How To Evaluate Occlusive Dressings For Burn Wound Recovery
AUG 21, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Burn Wound Recovery and Occlusive Dressing Objectives
Burn wound recovery is a critical process in the field of wound care, and occlusive dressings play a pivotal role in promoting healing and preventing complications. The primary objective of evaluating occlusive dressings for burn wound recovery is to determine their efficacy in creating an optimal healing environment while minimizing the risk of infection and further tissue damage.
One of the key goals in burn wound management is to maintain a moist wound environment, which is essential for promoting cell migration, proliferation, and tissue regeneration. Occlusive dressings are designed to create a barrier that retains moisture while allowing for gaseous exchange, thus facilitating the natural healing process. By evaluating these dressings, we aim to assess their ability to maintain this delicate balance and promote faster wound closure.
Another crucial objective is to minimize the risk of infection, which is a significant concern in burn wound care. Occlusive dressings should provide an effective barrier against external contaminants while allowing for the management of wound exudate. The evaluation process must therefore focus on the dressing's ability to maintain a sterile environment and prevent bacterial colonization.
Pain management is an essential aspect of burn wound recovery, and occlusive dressings can play a significant role in this regard. The evaluation should assess the dressing's ability to reduce pain during dressing changes and provide comfort to the patient throughout the healing process. This includes examining factors such as ease of application and removal, as well as the dressing's ability to conform to irregular wound surfaces.
Furthermore, the evaluation of occlusive dressings should consider their impact on the overall healing time and the quality of the healed tissue. This involves assessing the dressing's ability to promote epithelialization, reduce scarring, and maintain skin elasticity. Long-term outcomes, such as the prevention of contractures and the preservation of functional mobility, should also be taken into account.
Cost-effectiveness and ease of use are additional objectives in the evaluation process. Healthcare providers need dressings that are not only effective but also economically viable and simple to apply and manage. This includes considerations such as the frequency of dressing changes required, the need for additional wound care products, and the overall impact on nursing time and resources.
Lastly, the evaluation should aim to identify any potential adverse effects or limitations of occlusive dressings in burn wound recovery. This may include assessing the risk of maceration, allergic reactions, or other complications that could impede the healing process or cause discomfort to the patient.
One of the key goals in burn wound management is to maintain a moist wound environment, which is essential for promoting cell migration, proliferation, and tissue regeneration. Occlusive dressings are designed to create a barrier that retains moisture while allowing for gaseous exchange, thus facilitating the natural healing process. By evaluating these dressings, we aim to assess their ability to maintain this delicate balance and promote faster wound closure.
Another crucial objective is to minimize the risk of infection, which is a significant concern in burn wound care. Occlusive dressings should provide an effective barrier against external contaminants while allowing for the management of wound exudate. The evaluation process must therefore focus on the dressing's ability to maintain a sterile environment and prevent bacterial colonization.
Pain management is an essential aspect of burn wound recovery, and occlusive dressings can play a significant role in this regard. The evaluation should assess the dressing's ability to reduce pain during dressing changes and provide comfort to the patient throughout the healing process. This includes examining factors such as ease of application and removal, as well as the dressing's ability to conform to irregular wound surfaces.
Furthermore, the evaluation of occlusive dressings should consider their impact on the overall healing time and the quality of the healed tissue. This involves assessing the dressing's ability to promote epithelialization, reduce scarring, and maintain skin elasticity. Long-term outcomes, such as the prevention of contractures and the preservation of functional mobility, should also be taken into account.
Cost-effectiveness and ease of use are additional objectives in the evaluation process. Healthcare providers need dressings that are not only effective but also economically viable and simple to apply and manage. This includes considerations such as the frequency of dressing changes required, the need for additional wound care products, and the overall impact on nursing time and resources.
Lastly, the evaluation should aim to identify any potential adverse effects or limitations of occlusive dressings in burn wound recovery. This may include assessing the risk of maceration, allergic reactions, or other complications that could impede the healing process or cause discomfort to the patient.
Market Analysis of Occlusive Dressings for Burns
The global market for occlusive dressings in burn wound care has experienced significant growth in recent years, driven by increasing awareness of advanced wound care techniques and the rising incidence of burn injuries worldwide. The market is characterized by a diverse range of products, including hydrocolloid dressings, film dressings, and foam dressings, each offering unique benefits for burn wound management.
Market demand for occlusive dressings in burn care is primarily fueled by their ability to create a moist wound environment, which promotes faster healing and reduces the risk of infection. These dressings also offer pain reduction, improved patient comfort, and decreased frequency of dressing changes, contributing to their growing popularity among healthcare professionals and patients alike.
