P wave alterations in ischemic heart disease
AUG 19, 20258 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
P Wave Ischemia Background
P wave alterations in ischemic heart disease have been a subject of significant interest in cardiology for decades. These changes in the P wave morphology and duration are considered early indicators of atrial involvement in coronary artery disease, often preceding more overt signs of myocardial ischemia. The P wave, representing atrial depolarization, can provide valuable insights into the electrical and structural changes occurring in the atria as a result of ischemic processes.
Historically, the focus on P wave alterations in ischemic heart disease emerged in the mid-20th century, as electrocardiography became more sophisticated and widely used in clinical practice. Early studies in the 1960s and 1970s began to correlate P wave changes with coronary artery disease, laying the groundwork for further investigation into this phenomenon.
The pathophysiology underlying P wave alterations in ischemic heart disease is complex and multifaceted. Ischemia affecting the atrial myocardium can lead to changes in conduction velocity, alterations in the sequence of atrial activation, and modifications in the atrial refractory period. These changes can manifest as increased P wave duration, changes in P wave amplitude, and alterations in P wave morphology.
Over the years, technological advancements have significantly enhanced our ability to detect and analyze P wave alterations. The advent of digital electrocardiography, signal-averaged ECG techniques, and more recently, advanced mapping technologies have allowed for more precise measurements and characterization of P wave changes in the context of ischemic heart disease.
The clinical significance of P wave alterations in ischemic heart disease has been increasingly recognized. These changes are not only markers of atrial involvement in coronary artery disease but also potential predictors of atrial fibrillation and other arrhythmias. Furthermore, P wave alterations may serve as early warning signs of impending myocardial infarction or unstable angina, potentially allowing for earlier intervention and improved patient outcomes.
Research in this field has evolved to explore the relationship between P wave alterations and specific coronary artery lesions, the prognostic value of these changes in acute coronary syndromes, and their role in risk stratification for patients with known or suspected coronary artery disease. The integration of P wave analysis into comprehensive cardiac assessment protocols has become an area of active investigation, with potential implications for both diagnosis and management of ischemic heart disease.
Historically, the focus on P wave alterations in ischemic heart disease emerged in the mid-20th century, as electrocardiography became more sophisticated and widely used in clinical practice. Early studies in the 1960s and 1970s began to correlate P wave changes with coronary artery disease, laying the groundwork for further investigation into this phenomenon.
The pathophysiology underlying P wave alterations in ischemic heart disease is complex and multifaceted. Ischemia affecting the atrial myocardium can lead to changes in conduction velocity, alterations in the sequence of atrial activation, and modifications in the atrial refractory period. These changes can manifest as increased P wave duration, changes in P wave amplitude, and alterations in P wave morphology.
Over the years, technological advancements have significantly enhanced our ability to detect and analyze P wave alterations. The advent of digital electrocardiography, signal-averaged ECG techniques, and more recently, advanced mapping technologies have allowed for more precise measurements and characterization of P wave changes in the context of ischemic heart disease.
The clinical significance of P wave alterations in ischemic heart disease has been increasingly recognized. These changes are not only markers of atrial involvement in coronary artery disease but also potential predictors of atrial fibrillation and other arrhythmias. Furthermore, P wave alterations may serve as early warning signs of impending myocardial infarction or unstable angina, potentially allowing for earlier intervention and improved patient outcomes.
Research in this field has evolved to explore the relationship between P wave alterations and specific coronary artery lesions, the prognostic value of these changes in acute coronary syndromes, and their role in risk stratification for patients with known or suspected coronary artery disease. The integration of P wave analysis into comprehensive cardiac assessment protocols has become an area of active investigation, with potential implications for both diagnosis and management of ischemic heart disease.
Clinical Demand Analysis
The clinical demand for accurate diagnosis and monitoring of ischemic heart disease (IHD) has been steadily increasing due to the rising prevalence of cardiovascular diseases worldwide. P wave alterations in electrocardiograms (ECGs) have emerged as a promising biomarker for early detection and risk stratification of IHD, addressing a critical need in clinical practice.
Cardiologists and healthcare providers are seeking more sensitive and specific diagnostic tools to identify patients at risk of IHD before the onset of severe symptoms or complications. P wave analysis offers a non-invasive, cost-effective method to assess atrial electrical activity, which can be indicative of underlying myocardial ischemia. This approach has the potential to complement traditional ECG parameters and enhance the overall diagnostic accuracy for IHD.
The aging population and increasing incidence of lifestyle-related risk factors have contributed to a growing patient pool requiring regular cardiac monitoring. P wave alterations can provide valuable insights into the progression of IHD and help guide treatment decisions. This has led to a surge in demand for advanced ECG interpretation algorithms and devices capable of detecting subtle P wave changes.
