Analysis of P wave changes in hypertrophic cardiomyopathy
AUG 19, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
P Wave Analysis Background and Objectives
P wave analysis in electrocardiography (ECG) has been a crucial tool in cardiac diagnostics for decades. The P wave represents atrial depolarization and provides valuable insights into the electrical activity of the heart's upper chambers. In the context of hypertrophic cardiomyopathy (HCM), a genetic disorder characterized by thickening of the heart muscle, P wave analysis has gained significant attention due to its potential in early detection and risk stratification.
The evolution of P wave analysis techniques has been closely tied to advancements in ECG technology and signal processing. Early studies focused on basic measurements such as P wave duration and amplitude. However, as our understanding of cardiac electrophysiology improved, more sophisticated analyses emerged, including P wave morphology, dispersion, and terminal force.
Recent technological developments have further enhanced our ability to extract meaningful information from P waves. High-resolution ECG systems, advanced signal processing algorithms, and machine learning techniques have opened new avenues for P wave analysis in HCM. These advancements allow for more precise measurements and the identification of subtle changes that may indicate the presence or progression of the disease.
The primary objective of P wave analysis in HCM is to improve early diagnosis and risk assessment. HCM is often asymptomatic in its early stages, making early detection challenging. By identifying specific P wave alterations associated with HCM, clinicians aim to detect the disease before the onset of symptoms or the development of severe complications such as sudden cardiac death.
Another key goal is to enhance our understanding of the pathophysiological mechanisms underlying HCM. P wave changes can provide insights into atrial remodeling, conduction abnormalities, and electrophysiological adaptations in response to myocardial hypertrophy. This knowledge is crucial for developing targeted therapies and improving patient management strategies.
Furthermore, P wave analysis in HCM aims to contribute to risk stratification models. By correlating P wave parameters with clinical outcomes, researchers seek to identify high-risk individuals who may benefit from more aggressive interventions or closer monitoring. This personalized approach to patient care has the potential to significantly improve long-term outcomes in HCM patients.
As research in this field progresses, there is a growing emphasis on standardizing P wave analysis techniques and establishing robust, reproducible methods. This standardization is essential for comparing results across studies and translating findings into clinical practice. Additionally, efforts are being made to integrate P wave analysis with other diagnostic modalities, such as echocardiography and cardiac magnetic resonance imaging, to provide a more comprehensive assessment of cardiac structure and function in HCM patients.
The evolution of P wave analysis techniques has been closely tied to advancements in ECG technology and signal processing. Early studies focused on basic measurements such as P wave duration and amplitude. However, as our understanding of cardiac electrophysiology improved, more sophisticated analyses emerged, including P wave morphology, dispersion, and terminal force.
Recent technological developments have further enhanced our ability to extract meaningful information from P waves. High-resolution ECG systems, advanced signal processing algorithms, and machine learning techniques have opened new avenues for P wave analysis in HCM. These advancements allow for more precise measurements and the identification of subtle changes that may indicate the presence or progression of the disease.
The primary objective of P wave analysis in HCM is to improve early diagnosis and risk assessment. HCM is often asymptomatic in its early stages, making early detection challenging. By identifying specific P wave alterations associated with HCM, clinicians aim to detect the disease before the onset of symptoms or the development of severe complications such as sudden cardiac death.
Another key goal is to enhance our understanding of the pathophysiological mechanisms underlying HCM. P wave changes can provide insights into atrial remodeling, conduction abnormalities, and electrophysiological adaptations in response to myocardial hypertrophy. This knowledge is crucial for developing targeted therapies and improving patient management strategies.
Furthermore, P wave analysis in HCM aims to contribute to risk stratification models. By correlating P wave parameters with clinical outcomes, researchers seek to identify high-risk individuals who may benefit from more aggressive interventions or closer monitoring. This personalized approach to patient care has the potential to significantly improve long-term outcomes in HCM patients.
