Long-term P wave changes post-cardiac rehabilitation
AUG 19, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
P Wave Evolution Goals
The evolution of P wave characteristics following cardiac rehabilitation represents a critical area of focus in cardiovascular research. The primary goal is to comprehensively understand and quantify the long-term changes in P wave morphology, duration, and amplitude as indicators of atrial remodeling and improved cardiac function post-rehabilitation.
One key objective is to establish standardized methods for P wave analysis that can be consistently applied across different patient populations and rehabilitation programs. This includes developing advanced signal processing techniques and machine learning algorithms to extract and interpret P wave features from electrocardiogram (ECG) data with high accuracy and reliability.
Another important aim is to correlate P wave changes with specific physiological improvements resulting from cardiac rehabilitation. This involves investigating the relationship between P wave alterations and factors such as enhanced atrial conduction, reduced atrial fibrosis, and improved left atrial function. By establishing these correlations, clinicians can gain valuable insights into the effectiveness of rehabilitation protocols and their impact on atrial electrophysiology.
Longitudinal studies form a crucial component of P wave evolution research. The goal is to track P wave changes over extended periods, typically ranging from months to years post-rehabilitation. This long-term monitoring allows for the identification of sustained improvements in atrial function and helps distinguish between temporary adaptations and lasting structural changes in the heart.
Personalized prediction models represent another significant objective in this field. By integrating P wave data with other clinical parameters, researchers aim to develop algorithms that can forecast individual patient outcomes and tailor rehabilitation strategies accordingly. These models could potentially identify patients at higher risk of atrial fibrillation or other arrhythmias, enabling early intervention and personalized care.
Lastly, there is a growing emphasis on translating P wave evolution insights into practical clinical applications. This includes developing user-friendly tools for ECG interpretation, creating guidelines for incorporating P wave analysis into routine cardiac assessments, and establishing thresholds for P wave parameters that indicate successful rehabilitation outcomes or the need for additional interventions.
One key objective is to establish standardized methods for P wave analysis that can be consistently applied across different patient populations and rehabilitation programs. This includes developing advanced signal processing techniques and machine learning algorithms to extract and interpret P wave features from electrocardiogram (ECG) data with high accuracy and reliability.
Another important aim is to correlate P wave changes with specific physiological improvements resulting from cardiac rehabilitation. This involves investigating the relationship between P wave alterations and factors such as enhanced atrial conduction, reduced atrial fibrosis, and improved left atrial function. By establishing these correlations, clinicians can gain valuable insights into the effectiveness of rehabilitation protocols and their impact on atrial electrophysiology.
Longitudinal studies form a crucial component of P wave evolution research. The goal is to track P wave changes over extended periods, typically ranging from months to years post-rehabilitation. This long-term monitoring allows for the identification of sustained improvements in atrial function and helps distinguish between temporary adaptations and lasting structural changes in the heart.
Personalized prediction models represent another significant objective in this field. By integrating P wave data with other clinical parameters, researchers aim to develop algorithms that can forecast individual patient outcomes and tailor rehabilitation strategies accordingly. These models could potentially identify patients at higher risk of atrial fibrillation or other arrhythmias, enabling early intervention and personalized care.
Lastly, there is a growing emphasis on translating P wave evolution insights into practical clinical applications. This includes developing user-friendly tools for ECG interpretation, creating guidelines for incorporating P wave analysis into routine cardiac assessments, and establishing thresholds for P wave parameters that indicate successful rehabilitation outcomes or the need for additional interventions.
Cardiac Rehab Impact
Cardiac rehabilitation has emerged as a crucial intervention in the management of cardiovascular diseases, demonstrating significant long-term impacts on patients' cardiac health and overall well-being. The effects of cardiac rehabilitation on P wave changes, a key indicator of atrial electrical activity, have garnered increasing attention in recent years.
Studies have shown that cardiac rehabilitation programs can lead to substantial improvements in P wave characteristics over extended periods. These changes are often associated with reduced risk of atrial fibrillation and other arrhythmias, contributing to better long-term cardiac outcomes. The duration and intensity of rehabilitation programs appear to play a critical role in the extent of P wave modifications observed.
One of the primary mechanisms through which cardiac rehabilitation influences P wave morphology is through its effects on atrial remodeling. Regular exercise and lifestyle modifications, core components of rehabilitation programs, have been found to promote favorable structural and electrical changes in the atrial myocardium. This remodeling process can result in more organized atrial depolarization, reflected in alterations of P wave duration, amplitude, and dispersion.
Furthermore, cardiac rehabilitation has been shown to improve autonomic balance, a factor closely linked to P wave characteristics. Enhanced vagal tone and reduced sympathetic activity, often observed following rehabilitation, can lead to more stable atrial electrical properties. This autonomic modulation may contribute to the long-term stability of P wave parameters and potentially reduce the risk of atrial arrhythmogenesis.
