Hydrogel Safety and Biocompatibility Testing Checklist for R&D Teams
AUG 21, 202510 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Hydrogel Biocompatibility Background and Objectives
Hydrogels have emerged as versatile biomaterials with a rich history dating back to the 1960s when the first synthetic hydrogels were developed for contact lens applications. These three-dimensional networks of hydrophilic polymers can absorb and retain significant amounts of water while maintaining their structure, mimicking natural tissues and providing an ideal platform for biomedical applications. The evolution of hydrogel technology has accelerated dramatically over the past two decades, transitioning from simple homogeneous materials to sophisticated smart systems capable of responding to environmental stimuli.
The biocompatibility of hydrogels represents a critical aspect of their development and application in medical contexts. Biocompatibility refers to the ability of a material to perform with an appropriate host response in a specific application, encompassing aspects of both safety and functionality. Early hydrogels faced significant challenges related to foreign body responses and inflammation, driving continuous innovation in polymer chemistry and fabrication techniques to enhance their biological performance.
Current technological trends in hydrogel development focus on creating materials with precisely controlled properties, including degradation rates, mechanical strength, and biological interactions. Advanced hydrogels now incorporate bioactive components, such as growth factors, cell-adhesion motifs, and enzymatically degradable crosslinks, enabling unprecedented control over cell-material interactions and tissue regeneration processes.
The objectives of hydrogel biocompatibility testing are multifaceted, aiming to ensure patient safety while maximizing therapeutic efficacy. Primary goals include the comprehensive assessment of potential cytotoxicity, immunogenicity, thrombogenicity, and genotoxicity of novel hydrogel formulations. Additionally, testing must evaluate the material's performance under physiologically relevant conditions, including mechanical stability, degradation behavior, and interaction with host tissues over extended periods.
Regulatory frameworks governing hydrogel biocompatibility have evolved substantially, with organizations such as the FDA, ISO, and EMA establishing increasingly stringent standards for biomaterial evaluation. The ISO 10993 series of standards provides a structured approach to biological evaluation, while the FDA's guidance documents offer specific recommendations for different application categories, from wound dressings to implantable devices.
The development of standardized testing protocols represents a significant challenge in the field, as hydrogels' diverse compositions and applications necessitate tailored evaluation approaches. Current efforts focus on establishing predictive in vitro models that can accurately simulate in vivo responses, reducing reliance on animal testing while improving the translational value of preclinical data.
Looking forward, the field aims to develop comprehensive biocompatibility assessment frameworks that integrate traditional safety testing with advanced analytical techniques, including high-throughput screening, omics approaches, and computational modeling. These integrated approaches promise to accelerate hydrogel development while ensuring the highest standards of patient safety and therapeutic efficacy.
The biocompatibility of hydrogels represents a critical aspect of their development and application in medical contexts. Biocompatibility refers to the ability of a material to perform with an appropriate host response in a specific application, encompassing aspects of both safety and functionality. Early hydrogels faced significant challenges related to foreign body responses and inflammation, driving continuous innovation in polymer chemistry and fabrication techniques to enhance their biological performance.
Current technological trends in hydrogel development focus on creating materials with precisely controlled properties, including degradation rates, mechanical strength, and biological interactions. Advanced hydrogels now incorporate bioactive components, such as growth factors, cell-adhesion motifs, and enzymatically degradable crosslinks, enabling unprecedented control over cell-material interactions and tissue regeneration processes.
The objectives of hydrogel biocompatibility testing are multifaceted, aiming to ensure patient safety while maximizing therapeutic efficacy. Primary goals include the comprehensive assessment of potential cytotoxicity, immunogenicity, thrombogenicity, and genotoxicity of novel hydrogel formulations. Additionally, testing must evaluate the material's performance under physiologically relevant conditions, including mechanical stability, degradation behavior, and interaction with host tissues over extended periods.
Regulatory frameworks governing hydrogel biocompatibility have evolved substantially, with organizations such as the FDA, ISO, and EMA establishing increasingly stringent standards for biomaterial evaluation. The ISO 10993 series of standards provides a structured approach to biological evaluation, while the FDA's guidance documents offer specific recommendations for different application categories, from wound dressings to implantable devices.
The development of standardized testing protocols represents a significant challenge in the field, as hydrogels' diverse compositions and applications necessitate tailored evaluation approaches. Current efforts focus on establishing predictive in vitro models that can accurately simulate in vivo responses, reducing reliance on animal testing while improving the translational value of preclinical data.
