Comparative studies of P wave indices across cardiovascular pathologies
AUG 19, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
P Wave Analysis Background
P wave analysis has been a cornerstone in cardiovascular research and clinical practice for decades. The P wave, representing atrial depolarization in the electrocardiogram (ECG), provides valuable insights into atrial electrophysiology and structural changes. Its importance in diagnosing and predicting various cardiovascular pathologies has been increasingly recognized in recent years.
Historically, P wave analysis began with simple measurements of duration and amplitude. However, as technology and understanding advanced, more sophisticated indices were developed. These include P wave dispersion, P wave terminal force, P wave area, and various morphological characteristics. Each of these indices offers unique perspectives on atrial function and structure.
The evolution of P wave analysis has been closely tied to advancements in ECG technology. The transition from standard 12-lead ECGs to high-resolution and multi-lead systems has significantly enhanced the precision and scope of P wave measurements. This technological progress has enabled researchers and clinicians to detect subtle changes in atrial electrophysiology that were previously unobservable.
In the context of cardiovascular pathologies, P wave analysis has proven particularly valuable. It has been extensively studied in conditions such as atrial fibrillation, hypertension, heart failure, and various structural heart diseases. The ability of P wave indices to reflect both electrical and structural remodeling of the atria makes them powerful tools for risk stratification and early detection of cardiovascular abnormalities.
Comparative studies of P wave indices across different cardiovascular pathologies have emerged as a critical area of research. These studies aim to identify specific P wave characteristics associated with particular diseases, potentially leading to more accurate diagnostic and prognostic tools. For instance, differences in P wave morphology and duration have been observed between patients with paroxysmal atrial fibrillation and those with persistent atrial fibrillation.
The clinical significance of P wave analysis extends beyond diagnosis. It has shown promise in predicting the onset of atrial fibrillation, assessing the risk of recurrence after cardioversion, and evaluating the effectiveness of various therapeutic interventions. This predictive capability makes P wave analysis an invaluable tool in personalized medicine approaches to cardiovascular care.
As research in this field progresses, there is a growing emphasis on standardizing P wave measurement techniques and establishing normative values across different populations. This standardization is crucial for ensuring the reliability and comparability of results across studies and clinical settings. Additionally, efforts are being made to integrate P wave analysis into automated ECG interpretation systems, potentially expanding its use in routine clinical practice.
Historically, P wave analysis began with simple measurements of duration and amplitude. However, as technology and understanding advanced, more sophisticated indices were developed. These include P wave dispersion, P wave terminal force, P wave area, and various morphological characteristics. Each of these indices offers unique perspectives on atrial function and structure.
The evolution of P wave analysis has been closely tied to advancements in ECG technology. The transition from standard 12-lead ECGs to high-resolution and multi-lead systems has significantly enhanced the precision and scope of P wave measurements. This technological progress has enabled researchers and clinicians to detect subtle changes in atrial electrophysiology that were previously unobservable.
In the context of cardiovascular pathologies, P wave analysis has proven particularly valuable. It has been extensively studied in conditions such as atrial fibrillation, hypertension, heart failure, and various structural heart diseases. The ability of P wave indices to reflect both electrical and structural remodeling of the atria makes them powerful tools for risk stratification and early detection of cardiovascular abnormalities.
Comparative studies of P wave indices across different cardiovascular pathologies have emerged as a critical area of research. These studies aim to identify specific P wave characteristics associated with particular diseases, potentially leading to more accurate diagnostic and prognostic tools. For instance, differences in P wave morphology and duration have been observed between patients with paroxysmal atrial fibrillation and those with persistent atrial fibrillation.
The clinical significance of P wave analysis extends beyond diagnosis. It has shown promise in predicting the onset of atrial fibrillation, assessing the risk of recurrence after cardioversion, and evaluating the effectiveness of various therapeutic interventions. This predictive capability makes P wave analysis an invaluable tool in personalized medicine approaches to cardiovascular care.
As research in this field progresses, there is a growing emphasis on standardizing P wave measurement techniques and establishing normative values across different populations. This standardization is crucial for ensuring the reliability and comparability of results across studies and clinical settings. Additionally, efforts are being made to integrate P wave analysis into automated ECG interpretation systems, potentially expanding its use in routine clinical practice.