The impact of cardiac rehabilitation on P wave changes appears to extend beyond the immediate post-rehabilitation period. Long-term follow-up studies have reported sustained improvements in P wave indices for several years after completion of structured rehabilitation programs. This persistence of effects underscores the potential of cardiac rehabilitation as a strategy for long-term arrhythmia prevention and management.
It is important to note that the magnitude of P wave changes can vary among individuals, influenced by factors such as age, underlying cardiac pathology, and adherence to rehabilitation protocols. Personalized approaches to cardiac rehabilitation, tailored to individual patient characteristics and risk profiles, may optimize the long-term benefits on atrial electrical function.
In conclusion, the long-term impact of cardiac rehabilitation on P wave changes represents a promising area of cardiovascular care. The observed improvements in atrial electrical properties not only reflect enhanced cardiac health but also offer potential for reducing the burden of atrial arrhythmias in the long run. Further research is warranted to elucidate the precise mechanisms underlying these changes and to develop targeted rehabilitation strategies for maximizing long-term P wave improvements.
Studies have shown that cardiac rehabilitation programs can lead to substantial improvements in P wave characteristics over extended periods. These changes are often associated with reduced risk of atrial fibrillation and other arrhythmias, contributing to better long-term cardiac outcomes. The duration and intensity of rehabilitation programs appear to play a critical role in the extent of P wave modifications observed.
One of the primary mechanisms through which cardiac rehabilitation influences P wave morphology is through its effects on atrial remodeling. Regular exercise and lifestyle modifications, core components of rehabilitation programs, have been found to promote favorable structural and electrical changes in the atrial myocardium. This remodeling process can result in more organized atrial depolarization, reflected in alterations of P wave duration, amplitude, and dispersion.
Furthermore, cardiac rehabilitation has been shown to improve autonomic balance, a factor closely linked to P wave characteristics. Enhanced vagal tone and reduced sympathetic activity, often observed following rehabilitation, can lead to more stable atrial electrical properties. This autonomic modulation may contribute to the long-term stability of P wave parameters and potentially reduce the risk of atrial arrhythmogenesis.
The impact of cardiac rehabilitation on P wave changes appears to extend beyond the immediate post-rehabilitation period. Long-term follow-up studies have reported sustained improvements in P wave indices for several years after completion of structured rehabilitation programs. This persistence of effects underscores the potential of cardiac rehabilitation as a strategy for long-term arrhythmia prevention and management.
It is important to note that the magnitude of P wave changes can vary among individuals, influenced by factors such as age, underlying cardiac pathology, and adherence to rehabilitation protocols. Personalized approaches to cardiac rehabilitation, tailored to individual patient characteristics and risk profiles, may optimize the long-term benefits on atrial electrical function.
In conclusion, the long-term impact of cardiac rehabilitation on P wave changes represents a promising area of cardiovascular care. The observed improvements in atrial electrical properties not only reflect enhanced cardiac health but also offer potential for reducing the burden of atrial arrhythmias in the long run. Further research is warranted to elucidate the precise mechanisms underlying these changes and to develop targeted rehabilitation strategies for maximizing long-term P wave improvements.
P Wave Analysis Challenges
P wave analysis in electrocardiograms (ECGs) presents several significant challenges that hinder accurate interpretation and long-term monitoring of cardiac rehabilitation outcomes. One of the primary difficulties lies in the small amplitude and subtle morphology changes of P waves, which can be easily obscured by noise or artifacts in the ECG signal. This makes it particularly challenging to detect and measure P wave changes consistently over extended periods.
The variability in P wave morphology among different individuals further complicates the analysis. Factors such as age, gender, body composition, and underlying cardiac conditions can all influence the shape and duration of P waves. This heterogeneity makes it difficult to establish standardized criteria for assessing P wave changes across diverse patient populations undergoing cardiac rehabilitation.
Another significant challenge is the lack of robust automated algorithms for P wave detection and delineation. While numerous methods have been proposed, many still struggle with accuracy and reliability, especially in the presence of atrial fibrillation or other arrhythmias. This limitation often necessitates manual review and annotation by expert cardiologists, which is time-consuming and subject to inter-observer variability.
The dynamic nature of cardiac rehabilitation itself poses additional challenges for P wave analysis. As patients progress through their rehabilitation programs, physiological changes in the heart can lead to alterations in P wave characteristics. Distinguishing between normal adaptive changes and potentially pathological developments requires sophisticated analytical approaches and longitudinal data interpretation.
Furthermore, the integration of P wave analysis into existing cardiac monitoring systems and electronic health records presents technical and logistical hurdles. Ensuring interoperability between different ECG acquisition devices and analysis software, while maintaining data integrity and patient privacy, remains a complex issue in clinical settings.