As research in this field progresses, there is a growing emphasis on standardizing P wave analysis techniques and establishing robust, reproducible methods. This standardization is essential for comparing results across studies and translating findings into clinical practice. Additionally, efforts are being made to integrate P wave analysis with other diagnostic modalities, such as echocardiography and cardiac magnetic resonance imaging, to provide a more comprehensive assessment of cardiac structure and function in HCM patients.
Clinical Demand for HCM Diagnosis
Hypertrophic cardiomyopathy (HCM) is a complex cardiac condition characterized by thickening of the heart muscle, particularly the left ventricle. The clinical demand for accurate and early diagnosis of HCM has been steadily increasing due to its significant impact on patient outcomes and quality of life. As a leading cause of sudden cardiac death in young adults and athletes, HCM presents a critical challenge for healthcare providers and researchers alike.
The current diagnostic landscape for HCM relies heavily on imaging techniques such as echocardiography and cardiac magnetic resonance imaging (MRI). However, these methods often detect HCM only after significant structural changes have occurred in the heart. This limitation underscores the urgent need for more sensitive and specific diagnostic tools that can identify HCM at earlier stages, potentially before the onset of symptoms or irreversible cardiac remodeling.
Electrocardiography (ECG) has long been recognized as a valuable tool in the initial evaluation of patients suspected of having HCM. The analysis of P wave changes in ECG recordings has emerged as a promising avenue for enhancing HCM diagnosis. P waves, which represent atrial depolarization, can provide crucial insights into the electrical and structural abnormalities associated with HCM, even before visible changes in heart muscle thickness are detectable through imaging.
The clinical demand for improved HCM diagnosis through P wave analysis is driven by several factors. Firstly, ECG is a widely available, non-invasive, and cost-effective diagnostic tool, making it ideal for widespread screening and early detection efforts. Secondly, the potential for P wave analysis to detect subtle electrical changes that precede structural alterations could revolutionize the timing and effectiveness of HCM interventions.
Moreover, the integration of advanced signal processing techniques and machine learning algorithms in P wave analysis has opened new possibilities for enhancing diagnostic accuracy and predictive capabilities. This technological advancement aligns with the growing trend towards personalized medicine, where early and precise diagnosis can guide tailored treatment strategies and improve patient outcomes.
The clinical community has expressed a strong interest in developing standardized criteria for P wave analysis in HCM diagnosis. This demand is fueled by the need for reliable, reproducible, and easily interpretable diagnostic markers that can be widely adopted in clinical practice. Such standardization would not only improve diagnostic consistency across healthcare settings but also facilitate large-scale research efforts and clinical trials focused on HCM prevention and treatment.
In conclusion, the analysis of P wave changes in HCM represents a critical area of clinical demand, offering the potential to transform the diagnostic paradigm for this challenging cardiac condition. As research in this field progresses, it is anticipated that P wave analysis will become an integral component of comprehensive HCM evaluation protocols, complementing existing imaging techniques and genetic testing to provide a more complete picture of cardiac health and risk stratification.
The current diagnostic landscape for HCM relies heavily on imaging techniques such as echocardiography and cardiac magnetic resonance imaging (MRI). However, these methods often detect HCM only after significant structural changes have occurred in the heart. This limitation underscores the urgent need for more sensitive and specific diagnostic tools that can identify HCM at earlier stages, potentially before the onset of symptoms or irreversible cardiac remodeling.
Electrocardiography (ECG) has long been recognized as a valuable tool in the initial evaluation of patients suspected of having HCM. The analysis of P wave changes in ECG recordings has emerged as a promising avenue for enhancing HCM diagnosis. P waves, which represent atrial depolarization, can provide crucial insights into the electrical and structural abnormalities associated with HCM, even before visible changes in heart muscle thickness are detectable through imaging.
The clinical demand for improved HCM diagnosis through P wave analysis is driven by several factors. Firstly, ECG is a widely available, non-invasive, and cost-effective diagnostic tool, making it ideal for widespread screening and early detection efforts. Secondly, the potential for P wave analysis to detect subtle electrical changes that precede structural alterations could revolutionize the timing and effectiveness of HCM interventions.
