Hydrogel-based biosensors for glucose detection
OCT 14, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Hydrogel Biosensor Evolution and Objectives
Hydrogel-based biosensors for glucose detection have evolved significantly since their inception in the late 1980s. The journey began with simple polymer matrices containing glucose oxidase, which produced color changes in response to glucose concentration. These early systems suffered from poor sensitivity, slow response times, and limited stability in biological environments.
The 1990s witnessed the integration of electrochemical detection methods with hydrogels, enhancing sensitivity and enabling quantitative measurements. This period marked the transition from laboratory curiosities to potential clinical tools, though challenges in biocompatibility and long-term functionality remained substantial barriers to practical application.
A paradigm shift occurred in the early 2000s with the development of "smart" hydrogels that exhibited reversible volume or property changes in response to glucose. These materials, often incorporating phenylboronic acid derivatives, eliminated the need for enzymatic components, thereby addressing stability limitations of earlier designs. Concurrently, advances in nanomaterials enabled the creation of nanocomposite hydrogels with enhanced electrical conductivity and surface area, dramatically improving sensor performance.
The 2010s brought miniaturization and integration with wearable technologies, moving hydrogel glucose sensors closer to continuous monitoring applications. Significant improvements in response time, sensitivity, and selectivity were achieved through rational molecular design and incorporation of novel recognition elements such as aptamers and molecularly imprinted polymers.
The primary objective of current hydrogel biosensor research is to develop fully implantable or minimally invasive continuous glucose monitoring systems with long-term stability in vivo. These systems aim to provide real-time, accurate glucose measurements without requiring frequent calibration or replacement. Secondary objectives include reducing manufacturing costs, enhancing biocompatibility, and developing self-healing capabilities to extend sensor lifetime.
Future development targets include achieving glucose specificity in complex biological fluids, reducing response times to under 5 minutes, extending functional lifetimes to over 30 days in vivo, and integrating wireless communication capabilities for seamless data transmission to monitoring devices. Additionally, there is growing interest in developing dual-function hydrogels that not only sense glucose levels but also respond therapeutically, such as by releasing insulin in response to hyperglycemia.
The ultimate goal remains the creation of a "closed-loop" artificial pancreas system, where hydrogel-based glucose sensors would trigger appropriate insulin delivery without user intervention, effectively mimicking pancreatic function in diabetes management.
The 1990s witnessed the integration of electrochemical detection methods with hydrogels, enhancing sensitivity and enabling quantitative measurements. This period marked the transition from laboratory curiosities to potential clinical tools, though challenges in biocompatibility and long-term functionality remained substantial barriers to practical application.
A paradigm shift occurred in the early 2000s with the development of "smart" hydrogels that exhibited reversible volume or property changes in response to glucose. These materials, often incorporating phenylboronic acid derivatives, eliminated the need for enzymatic components, thereby addressing stability limitations of earlier designs. Concurrently, advances in nanomaterials enabled the creation of nanocomposite hydrogels with enhanced electrical conductivity and surface area, dramatically improving sensor performance.
The 2010s brought miniaturization and integration with wearable technologies, moving hydrogel glucose sensors closer to continuous monitoring applications. Significant improvements in response time, sensitivity, and selectivity were achieved through rational molecular design and incorporation of novel recognition elements such as aptamers and molecularly imprinted polymers.
The primary objective of current hydrogel biosensor research is to develop fully implantable or minimally invasive continuous glucose monitoring systems with long-term stability in vivo. These systems aim to provide real-time, accurate glucose measurements without requiring frequent calibration or replacement. Secondary objectives include reducing manufacturing costs, enhancing biocompatibility, and developing self-healing capabilities to extend sensor lifetime.
Future development targets include achieving glucose specificity in complex biological fluids, reducing response times to under 5 minutes, extending functional lifetimes to over 30 days in vivo, and integrating wireless communication capabilities for seamless data transmission to monitoring devices. Additionally, there is growing interest in developing dual-function hydrogels that not only sense glucose levels but also respond therapeutically, such as by releasing insulin in response to hyperglycemia.
The ultimate goal remains the creation of a "closed-loop" artificial pancreas system, where hydrogel-based glucose sensors would trigger appropriate insulin delivery without user intervention, effectively mimicking pancreatic function in diabetes management.
