Conduction system analysis using P wave parameters
AUG 19, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
P Wave Analysis Background
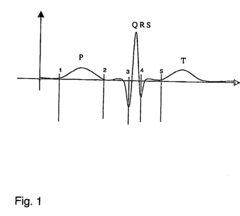
The P wave, also known as the primary wave or pressure wave, is a fundamental component of electrocardiography (ECG) and plays a crucial role in the analysis of cardiac conduction systems. As the first electrical signal detected in the cardiac cycle, the P wave represents atrial depolarization and provides valuable insights into the heart's electrical activity and potential abnormalities.
P wave analysis has a rich history in cardiology, dating back to the early 20th century when Willem Einthoven developed the first practical electrocardiograph. Since then, advancements in technology and understanding of cardiac electrophysiology have significantly enhanced our ability to interpret P wave parameters and their clinical significance.
The importance of P wave analysis lies in its potential to detect and diagnose various cardiac conditions, including atrial enlargement, conduction disorders, and arrhythmias. By examining the morphology, duration, and amplitude of P waves, clinicians can gain valuable information about the atrial activation sequence and identify potential abnormalities in the heart's conduction system.
In recent years, there has been a growing interest in utilizing P wave parameters for more advanced cardiac assessments. Researchers and clinicians have explored the use of P wave analysis in predicting the risk of atrial fibrillation, assessing left atrial function, and evaluating the effectiveness of various cardiac interventions.
The evolution of P wave analysis techniques has been driven by advancements in signal processing, machine learning, and computational modeling. These technological developments have enabled more precise and automated analysis of P wave parameters, leading to improved diagnostic accuracy and the potential for early detection of cardiac abnormalities.
Current research in P wave analysis focuses on several key areas, including the development of novel algorithms for P wave detection and delineation, the exploration of new P wave parameters with enhanced diagnostic value, and the integration of P wave analysis with other cardiac imaging modalities for comprehensive cardiac assessment.
As the field of cardiology continues to advance, P wave analysis remains a critical tool in understanding and diagnosing cardiac conduction system abnormalities. The ongoing research and technological innovations in this area promise to further enhance our ability to detect, diagnose, and manage a wide range of cardiac conditions, ultimately improving patient outcomes and quality of life.
P wave analysis has a rich history in cardiology, dating back to the early 20th century when Willem Einthoven developed the first practical electrocardiograph. Since then, advancements in technology and understanding of cardiac electrophysiology have significantly enhanced our ability to interpret P wave parameters and their clinical significance.
The importance of P wave analysis lies in its potential to detect and diagnose various cardiac conditions, including atrial enlargement, conduction disorders, and arrhythmias. By examining the morphology, duration, and amplitude of P waves, clinicians can gain valuable information about the atrial activation sequence and identify potential abnormalities in the heart's conduction system.
In recent years, there has been a growing interest in utilizing P wave parameters for more advanced cardiac assessments. Researchers and clinicians have explored the use of P wave analysis in predicting the risk of atrial fibrillation, assessing left atrial function, and evaluating the effectiveness of various cardiac interventions.
The evolution of P wave analysis techniques has been driven by advancements in signal processing, machine learning, and computational modeling. These technological developments have enabled more precise and automated analysis of P wave parameters, leading to improved diagnostic accuracy and the potential for early detection of cardiac abnormalities.
Current research in P wave analysis focuses on several key areas, including the development of novel algorithms for P wave detection and delineation, the exploration of new P wave parameters with enhanced diagnostic value, and the integration of P wave analysis with other cardiac imaging modalities for comprehensive cardiac assessment.
As the field of cardiology continues to advance, P wave analysis remains a critical tool in understanding and diagnosing cardiac conduction system abnormalities. The ongoing research and technological innovations in this area promise to further enhance our ability to detect, diagnose, and manage a wide range of cardiac conditions, ultimately improving patient outcomes and quality of life.