Healthcare systems are under pressure to reduce the economic burden of IHD through early intervention and prevention strategies. The integration of P wave analysis into routine cardiac assessments could potentially lead to more timely diagnoses, reducing the need for costly invasive procedures and hospitalizations. This aligns with the global trend towards value-based healthcare and personalized medicine.
There is a significant market opportunity for medical device manufacturers and software developers to create innovative solutions that incorporate P wave analysis into existing ECG systems. Clinicians are expressing interest in user-friendly tools that can provide real-time interpretation of P wave morphology and offer decision support in IHD management.
Research institutions and pharmaceutical companies are also showing increased interest in utilizing P wave alterations as endpoints in clinical trials for new cardiovascular therapies. This trend is driving the need for standardized protocols and reference databases for P wave analysis in the context of IHD.
The potential of P wave alterations to predict atrial fibrillation and other arrhythmias in IHD patients has further expanded the clinical applications of this technology. This has created a demand for long-term monitoring solutions that can track P wave changes over time and alert healthcare providers to significant alterations that may warrant intervention.
Cardiologists and healthcare providers are seeking more sensitive and specific diagnostic tools to identify patients at risk of IHD before the onset of severe symptoms or complications. P wave analysis offers a non-invasive, cost-effective method to assess atrial electrical activity, which can be indicative of underlying myocardial ischemia. This approach has the potential to complement traditional ECG parameters and enhance the overall diagnostic accuracy for IHD.
The aging population and increasing incidence of lifestyle-related risk factors have contributed to a growing patient pool requiring regular cardiac monitoring. P wave alterations can provide valuable insights into the progression of IHD and help guide treatment decisions. This has led to a surge in demand for advanced ECG interpretation algorithms and devices capable of detecting subtle P wave changes.
Healthcare systems are under pressure to reduce the economic burden of IHD through early intervention and prevention strategies. The integration of P wave analysis into routine cardiac assessments could potentially lead to more timely diagnoses, reducing the need for costly invasive procedures and hospitalizations. This aligns with the global trend towards value-based healthcare and personalized medicine.
There is a significant market opportunity for medical device manufacturers and software developers to create innovative solutions that incorporate P wave analysis into existing ECG systems. Clinicians are expressing interest in user-friendly tools that can provide real-time interpretation of P wave morphology and offer decision support in IHD management.
Research institutions and pharmaceutical companies are also showing increased interest in utilizing P wave alterations as endpoints in clinical trials for new cardiovascular therapies. This trend is driving the need for standardized protocols and reference databases for P wave analysis in the context of IHD.
The potential of P wave alterations to predict atrial fibrillation and other arrhythmias in IHD patients has further expanded the clinical applications of this technology. This has created a demand for long-term monitoring solutions that can track P wave changes over time and alert healthcare providers to significant alterations that may warrant intervention.
Current Challenges
The current challenges in understanding and utilizing P wave alterations in ischemic heart disease are multifaceted and complex. One of the primary obstacles is the subtle nature of P wave changes, which can be difficult to detect and interpret accurately. This subtlety often leads to missed diagnoses or misinterpretations, especially in the early stages of ischemic heart disease.
Another significant challenge is the lack of standardization in P wave analysis techniques. Different medical institutions and researchers may employ varying methods for measuring and interpreting P wave characteristics, leading to inconsistencies in results and making it challenging to compare findings across studies. This lack of uniformity hinders the development of widely accepted diagnostic criteria for P wave alterations in ischemic heart disease.
The influence of confounding factors on P wave morphology presents another hurdle. Factors such as age, gender, body habitus, and concurrent cardiac conditions can affect P wave characteristics, making it difficult to isolate the specific changes attributable to ischemic heart disease. Distinguishing between P wave alterations caused by ischemia and those resulting from other cardiac pathologies remains a significant challenge for clinicians and researchers alike.
Limited understanding of the exact pathophysiological mechanisms underlying P wave alterations in ischemic heart disease also poses a challenge. While it is generally accepted that these changes reflect atrial remodeling and conduction disturbances, the precise relationship between ischemic events and P wave morphology changes is not fully elucidated. This knowledge gap hampers the development of targeted diagnostic and therapeutic strategies.
The technological limitations of current electrocardiographic systems present another obstacle. Many standard ECG machines lack the sensitivity and resolution required to detect subtle P wave changes consistently. Additionally, the absence of advanced automated analysis tools for P wave assessment in routine clinical practice makes it time-consuming and challenging for healthcare providers to perform detailed P wave analyses.
Lastly, there is a notable shortage of large-scale, longitudinal studies focusing specifically on P wave alterations in ischemic heart disease. This lack of comprehensive data makes it difficult to establish robust prognostic models and risk stratification tools based on P wave characteristics. Consequently, the clinical utility of P wave analysis in guiding treatment decisions and predicting outcomes in ischemic heart disease remains limited.