Clinical Significance
P wave indices derived from electrocardiograms (ECGs) have emerged as valuable tools for assessing various cardiovascular pathologies. These indices, including P wave duration, amplitude, and morphology, provide crucial insights into atrial conduction and structural abnormalities. The clinical significance of comparative studies across different cardiovascular conditions lies in their potential to enhance diagnostic accuracy, risk stratification, and treatment planning.
In the realm of atrial fibrillation (AF), P wave indices have demonstrated remarkable utility. Prolonged P wave duration and increased P wave dispersion have been consistently associated with an elevated risk of AF development and recurrence. These markers reflect atrial conduction delays and heterogeneity, which are fundamental substrates for AF initiation and maintenance. By comparing P wave characteristics between AF patients and healthy controls, clinicians can identify individuals at higher risk for AF and implement preventive strategies more effectively.
Hypertension, a major risk factor for cardiovascular diseases, also manifests distinct P wave alterations. Comparative studies have revealed that hypertensive patients often exhibit increased P wave duration and amplitude compared to normotensive individuals. These changes are attributed to left atrial enlargement and increased atrial pressure, which are common consequences of chronic hypertension. The ability to detect these subtle ECG changes allows for early identification of hypertensive heart disease and prompt intervention to prevent further cardiac remodeling.
In the context of heart failure, P wave indices provide valuable prognostic information. Patients with heart failure often display prolonged P wave duration and altered P wave morphology, reflecting the complex atrial remodeling processes associated with the condition. Comparative analyses between heart failure patients with preserved and reduced ejection fraction have shown distinct P wave patterns, potentially aiding in differential diagnosis and tailored management strategies.
Coronary artery disease (CAD) is another area where P wave indices offer significant clinical value. Studies comparing CAD patients with healthy controls have demonstrated that P wave duration and dispersion are often increased in CAD, even in the absence of overt atrial enlargement. These findings suggest that P wave indices may serve as early markers of subclinical atrial dysfunction in CAD, potentially identifying patients who would benefit from more aggressive preventive measures.
The comparative approach extends to valvular heart diseases as well. Mitral valve disorders, particularly mitral stenosis, are associated with characteristic P wave changes. By comparing P wave indices across different valvular pathologies, clinicians can gain insights into the severity of atrial remodeling and the potential risk of complications such as atrial arrhythmias.
In conclusion, comparative studies of P wave indices across cardiovascular pathologies offer a wealth of clinically significant information. These studies enhance our understanding of disease-specific atrial remodeling processes, improve risk stratification, and guide personalized treatment approaches. As ECG technology continues to advance, the integration of P wave analysis into routine clinical practice holds promise for more precise and timely cardiovascular care.
In the realm of atrial fibrillation (AF), P wave indices have demonstrated remarkable utility. Prolonged P wave duration and increased P wave dispersion have been consistently associated with an elevated risk of AF development and recurrence. These markers reflect atrial conduction delays and heterogeneity, which are fundamental substrates for AF initiation and maintenance. By comparing P wave characteristics between AF patients and healthy controls, clinicians can identify individuals at higher risk for AF and implement preventive strategies more effectively.
Hypertension, a major risk factor for cardiovascular diseases, also manifests distinct P wave alterations. Comparative studies have revealed that hypertensive patients often exhibit increased P wave duration and amplitude compared to normotensive individuals. These changes are attributed to left atrial enlargement and increased atrial pressure, which are common consequences of chronic hypertension. The ability to detect these subtle ECG changes allows for early identification of hypertensive heart disease and prompt intervention to prevent further cardiac remodeling.
In the context of heart failure, P wave indices provide valuable prognostic information. Patients with heart failure often display prolonged P wave duration and altered P wave morphology, reflecting the complex atrial remodeling processes associated with the condition. Comparative analyses between heart failure patients with preserved and reduced ejection fraction have shown distinct P wave patterns, potentially aiding in differential diagnosis and tailored management strategies.
