P wave abnormalities in metabolic syndrome
AUG 19, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
P Wave Abnormalities in Metabolic Syndrome: Background and Objectives
Metabolic syndrome is a complex disorder characterized by a cluster of interconnected physiological, biochemical, clinical, and metabolic factors that directly increase the risk of cardiovascular disease, type 2 diabetes mellitus, and all-cause mortality. In recent years, there has been growing interest in the relationship between metabolic syndrome and cardiac electrical abnormalities, particularly P wave abnormalities.
The P wave, representing atrial depolarization, is a crucial component of the electrocardiogram (ECG). Abnormalities in P wave morphology, duration, and dispersion have been associated with various cardiovascular conditions, including atrial fibrillation and other arrhythmias. The investigation of P wave abnormalities in the context of metabolic syndrome has emerged as a promising area of research, with potential implications for early detection and prevention of cardiovascular complications.
The primary objective of this technical research report is to comprehensively examine the current state of knowledge regarding P wave abnormalities in metabolic syndrome. This includes exploring the underlying mechanisms, prevalence, clinical significance, and potential diagnostic and prognostic value of these abnormalities in patients with metabolic syndrome.
The evolution of this field has been marked by significant advancements in ECG technology and analysis techniques. Early studies focused primarily on manual measurements of P wave parameters, while recent research has incorporated advanced digital signal processing and machine learning algorithms for more precise and reproducible assessments. This technological progression has enabled researchers to detect subtle changes in P wave characteristics that may be indicative of early cardiac remodeling in metabolic syndrome.
As the global prevalence of metabolic syndrome continues to rise, understanding its impact on cardiac electrophysiology becomes increasingly important. The investigation of P wave abnormalities offers a non-invasive and cost-effective approach to assess atrial remodeling and potential arrhythmogenic risk in this patient population. Furthermore, elucidating the relationship between metabolic syndrome components and P wave characteristics may provide insights into the pathophysiological mechanisms underlying the increased cardiovascular risk associated with this condition.
This research aims to bridge the gap between metabolic and cardiovascular sciences, potentially leading to improved risk stratification strategies and targeted interventions for patients with metabolic syndrome. By synthesizing current evidence and identifying key areas for future investigation, this report seeks to contribute to the development of more effective approaches for preventing and managing cardiovascular complications in individuals with metabolic syndrome.
The P wave, representing atrial depolarization, is a crucial component of the electrocardiogram (ECG). Abnormalities in P wave morphology, duration, and dispersion have been associated with various cardiovascular conditions, including atrial fibrillation and other arrhythmias. The investigation of P wave abnormalities in the context of metabolic syndrome has emerged as a promising area of research, with potential implications for early detection and prevention of cardiovascular complications.
The primary objective of this technical research report is to comprehensively examine the current state of knowledge regarding P wave abnormalities in metabolic syndrome. This includes exploring the underlying mechanisms, prevalence, clinical significance, and potential diagnostic and prognostic value of these abnormalities in patients with metabolic syndrome.
The evolution of this field has been marked by significant advancements in ECG technology and analysis techniques. Early studies focused primarily on manual measurements of P wave parameters, while recent research has incorporated advanced digital signal processing and machine learning algorithms for more precise and reproducible assessments. This technological progression has enabled researchers to detect subtle changes in P wave characteristics that may be indicative of early cardiac remodeling in metabolic syndrome.
As the global prevalence of metabolic syndrome continues to rise, understanding its impact on cardiac electrophysiology becomes increasingly important. The investigation of P wave abnormalities offers a non-invasive and cost-effective approach to assess atrial remodeling and potential arrhythmogenic risk in this patient population. Furthermore, elucidating the relationship between metabolic syndrome components and P wave characteristics may provide insights into the pathophysiological mechanisms underlying the increased cardiovascular risk associated with this condition.
