P wave considerations in assessing diastolic dysfunction
AUG 19, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
P Wave Analysis Background and Objectives
P wave analysis has emerged as a crucial component in the assessment of diastolic dysfunction, representing a significant advancement in cardiac diagnostics. The P wave, which corresponds to atrial depolarization in the cardiac cycle, provides valuable insights into atrial function and structure. This analysis has gained prominence due to its potential to offer early indicators of diastolic dysfunction, a condition characterized by impaired relaxation and filling of the left ventricle during diastole.
The primary objective of P wave analysis in the context of diastolic dysfunction is to enhance the accuracy and early detection of this cardiac abnormality. By scrutinizing the morphology, duration, and amplitude of the P wave, clinicians aim to identify subtle changes that may precede more overt signs of diastolic dysfunction. This approach aligns with the growing emphasis on preventive cardiology and the need for more sensitive diagnostic tools.
Historically, the assessment of diastolic function has relied heavily on echocardiographic parameters. However, the integration of P wave analysis into this diagnostic paradigm represents a shift towards a more comprehensive evaluation. This evolution in cardiac diagnostics reflects the increasing recognition of the atria's role in overall cardiac performance and the complex interplay between atrial and ventricular function.
The technological advancements in electrocardiography have significantly contributed to the refinement of P wave analysis techniques. High-resolution ECG systems and sophisticated signal processing algorithms have enabled the extraction of more detailed information from the P wave, including subtle variations that were previously undetectable. These technological improvements have opened new avenues for research and clinical applications in the field of diastolic dysfunction assessment.
One of the key objectives in P wave analysis is to establish standardized criteria for interpreting P wave characteristics in the context of diastolic dysfunction. This standardization is crucial for ensuring consistency in diagnosis across different clinical settings and for facilitating comparative studies. Researchers are working towards developing robust algorithms that can automatically analyze P wave features and correlate them with various stages of diastolic dysfunction.
Another important goal is to integrate P wave analysis with other diagnostic modalities to create a more comprehensive assessment of cardiac function. This multi-modal approach aims to combine the strengths of different diagnostic techniques, potentially leading to earlier and more accurate detection of diastolic dysfunction. The synergy between P wave analysis and traditional echocardiographic parameters holds promise for improving risk stratification and guiding therapeutic interventions in patients with suspected or confirmed diastolic dysfunction.
The primary objective of P wave analysis in the context of diastolic dysfunction is to enhance the accuracy and early detection of this cardiac abnormality. By scrutinizing the morphology, duration, and amplitude of the P wave, clinicians aim to identify subtle changes that may precede more overt signs of diastolic dysfunction. This approach aligns with the growing emphasis on preventive cardiology and the need for more sensitive diagnostic tools.
Historically, the assessment of diastolic function has relied heavily on echocardiographic parameters. However, the integration of P wave analysis into this diagnostic paradigm represents a shift towards a more comprehensive evaluation. This evolution in cardiac diagnostics reflects the increasing recognition of the atria's role in overall cardiac performance and the complex interplay between atrial and ventricular function.
The technological advancements in electrocardiography have significantly contributed to the refinement of P wave analysis techniques. High-resolution ECG systems and sophisticated signal processing algorithms have enabled the extraction of more detailed information from the P wave, including subtle variations that were previously undetectable. These technological improvements have opened new avenues for research and clinical applications in the field of diastolic dysfunction assessment.
One of the key objectives in P wave analysis is to establish standardized criteria for interpreting P wave characteristics in the context of diastolic dysfunction. This standardization is crucial for ensuring consistency in diagnosis across different clinical settings and for facilitating comparative studies. Researchers are working towards developing robust algorithms that can automatically analyze P wave features and correlate them with various stages of diastolic dysfunction.
Another important goal is to integrate P wave analysis with other diagnostic modalities to create a more comprehensive assessment of cardiac function. This multi-modal approach aims to combine the strengths of different diagnostic techniques, potentially leading to earlier and more accurate detection of diastolic dysfunction. The synergy between P wave analysis and traditional echocardiographic parameters holds promise for improving risk stratification and guiding therapeutic interventions in patients with suspected or confirmed diastolic dysfunction.