The interpretation of P wave changes in the context of overall cardiac health and rehabilitation progress is another area of difficulty. Correlating subtle P wave alterations with functional improvements or potential complications requires a comprehensive understanding of cardiac electrophysiology and the rehabilitation process. This multifaceted analysis often necessitates the collaboration of cardiologists, rehabilitation specialists, and data scientists.
Lastly, the long-term nature of cardiac rehabilitation introduces challenges in maintaining consistent ECG recording quality over time. Factors such as electrode placement, patient positioning, and environmental conditions can all affect P wave measurements, potentially confounding the analysis of genuine physiological changes. Developing standardized protocols for long-term ECG monitoring in rehabilitation settings is crucial for obtaining reliable and comparable P wave data across multiple time points.
The variability in P wave morphology among different individuals further complicates the analysis. Factors such as age, gender, body composition, and underlying cardiac conditions can all influence the shape and duration of P waves. This heterogeneity makes it difficult to establish standardized criteria for assessing P wave changes across diverse patient populations undergoing cardiac rehabilitation.
Another significant challenge is the lack of robust automated algorithms for P wave detection and delineation. While numerous methods have been proposed, many still struggle with accuracy and reliability, especially in the presence of atrial fibrillation or other arrhythmias. This limitation often necessitates manual review and annotation by expert cardiologists, which is time-consuming and subject to inter-observer variability.
The dynamic nature of cardiac rehabilitation itself poses additional challenges for P wave analysis. As patients progress through their rehabilitation programs, physiological changes in the heart can lead to alterations in P wave characteristics. Distinguishing between normal adaptive changes and potentially pathological developments requires sophisticated analytical approaches and longitudinal data interpretation.
Furthermore, the integration of P wave analysis into existing cardiac monitoring systems and electronic health records presents technical and logistical hurdles. Ensuring interoperability between different ECG acquisition devices and analysis software, while maintaining data integrity and patient privacy, remains a complex issue in clinical settings.
The interpretation of P wave changes in the context of overall cardiac health and rehabilitation progress is another area of difficulty. Correlating subtle P wave alterations with functional improvements or potential complications requires a comprehensive understanding of cardiac electrophysiology and the rehabilitation process. This multifaceted analysis often necessitates the collaboration of cardiologists, rehabilitation specialists, and data scientists.
Lastly, the long-term nature of cardiac rehabilitation introduces challenges in maintaining consistent ECG recording quality over time. Factors such as electrode placement, patient positioning, and environmental conditions can all affect P wave measurements, potentially confounding the analysis of genuine physiological changes. Developing standardized protocols for long-term ECG monitoring in rehabilitation settings is crucial for obtaining reliable and comparable P wave data across multiple time points.
P Wave Monitoring Methods
01 Detection and analysis of P wave changes in ECG
Methods and systems for detecting and analyzing changes in P waves of electrocardiogram (ECG) signals. These techniques involve signal processing algorithms to identify variations in P wave morphology, amplitude, and duration, which can be indicative of various cardiac conditions.- Detection and analysis of P wave changes: Methods and systems for detecting and analyzing changes in P waves, which are important indicators of atrial activity in the heart. These techniques involve signal processing, pattern recognition, and machine learning algorithms to identify subtle variations in P wave morphology, duration, and amplitude.
- P wave monitoring in cardiac devices: Integration of P wave monitoring capabilities in implantable cardiac devices and external monitoring systems. These devices can continuously track P wave changes to detect early signs of atrial arrhythmias, heart failure progression, or other cardiac abnormalities.
- P wave signal enhancement and filtering: Techniques for improving the quality of P wave signals through advanced filtering and signal enhancement methods. These approaches aim to reduce noise, eliminate artifacts, and isolate P waves from other cardiac signals for more accurate analysis.
- P wave-based diagnostic algorithms: Development of diagnostic algorithms that utilize P wave changes as key inputs for detecting and predicting various cardiac conditions. These algorithms may incorporate multiple parameters derived from P wave analysis to improve diagnostic accuracy and provide early warning of potential cardiac events.
- P wave analysis in wearable devices: Integration of P wave monitoring and analysis capabilities in wearable health devices and smartwatches. These consumer-oriented devices can provide continuous P wave monitoring and alert users to significant changes that may require medical attention.