Market Analysis for Glucose Monitoring Solutions
The global glucose monitoring market has witnessed substantial growth in recent years, driven primarily by the increasing prevalence of diabetes worldwide. As of 2023, the global diabetes population exceeds 537 million adults, with projections indicating this number could reach 783 million by 2045. This growing patient population creates a significant and expanding market for glucose monitoring solutions, with the global market valued at approximately 16.4 billion USD in 2022 and expected to reach 32.0 billion USD by 2030, representing a compound annual growth rate of 8.7%.
Traditional glucose monitoring methods, primarily finger-prick blood tests, dominate the current market landscape. However, continuous glucose monitoring (CGM) systems have gained substantial traction, growing at nearly twice the rate of traditional methods. This shift reflects increasing patient preference for less invasive, more convenient monitoring options that provide real-time data.
Hydrogel-based biosensors represent an emerging segment within this market, positioned at the intersection of the growing demand for non-invasive monitoring solutions and the push toward wearable healthcare technologies. These biosensors offer several advantages that align with current market trends, including reduced invasiveness, potential for continuous monitoring, and integration capabilities with digital health platforms.
Market segmentation reveals distinct user groups with varying needs. Type 1 diabetes patients, requiring frequent monitoring, prioritize accuracy and continuous data. Type 2 diabetes patients, representing approximately 90% of all cases, seek cost-effective, user-friendly solutions. Healthcare institutions focus on solutions that integrate with existing systems and provide actionable data for clinical decision-making.
Geographically, North America currently leads the glucose monitoring market with approximately 43% market share, followed by Europe at 28% and Asia-Pacific at 22%. However, the Asia-Pacific region is experiencing the fastest growth rate due to increasing diabetes prevalence, improving healthcare infrastructure, and rising disposable incomes in countries like China and India.
Consumer preferences are evolving toward solutions offering minimal invasiveness, longer sensor lifespans, improved accuracy, and seamless data integration with smartphones and other devices. This trend creates a favorable market environment for hydrogel-based biosensors, which can potentially address these preferences more effectively than current mainstream technologies.
Reimbursement policies significantly influence market adoption, with variations across regions affecting accessibility and market penetration rates. Countries with comprehensive coverage for diabetes monitoring technologies show higher adoption rates of advanced solutions, creating regional disparities in market development.
Traditional glucose monitoring methods, primarily finger-prick blood tests, dominate the current market landscape. However, continuous glucose monitoring (CGM) systems have gained substantial traction, growing at nearly twice the rate of traditional methods. This shift reflects increasing patient preference for less invasive, more convenient monitoring options that provide real-time data.
Hydrogel-based biosensors represent an emerging segment within this market, positioned at the intersection of the growing demand for non-invasive monitoring solutions and the push toward wearable healthcare technologies. These biosensors offer several advantages that align with current market trends, including reduced invasiveness, potential for continuous monitoring, and integration capabilities with digital health platforms.
Market segmentation reveals distinct user groups with varying needs. Type 1 diabetes patients, requiring frequent monitoring, prioritize accuracy and continuous data. Type 2 diabetes patients, representing approximately 90% of all cases, seek cost-effective, user-friendly solutions. Healthcare institutions focus on solutions that integrate with existing systems and provide actionable data for clinical decision-making.
Geographically, North America currently leads the glucose monitoring market with approximately 43% market share, followed by Europe at 28% and Asia-Pacific at 22%. However, the Asia-Pacific region is experiencing the fastest growth rate due to increasing diabetes prevalence, improving healthcare infrastructure, and rising disposable incomes in countries like China and India.
Consumer preferences are evolving toward solutions offering minimal invasiveness, longer sensor lifespans, improved accuracy, and seamless data integration with smartphones and other devices. This trend creates a favorable market environment for hydrogel-based biosensors, which can potentially address these preferences more effectively than current mainstream technologies.
Reimbursement policies significantly influence market adoption, with variations across regions affecting accessibility and market penetration rates. Countries with comprehensive coverage for diabetes monitoring technologies show higher adoption rates of advanced solutions, creating regional disparities in market development.