Another significant challenge is the lack of standardization in P wave analysis techniques. Different medical institutions and researchers may employ varying methods for measuring and interpreting P wave characteristics, leading to inconsistencies in results and making it challenging to compare findings across studies. This lack of uniformity hinders the development of widely accepted diagnostic criteria for P wave alterations in ischemic heart disease.
The influence of confounding factors on P wave morphology presents another hurdle. Factors such as age, gender, body habitus, and concurrent cardiac conditions can affect P wave characteristics, making it difficult to isolate the specific changes attributable to ischemic heart disease. Distinguishing between P wave alterations caused by ischemia and those resulting from other cardiac pathologies remains a significant challenge for clinicians and researchers alike.
Limited understanding of the exact pathophysiological mechanisms underlying P wave alterations in ischemic heart disease also poses a challenge. While it is generally accepted that these changes reflect atrial remodeling and conduction disturbances, the precise relationship between ischemic events and P wave morphology changes is not fully elucidated. This knowledge gap hampers the development of targeted diagnostic and therapeutic strategies.
The technological limitations of current electrocardiographic systems present another obstacle. Many standard ECG machines lack the sensitivity and resolution required to detect subtle P wave changes consistently. Additionally, the absence of advanced automated analysis tools for P wave assessment in routine clinical practice makes it time-consuming and challenging for healthcare providers to perform detailed P wave analyses.
Lastly, there is a notable shortage of large-scale, longitudinal studies focusing specifically on P wave alterations in ischemic heart disease. This lack of comprehensive data makes it difficult to establish robust prognostic models and risk stratification tools based on P wave characteristics. Consequently, the clinical utility of P wave analysis in guiding treatment decisions and predicting outcomes in ischemic heart disease remains limited.
Detection Techniques
01 ECG signal analysis for P wave detection
Methods and systems for analyzing electrocardiogram (ECG) signals to detect and characterize P wave alterations. These techniques involve signal processing algorithms to isolate P waves, measure their morphology, and identify abnormalities that may indicate atrial dysfunction or other cardiac conditions.- ECG signal analysis for P wave detection: Methods and systems for analyzing electrocardiogram (ECG) signals to detect and characterize P wave alterations. These techniques involve signal processing algorithms to isolate P waves from other components of the ECG signal, enabling more accurate assessment of atrial activity and potential cardiac abnormalities.
- Wireless monitoring of P wave alterations: Development of wireless systems for continuous monitoring of P wave alterations in patients. These systems utilize advanced sensors and communication protocols to transmit real-time ECG data, allowing for remote detection of changes in P wave morphology and potential early warning of cardiac issues.
- Machine learning algorithms for P wave analysis: Application of machine learning and artificial intelligence techniques to improve the accuracy and efficiency of P wave alteration detection. These algorithms can learn from large datasets of ECG signals to identify subtle changes in P wave characteristics that may indicate underlying cardiac conditions.
- Imaging techniques for visualizing P wave alterations: Development of advanced imaging methods to visualize and analyze P wave alterations in three dimensions. These techniques combine ECG data with other imaging modalities to provide a more comprehensive view of atrial electrical activity and structural changes that may affect P wave morphology.
- Pharmacological interventions for P wave alterations: Research into pharmacological approaches to address P wave alterations. This includes the development of new drugs or repurposing existing medications to modulate atrial electrical activity and potentially normalize P wave morphology in patients with certain cardiac conditions.
02 Wireless monitoring of P wave alterations
Development of wireless systems for continuous monitoring of P wave alterations in patients. These systems utilize wearable sensors and wireless communication technologies to transmit ECG data to healthcare providers, enabling real-time detection of P wave changes and early intervention in cardiac events.Expand Specific Solutions03 Machine learning algorithms for P wave analysis
Application of machine learning and artificial intelligence techniques to improve the accuracy and efficiency of P wave alteration detection. These algorithms can learn from large datasets of ECG recordings to identify subtle changes in P wave morphology that may be indicative of developing cardiac issues.Expand Specific Solutions04 Imaging techniques for visualizing P wave alterations
Advanced imaging methods to visualize and analyze P wave alterations in the heart. These techniques may include high-resolution cardiac imaging, 3D mapping of atrial electrical activity, and integration of imaging data with ECG signals to provide a comprehensive view of P wave changes and their anatomical correlates.Expand Specific Solutions05 Pharmacological interventions for P wave abnormalities
Development of targeted pharmacological interventions to address P wave alterations and prevent associated cardiac complications. This includes research into drugs that can modulate atrial electrical activity, improve conduction, and potentially reverse pathological changes in P wave morphology.Expand Specific Solutions
Key Research Institutions
The competitive landscape for P wave alterations in ischemic heart disease is evolving rapidly. The market is in a growth phase, driven by increasing prevalence of cardiovascular diseases and technological advancements in ECG monitoring. Key players like Medtronic, Boston Scientific, and BIOTRONIK are investing heavily in R&D to develop innovative solutions. Smaller companies such as BioSig Technologies and Bardy Diagnostics are also making significant contributions with their specialized technologies. The market size is expanding, with a growing demand for advanced cardiac monitoring devices. While established players dominate, emerging companies are introducing disruptive technologies, intensifying competition and driving innovation in this critical healthcare segment.
