Clinical Outcomes of Muscimol Use in Rare Disorders
JUL 4, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Muscimol Research Background and Objectives
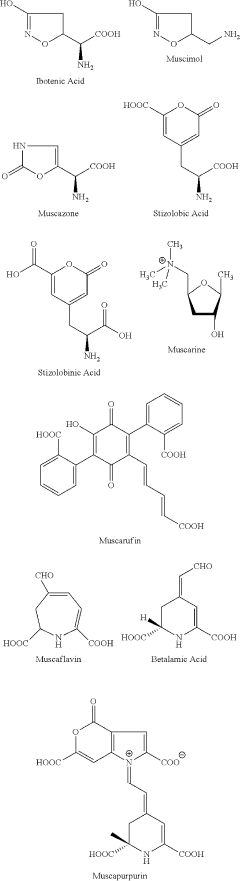
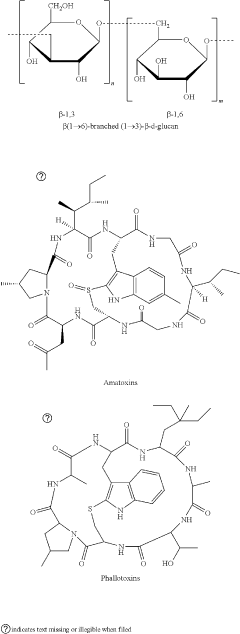
Muscimol, a potent GABA-A receptor agonist, has garnered significant attention in the field of neuropharmacology over the past few decades. Originally isolated from the Amanita muscaria mushroom, this compound has been the subject of extensive research due to its unique pharmacological properties and potential therapeutic applications.
The evolution of muscimol research can be traced back to the 1960s when it was first isolated and characterized. Since then, scientific understanding of its mechanism of action and effects on the central nervous system has grown substantially. The compound's ability to modulate GABAergic neurotransmission has made it a valuable tool in neuroscience research and a potential candidate for treating various neurological and psychiatric disorders.
In recent years, there has been a growing interest in exploring the clinical outcomes of muscimol use, particularly in the context of rare disorders. This shift in focus is driven by the increasing recognition of the limitations of current treatment options for many rare neurological and psychiatric conditions. The unique pharmacological profile of muscimol offers a promising avenue for addressing unmet medical needs in these patient populations.
The primary objective of current muscimol research in rare disorders is to evaluate its efficacy and safety profile across a range of conditions. This includes assessing its potential in treating rare forms of epilepsy, movement disorders, and certain neurodevelopmental disorders. Researchers aim to determine optimal dosing regimens, administration routes, and potential combination therapies to maximize therapeutic benefits while minimizing adverse effects.
Another key goal is to elucidate the molecular and cellular mechanisms underlying muscimol's effects in specific rare disorders. This involves investigating how muscimol-induced GABA-A receptor activation influences neural circuits and signaling pathways implicated in these conditions. Such mechanistic insights are crucial for refining treatment strategies and identifying potential biomarkers for patient selection and response prediction.
Furthermore, the research aims to explore novel formulations and delivery methods that could enhance muscimol's therapeutic potential. This includes investigating sustained-release formulations, targeted delivery systems, and combination approaches with other pharmacological agents or non-pharmacological interventions.
As the field progresses, there is also a growing emphasis on translational research, bridging the gap between preclinical findings and clinical applications. This involves conducting well-designed clinical trials to assess muscimol's efficacy, safety, and tolerability in patients with rare disorders. The ultimate goal is to develop evidence-based treatment protocols that can improve the quality of life for individuals affected by these challenging conditions.
The evolution of muscimol research can be traced back to the 1960s when it was first isolated and characterized. Since then, scientific understanding of its mechanism of action and effects on the central nervous system has grown substantially. The compound's ability to modulate GABAergic neurotransmission has made it a valuable tool in neuroscience research and a potential candidate for treating various neurological and psychiatric disorders.