Current Hydrogel Biosensor Technologies and Limitations
Hydrogel-based biosensors for glucose detection have evolved significantly over the past decade, with several distinct technological approaches currently dominating the field. Phenylboronic acid (PBA)-based hydrogels represent one of the most established platforms, utilizing the reversible binding between PBA and glucose to induce volume changes or optical property shifts. These systems offer good specificity but often suffer from pH sensitivity, requiring careful calibration in physiological environments where pH fluctuations can lead to false readings.
Enzymatic hydrogel biosensors, particularly those incorporating glucose oxidase (GOx), remain the gold standard for many applications due to their high selectivity. These systems typically transduce the enzymatic reaction of glucose into detectable signals through electrochemical, optical, or mechanical means. However, enzyme stability remains a significant limitation, with performance degradation occurring over time due to denaturation, especially in implantable or continuous monitoring scenarios.
Conductive polymer-hydrogel composites have emerged as promising alternatives, offering electrical signal transduction without requiring enzymes. These materials combine the biocompatibility of hydrogels with the electrical properties of conductive polymers like polyaniline or PEDOT:PSS. While they demonstrate excellent response times, their long-term stability and glucose specificity in complex biological fluids remain challenging issues.
Molecularly imprinted polymer (MIP) hydrogels represent a newer approach, where glucose-shaped cavities are created within the hydrogel matrix. These systems offer enzyme-free detection with potentially high specificity, but currently struggle with lower sensitivity compared to enzymatic methods and face challenges in achieving consistent manufacturing at scale.
A significant limitation across all hydrogel-based glucose sensors is response time, particularly for implantable or continuous monitoring applications. The diffusion-limited nature of hydrogels creates an inherent trade-off between sensitivity and speed, with thicker hydrogels offering better signal generation but slower response to changing glucose levels.
Biocompatibility and biofouling present persistent challenges, especially for long-term implantable sensors. Protein adsorption and foreign body responses can dramatically reduce sensor performance over time, with current surface modification strategies providing only partial solutions. Additionally, achieving consistent mechanical properties that balance flexibility for comfort with durability for longevity remains difficult.
Manufacturing scalability represents another significant hurdle, with many laboratory-demonstrated hydrogel biosensors proving difficult to produce at commercial scales with consistent performance. Variations in crosslinking density, functional group distribution, and overall hydrogel architecture can lead to batch-to-batch variability that complicates regulatory approval and clinical adoption.
Enzymatic hydrogel biosensors, particularly those incorporating glucose oxidase (GOx), remain the gold standard for many applications due to their high selectivity. These systems typically transduce the enzymatic reaction of glucose into detectable signals through electrochemical, optical, or mechanical means. However, enzyme stability remains a significant limitation, with performance degradation occurring over time due to denaturation, especially in implantable or continuous monitoring scenarios.
Conductive polymer-hydrogel composites have emerged as promising alternatives, offering electrical signal transduction without requiring enzymes. These materials combine the biocompatibility of hydrogels with the electrical properties of conductive polymers like polyaniline or PEDOT:PSS. While they demonstrate excellent response times, their long-term stability and glucose specificity in complex biological fluids remain challenging issues.
Molecularly imprinted polymer (MIP) hydrogels represent a newer approach, where glucose-shaped cavities are created within the hydrogel matrix. These systems offer enzyme-free detection with potentially high specificity, but currently struggle with lower sensitivity compared to enzymatic methods and face challenges in achieving consistent manufacturing at scale.
A significant limitation across all hydrogel-based glucose sensors is response time, particularly for implantable or continuous monitoring applications. The diffusion-limited nature of hydrogels creates an inherent trade-off between sensitivity and speed, with thicker hydrogels offering better signal generation but slower response to changing glucose levels.
Biocompatibility and biofouling present persistent challenges, especially for long-term implantable sensors. Protein adsorption and foreign body responses can dramatically reduce sensor performance over time, with current surface modification strategies providing only partial solutions. Additionally, achieving consistent mechanical properties that balance flexibility for comfort with durability for longevity remains difficult.
Manufacturing scalability represents another significant hurdle, with many laboratory-demonstrated hydrogel biosensors proving difficult to produce at commercial scales with consistent performance. Variations in crosslinking density, functional group distribution, and overall hydrogel architecture can lead to batch-to-batch variability that complicates regulatory approval and clinical adoption.