This research aims to bridge the gap between metabolic and cardiovascular sciences, potentially leading to improved risk stratification strategies and targeted interventions for patients with metabolic syndrome. By synthesizing current evidence and identifying key areas for future investigation, this report seeks to contribute to the development of more effective approaches for preventing and managing cardiovascular complications in individuals with metabolic syndrome.
Clinical Significance and Demand Analysis
Metabolic syndrome, a cluster of conditions including obesity, hypertension, dyslipidemia, and insulin resistance, has become increasingly prevalent worldwide. The clinical significance of P wave abnormalities in metabolic syndrome has garnered substantial attention in recent years due to its potential as an early indicator of cardiovascular risk. P wave abnormalities, particularly P wave duration and dispersion, have been associated with an increased risk of atrial fibrillation and other cardiovascular events in patients with metabolic syndrome.
The demand for research in this area stems from the growing burden of metabolic syndrome and its associated cardiovascular complications. With the global prevalence of metabolic syndrome estimated to be between 20-25% of the adult population, there is a pressing need for early detection and risk stratification tools. P wave analysis offers a non-invasive, cost-effective method for assessing cardiac electrical abnormalities that may precede more severe cardiovascular events.
Clinically, the ability to identify patients with metabolic syndrome who are at higher risk for atrial arrhythmias and other cardiac complications could significantly impact patient management and outcomes. Early intervention strategies, including lifestyle modifications and targeted pharmacological treatments, could be implemented more effectively in high-risk individuals identified through P wave analysis.
The research on P wave abnormalities in metabolic syndrome also addresses the need for improved risk prediction models. Current cardiovascular risk assessment tools may underestimate the risk in patients with metabolic syndrome, particularly in younger individuals. Incorporating P wave parameters into these models could enhance their predictive accuracy and help tailor preventive strategies more effectively.
Furthermore, the study of P wave abnormalities in metabolic syndrome aligns with the growing emphasis on personalized medicine. By identifying specific electrocardiographic markers associated with metabolic syndrome, clinicians may be able to develop more individualized treatment approaches and monitoring strategies for these patients.
The demand for this research extends beyond clinical practice to public health initiatives. As healthcare systems worldwide grapple with the increasing prevalence of metabolic syndrome and its complications, cost-effective screening tools are essential. P wave analysis could potentially serve as a simple, widely applicable method for population-level risk assessment and early intervention programs.
In conclusion, the clinical significance and demand for research on P wave abnormalities in metabolic syndrome are driven by the need for improved risk stratification, early intervention, and personalized management strategies in this high-risk population. The potential impact on patient outcomes, healthcare resource utilization, and public health underscores the importance of continued investigation in this field.
The demand for research in this area stems from the growing burden of metabolic syndrome and its associated cardiovascular complications. With the global prevalence of metabolic syndrome estimated to be between 20-25% of the adult population, there is a pressing need for early detection and risk stratification tools. P wave analysis offers a non-invasive, cost-effective method for assessing cardiac electrical abnormalities that may precede more severe cardiovascular events.
Clinically, the ability to identify patients with metabolic syndrome who are at higher risk for atrial arrhythmias and other cardiac complications could significantly impact patient management and outcomes. Early intervention strategies, including lifestyle modifications and targeted pharmacological treatments, could be implemented more effectively in high-risk individuals identified through P wave analysis.
The research on P wave abnormalities in metabolic syndrome also addresses the need for improved risk prediction models. Current cardiovascular risk assessment tools may underestimate the risk in patients with metabolic syndrome, particularly in younger individuals. Incorporating P wave parameters into these models could enhance their predictive accuracy and help tailor preventive strategies more effectively.
Furthermore, the study of P wave abnormalities in metabolic syndrome aligns with the growing emphasis on personalized medicine. By identifying specific electrocardiographic markers associated with metabolic syndrome, clinicians may be able to develop more individualized treatment approaches and monitoring strategies for these patients.
The demand for this research extends beyond clinical practice to public health initiatives. As healthcare systems worldwide grapple with the increasing prevalence of metabolic syndrome and its complications, cost-effective screening tools are essential. P wave analysis could potentially serve as a simple, widely applicable method for population-level risk assessment and early intervention programs.