The burn care market, including occlusive dressings, is projected to continue its upward trajectory, with a compound annual growth rate (CAGR) expected to remain strong over the next five years. This growth is attributed to factors such as the increasing geriatric population, rising prevalence of chronic wounds, and advancements in wound care technologies.
Geographically, North America and Europe currently dominate the occlusive dressings market for burn care, owing to well-established healthcare infrastructure and higher adoption rates of advanced wound care products. However, the Asia-Pacific region is emerging as a lucrative market, driven by improving healthcare access, rising disposable incomes, and growing awareness of advanced wound care techniques.
The competitive landscape of the occlusive dressings market for burn care is characterized by the presence of both multinational corporations and regional players. Key market players are focusing on product innovation, strategic partnerships, and mergers and acquisitions to strengthen their market position and expand their product portfolios.
Technological advancements in occlusive dressing materials, such as the incorporation of antimicrobial agents and the development of smart dressings with sensors for wound monitoring, are expected to further drive market growth. These innovations aim to address the challenges associated with burn wound management, including infection control and the need for frequent dressing changes.
Despite the positive market outlook, challenges such as the high cost of advanced dressings and limited reimbursement policies in some regions may hinder market growth. However, ongoing research and development efforts, coupled with increasing healthcare expenditure in emerging economies, are expected to create new opportunities for market expansion in the coming years.
Market demand for occlusive dressings in burn care is primarily fueled by their ability to create a moist wound environment, which promotes faster healing and reduces the risk of infection. These dressings also offer pain reduction, improved patient comfort, and decreased frequency of dressing changes, contributing to their growing popularity among healthcare professionals and patients alike.
The burn care market, including occlusive dressings, is projected to continue its upward trajectory, with a compound annual growth rate (CAGR) expected to remain strong over the next five years. This growth is attributed to factors such as the increasing geriatric population, rising prevalence of chronic wounds, and advancements in wound care technologies.
Geographically, North America and Europe currently dominate the occlusive dressings market for burn care, owing to well-established healthcare infrastructure and higher adoption rates of advanced wound care products. However, the Asia-Pacific region is emerging as a lucrative market, driven by improving healthcare access, rising disposable incomes, and growing awareness of advanced wound care techniques.
The competitive landscape of the occlusive dressings market for burn care is characterized by the presence of both multinational corporations and regional players. Key market players are focusing on product innovation, strategic partnerships, and mergers and acquisitions to strengthen their market position and expand their product portfolios.
Technological advancements in occlusive dressing materials, such as the incorporation of antimicrobial agents and the development of smart dressings with sensors for wound monitoring, are expected to further drive market growth. These innovations aim to address the challenges associated with burn wound management, including infection control and the need for frequent dressing changes.
Despite the positive market outlook, challenges such as the high cost of advanced dressings and limited reimbursement policies in some regions may hinder market growth. However, ongoing research and development efforts, coupled with increasing healthcare expenditure in emerging economies, are expected to create new opportunities for market expansion in the coming years.
Current Challenges in Occlusive Dressing Technology
Despite significant advancements in occlusive dressing technology for burn wound recovery, several challenges persist in this field. One of the primary issues is achieving the optimal balance between moisture retention and gas exchange. While occlusive dressings are designed to maintain a moist wound environment, excessive moisture can lead to maceration and delayed healing. Conversely, insufficient moisture can result in desiccation and impaired healing.
Another challenge lies in the management of wound exudate. Burn wounds often produce copious amounts of exudate, which can overwhelm the absorption capacity of some occlusive dressings. This can lead to leakage, increased risk of infection, and compromised wound healing. Developing dressings with enhanced fluid handling capabilities without sacrificing their occlusive properties remains a significant technical hurdle.
The prevention of bacterial colonization and infection is an ongoing concern in occlusive dressing technology. While these dressings create a barrier against external contaminants, they can also create an environment conducive to bacterial growth if not properly managed. Incorporating effective antimicrobial agents into occlusive dressings without compromising their healing properties or inducing resistance is a complex challenge.
Adhesion and removal of occlusive dressings present another set of difficulties. Strong adhesion is necessary to maintain the occlusive seal, but this can lead to trauma and pain during dressing changes, particularly in fragile burn wounds. Developing dressings that provide secure adhesion while allowing atraumatic removal is an area of ongoing research and development.
The variability in burn wound characteristics also poses challenges for occlusive dressing technology. Burns can vary in depth, location, and extent, making it difficult to create a one-size-fits-all solution. Customization and adaptability of occlusive dressings to suit different wound types and healing stages remain significant technical challenges.