Existing Hydrogel-based Glucose Detection Methods
01 Hydrogel compositions for glucose detection
Specific hydrogel compositions can be formulated for effective glucose detection in biosensors. These hydrogels typically contain glucose-responsive polymers that undergo physical or chemical changes in the presence of glucose. The compositions may include polyacrylamide, poly(ethylene glycol), or other biocompatible polymers that provide the necessary matrix for embedding glucose-sensing elements while maintaining biocompatibility and appropriate mechanical properties for biosensor applications.- Hydrogel compositions for glucose detection: Specific hydrogel compositions can be engineered for glucose detection in biosensors. These hydrogels typically contain glucose-responsive polymers that undergo physical or chemical changes in the presence of glucose. The compositions may include polyacrylamide, polyethylene glycol (PEG), or other biocompatible polymers that provide a suitable matrix for embedding glucose-sensing elements while maintaining biocompatibility and appropriate mechanical properties for biosensor applications.
- Enzyme-based hydrogel biosensors: Enzyme-based hydrogel biosensors incorporate glucose oxidase or other glucose-specific enzymes within the hydrogel matrix. These enzymes catalyze the oxidation of glucose, producing hydrogen peroxide or other detectable byproducts. The enzymatic reaction can be coupled with electrochemical, optical, or other detection methods to quantify glucose levels. The hydrogel structure provides a favorable microenvironment for enzyme stability and activity while allowing glucose diffusion to the sensing elements.
- Conductive hydrogels for electrochemical glucose sensing: Conductive hydrogels combine the biocompatibility of hydrogels with electrical conductivity for electrochemical glucose detection. These materials typically incorporate conductive polymers, carbon nanomaterials, or metal nanoparticles within the hydrogel network. The resulting composite provides efficient electron transfer pathways for electrochemical sensing while maintaining the hydrogel's favorable properties for biological applications. These conductive hydrogels enable sensitive and stable glucose detection in various biological fluids.
- Stimuli-responsive hydrogels for glucose monitoring: Stimuli-responsive hydrogels change their physical properties in response to glucose concentration. These smart materials can undergo volume changes, alter their optical properties, or display other measurable responses when exposed to varying glucose levels. Common mechanisms include glucose-binding with phenylboronic acid derivatives or competitive binding with glucose-responsive molecules. These responsive hydrogels enable continuous, real-time glucose monitoring without requiring enzymatic components, potentially offering longer sensor lifetimes and stability.
- Wearable and implantable hydrogel glucose sensors: Hydrogel-based glucose biosensors can be designed for wearable or implantable applications, enabling continuous glucose monitoring. These designs focus on biocompatibility, long-term stability, and integration with electronic components for signal processing and data transmission. Wearable sensors may be incorporated into patches or contact lenses, while implantable versions are engineered to minimize foreign body response and maintain functionality in the subcutaneous environment. Advanced fabrication techniques ensure proper interface between the hydrogel sensing element and electronic components.
02 Enzyme-based hydrogel biosensors
Enzyme-based hydrogel biosensors incorporate glucose oxidase or other glucose-specific enzymes within the hydrogel matrix. These enzymes catalyze the oxidation of glucose, producing hydrogen peroxide or other detectable byproducts. The enzymatic reaction can be coupled with various detection methods such as electrochemical, optical, or colorimetric techniques. The hydrogel structure provides a favorable microenvironment for enzyme stability and activity while allowing glucose molecules to diffuse through the matrix for detection.Expand Specific Solutions03 Wearable hydrogel glucose sensors
Wearable hydrogel-based glucose sensors are designed for continuous glucose monitoring with minimal invasiveness. These sensors can be applied directly to the skin or incorporated into wearable devices. The hydrogel matrix allows for sustained contact with interstitial fluid while providing comfort and flexibility. Advanced designs include smart hydrogels that can wirelessly transmit glucose measurements to monitoring devices, enabling real-time glucose tracking for diabetic patients.Expand Specific Solutions04 Conductive hydrogels for electrochemical glucose sensing