Clinical Demand for Diastolic Dysfunction Assessment
The clinical demand for accurate assessment of diastolic dysfunction has grown significantly in recent years, driven by the increasing prevalence of heart failure with preserved ejection fraction (HFpEF) and the recognition of diastolic dysfunction as a precursor to more severe cardiac conditions. Diastolic dysfunction, characterized by impaired relaxation and filling of the left ventricle, affects a substantial portion of the population, particularly older adults and those with hypertension, diabetes, or coronary artery disease.
The importance of early detection and management of diastolic dysfunction cannot be overstated. It is often asymptomatic in its early stages, making it challenging to diagnose without specific cardiac assessments. As the condition progresses, it can lead to heart failure, reduced quality of life, and increased mortality rates. This underscores the critical need for reliable and accessible diagnostic tools that can identify diastolic dysfunction in its initial phases.
Current diagnostic methods for diastolic dysfunction primarily rely on echocardiography, which provides valuable information about cardiac structure and function. However, the interpretation of echocardiographic data can be complex and subjective, leading to potential inconsistencies in diagnosis. This has created a demand for more objective and standardized assessment techniques, particularly those that can be easily integrated into routine clinical practice.
The incorporation of P wave analysis in the assessment of diastolic dysfunction represents a promising avenue for enhancing diagnostic accuracy. The P wave, which represents atrial depolarization, can provide insights into left atrial pressure and function, both of which are closely related to diastolic performance. By analyzing P wave characteristics such as duration, amplitude, and morphology, clinicians may be able to detect subtle changes indicative of early diastolic dysfunction.
There is a growing interest in developing non-invasive, cost-effective, and widely accessible methods for diastolic dysfunction assessment. This is particularly important in primary care settings, where early identification of at-risk patients can lead to timely interventions and improved outcomes. The potential for P wave analysis to be performed using standard electrocardiograms (ECGs) makes it an attractive option for widespread clinical implementation.
Furthermore, the integration of P wave analysis with other diagnostic modalities, such as biomarkers and imaging techniques, could provide a more comprehensive evaluation of cardiac function. This multi-modal approach aligns with the trend towards personalized medicine, allowing for tailored management strategies based on individual patient characteristics and risk profiles.
As the population ages and the burden of cardiovascular disease continues to grow, the demand for innovative approaches to diastolic dysfunction assessment is expected to increase. Healthcare systems are seeking solutions that can improve diagnostic accuracy, streamline patient care pathways, and ultimately reduce the morbidity and mortality associated with diastolic dysfunction and its sequelae.
The importance of early detection and management of diastolic dysfunction cannot be overstated. It is often asymptomatic in its early stages, making it challenging to diagnose without specific cardiac assessments. As the condition progresses, it can lead to heart failure, reduced quality of life, and increased mortality rates. This underscores the critical need for reliable and accessible diagnostic tools that can identify diastolic dysfunction in its initial phases.
Current diagnostic methods for diastolic dysfunction primarily rely on echocardiography, which provides valuable information about cardiac structure and function. However, the interpretation of echocardiographic data can be complex and subjective, leading to potential inconsistencies in diagnosis. This has created a demand for more objective and standardized assessment techniques, particularly those that can be easily integrated into routine clinical practice.
The incorporation of P wave analysis in the assessment of diastolic dysfunction represents a promising avenue for enhancing diagnostic accuracy. The P wave, which represents atrial depolarization, can provide insights into left atrial pressure and function, both of which are closely related to diastolic performance. By analyzing P wave characteristics such as duration, amplitude, and morphology, clinicians may be able to detect subtle changes indicative of early diastolic dysfunction.
There is a growing interest in developing non-invasive, cost-effective, and widely accessible methods for diastolic dysfunction assessment. This is particularly important in primary care settings, where early identification of at-risk patients can lead to timely interventions and improved outcomes. The potential for P wave analysis to be performed using standard electrocardiograms (ECGs) makes it an attractive option for widespread clinical implementation.
Furthermore, the integration of P wave analysis with other diagnostic modalities, such as biomarkers and imaging techniques, could provide a more comprehensive evaluation of cardiac function. This multi-modal approach aligns with the trend towards personalized medicine, allowing for tailored management strategies based on individual patient characteristics and risk profiles.
As the population ages and the burden of cardiovascular disease continues to grow, the demand for innovative approaches to diastolic dysfunction assessment is expected to increase. Healthcare systems are seeking solutions that can improve diagnostic accuracy, streamline patient care pathways, and ultimately reduce the morbidity and mortality associated with diastolic dysfunction and its sequelae.