Moreover, the integration of advanced signal processing techniques and machine learning algorithms in P wave analysis has opened new possibilities for enhancing diagnostic accuracy and predictive capabilities. This technological advancement aligns with the growing trend towards personalized medicine, where early and precise diagnosis can guide tailored treatment strategies and improve patient outcomes.
The clinical community has expressed a strong interest in developing standardized criteria for P wave analysis in HCM diagnosis. This demand is fueled by the need for reliable, reproducible, and easily interpretable diagnostic markers that can be widely adopted in clinical practice. Such standardization would not only improve diagnostic consistency across healthcare settings but also facilitate large-scale research efforts and clinical trials focused on HCM prevention and treatment.
In conclusion, the analysis of P wave changes in HCM represents a critical area of clinical demand, offering the potential to transform the diagnostic paradigm for this challenging cardiac condition. As research in this field progresses, it is anticipated that P wave analysis will become an integral component of comprehensive HCM evaluation protocols, complementing existing imaging techniques and genetic testing to provide a more complete picture of cardiac health and risk stratification.
Current P Wave Analysis Techniques and Challenges
P wave analysis in electrocardiograms (ECGs) has become increasingly important in the diagnosis and management of hypertrophic cardiomyopathy (HCM). Current techniques for P wave analysis primarily focus on measuring various parameters such as P wave duration, amplitude, and morphology. These measurements are typically performed using digital signal processing algorithms applied to high-resolution ECG recordings.
One of the most common methods for P wave analysis is the time-domain approach, which involves identifying the onset and offset of the P wave to calculate its duration. Advanced algorithms have been developed to automatically detect these fiducial points, improving the accuracy and reproducibility of measurements. However, challenges remain in precisely determining the P wave boundaries, especially in cases of low-amplitude or noisy signals.
Frequency-domain analysis techniques, such as spectral analysis and wavelet transforms, have also been employed to extract additional information from P waves. These methods can reveal subtle changes in P wave morphology that may not be apparent in time-domain measurements alone. Spectral analysis can provide insights into the frequency content of P waves, which may be altered in HCM patients due to atrial remodeling.
Machine learning and artificial intelligence approaches have recently gained traction in P wave analysis. These techniques leverage large datasets to identify complex patterns and features that may be indicative of HCM. Convolutional neural networks and deep learning models have shown promise in automatically classifying P waves and detecting abnormalities associated with HCM.
Despite these advancements, several challenges persist in P wave analysis for HCM. One major issue is the variability in P wave morphology among individuals, which can make it difficult to establish standardized criteria for abnormality. Additionally, the presence of noise and artifacts in ECG recordings can significantly impact the accuracy of P wave measurements, particularly in ambulatory or long-term monitoring settings.
Another challenge lies in the interpretation of P wave changes in the context of HCM. While certain P wave characteristics have been associated with HCM, such as increased P wave duration and altered morphology, the specificity and sensitivity of these markers remain subjects of ongoing research. Furthermore, distinguishing P wave changes due to HCM from those caused by other cardiac conditions or normal physiological variations can be challenging.
The integration of P wave analysis with other clinical and imaging data presents both an opportunity and a challenge. Combining P wave measurements with echocardiographic findings, genetic information, and other biomarkers could potentially improve the diagnostic accuracy for HCM. However, developing robust algorithms that can effectively synthesize this diverse data remains a significant technical hurdle.
One of the most common methods for P wave analysis is the time-domain approach, which involves identifying the onset and offset of the P wave to calculate its duration. Advanced algorithms have been developed to automatically detect these fiducial points, improving the accuracy and reproducibility of measurements. However, challenges remain in precisely determining the P wave boundaries, especially in cases of low-amplitude or noisy signals.
Frequency-domain analysis techniques, such as spectral analysis and wavelet transforms, have also been employed to extract additional information from P waves. These methods can reveal subtle changes in P wave morphology that may not be apparent in time-domain measurements alone. Spectral analysis can provide insights into the frequency content of P waves, which may be altered in HCM patients due to atrial remodeling.