Conductive hydrogels combine the biocompatibility of hydrogels with electrical conductivity for enhanced electrochemical glucose detection. These materials typically incorporate conductive elements such as carbon nanotubes, graphene, or conductive polymers within the hydrogel network. The conductive components facilitate electron transfer during glucose oxidation reactions, improving sensor sensitivity and response time. These hydrogels can be designed with specific pore structures to optimize glucose diffusion while maintaining electrical connectivity.Expand Specific Solutions05 Stimuli-responsive hydrogels for visual glucose detection
Stimuli-responsive hydrogels change their physical properties in response to glucose concentration, enabling visual detection without complex instrumentation. These smart hydrogels may change color, transparency, or volume in proportion to glucose levels. Some designs incorporate phenylboronic acid derivatives that form reversible bonds with glucose, triggering conformational changes in the hydrogel. These systems are particularly valuable for point-of-care applications where immediate visual feedback on glucose levels is beneficial.Expand Specific Solutions
Leading Companies in Hydrogel Biosensor Industry
The hydrogel-based biosensor market for glucose detection is currently in a growth phase, characterized by increasing adoption driven by the rising prevalence of diabetes globally. The market size is expanding rapidly, estimated to reach several billion dollars by 2025, with continuous glucose monitoring (CGM) systems representing the fastest-growing segment. Technologically, the field shows varying maturity levels, with companies like Dexcom, Medtronic MiniMed, and Abbott Diabetes Care leading with commercialized products, while newer entrants such as GlucoModicum and EyeSense are advancing novel approaches. Established medical device corporations (Siemens, Becton Dickinson) provide infrastructure support, while academic institutions (University of Hong Kong, Rice University) drive fundamental research. The competitive landscape is diversifying with specialized players like i-SENS and UXN focusing on electrochemical biosensor technologies for improved accuracy and non-invasive solutions.
EyeSense AG
Technical Solution: EyeSense has developed an innovative approach to glucose monitoring using hydrogel-based fluorescent biosensors implanted in the subconjunctival tissue of the eye. Their technology utilizes a specialized hydrogel microsphere containing glucose-responsive fluorescent molecules that change their fluorescence properties in proportion to glucose concentration. The hydrogel matrix is designed with specific porosity to allow glucose diffusion while retaining the sensing molecules. When exposed to light from a handheld reader device, the implanted sensor emits fluorescence that correlates with glucose levels, which is then detected and analyzed. The hydrogel composition has been engineered for long-term stability in the eye environment, with projected functionality for up to 12 months before replacement is needed. The hydrogel also incorporates biocompatible components that minimize inflammatory response and prevent protein fouling, ensuring consistent performance over the sensor lifetime. This approach eliminates the need for frequent sensor replacements and provides a less invasive alternative to traditional CGM systems.
Strengths: Extremely long sensor lifetime compared to traditional CGM systems; non-invasive reading process after initial implantation; potential for reduced cost over time due to infrequent replacements. Weaknesses: Requires minor surgical procedure for initial sensor placement; limited real-world validation data compared to established CGM technologies; potential for variability in readings based on eye conditions.
Medtronic MiniMed, Inc.
Technical Solution: Medtronic has developed sophisticated hydrogel-based glucose sensing technology integrated with their insulin pump systems. Their approach utilizes a multi-layered hydrogel membrane system surrounding a glucose oxidase-based electrochemical sensor. The outer layer consists of a biocompatible hydrogel designed to reduce protein adsorption and cellular adhesion, minimizing the foreign body response. The middle layer contains a precisely formulated hydrogel with controlled pore size that selectively allows glucose diffusion while blocking larger interfering molecules. The innermost layer incorporates the enzyme glucose oxidase within a specialized hydrogel matrix that maintains enzyme stability and activity. Medtronic's Guardian Sensor 3 technology employs this hydrogel system along with proprietary algorithms that compensate for the lag time between blood and interstitial glucose levels. Their hydrogel formulation has been engineered to maintain consistent diffusion characteristics across varying glucose concentrations and physiological conditions.
Strengths: Tight integration with automated insulin delivery systems; sophisticated algorithms compensating for physiological lag times; established clinical validation through extensive trials. Weaknesses: Shorter sensor lifetime (7 days) compared to some competitors; requires periodic calibration with fingerstick measurements; more complex insertion process than some alternative systems.