Current Challenges in P Wave Interpretation
The interpretation of P waves in assessing diastolic dysfunction presents several significant challenges that hinder accurate diagnosis and patient management. One primary obstacle is the variability in P wave morphology among individuals, which can make it difficult to establish standardized criteria for abnormality. This variability is influenced by factors such as age, body habitus, and underlying cardiac conditions, further complicating the interpretation process.
Another challenge lies in the subtle nature of P wave changes associated with diastolic dysfunction. These alterations can be easily overlooked or misinterpreted, especially in the presence of other ECG abnormalities or artifacts. The low amplitude of P waves compared to other ECG components also contributes to the difficulty in accurately measuring and analyzing their characteristics.
The lack of consensus on specific P wave parameters that definitively indicate diastolic dysfunction poses an additional hurdle. While various indices such as P wave duration, amplitude, and dispersion have been proposed, there is ongoing debate regarding their sensitivity and specificity in diagnosing diastolic dysfunction. This uncertainty can lead to inconsistencies in clinical practice and research methodologies.
Furthermore, the dynamic nature of diastolic function presents a challenge in P wave interpretation. Diastolic function can vary with physiological states, such as exercise or changes in loading conditions, making it difficult to capture and interpret P wave changes in a single ECG recording. This variability necessitates the consideration of multiple ECG recordings or the integration of other diagnostic modalities for a comprehensive assessment.
The influence of concurrent cardiac conditions on P wave morphology also complicates interpretation. Conditions such as left atrial enlargement, atrial fibrosis, or electrolyte imbalances can alter P wave characteristics independently of diastolic dysfunction, making it challenging to isolate the specific effects of diastolic abnormalities on the P wave.
Additionally, the limited spatial resolution of surface ECG recordings in capturing atrial electrical activity presents a technical challenge. The P wave represents a summation of electrical activity from both atria, making it difficult to discern regional differences in atrial activation that may be indicative of localized diastolic dysfunction.
Lastly, the integration of P wave analysis with other ECG parameters and imaging modalities in the assessment of diastolic dysfunction remains a complex task. Developing a comprehensive approach that combines P wave characteristics with other diagnostic tools requires further research and standardization to enhance the accuracy and reliability of diastolic dysfunction diagnosis.
Another challenge lies in the subtle nature of P wave changes associated with diastolic dysfunction. These alterations can be easily overlooked or misinterpreted, especially in the presence of other ECG abnormalities or artifacts. The low amplitude of P waves compared to other ECG components also contributes to the difficulty in accurately measuring and analyzing their characteristics.
The lack of consensus on specific P wave parameters that definitively indicate diastolic dysfunction poses an additional hurdle. While various indices such as P wave duration, amplitude, and dispersion have been proposed, there is ongoing debate regarding their sensitivity and specificity in diagnosing diastolic dysfunction. This uncertainty can lead to inconsistencies in clinical practice and research methodologies.
Furthermore, the dynamic nature of diastolic function presents a challenge in P wave interpretation. Diastolic function can vary with physiological states, such as exercise or changes in loading conditions, making it difficult to capture and interpret P wave changes in a single ECG recording. This variability necessitates the consideration of multiple ECG recordings or the integration of other diagnostic modalities for a comprehensive assessment.
The influence of concurrent cardiac conditions on P wave morphology also complicates interpretation. Conditions such as left atrial enlargement, atrial fibrosis, or electrolyte imbalances can alter P wave characteristics independently of diastolic dysfunction, making it challenging to isolate the specific effects of diastolic abnormalities on the P wave.
Additionally, the limited spatial resolution of surface ECG recordings in capturing atrial electrical activity presents a technical challenge. The P wave represents a summation of electrical activity from both atria, making it difficult to discern regional differences in atrial activation that may be indicative of localized diastolic dysfunction.
Lastly, the integration of P wave analysis with other ECG parameters and imaging modalities in the assessment of diastolic dysfunction remains a complex task. Developing a comprehensive approach that combines P wave characteristics with other diagnostic tools requires further research and standardization to enhance the accuracy and reliability of diastolic dysfunction diagnosis.