Clinical Demand for Conduction System Analysis
The clinical demand for conduction system analysis using P wave parameters has been steadily increasing in recent years. This growing interest stems from the recognition that P wave analysis can provide valuable insights into atrial conduction abnormalities and potential arrhythmogenic substrates. Cardiologists and electrophysiologists are particularly interested in this approach as it offers a non-invasive method to assess atrial electrical activity and predict the risk of atrial fibrillation.
In clinical practice, there is a significant need for early detection and risk stratification of atrial fibrillation, which is the most common sustained cardiac arrhythmia. P wave analysis can potentially identify patients at higher risk of developing atrial fibrillation before the onset of symptoms, allowing for earlier intervention and prevention strategies. This is particularly important in aging populations, where the prevalence of atrial fibrillation is higher and the associated complications, such as stroke and heart failure, are more severe.
Furthermore, the demand for conduction system analysis extends beyond atrial fibrillation prediction. Clinicians are seeking tools to evaluate the effectiveness of various treatments, including antiarrhythmic medications and ablation procedures. P wave parameters can serve as markers of atrial remodeling and help monitor the progression or regression of atrial pathology over time.
In the field of cardiac resynchronization therapy, there is a growing interest in using P wave analysis to optimize device programming and patient selection. By assessing atrial conduction patterns, clinicians aim to improve the response rates to cardiac resynchronization therapy and reduce the incidence of atrial arrhythmias in this patient population.
The integration of artificial intelligence and machine learning algorithms with P wave analysis has opened new avenues for research and clinical applications. There is a strong demand for automated systems that can process large volumes of ECG data and provide rapid, accurate interpretations of P wave parameters. This could significantly enhance the efficiency of cardiac care and enable more widespread screening for atrial conduction abnormalities.
Additionally, there is an increasing focus on personalized medicine in cardiology. Clinicians are looking for tools that can help tailor treatment strategies based on individual patient characteristics. P wave analysis offers the potential to identify specific conduction patterns that may guide therapeutic decisions, such as the choice between rate control and rhythm control strategies in atrial fibrillation management.
In summary, the clinical demand for conduction system analysis using P wave parameters is driven by the need for improved risk stratification, treatment monitoring, and personalized care in cardiac patients. As research in this field continues to advance, it is expected that P wave analysis will play an increasingly important role in clinical decision-making and patient management strategies.
In clinical practice, there is a significant need for early detection and risk stratification of atrial fibrillation, which is the most common sustained cardiac arrhythmia. P wave analysis can potentially identify patients at higher risk of developing atrial fibrillation before the onset of symptoms, allowing for earlier intervention and prevention strategies. This is particularly important in aging populations, where the prevalence of atrial fibrillation is higher and the associated complications, such as stroke and heart failure, are more severe.
Furthermore, the demand for conduction system analysis extends beyond atrial fibrillation prediction. Clinicians are seeking tools to evaluate the effectiveness of various treatments, including antiarrhythmic medications and ablation procedures. P wave parameters can serve as markers of atrial remodeling and help monitor the progression or regression of atrial pathology over time.
In the field of cardiac resynchronization therapy, there is a growing interest in using P wave analysis to optimize device programming and patient selection. By assessing atrial conduction patterns, clinicians aim to improve the response rates to cardiac resynchronization therapy and reduce the incidence of atrial arrhythmias in this patient population.
The integration of artificial intelligence and machine learning algorithms with P wave analysis has opened new avenues for research and clinical applications. There is a strong demand for automated systems that can process large volumes of ECG data and provide rapid, accurate interpretations of P wave parameters. This could significantly enhance the efficiency of cardiac care and enable more widespread screening for atrial conduction abnormalities.
Additionally, there is an increasing focus on personalized medicine in cardiology. Clinicians are looking for tools that can help tailor treatment strategies based on individual patient characteristics. P wave analysis offers the potential to identify specific conduction patterns that may guide therapeutic decisions, such as the choice between rate control and rhythm control strategies in atrial fibrillation management.