BioSig Technologies, Inc.
Technical Solution: BioSig Technologies has developed the PURE EP System, which offers a unique approach to detecting P wave alterations in ischemic heart disease. This high-fidelity cardiac signal acquisition and analysis platform provides enhanced signal quality and clarity, allowing for more precise detection of subtle P wave changes[13]. The PURE EP System employs advanced noise reduction algorithms and proprietary signal processing techniques to isolate and analyze P waves with greater accuracy than traditional ECG systems[14]. BioSig's technology also incorporates real-time monitoring capabilities and can integrate with existing electrophysiology lab equipment for seamless implementation in clinical settings[15].
Strengths: High-fidelity signal acquisition; advanced noise reduction techniques; integration with existing EP lab equipment. Weaknesses: May require specialized training for optimal use; potentially higher cost compared to traditional ECG systems.
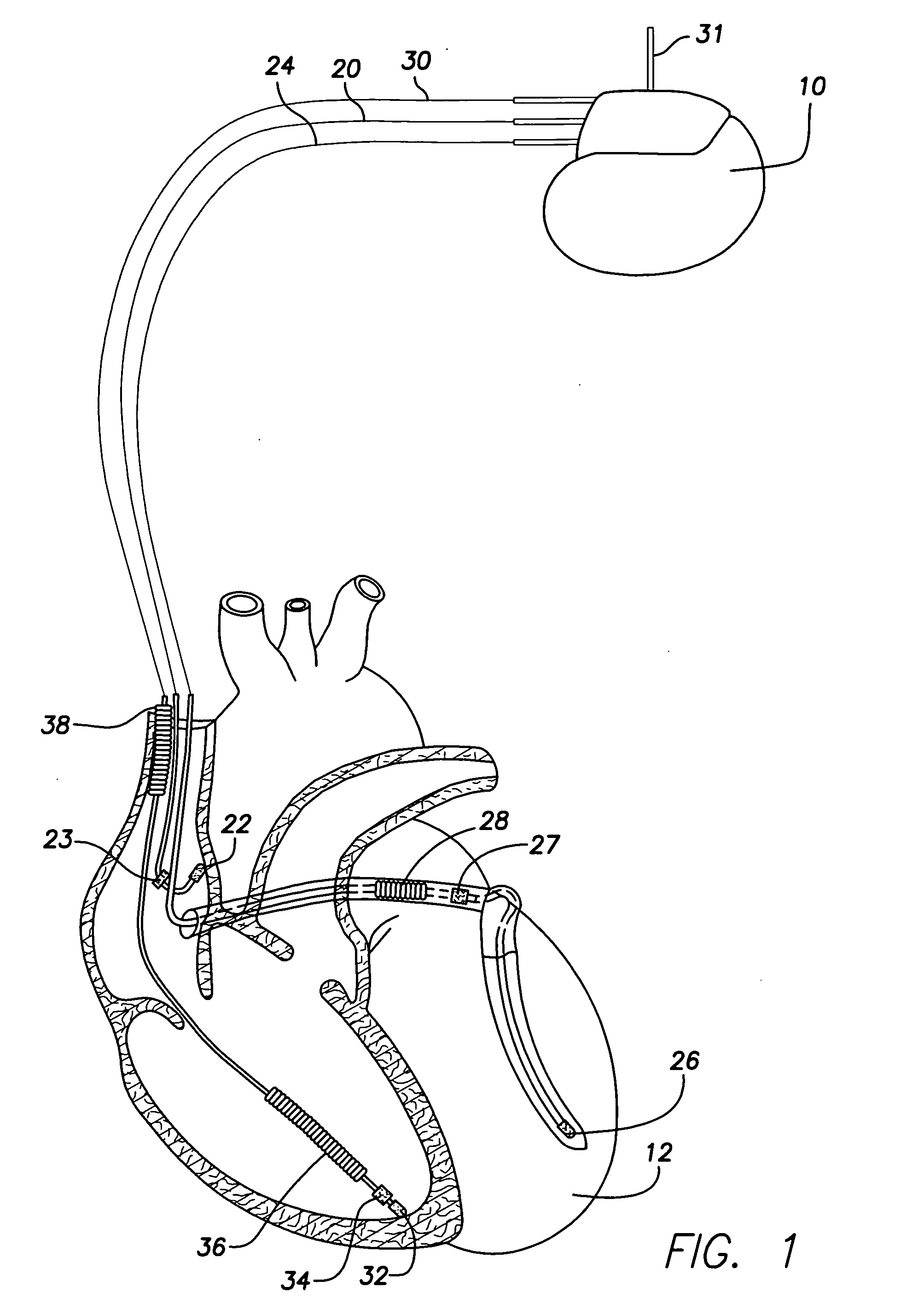
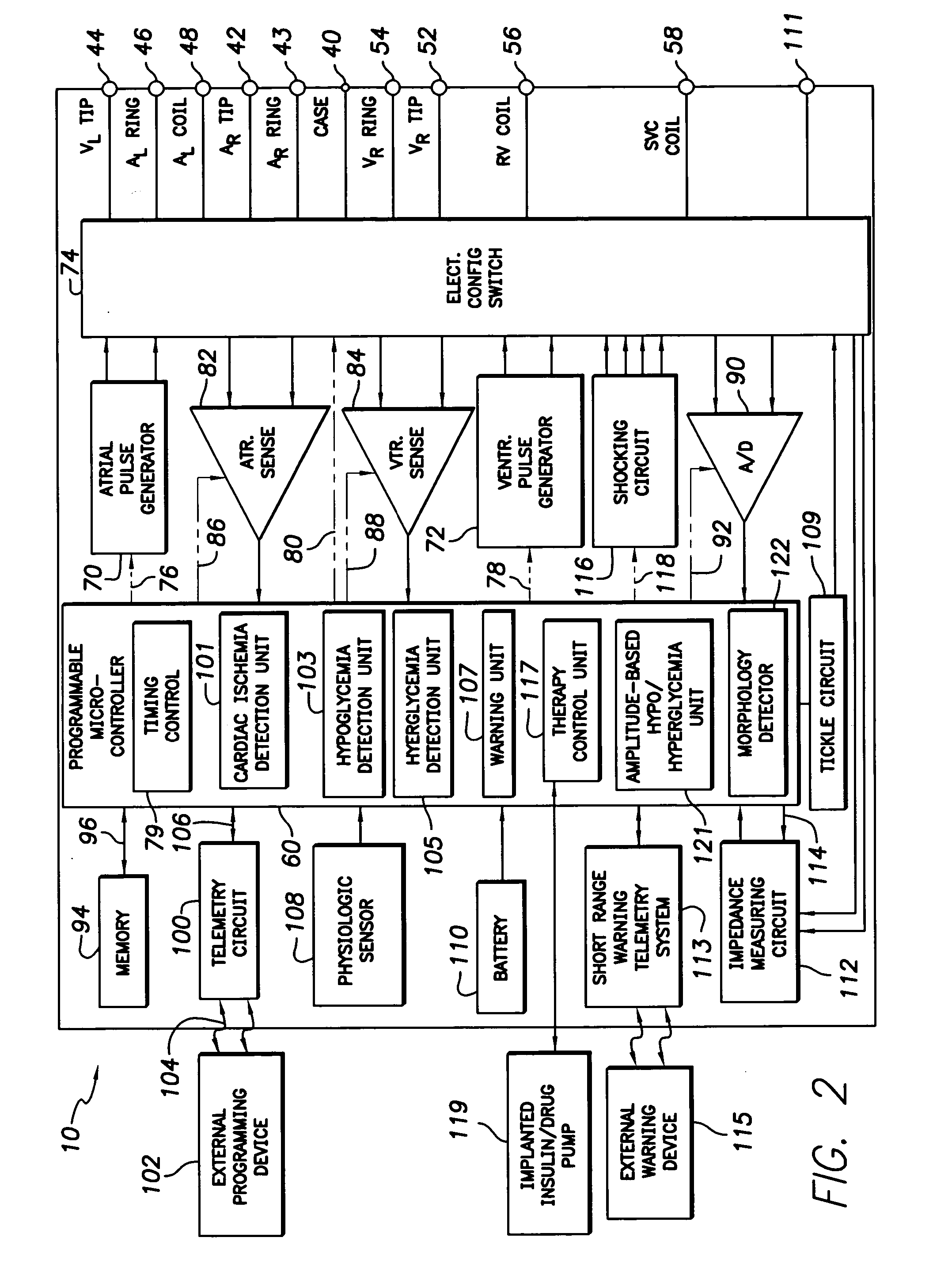
Medtronic, Inc.