02 P wave monitoring in cardiac devices
Implantable cardiac devices and external monitoring systems that specifically focus on P wave monitoring. These devices can track P wave changes over time, providing valuable data for diagnosing and managing atrial arrhythmias and other heart conditions.Expand Specific Solutions03 P wave analysis for atrial fibrillation detection
Techniques for using P wave analysis to detect and predict atrial fibrillation. These methods involve examining P wave characteristics and patterns to identify early signs of atrial fibrillation or assess the risk of its occurrence.Expand Specific Solutions04 P wave signal processing and enhancement
Advanced signal processing techniques for enhancing P wave detection and analysis in noisy ECG signals. These methods aim to improve the accuracy of P wave measurements and interpretations in various clinical and research settings.Expand Specific Solutions05 P wave changes in relation to other ECG components
Studies and methods focusing on the relationship between P wave changes and other ECG components, such as QRS complexes and T waves. This approach provides a more comprehensive understanding of cardiac electrical activity and its implications for heart health.Expand Specific Solutions
Cardiology Research Leaders
The competitive landscape for long-term P wave changes post-cardiac rehabilitation is in a developing stage, with a growing market driven by increasing cardiovascular disease prevalence and aging populations. The technology is moderately mature, with established players like Medtronic and Boston Scientific (via Cardiac Pacemakers, Inc.) leading in cardiac monitoring and pacing devices. Emerging companies such as Bardy Diagnostics and Stealth BioTherapeutics are focusing on innovative ECG monitoring and mitochondrial therapies, respectively. Academic institutions like MIT and Vanderbilt University contribute to research advancements. The market is characterized by a mix of large medical device manufacturers and specialized biotechnology firms, indicating a competitive and evolving landscape.
Medtronic, Inc.
Technical Solution: Medtronic has developed advanced cardiac monitoring systems that can detect long-term P wave changes post-cardiac rehabilitation. Their technology utilizes implantable loop recorders (ILRs) with enhanced P wave detection algorithms[1]. These devices can continuously monitor cardiac rhythms for up to three years, allowing for the detection of subtle P wave changes over extended periods. The company has also integrated machine learning algorithms into their cardiac monitoring systems to improve the accuracy of P wave analysis and reduce false positives[2]. Additionally, Medtronic has developed cloud-based data analytics platforms that enable healthcare providers to remotely monitor patients' P wave changes and adjust rehabilitation programs accordingly[3].
Strengths: Long-term continuous monitoring capability, advanced algorithms for P wave detection, and remote monitoring features. Weaknesses: Invasive nature of implantable devices and potential for data overload for healthcare providers.