Looking forward, the field aims to develop comprehensive biocompatibility assessment frameworks that integrate traditional safety testing with advanced analytical techniques, including high-throughput screening, omics approaches, and computational modeling. These integrated approaches promise to accelerate hydrogel development while ensuring the highest standards of patient safety and therapeutic efficacy.
Market Analysis for Biocompatible Hydrogel Applications
The global hydrogel market has experienced significant growth in recent years, driven primarily by increasing applications in healthcare, pharmaceuticals, and cosmetics. The biocompatible hydrogel segment specifically has shown remarkable expansion, with the market valued at approximately $15.3 billion in 2022 and projected to reach $23.8 billion by 2027, representing a compound annual growth rate of 9.2%.
Healthcare applications dominate the biocompatible hydrogel market, accounting for nearly 60% of total market share. Within this sector, wound care represents the largest application segment, followed by drug delivery systems and tissue engineering. The aging global population and rising prevalence of chronic wounds, including diabetic ulcers and pressure sores, are key factors driving demand in the wound care segment.
Regionally, North America holds the largest market share at 38%, followed by Europe at 29% and Asia-Pacific at 24%. However, the Asia-Pacific region is experiencing the fastest growth rate, projected at 11.7% annually through 2027, due to improving healthcare infrastructure, increasing healthcare expenditure, and growing awareness of advanced wound care products.
The pharmaceutical application segment is witnessing rapid expansion, particularly in controlled drug delivery systems. Biocompatible hydrogels offer significant advantages in this area, including targeted delivery, sustained release profiles, and reduced side effects. This segment is expected to grow at 10.5% annually, outpacing the overall market growth rate.
Consumer demand is increasingly focused on natural and sustainable hydrogel products, with 73% of surveyed consumers expressing preference for bio-based materials over synthetic alternatives. This trend is particularly pronounced in cosmetics and personal care applications, where natural hydrogels derived from plant sources are gaining significant market traction.
Regulatory considerations significantly impact market dynamics, with FDA and EMA approval processes influencing product development timelines and commercialization strategies. Products with established safety profiles and comprehensive biocompatibility testing documentation experience faster market entry and broader acceptance among healthcare providers.
Price sensitivity varies considerably across application segments, with medical device and pharmaceutical applications demonstrating lower price elasticity compared to cosmetic applications. Premium pricing strategies are viable for hydrogels with enhanced performance characteristics, particularly those with demonstrated improvements in biocompatibility and reduced adverse reactions.
Market barriers include stringent regulatory requirements, high development costs, and technical challenges in scaling production while maintaining consistent quality. New market entrants face significant challenges in establishing clinical evidence and securing reimbursement pathways, particularly in healthcare applications where established products have substantial market presence.
Healthcare applications dominate the biocompatible hydrogel market, accounting for nearly 60% of total market share. Within this sector, wound care represents the largest application segment, followed by drug delivery systems and tissue engineering. The aging global population and rising prevalence of chronic wounds, including diabetic ulcers and pressure sores, are key factors driving demand in the wound care segment.
Regionally, North America holds the largest market share at 38%, followed by Europe at 29% and Asia-Pacific at 24%. However, the Asia-Pacific region is experiencing the fastest growth rate, projected at 11.7% annually through 2027, due to improving healthcare infrastructure, increasing healthcare expenditure, and growing awareness of advanced wound care products.
The pharmaceutical application segment is witnessing rapid expansion, particularly in controlled drug delivery systems. Biocompatible hydrogels offer significant advantages in this area, including targeted delivery, sustained release profiles, and reduced side effects. This segment is expected to grow at 10.5% annually, outpacing the overall market growth rate.
Consumer demand is increasingly focused on natural and sustainable hydrogel products, with 73% of surveyed consumers expressing preference for bio-based materials over synthetic alternatives. This trend is particularly pronounced in cosmetics and personal care applications, where natural hydrogels derived from plant sources are gaining significant market traction.
Regulatory considerations significantly impact market dynamics, with FDA and EMA approval processes influencing product development timelines and commercialization strategies. Products with established safety profiles and comprehensive biocompatibility testing documentation experience faster market entry and broader acceptance among healthcare providers.