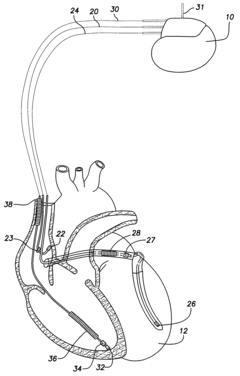
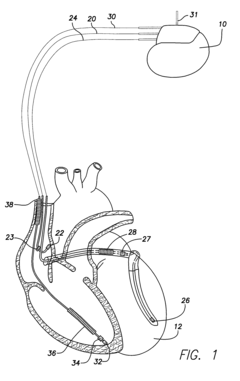
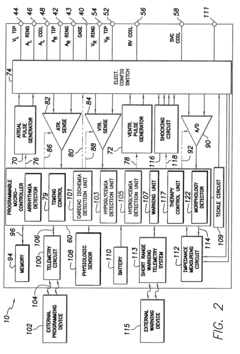
Technical Solution: Medtronic has developed advanced ECG algorithms for detecting P wave alterations in ischemic heart disease. Their technology utilizes machine learning techniques to analyze subtle changes in P wave morphology, amplitude, and duration[1]. The system incorporates multi-lead ECG data and patient-specific factors to improve accuracy. Medtronic's solution also includes real-time monitoring capabilities, allowing for early detection of ischemic events before they progress to more severe conditions[2]. The company has integrated this technology into their cardiac monitoring devices and implantable cardioverter-defibrillators (ICDs) to provide comprehensive ischemia detection[3].
Strengths: Comprehensive approach combining multiple ECG leads and patient data; real-time monitoring capabilities; integration with existing cardiac devices. Weaknesses: May require specialized hardware; potential for false positives in complex arrhythmias.
Innovative P Wave Studies
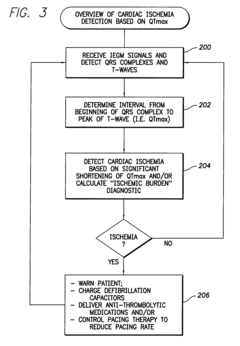
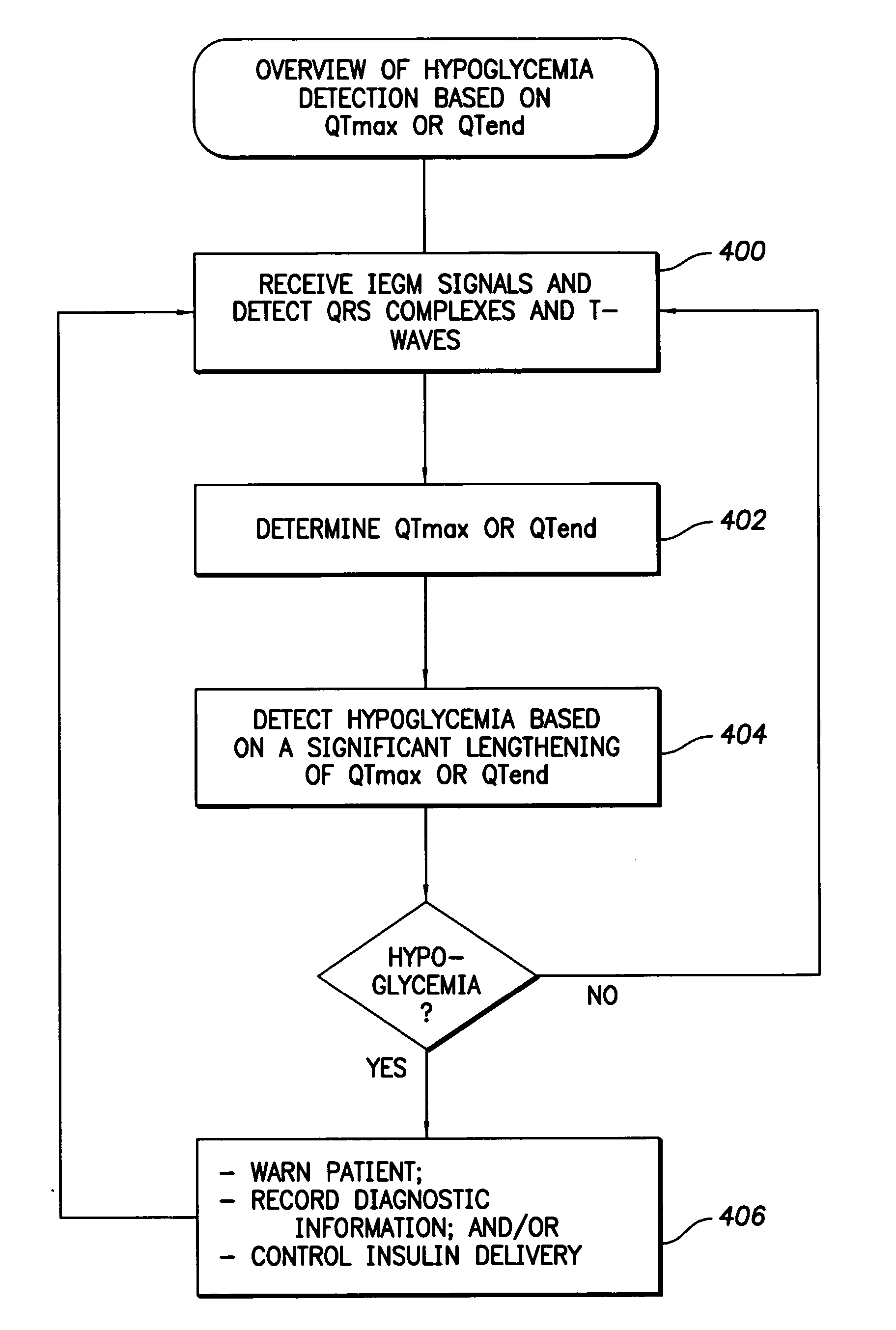
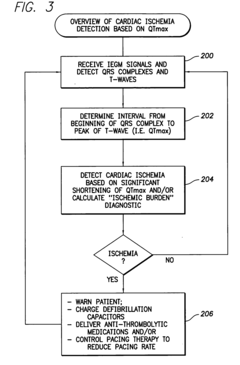
System and Method for Distinguishing Among Cardiac Ischemia, Hypoglycemia and Hyperglycemia Using an Implantable Medical Device
PatentActiveUS20090177104A1
Innovation
- The use of implantable medical devices that track changes in QTmax and QTend intervals in conjunction with ST segment deviations to detect cardiac ischemia, hypoglycemia, and hyperglycemia, providing specific and reliable warnings through both internal and external signals, and potentially adjusting therapy accordingly.