Key Patents and Innovations in Hydrogel Biosensors
Use of hydrogels for biosensors having elevated sensitivity
PatentActiveEP2652510A1
Innovation
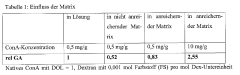
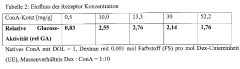
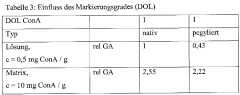
- A polymer-based hydrogel is used to enrich glucose-binding proteins, allowing interaction with ligands while maintaining glucose binding site availability, utilizing specific polymers like alginates and polyvinyl alcohols to create an interpenetrating network that enhances sensor component concentration and mobility, thereby increasing measurement sensitivity and accuracy.
Use of hydrogels for biosensors having elevated sensitivity
PatentWO2012080258A1
Innovation
- A polymer-based hydrogel matrix is used to enrich glucose-binding proteins, allowing interaction with ligands without blocking glucose binding sites, utilizing suitable polymers like alginates and polyvinyl alcohols to create an interpenetrating network that enhances sensor component mobility and concentration, combined with specific dye labeling for improved detection.
Biocompatibility and Safety Considerations
Biocompatibility represents a critical consideration in the development of hydrogel-based glucose biosensors, particularly for implantable or wearable applications where direct contact with biological tissues occurs. These biosensors must demonstrate minimal immune response and inflammation when interfacing with the human body. Current research indicates that natural polymers such as alginate, chitosan, and hyaluronic acid generally exhibit superior biocompatibility compared to synthetic alternatives, though modifications to synthetic hydrogels can significantly improve their biological acceptance.
The long-term stability of hydrogel materials in physiological environments presents ongoing challenges. Degradation products must be non-toxic and safely metabolized or excreted from the body. Recent studies have focused on developing self-healing hydrogels that maintain structural integrity while minimizing the release of potentially harmful degradation byproducts during extended use periods, which is particularly important for continuous glucose monitoring applications.
Sterilization processes represent another crucial safety consideration, as they must effectively eliminate microbial contamination without compromising the functional properties of the biosensor components. Common methods include gamma irradiation, ethylene oxide treatment, and autoclaving, each with distinct impacts on hydrogel structure and enzyme activity. Research indicates that gamma irradiation often provides the optimal balance between sterilization efficacy and preservation of glucose-sensing capabilities.
Leaching of components from hydrogel matrices poses significant safety concerns. Unreacted monomers, crosslinking agents, and other additives may elicit toxic responses if released into surrounding tissues. Advanced encapsulation techniques and thorough purification protocols have been developed to mitigate these risks, with particular attention to preventing the release of potentially harmful substances during sensor operation.
Regulatory frameworks governing hydrogel-based glucose biosensors vary globally but generally require comprehensive biocompatibility testing according to ISO 10993 standards. These evaluations typically include cytotoxicity assessments, sensitization studies, and implantation tests. The FDA has established specific guidance for continuous glucose monitoring systems that addresses both biocompatibility and performance requirements, creating a structured pathway for clinical translation.
Recent innovations focus on developing "stealth" hydrogels that minimize protein adsorption and foreign body responses, thereby extending functional lifetimes and improving safety profiles. Approaches include incorporating anti-fouling polymers like polyethylene glycol (PEG) and zwitterionic materials that resist non-specific protein adhesion and subsequent inflammatory cascades, representing promising directions for next-generation glucose monitoring technologies.
The long-term stability of hydrogel materials in physiological environments presents ongoing challenges. Degradation products must be non-toxic and safely metabolized or excreted from the body. Recent studies have focused on developing self-healing hydrogels that maintain structural integrity while minimizing the release of potentially harmful degradation byproducts during extended use periods, which is particularly important for continuous glucose monitoring applications.
Sterilization processes represent another crucial safety consideration, as they must effectively eliminate microbial contamination without compromising the functional properties of the biosensor components. Common methods include gamma irradiation, ethylene oxide treatment, and autoclaving, each with distinct impacts on hydrogel structure and enzyme activity. Research indicates that gamma irradiation often provides the optimal balance between sterilization efficacy and preservation of glucose-sensing capabilities.
Leaching of components from hydrogel matrices poses significant safety concerns. Unreacted monomers, crosslinking agents, and other additives may elicit toxic responses if released into surrounding tissues. Advanced encapsulation techniques and thorough purification protocols have been developed to mitigate these risks, with particular attention to preventing the release of potentially harmful substances during sensor operation.