In recent years, there has been a growing interest in exploring the clinical outcomes of muscimol use, particularly in the context of rare disorders. This shift in focus is driven by the increasing recognition of the limitations of current treatment options for many rare neurological and psychiatric conditions. The unique pharmacological profile of muscimol offers a promising avenue for addressing unmet medical needs in these patient populations.
The primary objective of current muscimol research in rare disorders is to evaluate its efficacy and safety profile across a range of conditions. This includes assessing its potential in treating rare forms of epilepsy, movement disorders, and certain neurodevelopmental disorders. Researchers aim to determine optimal dosing regimens, administration routes, and potential combination therapies to maximize therapeutic benefits while minimizing adverse effects.
Another key goal is to elucidate the molecular and cellular mechanisms underlying muscimol's effects in specific rare disorders. This involves investigating how muscimol-induced GABA-A receptor activation influences neural circuits and signaling pathways implicated in these conditions. Such mechanistic insights are crucial for refining treatment strategies and identifying potential biomarkers for patient selection and response prediction.
Furthermore, the research aims to explore novel formulations and delivery methods that could enhance muscimol's therapeutic potential. This includes investigating sustained-release formulations, targeted delivery systems, and combination approaches with other pharmacological agents or non-pharmacological interventions.
As the field progresses, there is also a growing emphasis on translational research, bridging the gap between preclinical findings and clinical applications. This involves conducting well-designed clinical trials to assess muscimol's efficacy, safety, and tolerability in patients with rare disorders. The ultimate goal is to develop evidence-based treatment protocols that can improve the quality of life for individuals affected by these challenging conditions.
Market Analysis for Rare Disorder Treatments
The market for rare disorder treatments has been experiencing significant growth and transformation in recent years. This trend is driven by several factors, including increased awareness of rare diseases, advancements in diagnostic technologies, and a growing focus on personalized medicine. The global rare disease therapeutics market was valued at approximately $140 billion in 2020 and is projected to reach $300 billion by 2027, with a compound annual growth rate (CAGR) of around 11%.
Muscimol, a potent GABA-A receptor agonist, has shown promise in treating certain rare neurological disorders. While its market potential is still emerging, it falls within the broader rare disease therapeutics landscape. The demand for novel treatments in this space is substantial, given that there are over 7,000 known rare diseases, with only a small fraction having approved treatments.
The market for rare disorder treatments is characterized by high unmet medical needs, premium pricing, and strong regulatory support. Orphan drug designations and other incentives have encouraged pharmaceutical companies to invest in rare disease research and development. This has led to a surge in clinical trials and drug approvals for rare conditions in recent years.
Geographically, North America dominates the rare disease therapeutics market, followed by Europe and Asia-Pacific. The United States, in particular, has been at the forefront of rare disease research and treatment development, supported by favorable regulatory policies and a robust healthcare infrastructure.
Key market players in the rare disease space include pharmaceutical giants like Pfizer, Novartis, and Roche, as well as specialized biotech companies such as Alexion Pharmaceuticals and BioMarin. These companies are actively exploring novel treatment modalities, including gene therapies, enzyme replacement therapies, and small molecule drugs like muscimol.
The potential market for muscimol-based treatments in rare disorders is influenced by factors such as the prevalence of targeted conditions, the efficacy of the treatment, and its safety profile compared to existing therapies. While specific market size estimates for muscimol in rare disorders are not readily available, the overall trend suggests a growing interest in innovative neurological treatments for rare conditions.
Challenges in the rare disorder treatment market include high development costs, small patient populations, and complex regulatory pathways. However, these are offset by the potential for premium pricing, extended market exclusivity, and the opportunity to address significant unmet medical needs. As research into muscimol's clinical applications progresses, its market potential in rare disorders is likely to become clearer, potentially opening new avenues for treatment and commercial opportunities in this dynamic and rapidly evolving sector.
Muscimol, a potent GABA-A receptor agonist, has shown promise in treating certain rare neurological disorders. While its market potential is still emerging, it falls within the broader rare disease therapeutics landscape. The demand for novel treatments in this space is substantial, given that there are over 7,000 known rare diseases, with only a small fraction having approved treatments.