Price sensitivity varies considerably across application segments, with medical device and pharmaceutical applications demonstrating lower price elasticity compared to cosmetic applications. Premium pricing strategies are viable for hydrogels with enhanced performance characteristics, particularly those with demonstrated improvements in biocompatibility and reduced adverse reactions.
Market barriers include stringent regulatory requirements, high development costs, and technical challenges in scaling production while maintaining consistent quality. New market entrants face significant challenges in establishing clinical evidence and securing reimbursement pathways, particularly in healthcare applications where established products have substantial market presence.
Current Challenges in Hydrogel Safety Testing
Despite significant advancements in hydrogel technology for biomedical applications, safety testing protocols face several critical challenges that impede efficient translation from laboratory to clinical use. The primary challenge stems from the complex and dynamic nature of hydrogels, whose properties can change significantly in physiological environments. Traditional biocompatibility testing methods, designed primarily for stable materials, often fail to capture these dynamic interactions, leading to incomplete safety profiles.
Regulatory inconsistency presents another major hurdle, with different regions implementing varying requirements for hydrogel safety evaluation. The FDA, EMA, and NMPA each maintain distinct testing protocols, creating confusion for R&D teams developing products for global markets. This regulatory fragmentation increases development costs and extends timelines as companies must navigate multiple compliance pathways.
The lack of standardized testing methodologies specifically designed for hydrogels represents a significant technical gap. Current ISO 10993 standards provide general guidance but lack specific protocols addressing the unique characteristics of hydrogels, such as their water content, degradation profiles, and potential leachable compounds. This absence of hydrogel-specific standards forces researchers to adapt existing protocols, often yielding inconsistent or incomparable results across different laboratories.
Long-term safety assessment remains particularly challenging due to the extended timeframes required to observe potential adverse effects. Hydrogels may undergo structural changes, degradation, or accumulation in tissues over months or years, yet most preclinical testing protocols are limited to weeks or months. This temporal disconnect creates uncertainty regarding long-term biocompatibility and safety profiles.
The diversity of hydrogel compositions further complicates testing approaches. With numerous natural, synthetic, and hybrid formulations available, each with unique chemical structures and biological interactions, developing comprehensive safety testing protocols becomes increasingly difficult. What works for one hydrogel composition may be entirely inappropriate for another, necessitating customized testing strategies.
Emerging applications in advanced therapies, such as 3D bioprinting, drug delivery systems, and tissue engineering, introduce additional complexities. These applications often involve cell-laden hydrogels or complex multi-material constructs that challenge conventional testing paradigms. Current methods struggle to evaluate the safety of these integrated systems where material-cell interactions play crucial roles.
Resource limitations also impact testing capabilities, particularly for startups and academic institutions. Comprehensive safety testing requires specialized equipment, expertise, and significant financial investment, creating barriers to innovation for smaller organizations with promising hydrogel technologies.
Regulatory inconsistency presents another major hurdle, with different regions implementing varying requirements for hydrogel safety evaluation. The FDA, EMA, and NMPA each maintain distinct testing protocols, creating confusion for R&D teams developing products for global markets. This regulatory fragmentation increases development costs and extends timelines as companies must navigate multiple compliance pathways.
The lack of standardized testing methodologies specifically designed for hydrogels represents a significant technical gap. Current ISO 10993 standards provide general guidance but lack specific protocols addressing the unique characteristics of hydrogels, such as their water content, degradation profiles, and potential leachable compounds. This absence of hydrogel-specific standards forces researchers to adapt existing protocols, often yielding inconsistent or incomparable results across different laboratories.
Long-term safety assessment remains particularly challenging due to the extended timeframes required to observe potential adverse effects. Hydrogels may undergo structural changes, degradation, or accumulation in tissues over months or years, yet most preclinical testing protocols are limited to weeks or months. This temporal disconnect creates uncertainty regarding long-term biocompatibility and safety profiles.
The diversity of hydrogel compositions further complicates testing approaches. With numerous natural, synthetic, and hybrid formulations available, each with unique chemical structures and biological interactions, developing comprehensive safety testing protocols becomes increasingly difficult. What works for one hydrogel composition may be entirely inappropriate for another, necessitating customized testing strategies.
Emerging applications in advanced therapies, such as 3D bioprinting, drug delivery systems, and tissue engineering, introduce additional complexities. These applications often involve cell-laden hydrogels or complex multi-material constructs that challenge conventional testing paradigms. Current methods struggle to evaluate the safety of these integrated systems where material-cell interactions play crucial roles.