Existing P Wave Assessment Methods
01 Diagnosis of diastolic dysfunction using P wave analysis
P wave analysis can be used to diagnose diastolic dysfunction. This method involves examining the characteristics of the P wave in electrocardiograms (ECGs) to identify abnormalities associated with impaired left ventricular relaxation and filling. The shape, duration, and amplitude of the P wave can provide valuable information about atrial function and pressure, which are often affected in diastolic dysfunction.- Diagnosis of diastolic dysfunction using P wave analysis: P wave analysis can be used to diagnose diastolic dysfunction. This method involves examining the characteristics of the P wave in electrocardiograms (ECGs) to identify abnormalities associated with impaired ventricular filling. The shape, duration, and amplitude of the P wave can provide valuable information about atrial function and its relationship to diastolic dysfunction.
- Pharmacological treatment of diastolic dysfunction: Various pharmaceutical compounds can be used to treat diastolic dysfunction. These medications may target different aspects of cardiac function, such as improving myocardial relaxation, reducing ventricular stiffness, or modulating calcium handling in cardiomyocytes. The goal of these treatments is to enhance diastolic function and improve overall cardiac performance.
- Non-invasive assessment of diastolic function: Non-invasive techniques can be employed to assess diastolic function and detect P wave abnormalities. These methods may include advanced echocardiography, tissue Doppler imaging, or novel ECG analysis algorithms. Such approaches allow for early detection and monitoring of diastolic dysfunction without the need for invasive procedures.
- Genetic factors influencing diastolic dysfunction: Genetic factors may play a role in the development of diastolic dysfunction and associated P wave abnormalities. Research into genetic markers and polymorphisms can help identify individuals at higher risk for diastolic dysfunction and guide personalized treatment approaches. Understanding the genetic basis of this condition may lead to novel therapeutic targets.
- Combination therapies for managing diastolic dysfunction: Combination therapies involving multiple drugs or treatment modalities may be effective in managing diastolic dysfunction and associated P wave abnormalities. These approaches may target different pathophysiological mechanisms simultaneously, potentially leading to improved outcomes compared to monotherapy. Careful consideration of drug interactions and patient-specific factors is essential when implementing combination treatments.
02 Pharmacological treatments for diastolic dysfunction
Various pharmacological agents can be used to treat diastolic dysfunction. These may include medications that improve myocardial relaxation, reduce ventricular stiffness, or modulate neurohormonal pathways involved in heart failure. Some treatments aim to address underlying conditions such as hypertension or diabetes that contribute to diastolic dysfunction.Expand Specific Solutions03 Non-invasive assessment of diastolic function
Non-invasive techniques can be employed to assess diastolic function and detect P wave abnormalities indicative of diastolic dysfunction. These methods may include echocardiography, tissue Doppler imaging, and advanced ECG analysis. Such techniques allow for the evaluation of left ventricular filling patterns, myocardial velocities, and atrial electromechanical properties.Expand Specific Solutions04 Biomarkers for diastolic dysfunction
Specific biomarkers can be used to identify and monitor diastolic dysfunction. These may include natriuretic peptides, inflammatory markers, or other molecules associated with myocardial stress and remodeling. The use of biomarkers in conjunction with P wave analysis can enhance the accuracy of diagnosis and help guide treatment strategies.Expand Specific Solutions05 Device-based therapies for diastolic dysfunction
Various medical devices and interventions can be used to manage diastolic dysfunction and its associated P wave abnormalities. These may include implantable devices for monitoring cardiac function, pacing therapies to optimize atrial-ventricular synchrony, or novel interventional approaches to improve left ventricular compliance and filling dynamics.Expand Specific Solutions
Key Players in Cardiac Imaging and ECG Technology
The P wave considerations in assessing diastolic dysfunction represent a complex technological landscape in the mature cardiac diagnostics market. The industry is in a growth phase, with increasing demand for non-invasive and accurate diagnostic tools. Major players like Medtronic, Boston Scientific, and Philips are investing heavily in R&D to develop advanced ECG and imaging technologies. Emerging companies such as CorVista Health and Bardy Diagnostics are introducing innovative AI-driven solutions and wearable monitors, focusing on P wave analysis for improved diastolic function assessment. The market is characterized by a mix of established medical device manufacturers and agile startups, driving technological advancements and competition in this specialized field.