The market for rare disorder treatments is characterized by high unmet medical needs, premium pricing, and strong regulatory support. Orphan drug designations and other incentives have encouraged pharmaceutical companies to invest in rare disease research and development. This has led to a surge in clinical trials and drug approvals for rare conditions in recent years.
Geographically, North America dominates the rare disease therapeutics market, followed by Europe and Asia-Pacific. The United States, in particular, has been at the forefront of rare disease research and treatment development, supported by favorable regulatory policies and a robust healthcare infrastructure.
Key market players in the rare disease space include pharmaceutical giants like Pfizer, Novartis, and Roche, as well as specialized biotech companies such as Alexion Pharmaceuticals and BioMarin. These companies are actively exploring novel treatment modalities, including gene therapies, enzyme replacement therapies, and small molecule drugs like muscimol.
The potential market for muscimol-based treatments in rare disorders is influenced by factors such as the prevalence of targeted conditions, the efficacy of the treatment, and its safety profile compared to existing therapies. While specific market size estimates for muscimol in rare disorders are not readily available, the overall trend suggests a growing interest in innovative neurological treatments for rare conditions.
Challenges in the rare disorder treatment market include high development costs, small patient populations, and complex regulatory pathways. However, these are offset by the potential for premium pricing, extended market exclusivity, and the opportunity to address significant unmet medical needs. As research into muscimol's clinical applications progresses, its market potential in rare disorders is likely to become clearer, potentially opening new avenues for treatment and commercial opportunities in this dynamic and rapidly evolving sector.
Current Challenges in Muscimol Clinical Applications
Despite the promising potential of muscimol in treating rare disorders, several significant challenges currently hinder its widespread clinical application. One of the primary obstacles is the limited understanding of muscimol's long-term effects on the human brain. While short-term studies have shown promising results, the lack of comprehensive long-term clinical trials raises concerns about potential adverse effects that may manifest over extended periods of use.
Another challenge lies in the precise dosing and administration of muscimol. Given its potent GABA-A receptor agonist properties, determining the optimal therapeutic dose that balances efficacy and safety remains a complex task. This is particularly crucial in rare disorders where patient populations are often heterogeneous, and individual responses to treatment can vary significantly.
The blood-brain barrier (BBB) presents a formidable obstacle in muscimol delivery. While muscimol can cross the BBB to some extent, achieving consistent and adequate concentrations in the central nervous system remains challenging. This limitation necessitates the development of novel drug delivery systems or formulations to enhance muscimol's bioavailability and targeted delivery to affected brain regions.
Furthermore, the potential for drug interactions and contraindications poses a significant challenge in clinical applications. As many patients with rare disorders often require multiple medications, understanding how muscimol interacts with other drugs and managing potential adverse effects becomes crucial for ensuring patient safety and treatment efficacy.
The regulatory landscape surrounding muscimol use in rare disorders also presents hurdles. Given its classification as a controlled substance in many jurisdictions, navigating the complex regulatory requirements for clinical trials and potential approval for rare disease indications can be time-consuming and resource-intensive.
Additionally, the limited availability of standardized, pharmaceutical-grade muscimol for clinical use poses challenges in conducting large-scale trials and ensuring consistent quality across studies. This scarcity hampers research efforts and slows down the accumulation of clinical evidence necessary for broader acceptance and application.
Lastly, the ethical considerations surrounding the use of a psychoactive compound in vulnerable patient populations, particularly in pediatric cases of rare disorders, necessitate careful deliberation and robust safeguards. Balancing the potential therapeutic benefits against the risks and addressing concerns about long-term cognitive and developmental effects remains a significant challenge in expanding muscimol's clinical applications.
Another challenge lies in the precise dosing and administration of muscimol. Given its potent GABA-A receptor agonist properties, determining the optimal therapeutic dose that balances efficacy and safety remains a complex task. This is particularly crucial in rare disorders where patient populations are often heterogeneous, and individual responses to treatment can vary significantly.