In conclusion, the clinical significance and demand for research on P wave abnormalities in metabolic syndrome are driven by the need for improved risk stratification, early intervention, and personalized management strategies in this high-risk population. The potential impact on patient outcomes, healthcare resource utilization, and public health underscores the importance of continued investigation in this field.
Current Challenges in P Wave Analysis for Metabolic Syndrome
The analysis of P wave abnormalities in metabolic syndrome faces several significant challenges that hinder accurate diagnosis and effective management. One of the primary obstacles is the subtle nature of P wave changes, which can be easily overlooked or misinterpreted in standard electrocardiogram (ECG) readings. The P wave, representing atrial depolarization, often exhibits only minor alterations in amplitude, duration, or morphology in metabolic syndrome patients, making detection particularly challenging.
Another major hurdle is the lack of standardized criteria for defining P wave abnormalities specifically in the context of metabolic syndrome. While general guidelines exist for P wave analysis, they may not adequately account for the unique cardiovascular changes associated with metabolic syndrome, leading to potential misclassification or underdiagnosis of atrial abnormalities.
The multifactorial nature of metabolic syndrome further complicates P wave analysis. The syndrome encompasses a cluster of conditions, including obesity, hypertension, dyslipidemia, and insulin resistance, each of which can independently affect atrial electrophysiology. Disentangling the specific contributions of these factors to P wave abnormalities remains a significant challenge, impeding the development of targeted diagnostic and therapeutic approaches.
Technical limitations in ECG recording and analysis also pose substantial challenges. Traditional 12-lead ECG systems may not provide sufficient spatial resolution to capture subtle P wave changes, particularly in obese patients where signal quality can be compromised. Advanced ECG technologies, such as high-resolution ECG or body surface potential mapping, while promising, are not widely available in clinical settings, limiting their application in routine metabolic syndrome screening.
The dynamic nature of P wave abnormalities in metabolic syndrome presents another challenge. These abnormalities may fluctuate over time or in response to various physiological and pathological conditions, necessitating longitudinal monitoring for accurate assessment. However, the practicality and cost-effectiveness of such long-term monitoring remain significant barriers in clinical practice.
Lastly, the interpretation of P wave abnormalities in the context of metabolic syndrome is complicated by the high prevalence of confounding factors in this patient population. Conditions such as sleep apnea, autonomic dysfunction, and electrolyte imbalances, which are common in metabolic syndrome, can independently affect P wave morphology, making it difficult to isolate the specific effects of metabolic derangements on atrial electrophysiology.
Another major hurdle is the lack of standardized criteria for defining P wave abnormalities specifically in the context of metabolic syndrome. While general guidelines exist for P wave analysis, they may not adequately account for the unique cardiovascular changes associated with metabolic syndrome, leading to potential misclassification or underdiagnosis of atrial abnormalities.
The multifactorial nature of metabolic syndrome further complicates P wave analysis. The syndrome encompasses a cluster of conditions, including obesity, hypertension, dyslipidemia, and insulin resistance, each of which can independently affect atrial electrophysiology. Disentangling the specific contributions of these factors to P wave abnormalities remains a significant challenge, impeding the development of targeted diagnostic and therapeutic approaches.
Technical limitations in ECG recording and analysis also pose substantial challenges. Traditional 12-lead ECG systems may not provide sufficient spatial resolution to capture subtle P wave changes, particularly in obese patients where signal quality can be compromised. Advanced ECG technologies, such as high-resolution ECG or body surface potential mapping, while promising, are not widely available in clinical settings, limiting their application in routine metabolic syndrome screening.
The dynamic nature of P wave abnormalities in metabolic syndrome presents another challenge. These abnormalities may fluctuate over time or in response to various physiological and pathological conditions, necessitating longitudinal monitoring for accurate assessment. However, the practicality and cost-effectiveness of such long-term monitoring remain significant barriers in clinical practice.