Furthermore, the integration of advanced functionalities, such as real-time wound monitoring or controlled drug delivery, into occlusive dressings presents both opportunities and challenges. While these features could potentially revolutionize burn wound care, their implementation requires overcoming technical hurdles related to miniaturization, biocompatibility, and cost-effectiveness.
Lastly, the environmental impact of occlusive dressings is becoming an increasingly important consideration. Developing biodegradable or recyclable materials that maintain the necessary occlusive and healing properties of these dressings is a growing challenge in the field, as the healthcare industry seeks to reduce its environmental footprint.
Another challenge lies in the management of wound exudate. Burn wounds often produce copious amounts of exudate, which can overwhelm the absorption capacity of some occlusive dressings. This can lead to leakage, increased risk of infection, and compromised wound healing. Developing dressings with enhanced fluid handling capabilities without sacrificing their occlusive properties remains a significant technical hurdle.
The prevention of bacterial colonization and infection is an ongoing concern in occlusive dressing technology. While these dressings create a barrier against external contaminants, they can also create an environment conducive to bacterial growth if not properly managed. Incorporating effective antimicrobial agents into occlusive dressings without compromising their healing properties or inducing resistance is a complex challenge.
Adhesion and removal of occlusive dressings present another set of difficulties. Strong adhesion is necessary to maintain the occlusive seal, but this can lead to trauma and pain during dressing changes, particularly in fragile burn wounds. Developing dressings that provide secure adhesion while allowing atraumatic removal is an area of ongoing research and development.
The variability in burn wound characteristics also poses challenges for occlusive dressing technology. Burns can vary in depth, location, and extent, making it difficult to create a one-size-fits-all solution. Customization and adaptability of occlusive dressings to suit different wound types and healing stages remain significant technical challenges.
Furthermore, the integration of advanced functionalities, such as real-time wound monitoring or controlled drug delivery, into occlusive dressings presents both opportunities and challenges. While these features could potentially revolutionize burn wound care, their implementation requires overcoming technical hurdles related to miniaturization, biocompatibility, and cost-effectiveness.
Lastly, the environmental impact of occlusive dressings is becoming an increasingly important consideration. Developing biodegradable or recyclable materials that maintain the necessary occlusive and healing properties of these dressings is a growing challenge in the field, as the healthcare industry seeks to reduce its environmental footprint.
Existing Occlusive Dressing Evaluation Methods
01 Moisture retention and wound healing
Occlusive dressings create a moist environment that promotes wound healing by preventing dehydration and maintaining optimal conditions for tissue repair. This environment facilitates cell migration, enhances autolytic debridement, and reduces pain during dressing changes.- Moisture retention and wound healing: Occlusive dressings create a moist environment that promotes wound healing by preventing dehydration, facilitating cell migration, and enhancing the natural healing process. This moist environment also helps in reducing pain and minimizing scarring.
- Barrier protection and infection prevention: Occlusive dressings act as a barrier against external contaminants, reducing the risk of infection and promoting a sterile healing environment. They also help maintain the integrity of the wound site and protect it from further trauma or irritation.
- Enhanced drug delivery and absorption: Occlusive dressings can improve the absorption and efficacy of topical medications by creating an occlusive environment that enhances drug penetration into the skin or wound bed. This can lead to more effective treatment and faster recovery.
- Temperature regulation and oxygen permeability: Advanced occlusive dressings are designed to maintain an optimal wound temperature while allowing for controlled oxygen permeability. This balance helps create an ideal environment for cellular activity and tissue regeneration, promoting faster healing.
- Customizable and adaptable dressing solutions: Modern occlusive dressings offer customizable solutions that can be adapted to various wound types and healing stages. These may include features such as absorbency control, transparency for wound monitoring, and easy application and removal to minimize trauma during dressing changes.
02 Barrier protection and infection control
These dressings act as a barrier against external contaminants, reducing the risk of infection. They maintain a sterile environment around the wound, which is crucial for preventing complications and promoting faster recovery.Expand Specific Solutions03 Enhanced drug delivery and absorption
Occlusive dressings can improve the absorption and efficacy of topical medications by increasing skin hydration and drug penetration. This feature is particularly useful for delivering antibiotics, growth factors, or other therapeutic agents directly to the wound site.Expand Specific Solutions04 Temperature regulation and oxygen permeability
Advanced occlusive dressings are designed to maintain an optimal wound temperature while allowing for adequate oxygen exchange. This balance promotes cellular activity and supports the natural healing process without causing maceration or hypoxia.Expand Specific Solutions05 Customizable and adaptable designs
Modern occlusive dressings come in various forms and materials, allowing for customization based on wound type, location, and healing stage. Some designs incorporate features like transparency for wound monitoring or adhesive borders for secure placement.Expand Specific Solutions
Key Players in Occlusive Dressing Manufacturing
The burn wound recovery market is in a growth phase, with increasing demand for advanced occlusive dressings. The global market size for wound care products is projected to reach significant figures in the coming years, driven by rising incidence of chronic wounds and burns. Technological advancements in occlusive dressings have led to improved healing outcomes, with major players like 3M, Smith & Nephew, and Avery Dennison leading innovation. These companies, along with emerging players such as Fidia Farmaceutici and MediVas, are investing heavily in R&D to develop next-generation dressings with enhanced occlusive and healing properties. The technology is maturing, with a focus on biocompatible materials and smart dressings that can monitor wound healing progress.