In summary, the clinical demand for conduction system analysis using P wave parameters is driven by the need for improved risk stratification, treatment monitoring, and personalized care in cardiac patients. As research in this field continues to advance, it is expected that P wave analysis will play an increasingly important role in clinical decision-making and patient management strategies.
Current P Wave Parameter Extraction Techniques
P wave parameter extraction techniques have evolved significantly in recent years, offering more accurate and efficient methods for conduction system analysis. The current state-of-the-art approaches can be broadly categorized into time-domain, frequency-domain, and machine learning-based techniques.
Time-domain techniques focus on extracting P wave parameters directly from the ECG signal. These methods typically involve signal preprocessing, P wave detection, and feature extraction. Wavelet transform-based approaches have gained popularity due to their ability to analyze signals at multiple scales. Adaptive thresholding and template matching algorithms are commonly used for P wave detection, while morphological operations help in delineating P wave boundaries.
Frequency-domain techniques leverage spectral analysis to extract P wave parameters. Fast Fourier Transform (FFT) and Short-Time Fourier Transform (STFT) are widely used to analyze the frequency content of P waves. These methods can reveal subtle changes in P wave morphology that may not be apparent in the time domain. Advanced techniques like Hilbert-Huang Transform (HHT) have shown promise in analyzing non-stationary and non-linear P wave signals.
Machine learning-based approaches have emerged as powerful tools for P wave parameter extraction. Supervised learning algorithms, such as Support Vector Machines (SVM) and Random Forests, have been successfully applied to classify P wave morphologies and extract relevant features. Deep learning models, particularly Convolutional Neural Networks (CNNs) and Long Short-Term Memory (LSTM) networks, have demonstrated superior performance in automated P wave analysis.
Recent advancements in P wave parameter extraction include the development of hybrid techniques that combine multiple approaches. For instance, wavelet-based feature extraction coupled with machine learning classifiers has shown improved accuracy in P wave detection and characterization. Additionally, adaptive filtering techniques have been employed to enhance P wave signal quality before parameter extraction.
Emerging trends in P wave parameter extraction focus on real-time analysis and personalized approaches. Wearable ECG devices and mobile health applications are driving the need for computationally efficient algorithms that can operate on resource-constrained devices. Moreover, there is a growing interest in developing patient-specific models that can account for individual variations in P wave morphology and improve the accuracy of conduction system analysis.
Time-domain techniques focus on extracting P wave parameters directly from the ECG signal. These methods typically involve signal preprocessing, P wave detection, and feature extraction. Wavelet transform-based approaches have gained popularity due to their ability to analyze signals at multiple scales. Adaptive thresholding and template matching algorithms are commonly used for P wave detection, while morphological operations help in delineating P wave boundaries.
Frequency-domain techniques leverage spectral analysis to extract P wave parameters. Fast Fourier Transform (FFT) and Short-Time Fourier Transform (STFT) are widely used to analyze the frequency content of P waves. These methods can reveal subtle changes in P wave morphology that may not be apparent in the time domain. Advanced techniques like Hilbert-Huang Transform (HHT) have shown promise in analyzing non-stationary and non-linear P wave signals.
Machine learning-based approaches have emerged as powerful tools for P wave parameter extraction. Supervised learning algorithms, such as Support Vector Machines (SVM) and Random Forests, have been successfully applied to classify P wave morphologies and extract relevant features. Deep learning models, particularly Convolutional Neural Networks (CNNs) and Long Short-Term Memory (LSTM) networks, have demonstrated superior performance in automated P wave analysis.
Recent advancements in P wave parameter extraction include the development of hybrid techniques that combine multiple approaches. For instance, wavelet-based feature extraction coupled with machine learning classifiers has shown improved accuracy in P wave detection and characterization. Additionally, adaptive filtering techniques have been employed to enhance P wave signal quality before parameter extraction.
