations to ensure patient safety. Proper assessment of the wound and surrounding skin is crucial before application. Clinicians must be vigilant for signs of infection, as the moist environment can potentially promote bacterial growth if not managed appropriately. Regular monitoring and timely dressing changes are essential to mitigate this risk.
One key advantage of occlusive dressings is their ability to reduce the frequency of dressing changes, minimizing disruption to the wound bed and decreasing the risk of nosocomial infections. A meta-analysis of 15 studies found that patients treated with occlusive dressings required 40% fewer dressing changes compared to those treated with conventional dressings, leading to improved patient comfort and reduced healthcare costs.
The choice of occlusive dressing material can significantly impact clinical outcomes. Hydrocolloid dressings have shown particular promise in managing exudate while maintaining an optimal moisture balance. A prospective study of 200 patients with chronic wounds reported that hydrocolloid dressings achieved complete wound closure in 78% of cases within 12 weeks, compared to 52% with standard care.
Patient factors such as wound location, exudate level, and underlying medical conditions must be considered when selecting an occlusive dressing. For instance, highly exudative wounds may benefit from dressings with higher absorption capacity to prevent maceration of surrounding skin. Conversely, dry wounds may require dressings with enhanced moisture-donating properties to promote optimal healing conditions.
Proper application technique is crucial for maximizing the benefits of occlusive dressings while minimizing potential complications. Healthcare providers should receive adequate training in dressing selection and application to ensure optimal outcomes. This includes proper cleansing of the wound, accurate sizing of the dressing, and secure application to prevent edge lifting and bacterial infiltration.
In conclusion, occlusive dressings have demonstrated significant clinical efficacy in promoting wound healing through optimal moisture balance. While generally safe, their use requires careful consideration of patient factors, wound characteristics, and proper application techniques to maximize benefits and minimize risks.
Cost-Effectiveness of Occlusive Dressing Therapies
The cost-effectiveness of occlusive dressing therapies is a critical consideration in wound care management, particularly when addressing the optimal moisture balance for wound healing. Occlusive dressings, designed to maintain a moist wound environment, have shown significant benefits in promoting faster healing and reducing the risk of infection. However, their cost-effectiveness must be evaluated in comparison to traditional wound care methods.
Several studies have demonstrated that occlusive dressings can lead to reduced overall treatment costs despite their higher initial price point. This is primarily due to faster healing times, decreased frequency of dressing changes, and reduced risk of complications. For instance, a meta-analysis of randomized controlled trials found that hydrocolloid dressings, a type of occlusive dressing, resulted in a 30% reduction in healing time compared to traditional gauze dressings.
The economic impact of occlusive dressings extends beyond direct material costs. By reducing the frequency of dressing changes, these therapies can significantly decrease nursing time and associated labor costs. A study in a hospital setting revealed that switching to occlusive dressings reduced dressing change frequency from daily to every 3-5 days, resulting in a 40% reduction in nursing time dedicated to wound care.
Furthermore, the improved healing outcomes associated with occlusive dressings can lead to shorter hospital stays and reduced risk of wound-related complications. A cost-benefit analysis conducted across multiple healthcare facilities showed that patients treated with occlusive dressings had, on average, 2.5 fewer days of hospitalization compared to those treated with conventional dressings, translating to substantial cost savings for healthcare providers.
However, the cost-effectiveness of occlusive dressings can vary depending on the wound type and patient characteristics. For chronic wounds, such as diabetic foot ulcers, the long-term cost savings of occlusive dressings are more pronounced due to the extended treatment duration. In contrast, for acute wounds with a shorter healing timeframe, the cost difference may be less significant.
It is also important to consider the potential for reduced pain and improved patient comfort associated with occlusive dressings. While challenging to quantify economically, these factors can contribute to improved patient satisfaction and potentially reduce the need for pain management interventions, further impacting overall treatment costs.
In conclusion, while occlusive dressings may have a higher upfront cost, their ability to optimize moisture balance and promote faster healing often results in improved cost-effectiveness over the course of treatment. Healthcare providers should consider these long-term economic benefits when making decisions about wound care protocols and resource allocation.
Several studies have demonstrated that occlusive dressings can lead to reduced overall treatment costs despite their higher initial price point. This is primarily due to faster healing times, decreased frequency of dressing changes, and reduced risk of complications. For instance, a meta-analysis of randomized controlled trials found that hydrocolloid dressings, a type of occlusive dressing, resulted in a 30% reduction in healing time compared to traditional gauze dressings.
The economic impact of occlusive dressings extends beyond direct material costs. By reducing the frequency of dressing changes, these therapies can significantly decrease nursing time and associated labor costs. A study in a hospital setting revealed that switching to occlusive dressings reduced dressing change frequency from daily to every 3-5 days, resulting in a 40% reduction in nursing time dedicated to wound care.
Furthermore, the improved healing outcomes associated with occlusive dressings can lead to shorter hospital stays and reduced risk of wound-related complications. A cost-benefit analysis conducted across multiple healthcare facilities showed that patients treated with occlusive dressings had, on average, 2.5 fewer days of hospitalization compared to those treated with conventional dressings, translating to substantial cost savings for healthcare providers.
However, the cost-effectiveness of occlusive dressings can vary depending on the wound type and patient characteristics. For chronic wounds, such as diabetic foot ulcers, the long-term cost savings of occlusive dressings are more pronounced due to the extended treatment duration. In contrast, for acute wounds with a shorter healing timeframe, the cost difference may be less significant.
It is also important to consider the potential for reduced pain and improved patient comfort associated with occlusive dressings. While challenging to quantify economically, these factors can contribute to improved patient satisfaction and potentially reduce the need for pain management interventions, further impacting overall treatment costs.
In conclusion, while occlusive dressings may have a higher upfront cost, their ability to optimize moisture balance and promote faster healing often results in improved cost-effectiveness over the course of treatment. Healthcare providers should consider these long-term economic benefits when making decisions about wound care protocols and resource allocation.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!