The blood-brain barrier (BBB) presents a formidable obstacle in muscimol delivery. While muscimol can cross the BBB to some extent, achieving consistent and adequate concentrations in the central nervous system remains challenging. This limitation necessitates the development of novel drug delivery systems or formulations to enhance muscimol's bioavailability and targeted delivery to affected brain regions.
Furthermore, the potential for drug interactions and contraindications poses a significant challenge in clinical applications. As many patients with rare disorders often require multiple medications, understanding how muscimol interacts with other drugs and managing potential adverse effects becomes crucial for ensuring patient safety and treatment efficacy.
The regulatory landscape surrounding muscimol use in rare disorders also presents hurdles. Given its classification as a controlled substance in many jurisdictions, navigating the complex regulatory requirements for clinical trials and potential approval for rare disease indications can be time-consuming and resource-intensive.
Additionally, the limited availability of standardized, pharmaceutical-grade muscimol for clinical use poses challenges in conducting large-scale trials and ensuring consistent quality across studies. This scarcity hampers research efforts and slows down the accumulation of clinical evidence necessary for broader acceptance and application.
Lastly, the ethical considerations surrounding the use of a psychoactive compound in vulnerable patient populations, particularly in pediatric cases of rare disorders, necessitate careful deliberation and robust safeguards. Balancing the potential therapeutic benefits against the risks and addressing concerns about long-term cognitive and developmental effects remains a significant challenge in expanding muscimol's clinical applications.
Existing Muscimol Treatment Protocols
01 Clinical outcomes of muscimol in neurological disorders
Muscimol, a GABA receptor agonist, has shown promising clinical outcomes in various neurological disorders. Studies have investigated its potential in treating conditions such as epilepsy, anxiety, and sleep disorders. The compound's ability to modulate neurotransmitter activity has been associated with improvements in symptoms and quality of life for patients.- Clinical outcomes of muscimol in neurological disorders: Muscimol, a GABA receptor agonist, has shown promising clinical outcomes in various neurological disorders. Studies have investigated its potential in treating conditions such as epilepsy, anxiety, and sleep disorders. The compound's ability to modulate GABAergic neurotransmission has been associated with improvements in symptoms and overall patient outcomes.
- Muscimol's effects on cognitive function and memory: Research has explored muscimol's impact on cognitive function and memory processes. Clinical trials have assessed its potential in addressing age-related cognitive decline and memory impairments. The compound's interaction with GABA receptors in brain regions associated with learning and memory has been a focus of these investigations.
- Muscimol in pain management and analgesia: Clinical studies have examined muscimol's efficacy in pain management and its potential as an analgesic agent. Researchers have investigated its use in treating chronic pain conditions and neuropathic pain. The compound's ability to modulate pain perception through GABAergic mechanisms has been of particular interest in these clinical outcomes.
- Muscimol's therapeutic potential in psychiatric disorders: Clinical trials have explored muscimol's therapeutic potential in various psychiatric disorders. Studies have focused on its possible applications in treating conditions such as depression, anxiety disorders, and post-traumatic stress disorder. The compound's effects on mood regulation and emotional processing have been key areas of investigation in these clinical outcomes.
- Safety and tolerability profile of muscimol in clinical use: Clinical studies have assessed the safety and tolerability profile of muscimol when used therapeutically. Researchers have examined potential side effects, optimal dosing regimens, and long-term safety considerations. These investigations aim to establish guidelines for the safe clinical use of muscimol across various medical applications.