Coronary artery disease (CAD) is another area where P wave indices offer significant clinical value. Studies comparing CAD patients with healthy controls have demonstrated that P wave duration and dispersion are often increased in CAD, even in the absence of overt atrial enlargement. These findings suggest that P wave indices may serve as early markers of subclinical atrial dysfunction in CAD, potentially identifying patients who would benefit from more aggressive preventive measures.
The comparative approach extends to valvular heart diseases as well. Mitral valve disorders, particularly mitral stenosis, are associated with characteristic P wave changes. By comparing P wave indices across different valvular pathologies, clinicians can gain insights into the severity of atrial remodeling and the potential risk of complications such as atrial arrhythmias.
In conclusion, comparative studies of P wave indices across cardiovascular pathologies offer a wealth of clinically significant information. These studies enhance our understanding of disease-specific atrial remodeling processes, improve risk stratification, and guide personalized treatment approaches. As ECG technology continues to advance, the integration of P wave analysis into routine clinical practice holds promise for more precise and timely cardiovascular care.
Current Challenges
The comparative study of P wave indices across cardiovascular pathologies faces several significant challenges that hinder progress in this field. One of the primary obstacles is the lack of standardization in P wave measurement and analysis techniques. Different research groups and clinical settings often employ varying methodologies, making it difficult to compare results across studies and establish consistent diagnostic criteria.
Another major challenge is the inherent variability of P wave morphology among individuals, even in healthy populations. This natural variation complicates the establishment of clear-cut thresholds for distinguishing between normal and pathological P wave characteristics. Furthermore, the influence of factors such as age, gender, and ethnicity on P wave indices is not fully understood, adding another layer of complexity to comparative analyses.
The limited resolution and signal-to-noise ratio of standard 12-lead ECG recordings pose technical challenges in accurately measuring subtle changes in P wave morphology. This is particularly problematic when attempting to detect early-stage cardiovascular pathologies or differentiate between similar conditions based on P wave indices alone.
There is also a significant gap in our understanding of the precise electrophysiological mechanisms underlying changes in P wave indices across different cardiovascular pathologies. This knowledge gap hampers the development of more targeted and effective diagnostic approaches based on P wave analysis.
The dynamic nature of cardiovascular pathologies presents another challenge. P wave indices may change over time as a disease progresses or in response to treatment, necessitating longitudinal studies that are often resource-intensive and logistically complex to conduct.
Additionally, the integration of P wave analysis into existing clinical workflows and decision-making processes remains a challenge. Many healthcare providers lack the specialized training required to interpret subtle P wave changes, and there is a shortage of user-friendly tools for automated P wave analysis in clinical settings.
Lastly, the field faces challenges in validating the clinical utility and cost-effectiveness of P wave indices as diagnostic or prognostic markers across various cardiovascular pathologies. Large-scale, multicenter studies are needed to establish the added value of P wave analysis in improving patient outcomes and guiding treatment decisions, but such studies are often difficult to organize and fund.
Another major challenge is the inherent variability of P wave morphology among individuals, even in healthy populations. This natural variation complicates the establishment of clear-cut thresholds for distinguishing between normal and pathological P wave characteristics. Furthermore, the influence of factors such as age, gender, and ethnicity on P wave indices is not fully understood, adding another layer of complexity to comparative analyses.
The limited resolution and signal-to-noise ratio of standard 12-lead ECG recordings pose technical challenges in accurately measuring subtle changes in P wave morphology. This is particularly problematic when attempting to detect early-stage cardiovascular pathologies or differentiate between similar conditions based on P wave indices alone.
There is also a significant gap in our understanding of the precise electrophysiological mechanisms underlying changes in P wave indices across different cardiovascular pathologies. This knowledge gap hampers the development of more targeted and effective diagnostic approaches based on P wave analysis.
The dynamic nature of cardiovascular pathologies presents another challenge. P wave indices may change over time as a disease progresses or in response to treatment, necessitating longitudinal studies that are often resource-intensive and logistically complex to conduct.
Additionally, the integration of P wave analysis into existing clinical workflows and decision-making processes remains a challenge. Many healthcare providers lack the specialized training required to interpret subtle P wave changes, and there is a shortage of user-friendly tools for automated P wave analysis in clinical settings.