3M Innovative Properties Co.
Technical Solution: 3M has developed advanced occlusive dressings for burn wound recovery, utilizing their expertise in adhesive technologies. Their Tegaderm™ line of transparent film dressings creates a moist wound healing environment while providing a barrier against external contaminants[1]. The dressings are designed with a unique adhesive that allows for gentle removal, minimizing trauma to healing tissue. 3M's occlusive dressings incorporate moisture vapor permeable films that help maintain optimal moisture balance, promoting faster healing and reducing the risk of maceration[2]. Additionally, they have integrated antimicrobial agents into some dressings to prevent infection, a critical factor in burn wound recovery[3].
Strengths: Advanced adhesive technology, moisture management, and infection control. Weaknesses: May not be suitable for all types of burns, especially those requiring frequent dressing changes or with heavy exudate.
Kendall Patient Recovery US LLC
Technical Solution: Kendall Patient Recovery, now part of Cardinal Health, has developed a range of occlusive dressings for burn wound recovery. Their KERLIX™ AMD antimicrobial gauze dressings provide a barrier against bacterial penetration while maintaining a moist wound environment[12]. For burn wounds, they offer TELFA™ AMD, a non-adherent pad with antimicrobial properties that minimizes trauma during dressing changes. Kendall's occlusive dressings incorporate technologies that balance moisture retention with breathability, crucial for burn wound healing. They have also introduced hydrocolloid dressings that form a gel when in contact with wound exudate, promoting autolytic debridement and facilitating the natural healing process in partial-thickness burns[13].