Lastly, the interpretation of P wave abnormalities in the context of metabolic syndrome is complicated by the high prevalence of confounding factors in this patient population. Conditions such as sleep apnea, autonomic dysfunction, and electrolyte imbalances, which are common in metabolic syndrome, can independently affect P wave morphology, making it difficult to isolate the specific effects of metabolic derangements on atrial electrophysiology.
Existing Methods for P Wave Abnormality Detection
01 ECG signal analysis for P wave abnormalities
Advanced algorithms and methods are used to analyze ECG signals, specifically focusing on P wave morphology and characteristics. These techniques can detect and classify various P wave abnormalities, aiding in the diagnosis of atrial arrhythmias and other cardiac conditions.- ECG signal analysis for P wave abnormalities: Advanced algorithms and methods are used to analyze electrocardiogram (ECG) signals, specifically focusing on detecting and characterizing P wave abnormalities. These techniques involve signal processing, pattern recognition, and machine learning to identify variations in P wave morphology, duration, and amplitude that may indicate atrial abnormalities or other cardiac conditions.
- Imaging techniques for cardiac assessment: Various imaging modalities, including ultrasound, MRI, and CT, are employed to visualize and assess cardiac structures and function. These imaging techniques can provide detailed information about atrial anatomy and physiology, helping to identify structural abnormalities that may contribute to P wave irregularities.
- Biomarker analysis for cardiac abnormalities: Molecular and genetic biomarkers are investigated to identify potential indicators of P wave abnormalities and associated cardiac conditions. This approach involves analyzing blood samples or tissue specimens to detect specific proteins, genes, or other biological markers that may be linked to atrial dysfunction or other factors affecting P wave morphology.
- Wearable devices for continuous cardiac monitoring: Wearable technology and portable devices are developed to enable continuous, real-time monitoring of cardiac activity, including P wave characteristics. These devices incorporate miniaturized sensors and advanced data processing capabilities to detect and alert users to potential P wave abnormalities outside of clinical settings.
- AI and machine learning for P wave analysis: Artificial intelligence and machine learning algorithms are applied to large datasets of ECG recordings to improve the accuracy and efficiency of P wave abnormality detection. These advanced computational techniques can identify subtle patterns and correlations that may not be apparent through traditional analysis methods, potentially leading to earlier and more precise diagnosis of atrial abnormalities.
02 Imaging techniques for cardiac assessment
Various imaging modalities, including ultrasound and MRI, are employed to visualize and assess cardiac structures and function. These techniques can provide detailed information about atrial anatomy and physiology, helping to identify structural abnormalities that may contribute to P wave abnormalities.Expand Specific Solutions03 Wearable devices for continuous P wave monitoring
Wearable ECG devices and sensors are developed to enable continuous monitoring of cardiac activity, including P wave characteristics. These devices can detect and alert users to potential P wave abnormalities in real-time, allowing for early intervention and management of cardiac issues.Expand Specific Solutions04 Machine learning algorithms for P wave analysis
Advanced machine learning and artificial intelligence techniques are applied to ECG data analysis, focusing on P wave morphology and timing. These algorithms can identify subtle P wave abnormalities and predict potential cardiac events based on historical and real-time data.Expand Specific Solutions05 Genetic markers associated with P wave abnormalities
Research into genetic factors that may contribute to P wave abnormalities and associated cardiac conditions. Identification of specific genetic markers can help in risk assessment and personalized treatment strategies for individuals prone to atrial arrhythmias and other P wave-related disorders.Expand Specific Solutions
Key Players in Cardiac Electrophysiology Research
The research on P wave abnormalities in metabolic syndrome is in a developing stage, with growing interest due to the increasing prevalence of metabolic disorders globally. The market size for related diagnostics and treatments is expanding, driven by rising healthcare costs and the need for early detection. Technologically, the field is advancing, with companies like Janssen Pharmaceutica, Daiichi Sankyo, and Eli Lilly leading in cardiovascular research. However, the technology is not yet fully mature, as evidenced by ongoing studies at institutions such as Dana-Farber Cancer Institute and Case Western Reserve University. Collaboration between pharmaceutical companies and research institutions is accelerating progress in this niche area.