Lastly, the field faces challenges in validating the clinical utility and cost-effectiveness of P wave indices as diagnostic or prognostic markers across various cardiovascular pathologies. Large-scale, multicenter studies are needed to establish the added value of P wave analysis in improving patient outcomes and guiding treatment decisions, but such studies are often difficult to organize and fund.
P Wave Measurement Methods
01 P wave detection and analysis in ECG signals
Methods and systems for detecting and analyzing P waves in electrocardiogram (ECG) signals. This includes techniques for identifying P wave onset, offset, and peak, as well as measuring P wave duration and amplitude. These analyses can be used to assess atrial function and detect abnormalities in cardiac conduction.- P wave detection and analysis in ECG signals: Methods and systems for detecting and analyzing P waves in electrocardiogram (ECG) signals. This includes techniques for identifying P wave onset, offset, and peak, as well as measuring P wave duration and amplitude. These analyses can be used to assess atrial function and detect cardiac abnormalities.
- P wave indices for arrhythmia detection: Utilization of various P wave indices, such as P wave duration, amplitude, and morphology, to detect and classify different types of arrhythmias. These indices can be used in algorithms to differentiate between normal sinus rhythm and various atrial arrhythmias, including atrial fibrillation and atrial flutter.
- P wave analysis in implantable cardiac devices: Integration of P wave analysis algorithms in implantable cardiac devices such as pacemakers and implantable cardioverter-defibrillators. These devices use P wave indices to optimize pacing therapy, detect atrial arrhythmias, and provide early warning of potential cardiac events.
- Advanced signal processing for P wave extraction: Development of advanced signal processing techniques to improve the extraction and analysis of P waves from noisy ECG signals. This includes wavelet transforms, adaptive filtering, and machine learning algorithms to enhance P wave detection accuracy and reduce false positives in challenging recording conditions.
- P wave indices for risk stratification: Use of P wave indices for risk stratification in various cardiac conditions. This involves analyzing P wave characteristics to predict the likelihood of developing atrial fibrillation, assessing the risk of stroke in patients with certain cardiac abnormalities, and evaluating the prognosis of patients with heart failure.
02 P wave indices for arrhythmia detection
Utilization of P wave indices to detect and classify various types of cardiac arrhythmias. This involves analyzing P wave morphology, timing, and variability to identify conditions such as atrial fibrillation, atrial flutter, and other supraventricular tachycardias.Expand Specific Solutions03 P wave analysis in implantable cardiac devices
Implementation of P wave analysis algorithms in implantable cardiac devices such as pacemakers and defibrillators. These algorithms can be used for real-time monitoring of atrial activity, optimizing device settings, and guiding therapy delivery.Expand Specific Solutions04 Advanced signal processing techniques for P wave analysis
Application of advanced signal processing techniques, including wavelet transforms, machine learning algorithms, and time-frequency analysis, to improve the accuracy and reliability of P wave detection and characterization in noisy or complex ECG signals.Expand Specific Solutions05 P wave indices for predicting cardiovascular events
Use of P wave indices as predictors of future cardiovascular events or disease progression. This includes studying the relationship between P wave characteristics and the risk of developing conditions such as atrial fibrillation, stroke, or heart failure.Expand Specific Solutions
Key Research Groups
The comparative studies of P wave indices across cardiovascular pathologies are in a developing stage, with the market showing significant growth potential. The industry is transitioning from early research to more advanced clinical applications, driven by increasing demand for non-invasive cardiac diagnostics. Companies like Bardy Diagnostics, Edwards Lifesciences, and Medtronic are leading the way in developing innovative ECG monitoring technologies. The market size is expanding rapidly, fueled by the rising prevalence of cardiovascular diseases globally. While the technology is maturing, there is still room for improvement in accuracy and specificity of P wave analysis across different pathologies, presenting opportunities for further research and development by both established players and emerging startups in the field.
Edwards Lifesciences Corp.
Technical Solution: Edwards Lifesciences has focused on integrating P wave analysis into their hemodynamic monitoring systems. Their technology combines P wave measurements with other cardiovascular parameters to provide a more comprehensive assessment of cardiac function[6]. They have developed algorithms that analyze P wave morphology changes in relation to variations in stroke volume and cardiac output. This approach allows for comparative studies of how P wave indices are affected by different cardiovascular pathologies and hemodynamic states[7]. Edwards' systems can track these relationships over time, potentially identifying early signs of deterioration in cardiac function.