Emerging trends in P wave parameter extraction focus on real-time analysis and personalized approaches. Wearable ECG devices and mobile health applications are driving the need for computationally efficient algorithms that can operate on resource-constrained devices. Moreover, there is a growing interest in developing patient-specific models that can account for individual variations in P wave morphology and improve the accuracy of conduction system analysis.
Existing P Wave Analysis Algorithms
01 P wave detection and analysis in ECG signals
Methods and systems for detecting and analyzing P waves in electrocardiogram (ECG) signals. This includes techniques for identifying P wave onset, offset, and morphology, which are crucial for assessing atrial conduction and potential cardiac abnormalities.- P wave detection and analysis in ECG signals: Methods and systems for detecting and analyzing P waves in electrocardiogram (ECG) signals. This includes techniques for identifying P wave onset, offset, and morphology, which are crucial for assessing atrial conduction and potential cardiac abnormalities.
- Conduction system modeling and simulation: Techniques for modeling and simulating the cardiac conduction system, including the generation and propagation of P waves. These models can be used to study normal and abnormal conduction patterns, aiding in the understanding of various cardiac conditions.
- P wave parameter extraction and measurement: Methods for extracting and measuring various P wave parameters, such as amplitude, duration, and area. These measurements are essential for quantifying atrial conduction properties and identifying potential abnormalities in the conduction system.
- Advanced signal processing for P wave analysis: Advanced signal processing techniques, including wavelet transforms and machine learning algorithms, applied to P wave analysis. These methods aim to improve the accuracy and reliability of P wave detection and characterization in complex ECG signals.
- P wave analysis in implantable cardiac devices: Integration of P wave analysis algorithms in implantable cardiac devices such as pacemakers and defibrillators. These algorithms enable real-time monitoring of atrial conduction and can be used to optimize device settings and detect potential arrhythmias.
02 Conduction system modeling and simulation
Approaches for modeling and simulating the cardiac conduction system, including the generation and propagation of P waves. These models help in understanding normal and abnormal conduction patterns and can be used for research and diagnostic purposes.Expand Specific Solutions03 P wave parameter measurement and quantification
Techniques for measuring and quantifying various P wave parameters, such as amplitude, duration, and area. These measurements are essential for diagnosing atrial abnormalities and assessing overall cardiac health.Expand Specific Solutions04 Signal processing for P wave enhancement
Advanced signal processing methods to enhance P wave detection and analysis in noisy or complex ECG recordings. These techniques improve the accuracy of P wave parameter measurements and interpretation.Expand Specific Solutions05 P wave analysis for arrhythmia detection
Utilization of P wave parameters and characteristics for detecting and classifying various cardiac arrhythmias. This includes methods for distinguishing between different types of atrial fibrillation and other conduction abnormalities.Expand Specific Solutions
Key Players in Cardiac Monitoring Industry
The conduction system analysis using P wave parameters is an emerging field in cardiac diagnostics, currently in its early development stage. The market size is growing, driven by increasing prevalence of cardiovascular diseases and demand for non-invasive diagnostic tools. While the technology is still evolving, several key players are advancing its maturity. Companies like Medtronic, Pacesetter (Abbott), and Cardiac Pacemakers (Boston Scientific) are leveraging their expertise in cardiac devices to develop P wave analysis technologies. Research institutions such as the University of Adelaide and University of Granada are contributing to the fundamental science. Emerging players like Bardy Diagnostics are introducing innovative P wave-centric ECG monitoring solutions, indicating a competitive and dynamic landscape in this niche but promising area of cardiac diagnostics.