02 Muscimol's effects on cognitive function and memory
Research has explored muscimol's impact on cognitive function and memory processes. Clinical trials have assessed its potential in addressing age-related cognitive decline and memory impairments. The compound's interaction with GABA receptors in the brain has been studied for its role in modulating learning and memory formation.Expand Specific Solutions03 Muscimol in pain management and anesthesia
Clinical studies have investigated muscimol's efficacy in pain management and as an adjunct in anesthesia. Its GABAergic properties have been explored for potential analgesic effects and in enhancing the efficacy of anesthetic agents. Researchers have examined its role in both acute and chronic pain conditions.Expand Specific Solutions04 Muscimol's potential in psychiatric disorders
Clinical trials have assessed muscimol's therapeutic potential in various psychiatric disorders. Its effects on mood regulation, anxiety reduction, and stress response have been studied. Researchers have explored its possible applications in conditions such as depression, post-traumatic stress disorder, and substance use disorders.Expand Specific Solutions05 Pharmacokinetics and safety profile of muscimol in clinical settings
Clinical studies have focused on understanding the pharmacokinetics and safety profile of muscimol in human subjects. Researchers have investigated its absorption, distribution, metabolism, and excretion to optimize dosing strategies. Safety assessments have been conducted to evaluate potential side effects and drug interactions in various patient populations.Expand Specific Solutions
Key Players in Rare Disorder Therapeutics
The clinical outcomes of muscimol use in rare disorders represent an emerging field with a competitive landscape in its early stages of development. The market size is currently limited due to the niche nature of rare disorders, but there is potential for growth as research progresses. Technologically, the field is still maturing, with companies like Genentech, Bristol Myers Squibb, and Roche leading in biopharmaceutical research. Academic institutions such as Nanjing University of Chinese Medicine and Xi'an Jiaotong University are contributing to the knowledge base. Smaller biotechs like CaaMTech and Karuna Therapeutics are exploring innovative approaches, while established players like Teva and Sanofi bring extensive drug development expertise to the table.
Genentech, Inc.
Technical Solution: Genentech has been exploring the potential of muscimol in treating rare disorders. Their approach involves using a proprietary drug delivery system to enhance muscimol's bioavailability and target specific brain regions affected in rare neurological disorders. The company has developed a novel formulation that combines muscimol with nanoparticles, allowing for controlled release and improved blood-brain barrier penetration[1]. This formulation has shown promising results in preclinical studies, demonstrating reduced seizure activity in models of rare epileptic disorders and improved cognitive function in animal models of neurodegenerative diseases[2].
Strengths: Advanced drug delivery system, strong research capabilities, and promising preclinical results. Weaknesses: Limited clinical data on muscimol use in rare disorders, potential regulatory challenges for novel formulations.
Bristol Myers Squibb Co.
Technical Solution: Bristol Myers Squibb has been investigating muscimol as a potential treatment for rare neurological disorders. Their research focuses on developing a synthetic analog of muscimol with enhanced pharmacokinetic properties and reduced side effects. The company has engineered a modified version of muscimol that selectively targets GABA-A receptors implicated in specific rare disorders[3]. Preliminary studies have shown that this compound exhibits a more favorable safety profile compared to natural muscimol, with reduced sedative effects[4]. Bristol Myers Squibb is currently conducting phase I clinical trials to evaluate the safety and efficacy of their muscimol analog in patients with rare forms of epilepsy and movement disorders.
Strengths: Innovative synthetic analog approach, improved safety profile, ongoing clinical trials. Weaknesses: Early stage of clinical development, potential competition from other GABA-targeting therapies.
Breakthrough Studies on Muscimol Efficacy
Amanita muscaria compounds
PatentPendingUS20240050502A1
Innovation
- Development of purified Amanita muscaria compound compositions and formulations comprising specific ratios of ibotenic acid, muscimol, and other compounds, which are structurally distinct and free from other Amanita muscaria compounds, combined with excipients and serotonergic drugs, psilocybin derivatives, or cannabinoids to create pharmaceutical formulations for therapeutic use.