Resource limitations also impact testing capabilities, particularly for startups and academic institutions. Comprehensive safety testing requires specialized equipment, expertise, and significant financial investment, creating barriers to innovation for smaller organizations with promising hydrogel technologies.
Standard Testing Protocols for Hydrogel Biocompatibility
01 Biocompatibility testing methods for hydrogels
Various testing methods are employed to evaluate the biocompatibility of hydrogels, including in vitro cell culture tests, cytotoxicity assays, and in vivo implantation studies. These methods assess cell viability, proliferation, and tissue response when in contact with hydrogels. Advanced techniques such as histological analysis and immunological testing help determine whether hydrogels cause adverse reactions in biological systems, which is crucial for medical applications.- Biocompatibility assessment methods for hydrogels: Various methods are used to assess the biocompatibility of hydrogels, including in vitro cell culture tests, in vivo implantation studies, and cytotoxicity assays. These methods evaluate cell viability, inflammatory responses, and tissue integration when in contact with hydrogels. Advanced techniques such as histological analysis and immunological testing help determine whether hydrogels are safe for medical applications by measuring cellular responses and potential adverse reactions.
- Natural polymer-based hydrogels for enhanced safety: Hydrogels derived from natural polymers such as collagen, alginate, chitosan, and hyaluronic acid demonstrate superior biocompatibility compared to synthetic alternatives. These biomaterials closely mimic the extracellular matrix of human tissues, reducing immune responses and improving integration with host tissues. Natural polymer-based hydrogels often exhibit lower toxicity profiles and better biodegradability, making them particularly suitable for applications in wound healing, tissue engineering, and drug delivery systems.
- Hydrogel surface modifications for improved biocompatibility: Surface modifications of hydrogels can significantly enhance their biocompatibility and safety profiles. Techniques such as plasma treatment, chemical functionalization, and biomolecule grafting alter the surface properties of hydrogels to improve cell adhesion, reduce protein adsorption, and minimize foreign body responses. These modifications can include incorporating anti-inflammatory agents, antimicrobial compounds, or cell-recognition motifs that promote positive biological interactions while reducing adverse reactions when implanted or applied to biological tissues.
- Degradation behavior and byproduct safety of hydrogels: The degradation behavior of hydrogels is crucial for their biocompatibility and long-term safety. Controlled biodegradation ensures that hydrogels break down into non-toxic byproducts that can be metabolized or excreted by the body. Research focuses on understanding degradation kinetics, identifying potential harmful byproducts, and engineering hydrogels with predictable degradation profiles. Hydrogels designed with environmentally responsive degradation mechanisms can enhance safety by breaking down only under specific physiological conditions, minimizing the risk of premature degradation or persistent foreign material.
- Immunological responses to hydrogel implants: Understanding and controlling immunological responses to hydrogel implants is essential for ensuring their safety and biocompatibility. Hydrogels can trigger various immune reactions ranging from acute inflammation to chronic foreign body responses and fibrotic encapsulation. Advanced hydrogel formulations incorporate immunomodulatory components that can suppress excessive inflammatory responses while promoting healing and tissue integration. Strategies include incorporating anti-inflammatory drugs, designing materials with specific mechanical properties that minimize immune activation, and developing hydrogels that release immunoregulatory factors in a controlled manner.