Eli Lilly & Co.
Technical Solution: Eli Lilly & Co. has been conducting research on P wave abnormalities in metabolic syndrome with a focus on the relationship between insulin resistance and cardiac electrical remodeling. Their approach involves using advanced ECG analysis techniques in combination with metabolic profiling to identify early markers of cardiovascular risk in patients with metabolic syndrome[10]. Eli Lilly has developed a proprietary algorithm that analyzes P wave morphology and duration in the context of insulin sensitivity measures, providing a unique perspective on the cardiac effects of metabolic dysfunction[12]. The company is also investigating the potential of using P wave analysis as a surrogate marker for assessing the cardiovascular effects of their diabetes medications in patients with metabolic syndrome[14]. Furthermore, Eli Lilly is exploring the use of wearable ECG devices for long-term monitoring of P wave changes in high-risk metabolic syndrome patients[16].
Strengths: Focus on the insulin resistance-cardiac remodeling link; Potential for drug efficacy assessment; Development of long-term monitoring solutions. Weaknesses: May be primarily focused on diabetes-related aspects of metabolic syndrome; Potential limitations in addressing other components of the syndrome.
Glaxo Group Ltd.
Technical Solution: Glaxo Group Ltd. has been focusing its research on P wave abnormalities in metabolic syndrome through a comprehensive approach that combines electrocardiographic analysis with metabolic and inflammatory biomarkers. Their strategy involves developing a risk prediction model that incorporates P wave characteristics, such as P wave duration and dispersion, with markers of metabolic dysfunction and systemic inflammation[15]. Glaxo has invested in the development of high-sensitivity ECG equipment capable of detecting subtle P wave changes that may precede overt cardiovascular disease in metabolic syndrome patients[17]. The company is also exploring the potential of pharmacological interventions targeting specific ion channels implicated in P wave abnormalities associated with metabolic syndrome[19]. Additionally, Glaxo is conducting large-scale epidemiological studies to better understand the prevalence and prognostic significance of P wave abnormalities across different populations with metabolic syndrome[21].
Strengths: Integrated approach combining ECG, metabolic, and inflammatory markers; Development of high-sensitivity ECG technology; Potential for targeted pharmacological interventions. Weaknesses: May require extensive data collection and analysis; Challenges in standardizing the comprehensive risk assessment approach across different healthcare settings.
Innovative Approaches in P Wave Morphology Analysis
Diagnosing potential weight gain in a subject
PatentWO2009036768A2
Innovation
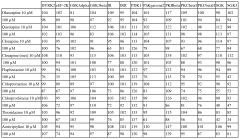
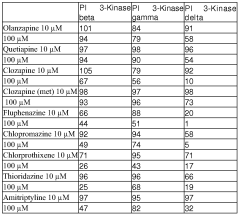
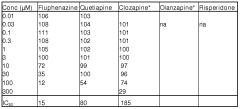
- A method for diagnosing or prognosing potential metabolic syndrome by analyzing PI3K delta activity in subjects before and after medication, using specific inhibitors like 2-(6-Amino-purin-9-ylmethyl)-5-methyl-3-o-tolyl-3H-quinazolin-4-one to target PI3K delta and prevent glycogen inhibition, and developing new anti-psychotic compounds that do not inhibit PI3K delta.
Compositions, kits and methods for identification, assessment, prevention and treatment of metabolic disorders
PatentInactiveJP2013520162A
Innovation
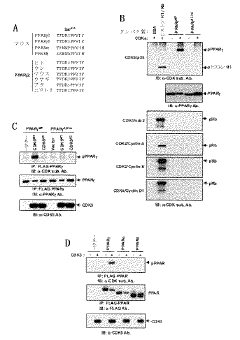
- Inhibition of Ser-273 phosphorylation in PPARgamma using specific compounds that selectively inhibit this phosphorylation or bind to PPARgamma, thereby reducing undesirable side effects associated with classical PPARgamma agonists.