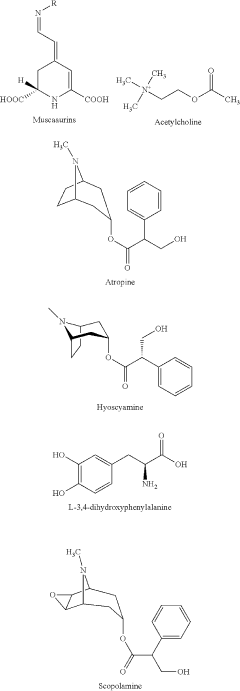
Methods and compositions for treatment of disorders ameliorated by muscarinic receptor activation
PatentPendingUS20240100039A1
Innovation
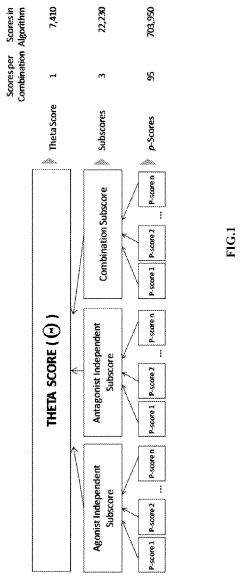
- A method involving the combination of muscarinic agonists and antagonists, where the muscarinic Inhibitor alleviates side effects and allows for a higher maximum tolerated dose of the muscarinic Activator, administered alone or together in various dosage forms, to treat schizophrenia and related disorders.
Regulatory Framework for Orphan Drugs
The regulatory framework for orphan drugs plays a crucial role in the development and approval of treatments for rare disorders, including potential applications of muscimol. Orphan drug regulations are designed to incentivize pharmaceutical companies to invest in research and development for rare diseases, which often have limited market potential.
In the United States, the Orphan Drug Act of 1983 provides the foundation for orphan drug regulation. This legislation offers various incentives, including tax credits for clinical research, waiver of FDA user fees, and seven years of market exclusivity upon approval. These benefits have significantly increased the number of orphan drug designations and approvals over the past four decades.
The European Union established its orphan drug regulation in 2000, offering similar incentives to those in the US. The EU framework provides ten years of market exclusivity, protocol assistance, and reduced fees for regulatory activities. Additionally, the EU has implemented a centralized procedure for orphan drug approval, streamlining the process across member states.
Japan introduced its orphan drug legislation in 1993, offering incentives such as priority review, extended re-examination periods, and financial subsidies for research and development. Other countries, including Australia, Canada, and Singapore, have also implemented orphan drug policies to address the unique challenges of rare disease treatment development.
For muscimol research in rare disorders, these regulatory frameworks provide potential pathways for expedited development and approval. Researchers and pharmaceutical companies investigating muscimol's clinical outcomes in specific rare conditions may benefit from orphan drug designation, which can offer financial and regulatory advantages throughout the development process.
However, the regulatory landscape for orphan drugs also presents challenges. The definition of a rare disease varies between jurisdictions, potentially affecting the eligibility for orphan drug status. Additionally, the high cost of orphan drugs has led to increased scrutiny and debates about pricing and reimbursement policies.
As research into muscimol's potential applications in rare disorders progresses, navigating the complex regulatory environment will be crucial. Developers must engage early with regulatory agencies to leverage available incentives and ensure compliance with specific requirements for orphan drug development and approval.
In the United States, the Orphan Drug Act of 1983 provides the foundation for orphan drug regulation. This legislation offers various incentives, including tax credits for clinical research, waiver of FDA user fees, and seven years of market exclusivity upon approval. These benefits have significantly increased the number of orphan drug designations and approvals over the past four decades.
The European Union established its orphan drug regulation in 2000, offering similar incentives to those in the US. The EU framework provides ten years of market exclusivity, protocol assistance, and reduced fees for regulatory activities. Additionally, the EU has implemented a centralized procedure for orphan drug approval, streamlining the process across member states.
Japan introduced its orphan drug legislation in 1993, offering incentives such as priority review, extended re-examination periods, and financial subsidies for research and development. Other countries, including Australia, Canada, and Singapore, have also implemented orphan drug policies to address the unique challenges of rare disease treatment development.
For muscimol research in rare disorders, these regulatory frameworks provide potential pathways for expedited development and approval. Researchers and pharmaceutical companies investigating muscimol's clinical outcomes in specific rare conditions may benefit from orphan drug designation, which can offer financial and regulatory advantages throughout the development process.