Strengths: Wide range of antimicrobial options, non-adherent technologies, and products supporting autolytic debridement. Weaknesses: Some dressings may require more frequent changes compared to advanced foam or film dressings.
Innovative Occlusive Dressing Materials Research
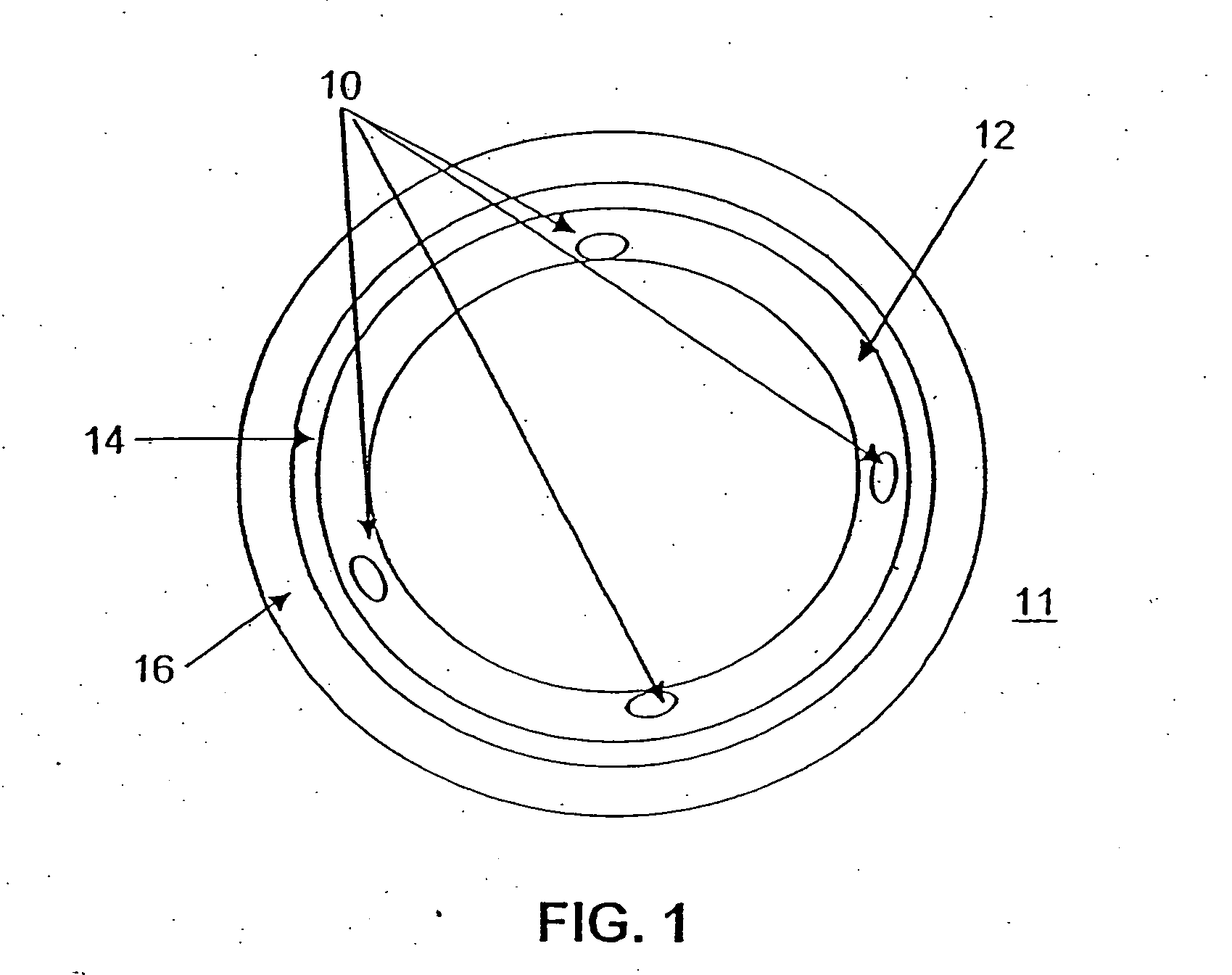
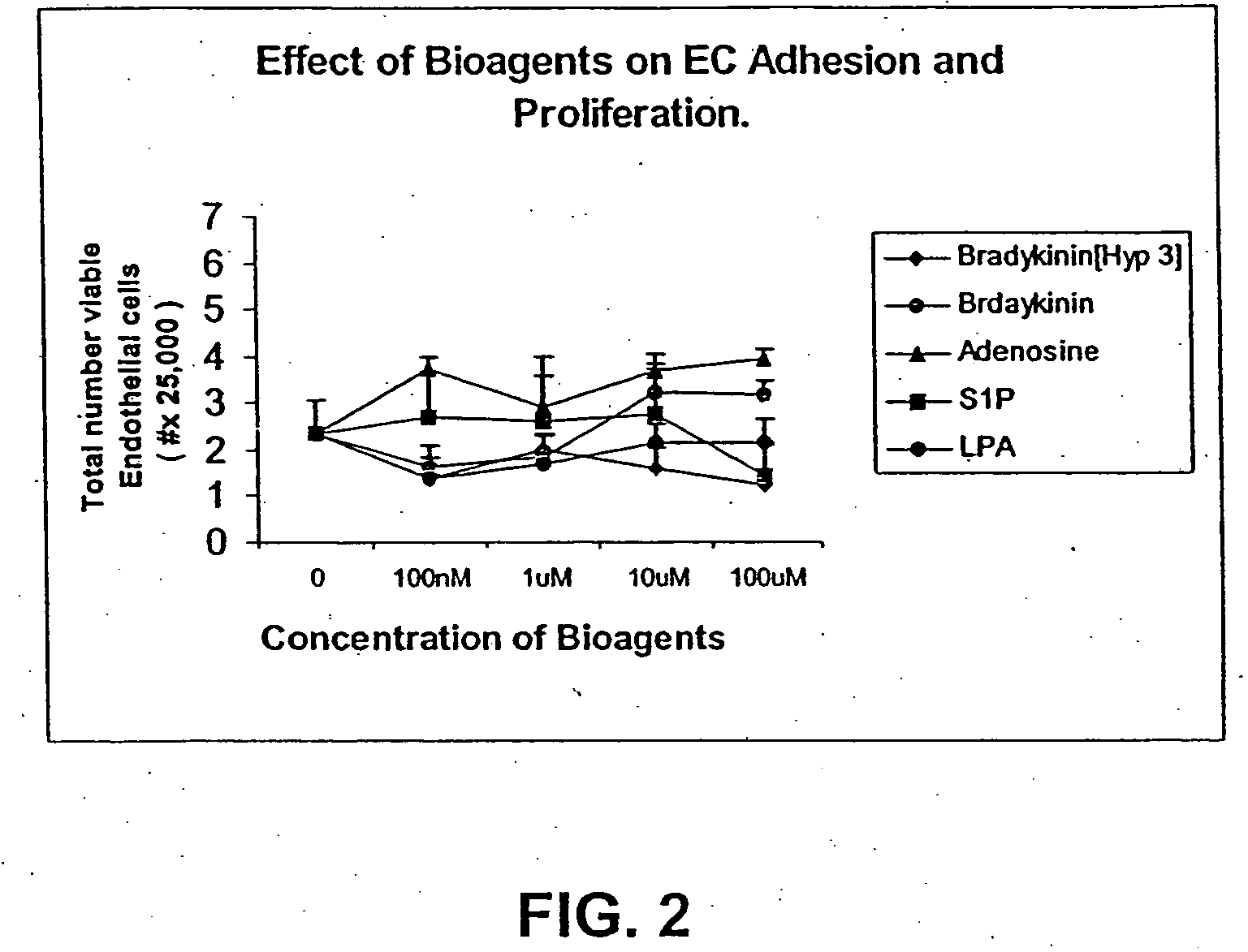
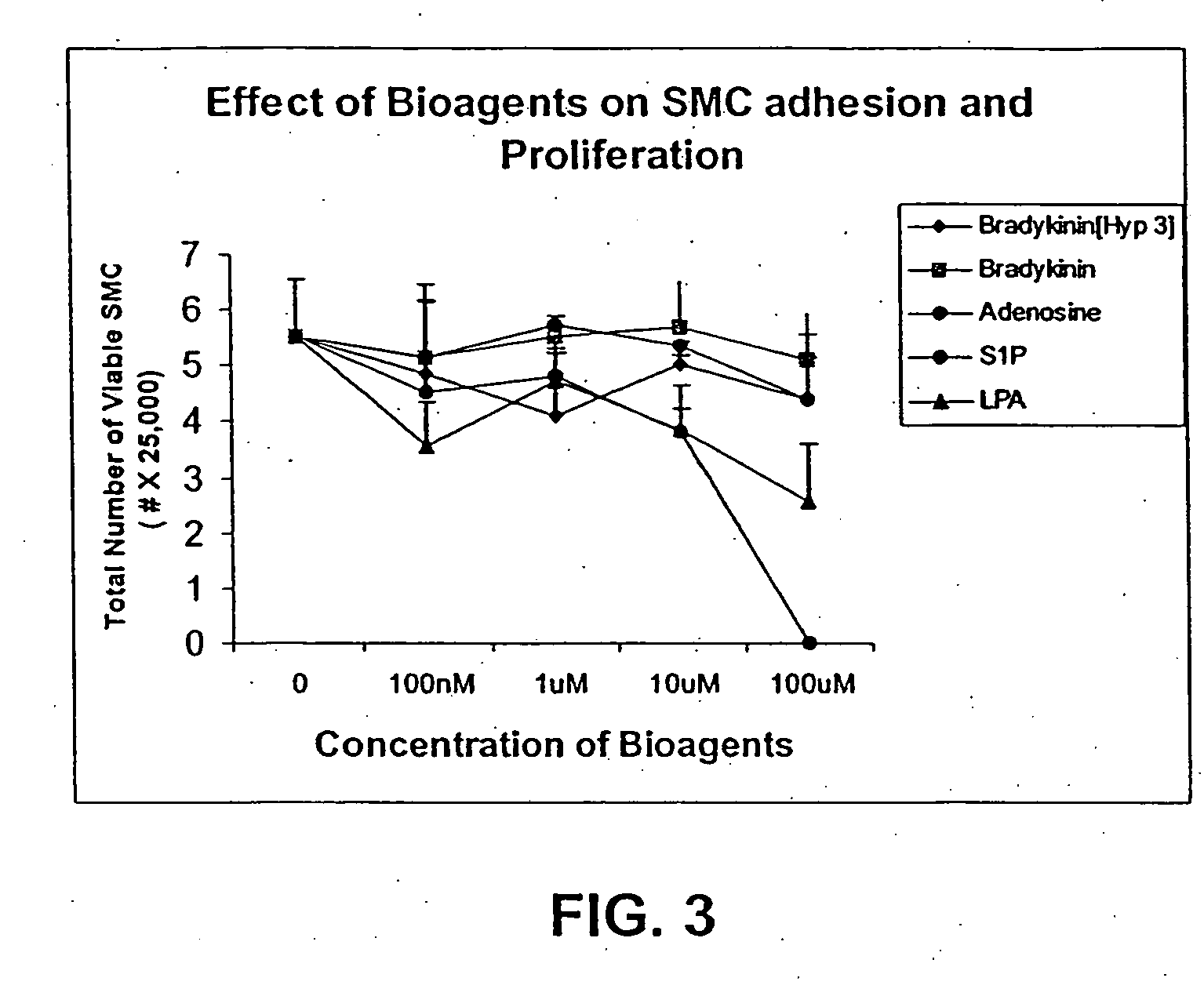
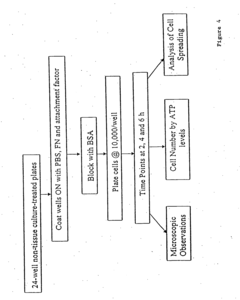
Wound care polymer compositions and methods for use thereof
PatentInactiveUS20060188486A1
Innovation
- Development of biodegradable polymer compositions, including poly(ester amide), poly(ester urethane), and poly(ester urea) polymers, that release wound healing agents to restore the natural healing process by promoting endothelialization and inhibiting smooth muscle cell proliferation, used in wound dressings, implants, and stent coatings.