Machine learning and artificial intelligence approaches have recently gained traction in P wave analysis. These techniques leverage large datasets to identify complex patterns and features that may be indicative of HCM. Convolutional neural networks and deep learning models have shown promise in automatically classifying P waves and detecting abnormalities associated with HCM.
Despite these advancements, several challenges persist in P wave analysis for HCM. One major issue is the variability in P wave morphology among individuals, which can make it difficult to establish standardized criteria for abnormality. Additionally, the presence of noise and artifacts in ECG recordings can significantly impact the accuracy of P wave measurements, particularly in ambulatory or long-term monitoring settings.
Another challenge lies in the interpretation of P wave changes in the context of HCM. While certain P wave characteristics have been associated with HCM, such as increased P wave duration and altered morphology, the specificity and sensitivity of these markers remain subjects of ongoing research. Furthermore, distinguishing P wave changes due to HCM from those caused by other cardiac conditions or normal physiological variations can be challenging.
The integration of P wave analysis with other clinical and imaging data presents both an opportunity and a challenge. Combining P wave measurements with echocardiographic findings, genetic information, and other biomarkers could potentially improve the diagnostic accuracy for HCM. However, developing robust algorithms that can effectively synthesize this diverse data remains a significant technical hurdle.
Existing P Wave Analysis Methods for HCM
01 P wave detection and analysis in ECG signals
Various methods and devices are developed for detecting and analyzing P waves in electrocardiogram (ECG) signals. These techniques aim to improve the accuracy of P wave identification, which is crucial for diagnosing cardiac conditions. The systems may involve signal processing, feature extraction, and machine learning algorithms to enhance P wave detection and characterization.- P wave detection and analysis in ECG signals: Various methods and devices are developed for detecting and analyzing P waves in electrocardiogram (ECG) signals. These techniques aim to improve the accuracy of P wave identification, which is crucial for diagnosing cardiac conditions related to atrial activity.
- P wave changes in seismic exploration: In seismic exploration, P wave changes are analyzed to gather information about subsurface structures. Technologies are developed to detect, measure, and interpret P wave variations for geological surveying and resource exploration purposes.
- P wave monitoring in medical devices: Medical devices are designed to monitor P wave changes in real-time, providing continuous assessment of cardiac function. These devices can be implantable or external and are used for both diagnostic and therapeutic purposes in cardiology.
- P wave signal processing and filtering: Advanced signal processing and filtering techniques are employed to enhance P wave detection and analysis. These methods aim to reduce noise, improve signal quality, and extract meaningful information from P wave changes in various applications.
- P wave changes in communication systems: In communication systems, P wave changes are utilized for signal modulation and transmission. Technologies are developed to manipulate P waves for efficient data transfer and to mitigate the effects of signal distortion during propagation.
02 P wave morphology changes in cardiac monitoring
Monitoring and analyzing changes in P wave morphology can provide valuable insights into cardiac health. Systems are designed to detect alterations in P wave shape, duration, and amplitude, which may indicate various cardiac abnormalities. These changes can be used for early detection of atrial fibrillation, atrial flutter, and other arrhythmias.Expand Specific Solutions03 P wave measurement in seismic exploration
In the field of seismic exploration, P waves are used to gather information about subsurface structures. Techniques and devices are developed to measure and analyze P wave characteristics, such as velocity and arrival time. These measurements are crucial for creating accurate subsurface models in oil and gas exploration, as well as in geological studies.Expand Specific Solutions04 P wave-based cardiac pacing systems
Advanced cardiac pacing systems utilize P wave detection and analysis to optimize pacing therapy. These systems can adjust pacing parameters based on P wave characteristics, ensuring proper synchronization between atrial and ventricular contractions. Such adaptive pacing techniques aim to improve cardiac function and patient outcomes in individuals with various heart rhythm disorders.Expand Specific Solutions05 P wave analysis in wearable health monitoring devices
Wearable devices incorporating P wave analysis capabilities are being developed for continuous cardiac monitoring. These devices can detect and analyze P waves in real-time, providing users with information about their heart rhythm and potential cardiac issues. The integration of P wave analysis in wearable technology allows for early detection of cardiac abnormalities and promotes proactive health management.Expand Specific Solutions
Key Players in Cardiac Imaging and ECG Analysis
The analysis of P wave changes in hypertrophic cardiomyopathy is currently in a growth phase, with increasing market size and technological advancements. The competitive landscape is diverse, featuring academic institutions like Wuhan University and Yale University, alongside established medical technology companies such as Medtronic and Boston Scientific Scimed. Emerging players like Bardy Diagnostics and Senbiosys are introducing innovative cardiac monitoring solutions, indicating a moderate level of technological maturity. The involvement of pharmaceutical giants like Roche and Novartis suggests potential for integrating diagnostics with targeted therapies. This multifaceted approach to P wave analysis reflects the growing importance of precise cardiac diagnostics in managing hypertrophic cardiomyopathy.