Massachusetts Institute of Technology
Technical Solution: MIT researchers have developed a novel approach to analyzing long-term P wave changes using advanced signal processing techniques and machine learning algorithms. Their method involves the use of high-resolution ECG recordings combined with sophisticated feature extraction algorithms to identify subtle changes in P wave morphology over time[6]. The team has also developed a deep learning model that can predict the likelihood of atrial fibrillation based on long-term P wave changes observed during cardiac rehabilitation[7]. Additionally, MIT has collaborated with clinical partners to validate their technology in real-world settings, demonstrating improved sensitivity and specificity in detecting clinically significant P wave changes compared to traditional methods[8].
Strengths: Cutting-edge machine learning algorithms, high-resolution signal processing, and strong clinical validation. Weaknesses: May require specialized equipment and expertise to implement in clinical settings.
P Wave Morphology Insights
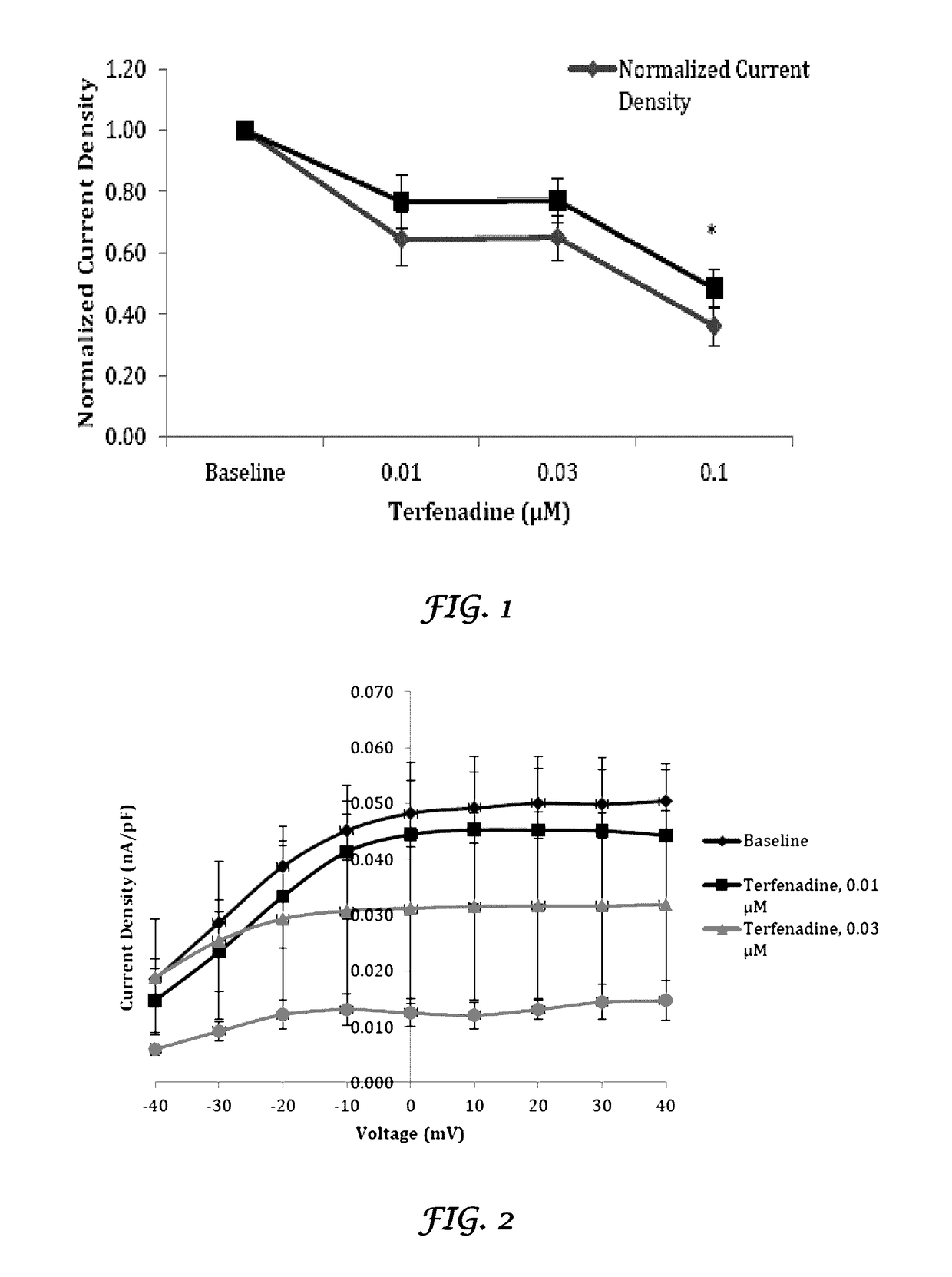
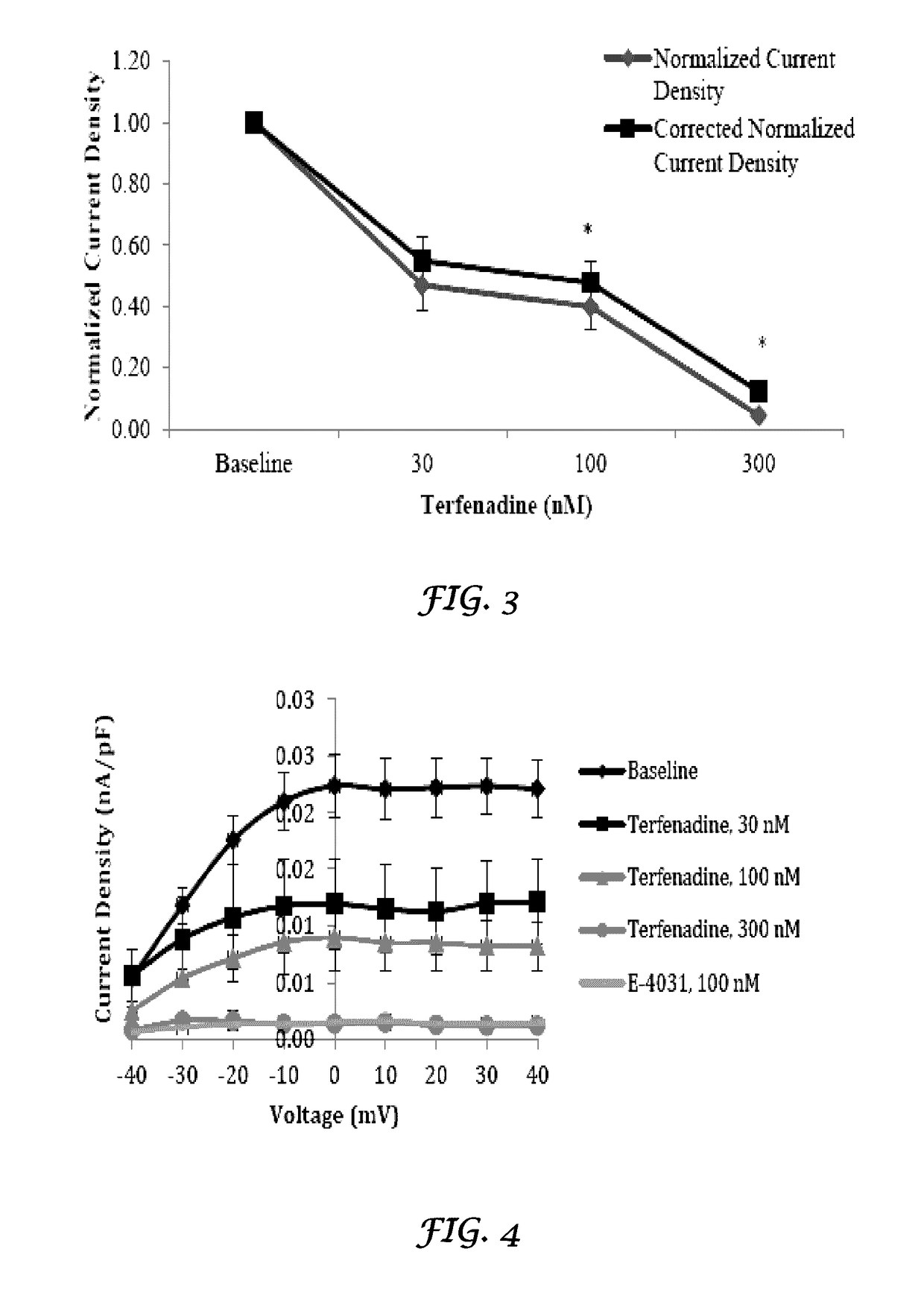
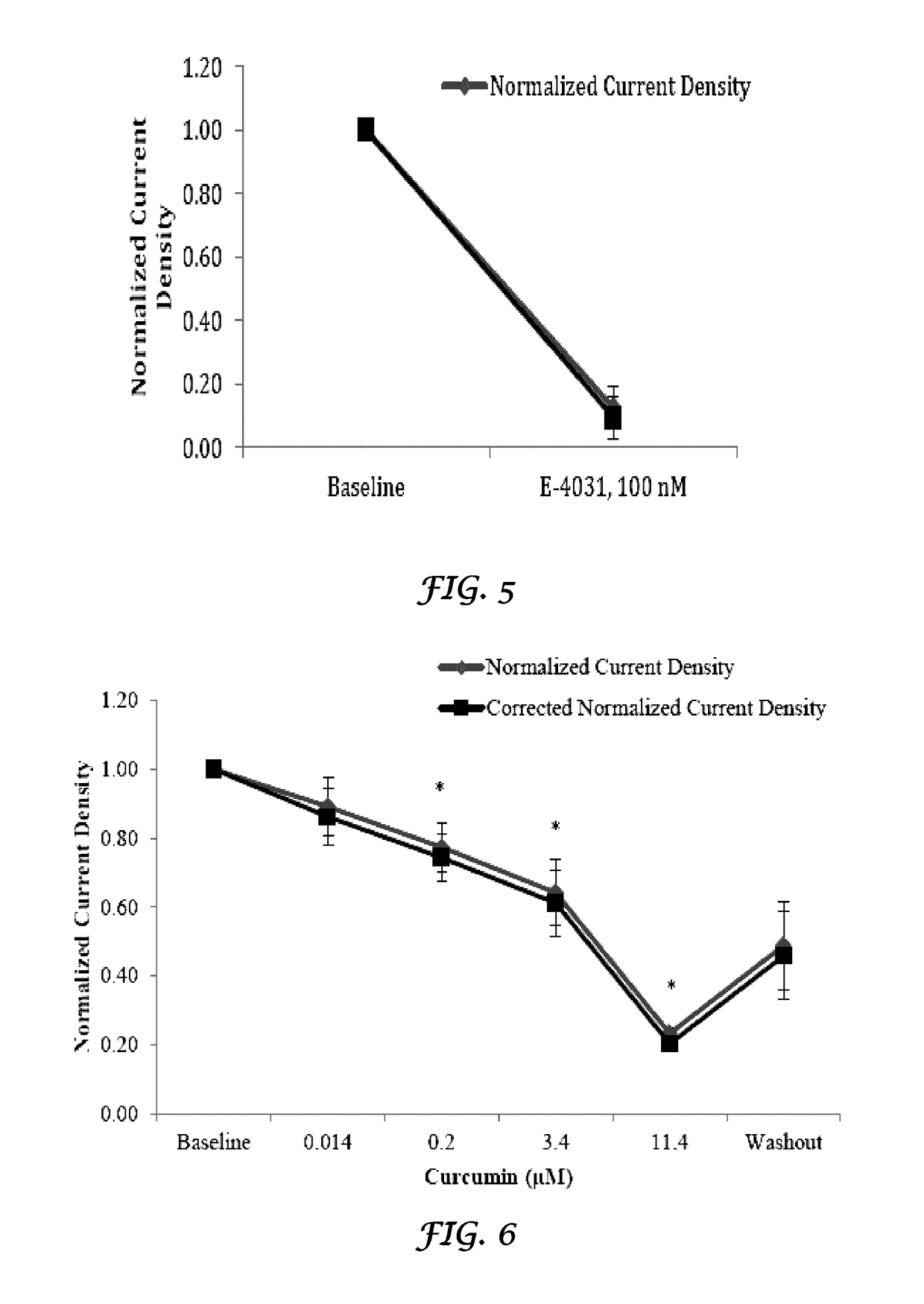
Liposomal mitigation of drug-induced inhibition of the cardiac IKR channel
PatentWO2015095576A1
Innovation
- Administering these drugs in conjunction with liposomes, either encapsulated or mixed with empty liposomes, to reduce their inhibitory effects on the IKr channel, thereby decreasing cardiac liability.