Burn wound dressing material
PatentInactiveUS4767619A
Innovation
- A burn wound-adherent dressing material composed of a complex of gelatin and a water-soluble resin, specifically polyethylenimine, which forms a preformed film or an aqueous coating that adheres to the wound without additional securing devices, controlling water loss and bacterial ingress while allowing easy removal and observation of the wound.
Clinical Trial Design for Occlusive Dressing Efficacy
Clinical trials are essential for evaluating the efficacy of occlusive dressings in burn wound recovery. A well-designed study should incorporate several key elements to ensure reliable and meaningful results. The trial should be randomized and controlled, with patients randomly assigned to either the occlusive dressing group or a control group using standard treatment methods.
The study population should include a diverse range of burn patients, considering factors such as age, gender, burn severity, and location. Inclusion and exclusion criteria must be clearly defined to ensure a representative sample while minimizing confounding variables. The sample size should be determined through power analysis to detect clinically significant differences between treatment groups.
Outcome measures should be comprehensive and include both objective and subjective assessments. Primary endpoints may include wound healing time, infection rates, and scar formation. Secondary endpoints could encompass pain levels, patient comfort, and ease of dressing application and removal. Standardized assessment tools, such as the Vancouver Scar Scale or the Patient and Observer Scar Assessment Scale, should be utilized for consistency.
The duration of the trial should be sufficient to capture both short-term and long-term outcomes. Follow-up periods should extend beyond initial wound closure to assess long-term scar quality and functional outcomes. Regular assessment intervals should be established to track progress throughout the healing process.
Blinding techniques should be employed where possible to minimize bias. While complete blinding may be challenging due to the nature of dressing applications, efforts should be made to blind outcome assessors and data analysts to treatment allocation.
Data collection methods should be standardized across all study sites, with clear protocols for wound measurement, photography, and documentation. Electronic data capture systems can enhance accuracy and facilitate real-time monitoring of trial progress.
Safety monitoring is crucial, with a clear protocol for adverse event reporting and management. An independent data safety monitoring board should be established to oversee the trial and ensure patient safety.
Statistical analysis plans should be pre-specified, including methods for handling missing data and conducting intention-to-treat analyses. Subgroup analyses may be planned to identify patient populations that may benefit most from occlusive dressings.
Finally, the trial design should adhere to Good Clinical Practice guidelines and obtain appropriate ethical approvals. Patient consent procedures must be thorough, ensuring participants understand the trial's purpose, potential risks, and benefits.
The study population should include a diverse range of burn patients, considering factors such as age, gender, burn severity, and location. Inclusion and exclusion criteria must be clearly defined to ensure a representative sample while minimizing confounding variables. The sample size should be determined through power analysis to detect clinically significant differences between treatment groups.
Outcome measures should be comprehensive and include both objective and subjective assessments. Primary endpoints may include wound healing time, infection rates, and scar formation. Secondary endpoints could encompass pain levels, patient comfort, and ease of dressing application and removal. Standardized assessment tools, such as the Vancouver Scar Scale or the Patient and Observer Scar Assessment Scale, should be utilized for consistency.
The duration of the trial should be sufficient to capture both short-term and long-term outcomes. Follow-up periods should extend beyond initial wound closure to assess long-term scar quality and functional outcomes. Regular assessment intervals should be established to track progress throughout the healing process.
Blinding techniques should be employed where possible to minimize bias. While complete blinding may be challenging due to the nature of dressing applications, efforts should be made to blind outcome assessors and data analysts to treatment allocation.
Data collection methods should be standardized across all study sites, with clear protocols for wound measurement, photography, and documentation. Electronic data capture systems can enhance accuracy and facilitate real-time monitoring of trial progress.
Safety monitoring is crucial, with a clear protocol for adverse event reporting and management. An independent data safety monitoring board should be established to oversee the trial and ensure patient safety.