Strengths: Integration of P wave analysis with hemodynamic monitoring; ability to correlate P wave changes with other cardiovascular parameters. Weaknesses: May be less sensitive to subtle P wave changes that are not associated with immediate hemodynamic effects.
Biosense Webster (Israel) Ltd.
Technical Solution: Biosense Webster has developed the CARTO 3 System, which includes advanced P wave mapping capabilities. Their technology uses a combination of contact and non-contact mapping to create high-resolution 3D models of atrial activation[8]. The system can analyze P wave propagation patterns and identify areas of conduction block or slow conduction. Biosense Webster's approach allows for detailed comparative studies of P wave characteristics across different atrial pathologies, including atrial fibrillation, atrial flutter, and focal atrial tachycardias[9]. The CARTO 3 System also incorporates machine learning algorithms to classify P wave patterns and assist in diagnosis.
Strengths: Combination of contact and non-contact mapping for comprehensive P wave analysis; integration with 3D electroanatomical mapping. Weaknesses: Primarily designed for use in electrophysiology labs; may have limited applicability for long-term monitoring or outpatient settings.
Innovative P Wave Metrics
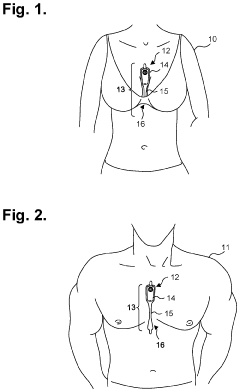
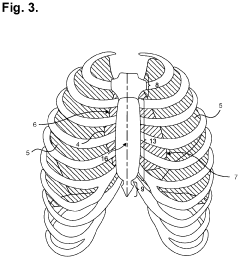
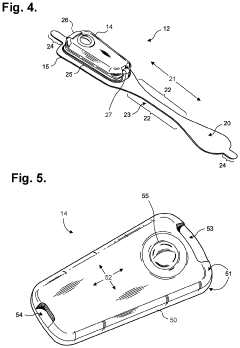
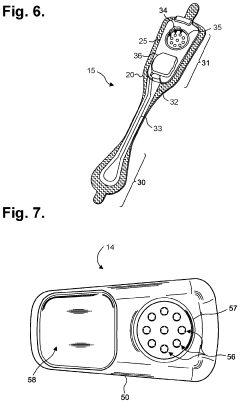
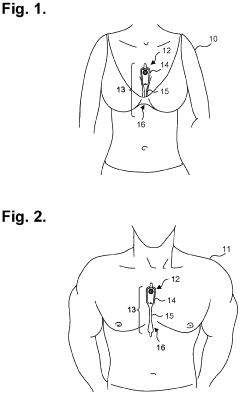
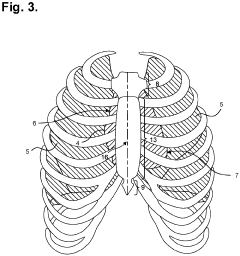
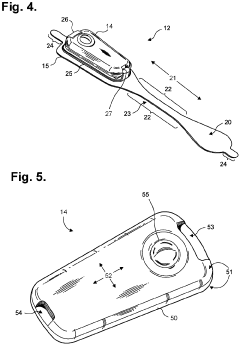
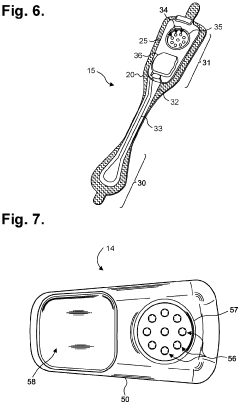
Moisture-resistant electrocardiography monitor
PatentActiveUS20230301576A1
Innovation
- A lightweight, wearable electrocardiography monitor with a flexible extended wear electrode patch and a reusable recorder that can be easily positioned on the sternal midline, optimized for sensing cardiac electrical potentials, including P-waves, and designed for extended wear with patient-friendly replacement and moisture resistance.