Koninklijke Philips NV
Technical Solution: Philips has developed a sophisticated P wave analysis system for conduction system evaluation. Their approach combines high-resolution ECG acquisition with advanced signal processing algorithms to extract detailed P wave characteristics[4]. The system utilizes a multi-lead ECG approach, analyzing P wave morphology, duration, and axis across 12 leads to provide a comprehensive assessment of atrial conduction[5]. Philips' technology incorporates machine learning models trained on large datasets to identify subtle P wave abnormalities indicative of various conduction disorders. The system also features automated P wave segmentation and measurement, improving consistency and reducing analysis time[6].
Strengths: High-resolution ECG acquisition, comprehensive multi-lead analysis, automated measurements for improved efficiency. Weaknesses: May require specialized ECG equipment, potentially complex for use in some clinical settings.
Pacesetter, Inc.
Technical Solution: Pacesetter has developed an innovative approach to conduction system analysis using P wave parameters. Their technology focuses on high-precision P wave timing and morphology assessment across multiple cardiac cycles[7]. The system utilizes advanced signal averaging techniques to enhance P wave signal quality and reduce noise. Pacesetter's algorithm analyzes P wave onset, peak, and offset timings, as well as amplitude and area under the curve, to provide detailed insights into atrial conduction properties[8]. The technology also incorporates P wave variability analysis to detect subtle changes in conduction patterns over time, which can be indicative of developing arrhythmias or conduction disorders[9].
Strengths: High-precision P wave timing analysis, assessment of P wave variability over time. Weaknesses: May require longer recording durations for optimal analysis, potentially less suitable for rapid bedside assessment.
Innovations in P Wave Morphology Assessment
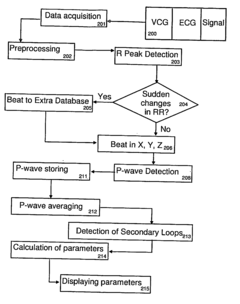
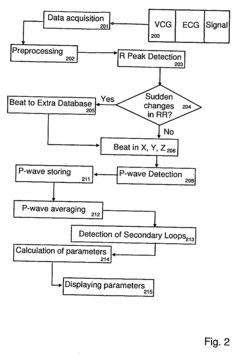
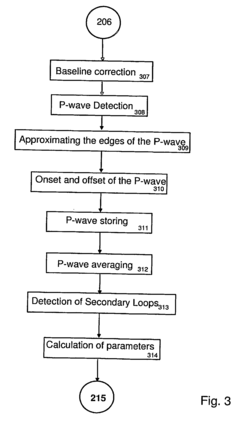
System and method for analysing the p-wave of an ecg-signal
PatentInactiveUS20070010752A1
Innovation
- A cardiac analysis method and system that acquires ECG signals, detects P-waves using a template-based approach, and calculates parameter values to focus on the dynamic changes of the P-wave, comparing each detected wave to a reference wave in a defined time period, providing a three-dimensional analysis of P-wave dynamics.
P Wave detection system
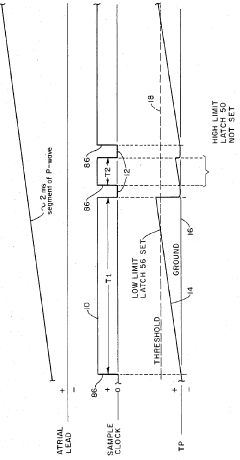
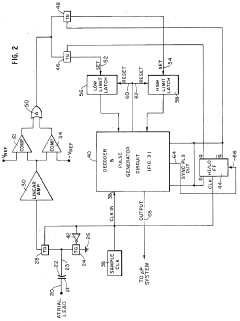
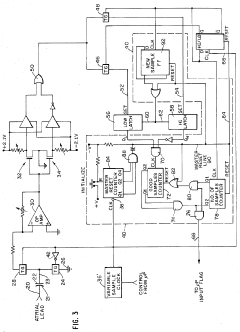
PatentInactiveUS4510945A
Innovation
- A P wave detection system that employs sampling means with adjustable timing to determine the slew rate of cardiac signals, using consecutively alternating sample windows to differentiate between P and R waves without relying on amplitude discrimination or analog filtering, generating a signal only when the sampled signal meets specific slew rate criteria.