Koninklijke Philips NV
Technical Solution: Philips has developed a non-invasive approach to assess diastolic dysfunction using P wave analysis in combination with advanced echocardiography techniques. Their system utilizes high-resolution ECG recordings to capture detailed P wave characteristics, including duration, amplitude, and morphology[4]. This data is then integrated with echocardiographic measurements of left atrial size, mitral inflow patterns, and tissue Doppler imaging[5]. Philips' proprietary algorithms analyze these combined parameters to provide a comprehensive assessment of diastolic function. The technology also incorporates artificial intelligence to improve diagnostic accuracy and detect subtle changes in P wave characteristics that may indicate early-stage diastolic dysfunction[6].
Strengths: Non-invasive approach, integration of multiple diagnostic modalities, and AI-enhanced analysis for improved accuracy. Weaknesses: Requires specialized equipment and trained personnel for echocardiography, potential for variability in ECG electrode placement affecting P wave analysis.
CorVista Health, Inc.
Technical Solution: CorVista Health has developed a novel, non-invasive approach to assessing diastolic dysfunction using advanced signal processing of P waves combined with machine learning algorithms. Their proprietary technology, CorVista® System, utilizes a specialized sensor array to capture high-fidelity cardiac electrical signals, including detailed P wave characteristics[11]. The system analyzes multiple features of the P wave, such as duration, amplitude, and morphology, in conjunction with other ECG parameters. Advanced machine learning algorithms process this data to provide a rapid assessment of diastolic function without the need for echocardiography or other imaging modalities[12]. The technology aims to offer a quick, point-of-care solution for identifying patients at risk of diastolic dysfunction.
Strengths: Rapid, non-invasive assessment, no need for specialized imaging equipment, and potential for use in primary care settings. Weaknesses: Lack of direct hemodynamic measurements, potential for reduced accuracy compared to multi-modal imaging approaches.
Innovative P Wave Interpretation Algorithms
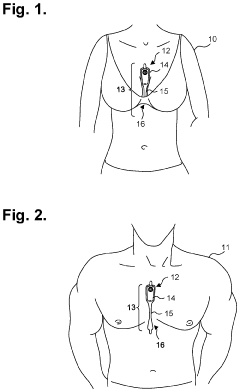
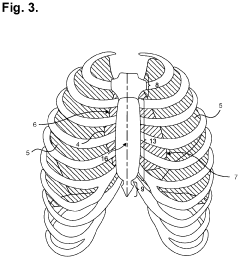
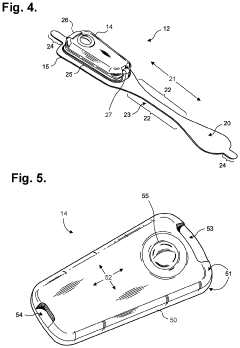
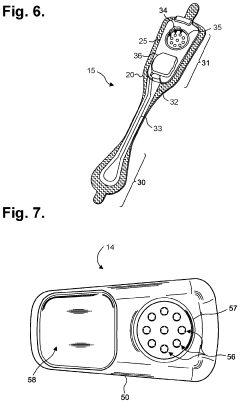
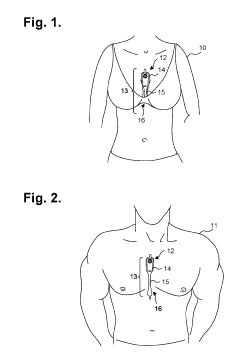
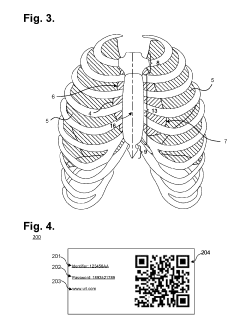
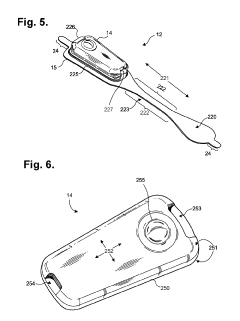
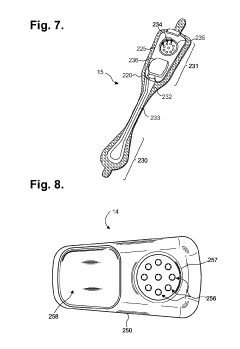
Moisture-resistant electrocardiography monitor
PatentActiveUS20230301576A1
Innovation
- A lightweight, wearable electrocardiography monitor with a flexible extended wear electrode patch and a reusable recorder that can be easily positioned on the sternal midline, optimized for sensing cardiac electrical potentials, including P-waves, and designed for extended wear with patient-friendly replacement and moisture resistance.