Liposomal mitigation of drug-induced inhibition of the cardiac ikr channel
PatentActiveUS20170119802A1
Innovation
- Administering these drugs in conjunction with liposomes, which can encapsulate or mix with them, to reduce their inhibitory effects on the IKr channel, thereby decreasing cardiac liability.
Rehab Protocol Optimization
Optimizing cardiac rehabilitation protocols is crucial for maximizing the long-term benefits of P wave changes in patients post-rehabilitation. A comprehensive approach to protocol optimization involves several key components that address both the physiological and practical aspects of rehabilitation.
One primary focus is on tailoring exercise regimens to individual patient needs. This personalization takes into account factors such as age, pre-existing conditions, and the severity of cardiac issues. By customizing the intensity, duration, and type of exercises, rehabilitation programs can more effectively target specific P wave abnormalities and promote sustained improvements.
Incorporating advanced monitoring technologies is another vital aspect of protocol optimization. Continuous electrocardiogram (ECG) monitoring during rehabilitation sessions allows for real-time assessment of P wave changes. This data can be used to adjust exercise parameters on the fly, ensuring that patients are working within safe and effective ranges.
Timing and frequency of rehabilitation sessions play a significant role in optimizing outcomes. Research suggests that a combination of supervised in-clinic sessions and home-based exercises may yield the best results for long-term P wave improvements. Establishing a balanced schedule that maintains patient engagement while providing adequate recovery time is essential.
Integrating cardiovascular and respiratory exercises with specific activities aimed at improving atrial function can enhance the overall effectiveness of rehabilitation protocols. Techniques such as breathing exercises, yoga, and tai chi have shown promise in complementing traditional cardiac rehabilitation methods and potentially influencing P wave morphology.
Nutritional guidance is an often-overlooked component of cardiac rehabilitation that can significantly impact long-term outcomes. Developing protocols that include personalized dietary recommendations, with a focus on heart-healthy foods and appropriate supplementation, can support sustained improvements in cardiac function and P wave characteristics.
Patient education and psychological support are critical elements in optimizing rehabilitation protocols. Ensuring that patients understand the importance of adherence to their rehabilitation program and providing strategies for maintaining motivation can lead to better long-term outcomes. Incorporating stress management techniques and cognitive-behavioral interventions can further enhance the effectiveness of rehabilitation efforts.
Regular assessment and adjustment of rehabilitation protocols based on patient progress and the latest research findings are necessary for continuous improvement. Implementing a system for periodic review of P wave changes and other cardiac parameters allows for timely modifications to the rehabilitation approach, ensuring that patients continue to make progress throughout their recovery journey.
One primary focus is on tailoring exercise regimens to individual patient needs. This personalization takes into account factors such as age, pre-existing conditions, and the severity of cardiac issues. By customizing the intensity, duration, and type of exercises, rehabilitation programs can more effectively target specific P wave abnormalities and promote sustained improvements.
Incorporating advanced monitoring technologies is another vital aspect of protocol optimization. Continuous electrocardiogram (ECG) monitoring during rehabilitation sessions allows for real-time assessment of P wave changes. This data can be used to adjust exercise parameters on the fly, ensuring that patients are working within safe and effective ranges.
Timing and frequency of rehabilitation sessions play a significant role in optimizing outcomes. Research suggests that a combination of supervised in-clinic sessions and home-based exercises may yield the best results for long-term P wave improvements. Establishing a balanced schedule that maintains patient engagement while providing adequate recovery time is essential.
Integrating cardiovascular and respiratory exercises with specific activities aimed at improving atrial function can enhance the overall effectiveness of rehabilitation protocols. Techniques such as breathing exercises, yoga, and tai chi have shown promise in complementing traditional cardiac rehabilitation methods and potentially influencing P wave morphology.
Nutritional guidance is an often-overlooked component of cardiac rehabilitation that can significantly impact long-term outcomes. Developing protocols that include personalized dietary recommendations, with a focus on heart-healthy foods and appropriate supplementation, can support sustained improvements in cardiac function and P wave characteristics.