Regulatory frameworks governing hydrogel-based glucose biosensors vary globally but generally require comprehensive biocompatibility testing according to ISO 10993 standards. These evaluations typically include cytotoxicity assessments, sensitization studies, and implantation tests. The FDA has established specific guidance for continuous glucose monitoring systems that addresses both biocompatibility and performance requirements, creating a structured pathway for clinical translation.
Recent innovations focus on developing "stealth" hydrogels that minimize protein adsorption and foreign body responses, thereby extending functional lifetimes and improving safety profiles. Approaches include incorporating anti-fouling polymers like polyethylene glycol (PEG) and zwitterionic materials that resist non-specific protein adhesion and subsequent inflammatory cascades, representing promising directions for next-generation glucose monitoring technologies.
Commercialization Pathways and Cost Analysis
The commercialization of hydrogel-based glucose biosensors presents multiple pathways with varying degrees of market entry barriers and potential returns. Medical device partnerships represent the most established route, wherein biosensor developers collaborate with established medical device manufacturers like Medtronic, Abbott, or Dexcom. This approach leverages existing distribution channels and regulatory expertise but typically involves revenue-sharing arrangements that may limit profit margins to 15-25%.
Direct-to-consumer wellness products offer an alternative pathway with fewer regulatory hurdles when marketed as non-diagnostic devices. This approach enables faster market entry and potentially higher margins (30-45%), though it requires significant investment in consumer marketing and brand development. Several startups have successfully utilized this model, particularly for non-invasive monitoring solutions.
Licensing technology to established players represents a lower-risk strategy, generating revenue through upfront payments and royalties (typically 5-12% of net sales). While this minimizes commercialization costs, it relinquishes control over product development and market positioning.
Cost analysis reveals significant variation across development stages. Initial R&D expenses for hydrogel-based glucose sensors typically range from $2-5 million, covering material optimization, enzyme stabilization, and prototype development. Clinical validation adds $3-7 million, while regulatory approval processes contribute an additional $1-3 million for wellness products or $5-10 million for medical devices requiring FDA approval.
Manufacturing scale-up presents substantial cost considerations. Small-batch production costs approximately $15-25 per sensor, while high-volume manufacturing can reduce unit costs to $3-8. Key cost drivers include enzyme purification (30-40% of material costs), specialized hydrogel polymers (15-25%), and precision manufacturing processes (20-30%).
Market entry and distribution costs vary significantly by commercialization pathway. Direct-to-consumer approaches require substantial marketing investments ($5-10 million initially), while medical partnerships may reduce these costs but introduce revenue-sharing obligations.
Break-even analysis suggests most hydrogel glucose sensor ventures require 3-5 years to achieve profitability, with initial investment recovery typically occurring after 100,000-500,000 units sold, depending on pricing strategy and commercialization pathway selected.
Direct-to-consumer wellness products offer an alternative pathway with fewer regulatory hurdles when marketed as non-diagnostic devices. This approach enables faster market entry and potentially higher margins (30-45%), though it requires significant investment in consumer marketing and brand development. Several startups have successfully utilized this model, particularly for non-invasive monitoring solutions.
Licensing technology to established players represents a lower-risk strategy, generating revenue through upfront payments and royalties (typically 5-12% of net sales). While this minimizes commercialization costs, it relinquishes control over product development and market positioning.
Cost analysis reveals significant variation across development stages. Initial R&D expenses for hydrogel-based glucose sensors typically range from $2-5 million, covering material optimization, enzyme stabilization, and prototype development. Clinical validation adds $3-7 million, while regulatory approval processes contribute an additional $1-3 million for wellness products or $5-10 million for medical devices requiring FDA approval.
Manufacturing scale-up presents substantial cost considerations. Small-batch production costs approximately $15-25 per sensor, while high-volume manufacturing can reduce unit costs to $3-8. Key cost drivers include enzyme purification (30-40% of material costs), specialized hydrogel polymers (15-25%), and precision manufacturing processes (20-30%).
Market entry and distribution costs vary significantly by commercialization pathway. Direct-to-consumer approaches require substantial marketing investments ($5-10 million initially), while medical partnerships may reduce these costs but introduce revenue-sharing obligations.
Break-even analysis suggests most hydrogel glucose sensor ventures require 3-5 years to achieve profitability, with initial investment recovery typically occurring after 100,000-500,000 units sold, depending on pricing strategy and commercialization pathway selected.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!