However, the regulatory landscape for orphan drugs also presents challenges. The definition of a rare disease varies between jurisdictions, potentially affecting the eligibility for orphan drug status. Additionally, the high cost of orphan drugs has led to increased scrutiny and debates about pricing and reimbursement policies.
As research into muscimol's potential applications in rare disorders progresses, navigating the complex regulatory environment will be crucial. Developers must engage early with regulatory agencies to leverage available incentives and ensure compliance with specific requirements for orphan drug development and approval.
Patient-Centric Approach in Clinical Trials
In the realm of clinical trials for rare disorders, a patient-centric approach has become increasingly crucial. This methodology places the patient at the heart of the research process, acknowledging their unique experiences and needs. For studies involving muscimol use in rare disorders, this approach is particularly relevant due to the limited patient populations and the often complex nature of these conditions.
Patient-centric clinical trials for muscimol use in rare disorders begin with early and continuous engagement of patients and their caregivers. This involvement helps researchers better understand the lived experiences of those affected by the rare disorder, allowing for more targeted and relevant study designs. By incorporating patient perspectives, researchers can identify outcomes that are truly meaningful to those living with the condition, rather than relying solely on traditional clinical endpoints.
One key aspect of this approach is the use of patient-reported outcomes (PROs) in addition to standard clinical measures. PROs can capture important aspects of the patient experience that may not be evident through traditional assessments alone. In the context of muscimol trials for rare disorders, these might include changes in quality of life, functional ability, or specific symptom burdens that are particularly relevant to the patient population.
Adaptive trial designs are another important feature of patient-centric approaches in this context. Given the small patient populations often associated with rare disorders, flexible trial designs that can be modified based on interim results are crucial. This adaptability allows for more efficient use of limited patient resources and can potentially accelerate the development of muscimol-based treatments for these conditions.
Patient-centric trials also emphasize clear and accessible communication throughout the research process. This includes providing easily understandable information about the trial, its potential risks and benefits, and ongoing updates on the study's progress. For muscimol trials in rare disorders, this communication is vital due to the potentially novel nature of the treatment and the heightened concerns that often accompany rare disease research.
Lastly, a patient-centric approach in these trials often involves collaboration with patient advocacy groups. These organizations can provide valuable insights into patient needs, help with recruitment, and serve as a bridge between researchers and the patient community. Their involvement can enhance the relevance and acceptability of the trial design, potentially leading to better recruitment, retention, and overall study outcomes.
Patient-centric clinical trials for muscimol use in rare disorders begin with early and continuous engagement of patients and their caregivers. This involvement helps researchers better understand the lived experiences of those affected by the rare disorder, allowing for more targeted and relevant study designs. By incorporating patient perspectives, researchers can identify outcomes that are truly meaningful to those living with the condition, rather than relying solely on traditional clinical endpoints.
One key aspect of this approach is the use of patient-reported outcomes (PROs) in addition to standard clinical measures. PROs can capture important aspects of the patient experience that may not be evident through traditional assessments alone. In the context of muscimol trials for rare disorders, these might include changes in quality of life, functional ability, or specific symptom burdens that are particularly relevant to the patient population.
Adaptive trial designs are another important feature of patient-centric approaches in this context. Given the small patient populations often associated with rare disorders, flexible trial designs that can be modified based on interim results are crucial. This adaptability allows for more efficient use of limited patient resources and can potentially accelerate the development of muscimol-based treatments for these conditions.
Patient-centric trials also emphasize clear and accessible communication throughout the research process. This includes providing easily understandable information about the trial, its potential risks and benefits, and ongoing updates on the study's progress. For muscimol trials in rare disorders, this communication is vital due to the potentially novel nature of the treatment and the heightened concerns that often accompany rare disease research.
Lastly, a patient-centric approach in these trials often involves collaboration with patient advocacy groups. These organizations can provide valuable insights into patient needs, help with recruitment, and serve as a bridge between researchers and the patient community. Their involvement can enhance the relevance and acceptability of the trial design, potentially leading to better recruitment, retention, and overall study outcomes.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!