System And Method For Secure Cloud-Based Physiological Data Processing And Delivery
PatentActiveUS20190117099A1
Innovation
- A lightweight wearable monitor with a flexible extended wear electrode patch and a reusable recorder that improves P-wave sensing by positioning electrodes along the sternal midline, combined with secure cloud-based data processing and storage to enhance patient comfort, usability, and data security.
Regulatory Framework for Cardiac Diagnostic Tools
The regulatory framework for cardiac diagnostic tools plays a crucial role in ensuring the safety, efficacy, and quality of devices used in assessing diastolic dysfunction, including those that utilize P wave analysis. In the United States, the Food and Drug Administration (FDA) oversees the approval and regulation of medical devices, including cardiac diagnostic tools.
For devices that analyze P waves to assess diastolic dysfunction, manufacturers must navigate the FDA's premarket approval (PMA) or 510(k) clearance process, depending on the device's classification. Class II devices, which include many cardiac diagnostic tools, typically require 510(k) clearance. This process involves demonstrating that the new device is substantially equivalent to a legally marketed predicate device in terms of safety and effectiveness.
The regulatory pathway for these devices often includes clinical trials to validate their accuracy and reliability in assessing diastolic dysfunction. Manufacturers must provide evidence that P wave analysis contributes meaningfully to the diagnosis and does not introduce unacceptable risks or false readings.
In Europe, the regulatory landscape is governed by the Medical Device Regulation (MDR), which came into full effect in May 2021. Under the MDR, cardiac diagnostic tools that incorporate P wave analysis for diastolic dysfunction assessment would likely fall under Class IIa or IIb, depending on their specific characteristics and intended use.
Regulatory bodies worldwide emphasize the importance of post-market surveillance for cardiac diagnostic tools. Manufacturers are required to implement systems for collecting and analyzing real-world data on device performance and safety. This ongoing monitoring helps identify any potential issues or areas for improvement in P wave analysis techniques for assessing diastolic dysfunction.
Interoperability and data security are also key considerations in the regulatory framework. As cardiac diagnostic tools increasingly integrate with electronic health records and other digital health systems, regulators require manufacturers to demonstrate robust data protection measures and compliance with relevant privacy laws, such as HIPAA in the United States and GDPR in Europe.
The regulatory landscape for cardiac diagnostic tools is continually evolving to keep pace with technological advancements. Regulatory bodies are increasingly adopting a risk-based approach, focusing on the potential impact of the device on patient safety and clinical outcomes. This approach allows for more flexible and adaptive regulation, particularly important for innovative technologies like P wave analysis in diastolic dysfunction assessment.
For devices that analyze P waves to assess diastolic dysfunction, manufacturers must navigate the FDA's premarket approval (PMA) or 510(k) clearance process, depending on the device's classification. Class II devices, which include many cardiac diagnostic tools, typically require 510(k) clearance. This process involves demonstrating that the new device is substantially equivalent to a legally marketed predicate device in terms of safety and effectiveness.
The regulatory pathway for these devices often includes clinical trials to validate their accuracy and reliability in assessing diastolic dysfunction. Manufacturers must provide evidence that P wave analysis contributes meaningfully to the diagnosis and does not introduce unacceptable risks or false readings.
In Europe, the regulatory landscape is governed by the Medical Device Regulation (MDR), which came into full effect in May 2021. Under the MDR, cardiac diagnostic tools that incorporate P wave analysis for diastolic dysfunction assessment would likely fall under Class IIa or IIb, depending on their specific characteristics and intended use.
Regulatory bodies worldwide emphasize the importance of post-market surveillance for cardiac diagnostic tools. Manufacturers are required to implement systems for collecting and analyzing real-world data on device performance and safety. This ongoing monitoring helps identify any potential issues or areas for improvement in P wave analysis techniques for assessing diastolic dysfunction.
Interoperability and data security are also key considerations in the regulatory framework. As cardiac diagnostic tools increasingly integrate with electronic health records and other digital health systems, regulators require manufacturers to demonstrate robust data protection measures and compliance with relevant privacy laws, such as HIPAA in the United States and GDPR in Europe.