Boston Scientific Scimed, Inc.
Technical Solution: Boston Scientific has developed a comprehensive P wave analysis platform for HCM patients, focusing on both invasive and non-invasive assessment methods. Their approach combines surface ECG analysis with intracardiac electrogram data obtained from implantable cardiac monitors or electrophysiology studies[8]. The system utilizes advanced signal processing algorithms to analyze P wave morphology, duration, and dispersion across multiple leads. Boston Scientific's technology also incorporates atrial strain analysis derived from echocardiography to provide a more complete picture of atrial remodeling in HCM patients[10]. The platform includes predictive models that use P wave characteristics to assess the risk of atrial fibrillation and other arrhythmias commonly associated with HCM[12].
Strengths: Combination of invasive and non-invasive assessment methods, integration of multiple data sources. Weaknesses: May require invasive procedures for comprehensive analysis, potentially limiting widespread applicability.
Koninklijke Philips NV
Technical Solution: Philips has developed an AI-powered ECG analysis system for detecting P wave changes in HCM patients. Their approach utilizes deep learning algorithms trained on large datasets of ECG recordings from HCM patients and healthy controls[7]. The system can automatically segment P waves and extract relevant features such as duration, amplitude, and morphology. Philips' technology also incorporates vectorcardiography to provide a three-dimensional analysis of atrial depolarization[9]. The AI model can detect subtle P wave abnormalities that may be indicative of HCM, even in its early stages. Furthermore, the system integrates with Philips' broader cardiac care ecosystem, allowing for seamless data sharing and longitudinal patient monitoring[11].
Strengths: AI-powered analysis, integration with broader cardiac care ecosystem, and vectorcardiography capabilities. Weaknesses: Dependence on large datasets for AI training and potential need for ongoing algorithm updates.
Innovative P Wave Morphology Assessment in HCM
Sensor for ventricular and outflow tract obstruction
PatentWO2017044870A1
Innovation
- A non-invasive method using plethysmographic signals from wrist or fingertip sensors to generate waveforms, processing them to estimate systolic time intervals and pressure gradients between the left ventricle and aorta, allowing for continuous monitoring outside a clinical setting.
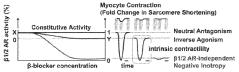
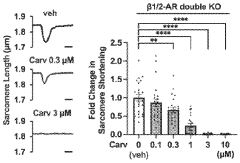
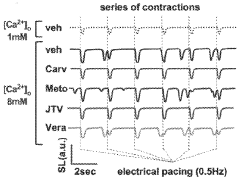
Formulations and methods of treatment for hypertrophic cardiomyopathy
PatentWO2024151866A1
Innovation
- The use of enantiomeric R-carvedilol, which is non-beta-blocking, is administered to suppress contractility and arrhythmias in cardiomyocytes with genetic mutations causing HCM, without lowering heart rate or cardiac output, thereby alleviating hypercontractility and improving cardiac output.
AI Integration in ECG Interpretation
The integration of artificial intelligence (AI) in ECG interpretation has revolutionized the analysis of P wave changes in hypertrophic cardiomyopathy (HCM). This technological advancement has significantly enhanced the accuracy and efficiency of diagnosing and monitoring this complex cardiac condition.