Regulatory Framework for ECG Analysis Tools
The regulatory framework for ECG analysis tools plays a crucial role in ensuring the safety, efficacy, and reliability of these devices in clinical practice. In the United States, the Food and Drug Administration (FDA) is responsible for overseeing the regulation of medical devices, including ECG analysis tools. These tools are typically classified as Class II medical devices, requiring premarket notification (510(k)) clearance before they can be marketed.
The FDA's regulatory approach for ECG analysis tools focuses on several key aspects. First, manufacturers must demonstrate that their devices are substantially equivalent to predicate devices already on the market. This involves providing evidence of similar intended use, technological characteristics, and performance data. Additionally, the FDA requires manufacturers to implement and maintain quality management systems that comply with Good Manufacturing Practice (GMP) regulations.
For ECG analysis tools specifically designed for P wave parameter analysis, the regulatory requirements may be more stringent due to the specialized nature of the technology. Manufacturers must provide comprehensive clinical data demonstrating the accuracy and reliability of their P wave analysis algorithms. This often involves conducting clinical studies to validate the tool's performance against established gold standards or expert interpretations.
The regulatory framework also addresses software validation and verification processes. As ECG analysis tools increasingly rely on complex algorithms and artificial intelligence, the FDA has developed guidance documents specifically tailored to software as a medical device (SaMD). These guidelines outline the expectations for software development, testing, and maintenance throughout the product lifecycle.
Internationally, regulatory bodies such as the European Medicines Agency (EMA) and Japan's Pharmaceuticals and Medical Devices Agency (PMDA) have similar frameworks in place. The International Medical Device Regulators Forum (IMDRF) works to harmonize regulatory approaches across different countries, facilitating global market access for ECG analysis tools.
Cybersecurity considerations have become increasingly important in the regulatory landscape for ECG analysis tools. As these devices often connect to hospital networks and store sensitive patient data, manufacturers must implement robust security measures to protect against potential breaches or unauthorized access. The FDA and other regulatory bodies have issued guidance on cybersecurity best practices for medical devices, which manufacturers must adhere to throughout the product development and post-market phases.
The FDA's regulatory approach for ECG analysis tools focuses on several key aspects. First, manufacturers must demonstrate that their devices are substantially equivalent to predicate devices already on the market. This involves providing evidence of similar intended use, technological characteristics, and performance data. Additionally, the FDA requires manufacturers to implement and maintain quality management systems that comply with Good Manufacturing Practice (GMP) regulations.
For ECG analysis tools specifically designed for P wave parameter analysis, the regulatory requirements may be more stringent due to the specialized nature of the technology. Manufacturers must provide comprehensive clinical data demonstrating the accuracy and reliability of their P wave analysis algorithms. This often involves conducting clinical studies to validate the tool's performance against established gold standards or expert interpretations.
The regulatory framework also addresses software validation and verification processes. As ECG analysis tools increasingly rely on complex algorithms and artificial intelligence, the FDA has developed guidance documents specifically tailored to software as a medical device (SaMD). These guidelines outline the expectations for software development, testing, and maintenance throughout the product lifecycle.
Internationally, regulatory bodies such as the European Medicines Agency (EMA) and Japan's Pharmaceuticals and Medical Devices Agency (PMDA) have similar frameworks in place. The International Medical Device Regulators Forum (IMDRF) works to harmonize regulatory approaches across different countries, facilitating global market access for ECG analysis tools.
Cybersecurity considerations have become increasingly important in the regulatory landscape for ECG analysis tools. As these devices often connect to hospital networks and store sensitive patient data, manufacturers must implement robust security measures to protect against potential breaches or unauthorized access. The FDA and other regulatory bodies have issued guidance on cybersecurity best practices for medical devices, which manufacturers must adhere to throughout the product development and post-market phases.