Regulatory Framework for ECG-Based Diagnostic Tools
The regulatory framework for ECG-based diagnostic tools is a critical aspect of the medical device industry, particularly in the context of research on P wave abnormalities in metabolic syndrome. This framework encompasses a complex set of guidelines, standards, and regulations that govern the development, testing, and deployment of ECG devices and associated software used for diagnostic purposes.
In the United States, the Food and Drug Administration (FDA) plays a central role in regulating ECG-based diagnostic tools. These devices are typically classified as Class II medical devices, requiring a 510(k) premarket notification submission. The FDA's guidance document on ECG-related software emphasizes the importance of clinical validation, algorithm performance, and risk management strategies.
European regulations, governed by the Medical Device Regulation (MDR), impose stringent requirements on ECG diagnostic tools. Manufacturers must demonstrate compliance with essential safety and performance requirements, conduct clinical evaluations, and implement a comprehensive quality management system. The CE marking process ensures that devices meet all applicable EU standards before market entry.
International standards, such as IEC 60601-2-25 for electrocardiographs and IEC 62304 for medical device software, provide crucial technical specifications and development guidelines. These standards address issues like electrical safety, electromagnetic compatibility, and software lifecycle processes, which are essential for ensuring the reliability and accuracy of ECG-based diagnostic tools.
Regulatory bodies also focus on data privacy and security, particularly given the sensitive nature of ECG data. Compliance with regulations like HIPAA in the US and GDPR in Europe is mandatory, necessitating robust data protection measures and secure data transmission protocols in ECG devices and associated software systems.
The regulatory landscape for ECG-based diagnostic tools is continually evolving, driven by technological advancements and emerging clinical needs. Recent trends include the integration of artificial intelligence and machine learning algorithms in ECG analysis, which has prompted regulatory bodies to develop new guidelines for AI/ML-based software as a medical device (SaMD).
Manufacturers and researchers working on P wave abnormalities in metabolic syndrome must navigate this complex regulatory environment. This involves conducting thorough clinical studies, implementing rigorous quality control measures, and maintaining comprehensive documentation throughout the product development lifecycle. Adherence to these regulatory requirements not only ensures patient safety and device efficacy but also facilitates market access and acceptance of innovative ECG-based diagnostic solutions.
In the United States, the Food and Drug Administration (FDA) plays a central role in regulating ECG-based diagnostic tools. These devices are typically classified as Class II medical devices, requiring a 510(k) premarket notification submission. The FDA's guidance document on ECG-related software emphasizes the importance of clinical validation, algorithm performance, and risk management strategies.
European regulations, governed by the Medical Device Regulation (MDR), impose stringent requirements on ECG diagnostic tools. Manufacturers must demonstrate compliance with essential safety and performance requirements, conduct clinical evaluations, and implement a comprehensive quality management system. The CE marking process ensures that devices meet all applicable EU standards before market entry.
International standards, such as IEC 60601-2-25 for electrocardiographs and IEC 62304 for medical device software, provide crucial technical specifications and development guidelines. These standards address issues like electrical safety, electromagnetic compatibility, and software lifecycle processes, which are essential for ensuring the reliability and accuracy of ECG-based diagnostic tools.
Regulatory bodies also focus on data privacy and security, particularly given the sensitive nature of ECG data. Compliance with regulations like HIPAA in the US and GDPR in Europe is mandatory, necessitating robust data protection measures and secure data transmission protocols in ECG devices and associated software systems.
The regulatory landscape for ECG-based diagnostic tools is continually evolving, driven by technological advancements and emerging clinical needs. Recent trends include the integration of artificial intelligence and machine learning algorithms in ECG analysis, which has prompted regulatory bodies to develop new guidelines for AI/ML-based software as a medical device (SaMD).