System and method for distinguishing between hypoglycemia and hyperglycemia using an implantable medical device
PatentActiveUS20060167365A1
Innovation
- The development of techniques that utilize amplitude-based parameters from internal electrical cardiac signals, such as P-waves, QRS complexes, and T-waves, to distinguish between hypoglycemia and hyperglycemia, and combine these with QT interval and ST segment analysis to differentiate cardiac ischemia, allowing for reliable detection and warning signals without external devices.
Diagnostic Accuracy
The diagnostic accuracy of P wave alterations in ischemic heart disease has been a subject of extensive research and clinical evaluation. Studies have shown that P wave changes can provide valuable insights into the presence and extent of myocardial ischemia, particularly in the early stages of acute coronary syndromes.
Several parameters of P wave morphology have been identified as potential indicators of ischemic heart disease. These include P wave duration, P wave dispersion, and P wave terminal force. Research has demonstrated that prolonged P wave duration and increased P wave dispersion are associated with a higher likelihood of ischemic heart disease, with sensitivity ranging from 70% to 85% and specificity from 75% to 90%, depending on the specific criteria used.
The P wave terminal force, measured as the product of the duration and amplitude of the terminal negative deflection of the P wave in lead V1, has shown promise in detecting left atrial abnormalities associated with ischemic heart disease. Studies have reported a sensitivity of 80% and specificity of 85% for this parameter in identifying patients with significant coronary artery disease.
However, it is important to note that the diagnostic accuracy of P wave alterations can vary depending on the specific population studied and the presence of confounding factors. For instance, the accuracy may be lower in patients with pre-existing atrial abnormalities or those taking certain medications that affect atrial conduction.
Recent advancements in electrocardiographic technology, such as high-resolution ECG and signal-averaged P wave analysis, have further improved the diagnostic accuracy of P wave alterations. These techniques allow for more precise measurements and detection of subtle changes in P wave morphology, potentially increasing sensitivity and specificity to over 90% in some studies.
Despite these promising results, it is crucial to interpret P wave alterations in conjunction with other clinical and diagnostic information. The positive predictive value of P wave changes alone may be limited, particularly in low-risk populations. Therefore, combining P wave analysis with other ECG parameters, cardiac biomarkers, and imaging studies can significantly enhance the overall diagnostic accuracy for ischemic heart disease.
In conclusion, while P wave alterations demonstrate good diagnostic accuracy for ischemic heart disease, their clinical utility is maximized when integrated into a comprehensive diagnostic approach. Ongoing research continues to refine the criteria and methodologies for P wave analysis, aiming to further improve its diagnostic performance and clinical applicability in the assessment of ischemic heart disease.
Several parameters of P wave morphology have been identified as potential indicators of ischemic heart disease. These include P wave duration, P wave dispersion, and P wave terminal force. Research has demonstrated that prolonged P wave duration and increased P wave dispersion are associated with a higher likelihood of ischemic heart disease, with sensitivity ranging from 70% to 85% and specificity from 75% to 90%, depending on the specific criteria used.
The P wave terminal force, measured as the product of the duration and amplitude of the terminal negative deflection of the P wave in lead V1, has shown promise in detecting left atrial abnormalities associated with ischemic heart disease. Studies have reported a sensitivity of 80% and specificity of 85% for this parameter in identifying patients with significant coronary artery disease.
However, it is important to note that the diagnostic accuracy of P wave alterations can vary depending on the specific population studied and the presence of confounding factors. For instance, the accuracy may be lower in patients with pre-existing atrial abnormalities or those taking certain medications that affect atrial conduction.