AI Integration in P Wave Analysis
The integration of artificial intelligence (AI) in P wave analysis represents a significant advancement in conduction system analysis. Machine learning algorithms, particularly deep learning models, have demonstrated remarkable capabilities in extracting and interpreting complex patterns from electrocardiogram (ECG) data. These AI-driven approaches offer enhanced accuracy, efficiency, and reproducibility in analyzing P wave parameters.
One of the primary applications of AI in P wave analysis is automated feature extraction. Convolutional neural networks (CNNs) have shown promise in identifying and measuring key P wave characteristics, such as amplitude, duration, and morphology. These models can process large volumes of ECG data rapidly, enabling more comprehensive and consistent analyses compared to traditional manual methods.
AI algorithms also excel in detecting subtle P wave abnormalities that may be challenging for human interpreters to identify consistently. By leveraging vast datasets of annotated ECGs, these systems can learn to recognize patterns associated with various cardiac conduction disorders, including atrial fibrillation, atrial flutter, and interatrial block.
Furthermore, AI-powered predictive models are being developed to assess the risk of future cardiac events based on P wave parameters. These models integrate multiple features extracted from the P wave, along with other clinical data, to provide personalized risk stratification for patients. Such predictive capabilities have the potential to enhance early intervention strategies and improve patient outcomes.
The implementation of AI in P wave analysis also facilitates longitudinal studies and population-level assessments. By automating the analysis process, researchers can efficiently process large-scale ECG databases, enabling the identification of trends and patterns across diverse patient populations. This capability is particularly valuable for epidemiological studies and the development of more refined diagnostic criteria.
However, the integration of AI in P wave analysis is not without challenges. Ensuring the interpretability and explainability of AI-derived results remains a crucial concern, particularly in clinical settings where transparency in decision-making processes is essential. Additionally, the generalizability of AI models across different patient populations and ECG recording systems requires ongoing validation and refinement.
As AI technologies continue to evolve, their role in P wave analysis is expected to expand further. Future developments may include real-time analysis capabilities for continuous monitoring, integration with other cardiac imaging modalities for more comprehensive assessments, and the development of AI-assisted diagnostic support systems for clinicians.
One of the primary applications of AI in P wave analysis is automated feature extraction. Convolutional neural networks (CNNs) have shown promise in identifying and measuring key P wave characteristics, such as amplitude, duration, and morphology. These models can process large volumes of ECG data rapidly, enabling more comprehensive and consistent analyses compared to traditional manual methods.
AI algorithms also excel in detecting subtle P wave abnormalities that may be challenging for human interpreters to identify consistently. By leveraging vast datasets of annotated ECGs, these systems can learn to recognize patterns associated with various cardiac conduction disorders, including atrial fibrillation, atrial flutter, and interatrial block.
Furthermore, AI-powered predictive models are being developed to assess the risk of future cardiac events based on P wave parameters. These models integrate multiple features extracted from the P wave, along with other clinical data, to provide personalized risk stratification for patients. Such predictive capabilities have the potential to enhance early intervention strategies and improve patient outcomes.
The implementation of AI in P wave analysis also facilitates longitudinal studies and population-level assessments. By automating the analysis process, researchers can efficiently process large-scale ECG databases, enabling the identification of trends and patterns across diverse patient populations. This capability is particularly valuable for epidemiological studies and the development of more refined diagnostic criteria.
However, the integration of AI in P wave analysis is not without challenges. Ensuring the interpretability and explainability of AI-derived results remains a crucial concern, particularly in clinical settings where transparency in decision-making processes is essential. Additionally, the generalizability of AI models across different patient populations and ECG recording systems requires ongoing validation and refinement.
As AI technologies continue to evolve, their role in P wave analysis is expected to expand further. Future developments may include real-time analysis capabilities for continuous monitoring, integration with other cardiac imaging modalities for more comprehensive assessments, and the development of AI-assisted diagnostic support systems for clinicians.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!