The regulatory landscape for cardiac diagnostic tools is continually evolving to keep pace with technological advancements. Regulatory bodies are increasingly adopting a risk-based approach, focusing on the potential impact of the device on patient safety and clinical outcomes. This approach allows for more flexible and adaptive regulation, particularly important for innovative technologies like P wave analysis in diastolic dysfunction assessment.
Integration with AI and Machine Learning
The integration of Artificial Intelligence (AI) and Machine Learning (ML) in assessing diastolic dysfunction through P wave analysis represents a significant advancement in cardiac diagnostics. These technologies offer the potential to enhance the accuracy, efficiency, and predictive capabilities of diastolic function evaluation.
Machine learning algorithms can be trained on large datasets of electrocardiograms (ECGs) to recognize subtle patterns in P wave morphology that may indicate diastolic dysfunction. These algorithms can potentially identify features that are not easily discernible to the human eye, improving the sensitivity and specificity of diagnosis.
Deep learning models, particularly convolutional neural networks (CNNs), have shown promise in automatically extracting relevant features from ECG signals. These models can be trained to analyze P wave characteristics such as duration, amplitude, and area, correlating them with various stages of diastolic dysfunction.
AI-powered systems can integrate P wave data with other clinical parameters, such as patient demographics, medical history, and echocardiographic findings. This holistic approach allows for a more comprehensive assessment of diastolic function and potentially improves risk stratification for heart failure.
Real-time analysis of P waves using AI algorithms could enable continuous monitoring of diastolic function in both inpatient and outpatient settings. This capability may lead to earlier detection of deteriorating cardiac function and allow for timely interventions.
Machine learning models can be developed to predict the progression of diastolic dysfunction based on longitudinal P wave data. Such predictive models could assist clinicians in tailoring treatment strategies and monitoring the effectiveness of interventions over time.
The integration of AI and ML also opens up possibilities for personalized medicine in the context of diastolic dysfunction. By analyzing individual P wave patterns and their changes over time, AI systems could help identify patient-specific risk factors and guide personalized treatment approaches.
However, challenges remain in the widespread adoption of AI and ML for P wave analysis in diastolic dysfunction assessment. These include the need for large, diverse, and high-quality datasets for training algorithms, ensuring the interpretability and explainability of AI-derived results, and validating the clinical efficacy of these technologies through rigorous clinical trials.
As AI and ML continue to evolve, their integration with P wave analysis for assessing diastolic dysfunction holds the promise of revolutionizing cardiac diagnostics, potentially leading to improved patient outcomes and more efficient healthcare delivery.
Machine learning algorithms can be trained on large datasets of electrocardiograms (ECGs) to recognize subtle patterns in P wave morphology that may indicate diastolic dysfunction. These algorithms can potentially identify features that are not easily discernible to the human eye, improving the sensitivity and specificity of diagnosis.
Deep learning models, particularly convolutional neural networks (CNNs), have shown promise in automatically extracting relevant features from ECG signals. These models can be trained to analyze P wave characteristics such as duration, amplitude, and area, correlating them with various stages of diastolic dysfunction.
AI-powered systems can integrate P wave data with other clinical parameters, such as patient demographics, medical history, and echocardiographic findings. This holistic approach allows for a more comprehensive assessment of diastolic function and potentially improves risk stratification for heart failure.
Real-time analysis of P waves using AI algorithms could enable continuous monitoring of diastolic function in both inpatient and outpatient settings. This capability may lead to earlier detection of deteriorating cardiac function and allow for timely interventions.
Machine learning models can be developed to predict the progression of diastolic dysfunction based on longitudinal P wave data. Such predictive models could assist clinicians in tailoring treatment strategies and monitoring the effectiveness of interventions over time.
The integration of AI and ML also opens up possibilities for personalized medicine in the context of diastolic dysfunction. By analyzing individual P wave patterns and their changes over time, AI systems could help identify patient-specific risk factors and guide personalized treatment approaches.
However, challenges remain in the widespread adoption of AI and ML for P wave analysis in diastolic dysfunction assessment. These include the need for large, diverse, and high-quality datasets for training algorithms, ensuring the interpretability and explainability of AI-derived results, and validating the clinical efficacy of these technologies through rigorous clinical trials.
As AI and ML continue to evolve, their integration with P wave analysis for assessing diastolic dysfunction holds the promise of revolutionizing cardiac diagnostics, potentially leading to improved patient outcomes and more efficient healthcare delivery.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!