Statistical analysis plans should be pre-specified, including methods for handling missing data and conducting intention-to-treat analyses. Subgroup analyses may be planned to identify patient populations that may benefit most from occlusive dressings.
Finally, the trial design should adhere to Good Clinical Practice guidelines and obtain appropriate ethical approvals. Patient consent procedures must be thorough, ensuring participants understand the trial's purpose, potential risks, and benefits.
Regulatory Framework for Burn Treatment Products
The regulatory framework for burn treatment products, including occlusive dressings, is a complex and evolving landscape designed to ensure patient safety and product efficacy. In the United States, the Food and Drug Administration (FDA) plays a pivotal role in regulating these medical devices. Occlusive dressings for burn wound recovery are typically classified as Class II medical devices, requiring a 510(k) premarket notification submission to demonstrate substantial equivalence to a legally marketed predicate device.
The FDA's guidance document on "Premarket Notification [510(k)] Submissions for Wound Dressings Containing Antimicrobial Agents" provides specific recommendations for manufacturers. This guidance outlines the necessary data and testing requirements for these products, including in vitro and in vivo studies to evaluate antimicrobial effectiveness and potential cytotoxicity.
In the European Union, burn treatment products fall under the Medical Device Regulation (MDR) 2017/745. This regulation, which came into full effect in May 2021, imposes stricter requirements for clinical evaluation and post-market surveillance. Manufacturers must obtain CE marking to market their products in the EU, which involves demonstrating compliance with the MDR's essential requirements.
The International Organization for Standardization (ISO) has developed several standards relevant to burn dressings, such as ISO 10993 for biocompatibility testing and ISO 13485 for quality management systems. These standards are often recognized by regulatory bodies and serve as important benchmarks for product development and evaluation.
Japan's Pharmaceuticals and Medical Devices Agency (PMDA) regulates burn treatment products under the Pharmaceutical and Medical Device Act. The PMDA's approval process includes rigorous safety and efficacy evaluations, with specific requirements for foreign manufacturers seeking to enter the Japanese market.
Globally, there is a trend towards harmonization of regulatory frameworks, as evidenced by the Medical Device Single Audit Program (MDSAP). This program allows for a single regulatory audit to satisfy the requirements of multiple regulatory jurisdictions, potentially streamlining the approval process for manufacturers.
Regulatory bodies are increasingly focusing on real-world evidence and post-market surveillance data to complement traditional clinical trials. This shift recognizes the importance of long-term safety and effectiveness data in the evaluation of burn treatment products.
As new technologies emerge, such as advanced biomaterials and smart dressings, regulatory frameworks are adapting to address novel challenges. Agencies are developing guidance documents and adapting existing regulations to encompass these innovations while maintaining high standards of safety and efficacy.
The FDA's guidance document on "Premarket Notification [510(k)] Submissions for Wound Dressings Containing Antimicrobial Agents" provides specific recommendations for manufacturers. This guidance outlines the necessary data and testing requirements for these products, including in vitro and in vivo studies to evaluate antimicrobial effectiveness and potential cytotoxicity.
In the European Union, burn treatment products fall under the Medical Device Regulation (MDR) 2017/745. This regulation, which came into full effect in May 2021, imposes stricter requirements for clinical evaluation and post-market surveillance. Manufacturers must obtain CE marking to market their products in the EU, which involves demonstrating compliance with the MDR's essential requirements.
The International Organization for Standardization (ISO) has developed several standards relevant to burn dressings, such as ISO 10993 for biocompatibility testing and ISO 13485 for quality management systems. These standards are often recognized by regulatory bodies and serve as important benchmarks for product development and evaluation.
Japan's Pharmaceuticals and Medical Devices Agency (PMDA) regulates burn treatment products under the Pharmaceutical and Medical Device Act. The PMDA's approval process includes rigorous safety and efficacy evaluations, with specific requirements for foreign manufacturers seeking to enter the Japanese market.
Globally, there is a trend towards harmonization of regulatory frameworks, as evidenced by the Medical Device Single Audit Program (MDSAP). This program allows for a single regulatory audit to satisfy the requirements of multiple regulatory jurisdictions, potentially streamlining the approval process for manufacturers.
Regulatory bodies are increasingly focusing on real-world evidence and post-market surveillance data to complement traditional clinical trials. This shift recognizes the importance of long-term safety and effectiveness data in the evaluation of burn treatment products.
As new technologies emerge, such as advanced biomaterials and smart dressings, regulatory frameworks are adapting to address novel challenges. Agencies are developing guidance documents and adapting existing regulations to encompass these innovations while maintaining high standards of safety and efficacy.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!