Recent advancements in electrocardiographic technology, such as high-resolution ECG and signal-averaged P wave analysis, have further improved the diagnostic accuracy of P wave alterations. These techniques allow for more precise measurements and detection of subtle changes in P wave morphology, potentially increasing sensitivity and specificity to over 90% in some studies.
Despite these promising results, it is crucial to interpret P wave alterations in conjunction with other clinical and diagnostic information. The positive predictive value of P wave changes alone may be limited, particularly in low-risk populations. Therefore, combining P wave analysis with other ECG parameters, cardiac biomarkers, and imaging studies can significantly enhance the overall diagnostic accuracy for ischemic heart disease.
In conclusion, while P wave alterations demonstrate good diagnostic accuracy for ischemic heart disease, their clinical utility is maximized when integrated into a comprehensive diagnostic approach. Ongoing research continues to refine the criteria and methodologies for P wave analysis, aiming to further improve its diagnostic performance and clinical applicability in the assessment of ischemic heart disease.
Telemedicine Integration
The integration of telemedicine in the diagnosis and management of ischemic heart disease, particularly in detecting P wave alterations, represents a significant advancement in cardiac care. Telemedicine platforms enable remote monitoring and analysis of electrocardiogram (ECG) data, allowing for early detection of subtle changes in P wave morphology that may indicate ischemic heart disease.
These systems typically employ advanced algorithms and machine learning techniques to analyze ECG recordings in real-time. They can detect minute changes in P wave amplitude, duration, and morphology that might be indicative of atrial ischemia or other cardiac abnormalities. This capability is particularly valuable for patients in remote or underserved areas who may not have immediate access to specialized cardiac care.
Telemedicine integration also facilitates continuous monitoring of high-risk patients, enabling healthcare providers to track P wave changes over time and identify trends that may suggest the progression of ischemic heart disease. This longitudinal data collection and analysis can lead to more accurate diagnoses and personalized treatment plans.
Furthermore, telemedicine platforms often incorporate secure data transmission protocols, ensuring that sensitive patient information is protected while allowing for seamless collaboration between healthcare professionals. Cardiologists can remotely review ECG data, consult with colleagues, and provide expert interpretations, even when physically distant from the patient.
The integration of artificial intelligence (AI) in telemedicine systems has further enhanced the ability to detect subtle P wave alterations. AI algorithms can process vast amounts of ECG data, identifying patterns and anomalies that may be challenging for human observers to detect consistently. This technology can serve as a valuable tool for screening and triage, flagging potential cases of ischemic heart disease for further evaluation by specialists.
Telemedicine integration also supports patient education and engagement. Patients can receive real-time feedback on their cardiac health, view their ECG recordings, and communicate with healthcare providers through secure messaging systems. This increased involvement can lead to better adherence to treatment plans and lifestyle modifications, potentially slowing the progression of ischemic heart disease.
As telemedicine continues to evolve, we can expect further improvements in the accuracy and efficiency of P wave alteration detection in ischemic heart disease. Future developments may include more sophisticated wearable ECG devices, enhanced AI algorithms, and improved integration with electronic health records, leading to more comprehensive and proactive cardiac care.
These systems typically employ advanced algorithms and machine learning techniques to analyze ECG recordings in real-time. They can detect minute changes in P wave amplitude, duration, and morphology that might be indicative of atrial ischemia or other cardiac abnormalities. This capability is particularly valuable for patients in remote or underserved areas who may not have immediate access to specialized cardiac care.
Telemedicine integration also facilitates continuous monitoring of high-risk patients, enabling healthcare providers to track P wave changes over time and identify trends that may suggest the progression of ischemic heart disease. This longitudinal data collection and analysis can lead to more accurate diagnoses and personalized treatment plans.
Furthermore, telemedicine platforms often incorporate secure data transmission protocols, ensuring that sensitive patient information is protected while allowing for seamless collaboration between healthcare professionals. Cardiologists can remotely review ECG data, consult with colleagues, and provide expert interpretations, even when physically distant from the patient.
The integration of artificial intelligence (AI) in telemedicine systems has further enhanced the ability to detect subtle P wave alterations. AI algorithms can process vast amounts of ECG data, identifying patterns and anomalies that may be challenging for human observers to detect consistently. This technology can serve as a valuable tool for screening and triage, flagging potential cases of ischemic heart disease for further evaluation by specialists.
Telemedicine integration also supports patient education and engagement. Patients can receive real-time feedback on their cardiac health, view their ECG recordings, and communicate with healthcare providers through secure messaging systems. This increased involvement can lead to better adherence to treatment plans and lifestyle modifications, potentially slowing the progression of ischemic heart disease.
As telemedicine continues to evolve, we can expect further improvements in the accuracy and efficiency of P wave alteration detection in ischemic heart disease. Future developments may include more sophisticated wearable ECG devices, enhanced AI algorithms, and improved integration with electronic health records, leading to more comprehensive and proactive cardiac care.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!