02 Natural polymer-based hydrogels for enhanced safety
Hydrogels derived from natural polymers such as collagen, alginate, chitosan, and hyaluronic acid demonstrate superior biocompatibility compared to synthetic alternatives. These biomaterials closely mimic the extracellular matrix of natural tissues, reducing immune responses and inflammation. Natural polymer-based hydrogels support cell adhesion, proliferation, and tissue integration, making them particularly suitable for wound healing, tissue engineering, and drug delivery applications.Expand Specific Solutions03 Hydrogel surface modifications for improved biocompatibility
Surface modification techniques can significantly enhance the biocompatibility of hydrogels. Methods include plasma treatment, chemical grafting, and incorporation of bioactive molecules such as peptides or growth factors. These modifications can reduce protein adsorption, prevent bacterial adhesion, and promote specific cell interactions. By tailoring the surface properties, hydrogels can be optimized for specific biomedical applications while minimizing adverse biological responses.Expand Specific Solutions04 Biodegradable hydrogels for medical applications
Biodegradable hydrogels offer significant safety advantages for temporary medical applications as they eliminate the need for removal procedures. These hydrogels are designed to degrade at controlled rates through hydrolytic or enzymatic mechanisms, with degradation products that can be metabolized or excreted by the body. The degradation rate can be tailored by adjusting crosslinking density, polymer composition, and molecular weight, ensuring optimal tissue integration and minimal inflammatory response during the healing process.Expand Specific Solutions05 Toxicity assessment and regulatory considerations for hydrogels
Comprehensive toxicity assessment is essential for hydrogel approval in medical applications. This includes evaluating potential leachables, degradation products, and long-term effects. Regulatory frameworks such as ISO 10993 standards provide guidelines for biological evaluation of medical devices containing hydrogels. Considerations include genotoxicity, carcinogenicity, reproductive toxicity, and systemic effects. Meeting these regulatory requirements ensures that hydrogel-based products are safe for their intended use and can successfully navigate the approval process.Expand Specific Solutions
Leading Organizations in Hydrogel Safety Research
The hydrogel safety and biocompatibility testing landscape is currently in a growth phase, with an expanding market driven by increasing biomedical applications. The field demonstrates moderate technological maturity, with established research institutions like Northwestern University, Ottawa Health Research Institute, and National Research Council of Canada leading fundamental research. Commercial development is advancing through companies including Novo Nordisk, Alkermes, and SentryX BV, which are applying hydrogel technologies in drug delivery and medical devices. Academic-industry partnerships are prominent, with universities (Tsinghua, Zhejiang, Johns Hopkins) collaborating with pharmaceutical companies to address regulatory challenges. The competitive environment is characterized by specialized players focusing on specific applications rather than broad market dominance.
Northwestern University
Technical Solution: Northwestern University has developed a comprehensive hydrogel safety testing protocol that integrates multiple biocompatibility assessment methods. Their approach includes a tiered testing strategy beginning with in vitro cytotoxicity assays using multiple cell lines relevant to the intended application site, followed by protein adsorption studies to evaluate potential immunogenic responses. They've pioneered advanced 3D cell culture models that better mimic in vivo tissue environments for more predictive toxicity screening. Northwestern's researchers have developed specialized protocols for testing stimuli-responsive hydrogels, where biocompatibility is assessed both in the initial and triggered states to ensure safety throughout the material's functional cycle. Their methodology includes degradation product characterization using mass spectrometry and chromatography techniques to identify potentially harmful leachables and extractables that might emerge over the hydrogel's lifecycle.
Strengths: Their integrated approach combining multiple assessment methods provides comprehensive safety profiles. The specialized protocols for stimuli-responsive hydrogels address a critical gap in standard testing procedures. Weaknesses: Their methods often require specialized equipment and expertise not available in all laboratories, potentially limiting widespread adoption of their testing protocols.
Tsinghua University
Technical Solution: Tsinghua University has established a comprehensive hydrogel safety evaluation system that integrates traditional biocompatibility testing with advanced molecular and cellular analysis techniques. Their approach includes high-throughput screening methods for rapidly assessing cytotoxicity across multiple hydrogel formulations, enabling efficient optimization of material compositions. Tsinghua researchers have developed specialized protocols for evaluating the biocompatibility of stimuli-responsive and self-healing hydrogels, with particular attention to potential toxicity of the dynamic chemistries involved in these advanced materials. Their testing checklist includes detailed assessment of protein and cell interactions with hydrogel surfaces using advanced imaging techniques such as atomic force microscopy and super-resolution microscopy to visualize nanoscale biological responses. They've also pioneered methods for evaluating the immunomodulatory properties of hydrogels, recognizing that some applications may benefit from materials that actively direct immune responses rather than simply avoiding them.
Strengths: Their high-throughput screening approaches enable efficient material optimization early in development. Their focus on advanced functional hydrogels addresses emerging safety considerations in next-generation biomaterials. Weaknesses: Some of their more sophisticated analytical techniques may be difficult to standardize across different laboratories, potentially limiting reproducibility of safety assessments.
Critical Biocompatibility Parameters and Testing Innovations
Thermoresponsive Compositions for Dermatological Use and Methods Thereof
PatentInactiveUS20150174292A1
Innovation
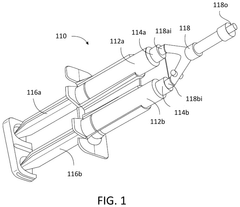
- Development of physically crosslinked dermal fillers using thermoresponsive polymers that transition from a liquid to a hydrogel at physiological temperatures, allowing for minimally invasive administration and enhanced mechanical strength and duration.