AI algorithms, particularly deep learning models, have demonstrated remarkable capabilities in detecting subtle P wave abnormalities associated with HCM. These models can analyze vast amounts of ECG data, identifying patterns and changes that may be challenging for human interpreters to discern consistently. By leveraging large datasets of ECG recordings from HCM patients, AI systems have been trained to recognize specific P wave morphologies, durations, and amplitudes characteristic of the disease.
One of the key advantages of AI integration in ECG interpretation for HCM is its ability to provide quantitative assessments of P wave changes over time. This longitudinal analysis can help clinicians track disease progression and evaluate the effectiveness of interventions. AI-powered ECG analysis tools can automatically measure and report P wave parameters, such as P wave duration, amplitude, and dispersion, which are crucial indicators of atrial remodeling in HCM.
Furthermore, AI algorithms have shown promise in risk stratification for HCM patients based on P wave characteristics. By correlating P wave changes with clinical outcomes, these systems can assist in identifying patients at higher risk of developing complications such as atrial fibrillation or sudden cardiac death. This predictive capability enables more personalized management strategies and targeted interventions.
The integration of AI in ECG interpretation has also facilitated the development of mobile and wearable ECG devices for continuous monitoring of HCM patients. These AI-enabled devices can perform real-time analysis of P wave changes, providing early warning signs of potential cardiac events and allowing for timely medical intervention.
Despite these advancements, challenges remain in the widespread adoption of AI for ECG interpretation in HCM. Ensuring the generalizability of AI models across diverse patient populations and different ECG recording systems is crucial. Additionally, the interpretability of AI-generated results and the integration of these tools into existing clinical workflows require ongoing research and development.
As AI technology continues to evolve, its role in analyzing P wave changes in HCM is expected to expand further. Future developments may include more sophisticated algorithms capable of integrating ECG data with other clinical and imaging parameters, providing a more comprehensive assessment of HCM patients. The ongoing collaboration between cardiologists, data scientists, and AI researchers will be essential in refining these tools and maximizing their clinical impact in the management of hypertrophic cardiomyopathy.
AI algorithms, particularly deep learning models, have demonstrated remarkable capabilities in detecting subtle P wave abnormalities associated with HCM. These models can analyze vast amounts of ECG data, identifying patterns and changes that may be challenging for human interpreters to discern consistently. By leveraging large datasets of ECG recordings from HCM patients, AI systems have been trained to recognize specific P wave morphologies, durations, and amplitudes characteristic of the disease.
One of the key advantages of AI integration in ECG interpretation for HCM is its ability to provide quantitative assessments of P wave changes over time. This longitudinal analysis can help clinicians track disease progression and evaluate the effectiveness of interventions. AI-powered ECG analysis tools can automatically measure and report P wave parameters, such as P wave duration, amplitude, and dispersion, which are crucial indicators of atrial remodeling in HCM.
Furthermore, AI algorithms have shown promise in risk stratification for HCM patients based on P wave characteristics. By correlating P wave changes with clinical outcomes, these systems can assist in identifying patients at higher risk of developing complications such as atrial fibrillation or sudden cardiac death. This predictive capability enables more personalized management strategies and targeted interventions.
The integration of AI in ECG interpretation has also facilitated the development of mobile and wearable ECG devices for continuous monitoring of HCM patients. These AI-enabled devices can perform real-time analysis of P wave changes, providing early warning signs of potential cardiac events and allowing for timely medical intervention.
Despite these advancements, challenges remain in the widespread adoption of AI for ECG interpretation in HCM. Ensuring the generalizability of AI models across diverse patient populations and different ECG recording systems is crucial. Additionally, the interpretability of AI-generated results and the integration of these tools into existing clinical workflows require ongoing research and development.
As AI technology continues to evolve, its role in analyzing P wave changes in HCM is expected to expand further. Future developments may include more sophisticated algorithms capable of integrating ECG data with other clinical and imaging parameters, providing a more comprehensive assessment of HCM patients. The ongoing collaboration between cardiologists, data scientists, and AI researchers will be essential in refining these tools and maximizing their clinical impact in the management of hypertrophic cardiomyopathy.