Electrocardiography monitor configured for self-optimizing ECG data compression
PatentActiveEP3847966A1
Innovation
- A lightweight, wearable electrocardiography monitor with a flexible extended wear electrode patch and a reusable monitor recorder that optimizes P-wave sensing through axial placement on the sternal midline, features automatic self-optimizing compression algorithms, and allows patient-friendly replacement and use, enhancing comfort and monitoring duration.
Standardization Efforts
Standardization efforts in P wave indices analysis across cardiovascular pathologies have become increasingly important in recent years. These efforts aim to establish consistent methodologies and criteria for measuring and interpreting P wave characteristics, ensuring comparability and reproducibility of results across different studies and clinical settings.
One of the primary focuses of standardization has been the development of uniform definitions for P wave morphology and duration. Consensus guidelines have been proposed by international cardiology organizations to define specific P wave indices, such as P wave duration, amplitude, and area. These standardized definitions help researchers and clinicians to use consistent terminology and measurement techniques, facilitating more accurate comparisons between studies.
Efforts have also been made to standardize the technical aspects of P wave analysis. This includes recommendations for ECG recording techniques, such as lead placement, sampling rate, and filtering methods. Standardized protocols for signal processing and noise reduction have been developed to ensure that P wave measurements are not influenced by technical variations between different ECG systems or recording environments.
Another crucial aspect of standardization is the establishment of normative values for P wave indices across different populations. Large-scale studies have been conducted to determine reference ranges for various P wave parameters, taking into account factors such as age, gender, and ethnicity. These normative values provide a baseline for identifying abnormal P wave characteristics in different cardiovascular pathologies.
Standardization efforts have also extended to the development of automated algorithms for P wave analysis. These algorithms aim to provide consistent and objective measurements of P wave indices, reducing inter-observer variability and improving the efficiency of large-scale studies. Efforts are ongoing to validate and refine these algorithms across different patient populations and cardiovascular conditions.
International collaborations and consensus meetings have played a crucial role in driving standardization efforts. These initiatives bring together experts from various fields, including cardiology, electrophysiology, and biomedical engineering, to develop and refine guidelines for P wave analysis. Regular updates to these guidelines ensure that standardization efforts keep pace with advances in technology and clinical knowledge.
Despite significant progress, challenges remain in achieving full standardization of P wave indices analysis. Variations in ECG equipment, recording techniques, and analysis software still exist, potentially affecting the comparability of results between different centers. Ongoing efforts are focused on addressing these challenges and further refining standardization protocols to enhance the clinical utility and research value of P wave indices across cardiovascular pathologies.
One of the primary focuses of standardization has been the development of uniform definitions for P wave morphology and duration. Consensus guidelines have been proposed by international cardiology organizations to define specific P wave indices, such as P wave duration, amplitude, and area. These standardized definitions help researchers and clinicians to use consistent terminology and measurement techniques, facilitating more accurate comparisons between studies.
Efforts have also been made to standardize the technical aspects of P wave analysis. This includes recommendations for ECG recording techniques, such as lead placement, sampling rate, and filtering methods. Standardized protocols for signal processing and noise reduction have been developed to ensure that P wave measurements are not influenced by technical variations between different ECG systems or recording environments.
Another crucial aspect of standardization is the establishment of normative values for P wave indices across different populations. Large-scale studies have been conducted to determine reference ranges for various P wave parameters, taking into account factors such as age, gender, and ethnicity. These normative values provide a baseline for identifying abnormal P wave characteristics in different cardiovascular pathologies.
Standardization efforts have also extended to the development of automated algorithms for P wave analysis. These algorithms aim to provide consistent and objective measurements of P wave indices, reducing inter-observer variability and improving the efficiency of large-scale studies. Efforts are ongoing to validate and refine these algorithms across different patient populations and cardiovascular conditions.
International collaborations and consensus meetings have played a crucial role in driving standardization efforts. These initiatives bring together experts from various fields, including cardiology, electrophysiology, and biomedical engineering, to develop and refine guidelines for P wave analysis. Regular updates to these guidelines ensure that standardization efforts keep pace with advances in technology and clinical knowledge.