Hydrogel-forming systems including biologically innocuous buffer
PatentPendingUS20250064728A1
Innovation
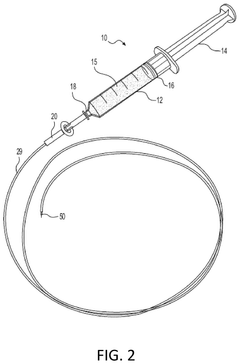
- A hydrogel-forming system comprising a reactive polymer with first reactive groups, a multifunctional compound with second reactive groups that react with the first groups at a pH greater than 7.4, and a biologically innocuous buffer with a pH ranging from 8 to 12, which enhances the safety and efficacy of hydrogel formation.
Regulatory Framework for Hydrogel Medical Applications
The regulatory landscape for hydrogel medical applications is complex and multifaceted, encompassing various international, regional, and national frameworks. At the international level, the International Organization for Standardization (ISO) provides critical standards, particularly ISO 10993 series for biological evaluation of medical devices, which serves as the foundation for hydrogel biocompatibility assessment. These standards outline systematic approaches to evaluate cytotoxicity, sensitization, irritation, and systemic toxicity of hydrogel-based products.
In the United States, the Food and Drug Administration (FDA) regulates hydrogels through various pathways depending on their intended use and risk classification. Hydrogels may be regulated as medical devices under the 510(k) or Premarket Approval (PMA) pathways, or as combination products when incorporating drugs or biologics. The FDA's guidance document "Use of International Standard ISO 10993-1" provides specific recommendations for biocompatibility testing of hydrogels based on their patient contact duration and tissue interaction.
The European Union's regulatory framework has undergone significant transformation with the implementation of the Medical Device Regulation (MDR 2017/745) and In Vitro Diagnostic Regulation (IVDR 2017/746). These regulations impose more stringent requirements for clinical evidence, post-market surveillance, and technical documentation for hydrogel-based medical devices. The classification rules under MDR have particular implications for hydrogels, especially those intended for wound healing, drug delivery, or tissue engineering applications.
In Asia, Japan's Pharmaceuticals and Medical Devices Agency (PMDA) and China's National Medical Products Administration (NMPA) have established specific pathways for hydrogel medical applications. Japan's approach emphasizes early consultation and stepwise development, while China has implemented a reformed regulatory system with special provisions for innovative medical technologies including advanced hydrogels.
Regulatory considerations specifically for hydrogel safety testing include leachable and extractable testing requirements, degradation product characterization, and long-term biocompatibility assessment. The FDA's recent emphasis on the use of alternative testing methods to reduce animal testing has implications for hydrogel developers, encouraging the adoption of in vitro methods where scientifically justified.
Emerging regulatory trends affecting hydrogel medical applications include the development of specific guidance for tissue-engineered products, increased scrutiny of nanomaterials in medical applications, and growing emphasis on real-world evidence for regulatory decision-making. Regulatory agencies are also increasingly focusing on environmental impact assessments for biodegradable hydrogels, particularly those containing novel synthetic polymers.
In the United States, the Food and Drug Administration (FDA) regulates hydrogels through various pathways depending on their intended use and risk classification. Hydrogels may be regulated as medical devices under the 510(k) or Premarket Approval (PMA) pathways, or as combination products when incorporating drugs or biologics. The FDA's guidance document "Use of International Standard ISO 10993-1" provides specific recommendations for biocompatibility testing of hydrogels based on their patient contact duration and tissue interaction.
The European Union's regulatory framework has undergone significant transformation with the implementation of the Medical Device Regulation (MDR 2017/745) and In Vitro Diagnostic Regulation (IVDR 2017/746). These regulations impose more stringent requirements for clinical evidence, post-market surveillance, and technical documentation for hydrogel-based medical devices. The classification rules under MDR have particular implications for hydrogels, especially those intended for wound healing, drug delivery, or tissue engineering applications.
In Asia, Japan's Pharmaceuticals and Medical Devices Agency (PMDA) and China's National Medical Products Administration (NMPA) have established specific pathways for hydrogel medical applications. Japan's approach emphasizes early consultation and stepwise development, while China has implemented a reformed regulatory system with special provisions for innovative medical technologies including advanced hydrogels.