Patient education and psychological support are critical elements in optimizing rehabilitation protocols. Ensuring that patients understand the importance of adherence to their rehabilitation program and providing strategies for maintaining motivation can lead to better long-term outcomes. Incorporating stress management techniques and cognitive-behavioral interventions can further enhance the effectiveness of rehabilitation efforts.
Regular assessment and adjustment of rehabilitation protocols based on patient progress and the latest research findings are necessary for continuous improvement. Implementing a system for periodic review of P wave changes and other cardiac parameters allows for timely modifications to the rehabilitation approach, ensuring that patients continue to make progress throughout their recovery journey.
Patient Data Privacy Issues
Patient data privacy is a critical concern in the context of long-term P wave changes post-cardiac rehabilitation. As healthcare providers collect and analyze sensitive cardiac data over extended periods, robust privacy measures must be implemented to protect patients' personal information and medical records.
One of the primary challenges is ensuring secure data storage and transmission. Healthcare institutions must employ state-of-the-art encryption technologies and secure protocols to safeguard patient data from unauthorized access or breaches. This includes implementing end-to-end encryption for data in transit and at rest, as well as utilizing secure cloud storage solutions with stringent access controls.
Another crucial aspect is patient consent and data ownership. Patients undergoing long-term cardiac monitoring should be fully informed about the types of data collected, how it will be used, and who will have access to it. Clear, comprehensive consent forms must be developed, allowing patients to make informed decisions about their data sharing preferences.
Data anonymization and de-identification techniques play a vital role in protecting patient privacy while enabling valuable research and analysis. By removing personally identifiable information from cardiac data sets, researchers can conduct studies on P wave changes without compromising individual privacy. However, care must be taken to ensure that de-identification methods are robust enough to prevent re-identification through data correlation or advanced analytics.
Compliance with healthcare data protection regulations, such as HIPAA in the United States or GDPR in Europe, is essential. These regulations set standards for data handling, storage, and sharing in healthcare settings. Organizations involved in long-term cardiac rehabilitation must establish comprehensive policies and procedures to ensure compliance with these regulations, including regular audits and staff training.
Access control and authentication mechanisms are crucial for maintaining patient data privacy. Healthcare providers should implement multi-factor authentication, role-based access controls, and detailed audit logs to monitor and restrict access to sensitive cardiac data. This helps prevent unauthorized personnel from viewing or modifying patient information.
As telemedicine and remote monitoring become increasingly prevalent in cardiac rehabilitation, additional privacy considerations arise. Secure video conferencing platforms, encrypted communication channels, and patient-controlled data sharing options must be integrated into remote monitoring systems to protect patient privacy during virtual consultations and data transmission.
Lastly, patient education on data privacy is vital. Healthcare providers should offer clear guidance on how patients can protect their own data, including best practices for securing personal devices used for cardiac monitoring and understanding the implications of sharing health data on social media or other platforms.
One of the primary challenges is ensuring secure data storage and transmission. Healthcare institutions must employ state-of-the-art encryption technologies and secure protocols to safeguard patient data from unauthorized access or breaches. This includes implementing end-to-end encryption for data in transit and at rest, as well as utilizing secure cloud storage solutions with stringent access controls.
Another crucial aspect is patient consent and data ownership. Patients undergoing long-term cardiac monitoring should be fully informed about the types of data collected, how it will be used, and who will have access to it. Clear, comprehensive consent forms must be developed, allowing patients to make informed decisions about their data sharing preferences.
Data anonymization and de-identification techniques play a vital role in protecting patient privacy while enabling valuable research and analysis. By removing personally identifiable information from cardiac data sets, researchers can conduct studies on P wave changes without compromising individual privacy. However, care must be taken to ensure that de-identification methods are robust enough to prevent re-identification through data correlation or advanced analytics.
Compliance with healthcare data protection regulations, such as HIPAA in the United States or GDPR in Europe, is essential. These regulations set standards for data handling, storage, and sharing in healthcare settings. Organizations involved in long-term cardiac rehabilitation must establish comprehensive policies and procedures to ensure compliance with these regulations, including regular audits and staff training.
Access control and authentication mechanisms are crucial for maintaining patient data privacy. Healthcare providers should implement multi-factor authentication, role-based access controls, and detailed audit logs to monitor and restrict access to sensitive cardiac data. This helps prevent unauthorized personnel from viewing or modifying patient information.
As telemedicine and remote monitoring become increasingly prevalent in cardiac rehabilitation, additional privacy considerations arise. Secure video conferencing platforms, encrypted communication channels, and patient-controlled data sharing options must be integrated into remote monitoring systems to protect patient privacy during virtual consultations and data transmission.
Lastly, patient education on data privacy is vital. Healthcare providers should offer clear guidance on how patients can protect their own data, including best practices for securing personal devices used for cardiac monitoring and understanding the implications of sharing health data on social media or other platforms.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!