Despite significant progress, challenges remain in achieving full standardization of P wave indices analysis. Variations in ECG equipment, recording techniques, and analysis software still exist, potentially affecting the comparability of results between different centers. Ongoing efforts are focused on addressing these challenges and further refining standardization protocols to enhance the clinical utility and research value of P wave indices across cardiovascular pathologies.
AI in P Wave Analysis
Artificial Intelligence (AI) has emerged as a powerful tool in the analysis of P waves, offering new possibilities for enhancing the accuracy and efficiency of cardiovascular diagnostics. The integration of AI techniques in P wave analysis has revolutionized the way clinicians interpret electrocardiogram (ECG) data, particularly in the context of comparative studies across various cardiovascular pathologies.
Machine learning algorithms, particularly deep learning models, have demonstrated remarkable capabilities in detecting subtle patterns and anomalies in P wave morphology. These AI-driven approaches can process vast amounts of ECG data, identifying features that may be imperceptible to the human eye. This has led to improved sensitivity and specificity in diagnosing conditions such as atrial fibrillation, atrial flutter, and other cardiac arrhythmias.
One of the key advantages of AI in P wave analysis is its ability to perform automated measurements of P wave indices with high precision and consistency. This includes parameters such as P wave duration, amplitude, and dispersion, which are crucial for assessing atrial conduction abnormalities. By standardizing these measurements across large datasets, AI facilitates more robust comparative studies between different cardiovascular pathologies.
Furthermore, AI algorithms have shown promise in predicting the onset of atrial fibrillation and other cardiac events based on P wave characteristics. These predictive models analyze temporal changes in P wave morphology, potentially enabling early intervention and personalized treatment strategies. This proactive approach to cardiac care represents a significant advancement in preventive cardiology.
The application of AI in P wave analysis extends beyond traditional ECG interpretation. Advanced signal processing techniques, combined with machine learning, have enabled the extraction of additional information from P waves, such as estimating left atrial pressure and identifying structural changes in the atria. These insights provide clinicians with a more comprehensive understanding of cardiac function and pathology.
As AI continues to evolve, its role in P wave analysis is expected to expand further. Ongoing research focuses on developing more sophisticated algorithms capable of integrating multiple data sources, including genetic information and imaging studies, to provide a holistic view of cardiovascular health. This multidimensional approach promises to enhance the diagnostic accuracy and prognostic value of P wave analysis across a wide spectrum of cardiovascular diseases.
Machine learning algorithms, particularly deep learning models, have demonstrated remarkable capabilities in detecting subtle patterns and anomalies in P wave morphology. These AI-driven approaches can process vast amounts of ECG data, identifying features that may be imperceptible to the human eye. This has led to improved sensitivity and specificity in diagnosing conditions such as atrial fibrillation, atrial flutter, and other cardiac arrhythmias.
One of the key advantages of AI in P wave analysis is its ability to perform automated measurements of P wave indices with high precision and consistency. This includes parameters such as P wave duration, amplitude, and dispersion, which are crucial for assessing atrial conduction abnormalities. By standardizing these measurements across large datasets, AI facilitates more robust comparative studies between different cardiovascular pathologies.
Furthermore, AI algorithms have shown promise in predicting the onset of atrial fibrillation and other cardiac events based on P wave characteristics. These predictive models analyze temporal changes in P wave morphology, potentially enabling early intervention and personalized treatment strategies. This proactive approach to cardiac care represents a significant advancement in preventive cardiology.
The application of AI in P wave analysis extends beyond traditional ECG interpretation. Advanced signal processing techniques, combined with machine learning, have enabled the extraction of additional information from P waves, such as estimating left atrial pressure and identifying structural changes in the atria. These insights provide clinicians with a more comprehensive understanding of cardiac function and pathology.
As AI continues to evolve, its role in P wave analysis is expected to expand further. Ongoing research focuses on developing more sophisticated algorithms capable of integrating multiple data sources, including genetic information and imaging studies, to provide a holistic view of cardiovascular health. This multidimensional approach promises to enhance the diagnostic accuracy and prognostic value of P wave analysis across a wide spectrum of cardiovascular diseases.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!