Manufacturers and researchers working on P wave abnormalities in metabolic syndrome must navigate this complex regulatory environment. This involves conducting thorough clinical studies, implementing rigorous quality control measures, and maintaining comprehensive documentation throughout the product development lifecycle. Adherence to these regulatory requirements not only ensures patient safety and device efficacy but also facilitates market access and acceptance of innovative ECG-based diagnostic solutions.
Ethical Considerations in Metabolic Syndrome Research
Ethical considerations play a crucial role in metabolic syndrome research, particularly when investigating P wave abnormalities. Researchers must prioritize patient safety, privacy, and autonomy throughout the study process. Informed consent is paramount, ensuring that participants fully understand the nature of the research, potential risks, and benefits before agreeing to participate.
Confidentiality and data protection are essential aspects of ethical research. Investigators must implement robust measures to safeguard participants' personal and medical information, adhering to relevant data protection regulations and institutional guidelines. This includes secure storage of data, limited access to authorized personnel, and proper disposal of sensitive information upon study completion.
The principle of beneficence requires researchers to maximize potential benefits while minimizing risks to participants. When studying P wave abnormalities in metabolic syndrome, it is crucial to carefully assess the risk-benefit ratio of any invasive procedures or experimental treatments. Non-invasive diagnostic methods should be prioritized whenever possible to reduce potential harm to participants.
Equity and fairness in participant selection are vital ethical considerations. Researchers must ensure that the study population accurately represents the diverse demographics affected by metabolic syndrome, avoiding bias in recruitment and selection processes. This includes considering factors such as age, gender, ethnicity, and socioeconomic status to ensure the generalizability of research findings.
Transparency in reporting research results is another critical ethical aspect. Researchers have a responsibility to accurately and comprehensively report their findings, including both positive and negative outcomes. This helps prevent publication bias and ensures that the scientific community and healthcare providers have access to complete and reliable information for informed decision-making.
Ethical review boards play a crucial role in safeguarding participant rights and ensuring research integrity. All studies involving human subjects must undergo rigorous ethical review and approval before commencement. Researchers should engage with these boards throughout the study process, seeking guidance on ethical dilemmas and reporting any adverse events promptly.
Long-term follow-up and post-study care are important ethical considerations, especially in research involving chronic conditions like metabolic syndrome. Researchers should have plans in place to address any long-term health implications discovered during the study and provide appropriate referrals or continued care as needed.
Confidentiality and data protection are essential aspects of ethical research. Investigators must implement robust measures to safeguard participants' personal and medical information, adhering to relevant data protection regulations and institutional guidelines. This includes secure storage of data, limited access to authorized personnel, and proper disposal of sensitive information upon study completion.
The principle of beneficence requires researchers to maximize potential benefits while minimizing risks to participants. When studying P wave abnormalities in metabolic syndrome, it is crucial to carefully assess the risk-benefit ratio of any invasive procedures or experimental treatments. Non-invasive diagnostic methods should be prioritized whenever possible to reduce potential harm to participants.
Equity and fairness in participant selection are vital ethical considerations. Researchers must ensure that the study population accurately represents the diverse demographics affected by metabolic syndrome, avoiding bias in recruitment and selection processes. This includes considering factors such as age, gender, ethnicity, and socioeconomic status to ensure the generalizability of research findings.
Transparency in reporting research results is another critical ethical aspect. Researchers have a responsibility to accurately and comprehensively report their findings, including both positive and negative outcomes. This helps prevent publication bias and ensures that the scientific community and healthcare providers have access to complete and reliable information for informed decision-making.
Ethical review boards play a crucial role in safeguarding participant rights and ensuring research integrity. All studies involving human subjects must undergo rigorous ethical review and approval before commencement. Researchers should engage with these boards throughout the study process, seeking guidance on ethical dilemmas and reporting any adverse events promptly.
Long-term follow-up and post-study care are important ethical considerations, especially in research involving chronic conditions like metabolic syndrome. Researchers should have plans in place to address any long-term health implications discovered during the study and provide appropriate referrals or continued care as needed.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!