Regulatory considerations specifically for hydrogel safety testing include leachable and extractable testing requirements, degradation product characterization, and long-term biocompatibility assessment. The FDA's recent emphasis on the use of alternative testing methods to reduce animal testing has implications for hydrogel developers, encouraging the adoption of in vitro methods where scientifically justified.
Emerging regulatory trends affecting hydrogel medical applications include the development of specific guidance for tissue-engineered products, increased scrutiny of nanomaterials in medical applications, and growing emphasis on real-world evidence for regulatory decision-making. Regulatory agencies are also increasingly focusing on environmental impact assessments for biodegradable hydrogels, particularly those containing novel synthetic polymers.
Risk Management Strategies for Hydrogel Development
Effective risk management is essential for successful hydrogel development, particularly when considering the complex safety and biocompatibility requirements these materials must meet. A comprehensive risk management framework begins with systematic hazard identification across the entire development lifecycle, from raw material selection to final product disposal. This process should incorporate both historical data from similar hydrogel applications and theoretical risk analysis to identify potential failure modes.
Risk assessment methodologies for hydrogels should follow established standards such as ISO 14971 for medical applications, with particular attention to chemical leaching, degradation byproducts, and immunological responses. Quantitative risk scoring systems that evaluate both the severity and probability of adverse events provide valuable metrics for prioritizing mitigation efforts. Teams should develop risk matrices specific to hydrogel applications that account for the unique properties of these materials.
Mitigation strategies must be tailored to the specific risks identified. For cytotoxicity concerns, purification protocols can be enhanced and residual monomer content strictly controlled. Immunogenicity risks may be addressed through careful polymer selection and surface modification techniques. Mechanical failure risks require thorough testing under physiological conditions that simulate the intended application environment. Documentation of these strategies should be maintained in a living risk management file that evolves throughout development.
Continuous monitoring represents a critical component of effective risk management. This includes implementing robust change control procedures that evaluate how modifications to formulation, processing, or application might impact the safety profile. Regular review cycles should be scheduled at predetermined development milestones, with additional reviews triggered by significant findings or changes to regulatory requirements.
Cross-functional collaboration enhances risk management effectiveness by incorporating diverse perspectives. Regular risk review meetings should include representatives from R&D, regulatory affairs, quality assurance, and clinical specialists when applicable. This collaborative approach ensures comprehensive risk identification and practical mitigation strategies that balance innovation with safety considerations.
Regulatory compliance must be integrated into the risk management process from the earliest stages. Teams should maintain awareness of evolving regulatory frameworks for hydrogels across target markets and proactively address emerging concerns. This forward-looking approach not only facilitates eventual regulatory approval but also builds a foundation of safety data that supports continued development and commercialization efforts.
Risk assessment methodologies for hydrogels should follow established standards such as ISO 14971 for medical applications, with particular attention to chemical leaching, degradation byproducts, and immunological responses. Quantitative risk scoring systems that evaluate both the severity and probability of adverse events provide valuable metrics for prioritizing mitigation efforts. Teams should develop risk matrices specific to hydrogel applications that account for the unique properties of these materials.
Mitigation strategies must be tailored to the specific risks identified. For cytotoxicity concerns, purification protocols can be enhanced and residual monomer content strictly controlled. Immunogenicity risks may be addressed through careful polymer selection and surface modification techniques. Mechanical failure risks require thorough testing under physiological conditions that simulate the intended application environment. Documentation of these strategies should be maintained in a living risk management file that evolves throughout development.
Continuous monitoring represents a critical component of effective risk management. This includes implementing robust change control procedures that evaluate how modifications to formulation, processing, or application might impact the safety profile. Regular review cycles should be scheduled at predetermined development milestones, with additional reviews triggered by significant findings or changes to regulatory requirements.
Cross-functional collaboration enhances risk management effectiveness by incorporating diverse perspectives. Regular risk review meetings should include representatives from R&D, regulatory affairs, quality assurance, and clinical specialists when applicable. This collaborative approach ensures comprehensive risk identification and practical mitigation strategies that balance innovation with safety considerations.
Regulatory compliance must be integrated into the risk management process from the earliest stages. Teams should maintain awareness of evolving regulatory frameworks for hydrogels across target markets and proactively address emerging concerns. This forward-looking approach not only facilitates eventual regulatory approval but also builds a foundation of safety data that supports continued development and commercialization efforts.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!