Standardization of P Wave Analysis Criteria
The standardization of P wave analysis criteria is crucial for accurate and consistent evaluation of P wave changes in hypertrophic cardiomyopathy (HCM). This process involves establishing uniform guidelines for measuring and interpreting P wave characteristics across different electrocardiogram (ECG) recordings and clinical settings.
One of the primary aspects of standardization is defining precise measurement techniques for P wave duration, amplitude, and morphology. This includes specifying the exact lead positions and time intervals for measurements, as well as establishing clear criteria for identifying the onset and offset of the P wave. Standardized methods for calculating P wave dispersion and assessing P wave axis are also essential components of this process.
Another critical element is the development of normative values for P wave parameters in healthy individuals, which serve as reference points for identifying abnormalities in HCM patients. These reference ranges should account for variations due to age, gender, and other demographic factors to ensure accurate interpretation across diverse patient populations.
Standardization efforts also focus on defining specific criteria for classifying P wave abnormalities in HCM. This includes establishing thresholds for P wave duration, amplitude, and morphology changes that are indicative of left atrial enlargement or other atrial remodeling processes associated with HCM. Clear guidelines for identifying and categorizing P wave notching, fragmentation, and other morphological alterations are crucial for consistent diagnosis and monitoring of disease progression.
The implementation of automated P wave analysis algorithms is an important aspect of standardization. These algorithms should be validated against expert manual measurements and demonstrate high reproducibility across different ECG recording systems. Standardized protocols for algorithm development, testing, and validation are necessary to ensure reliability and comparability of results across different research studies and clinical settings.
Efforts to standardize P wave analysis criteria also involve establishing consensus guidelines for reporting and interpreting P wave changes in HCM. This includes developing standardized terminology and classification systems for describing P wave abnormalities, as well as providing clear recommendations for integrating P wave analysis into overall ECG interpretation and clinical decision-making processes for HCM patients.
International collaboration and consensus-building among cardiology experts, electrophysiologists, and ECG specialists are essential for developing and implementing standardized P wave analysis criteria. Regular review and updates of these standards are necessary to incorporate new research findings and technological advancements in ECG recording and analysis techniques.
One of the primary aspects of standardization is defining precise measurement techniques for P wave duration, amplitude, and morphology. This includes specifying the exact lead positions and time intervals for measurements, as well as establishing clear criteria for identifying the onset and offset of the P wave. Standardized methods for calculating P wave dispersion and assessing P wave axis are also essential components of this process.
Another critical element is the development of normative values for P wave parameters in healthy individuals, which serve as reference points for identifying abnormalities in HCM patients. These reference ranges should account for variations due to age, gender, and other demographic factors to ensure accurate interpretation across diverse patient populations.
Standardization efforts also focus on defining specific criteria for classifying P wave abnormalities in HCM. This includes establishing thresholds for P wave duration, amplitude, and morphology changes that are indicative of left atrial enlargement or other atrial remodeling processes associated with HCM. Clear guidelines for identifying and categorizing P wave notching, fragmentation, and other morphological alterations are crucial for consistent diagnosis and monitoring of disease progression.
The implementation of automated P wave analysis algorithms is an important aspect of standardization. These algorithms should be validated against expert manual measurements and demonstrate high reproducibility across different ECG recording systems. Standardized protocols for algorithm development, testing, and validation are necessary to ensure reliability and comparability of results across different research studies and clinical settings.
Efforts to standardize P wave analysis criteria also involve establishing consensus guidelines for reporting and interpreting P wave changes in HCM. This includes developing standardized terminology and classification systems for describing P wave abnormalities, as well as providing clear recommendations for integrating P wave analysis into overall ECG interpretation and clinical decision-making processes for HCM patients.
International collaboration and consensus-building among cardiology experts, electrophysiologists, and ECG specialists are essential for developing and implementing standardized P wave analysis criteria. Regular review and updates of these standards are necessary to incorporate new research findings and technological advancements in ECG recording and analysis techniques.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!