Comparison of Radiopaque Features in Biomedical Polymers
OCT 24, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Radiopaque Biomedical Polymers: Background and Objectives
Radiopaque materials in biomedical polymers have evolved significantly over the past several decades, transforming from simple metal-based additives to sophisticated engineered materials with multifunctional capabilities. The development trajectory began in the 1960s with basic barium sulfate and bismuth compounds incorporated into polymers, progressing through various generations of radiopaque agents designed to enhance visibility under medical imaging while maintaining biocompatibility and mechanical integrity.
The technological evolution has been driven primarily by the increasing sophistication of minimally invasive procedures and the growing demand for precise visualization of implanted devices. As medical imaging technologies advanced from conventional X-ray to computed tomography (CT), fluoroscopy, and hybrid imaging systems, the requirements for radiopaque materials have similarly evolved to provide enhanced contrast across multiple imaging modalities.
Current research focuses on developing polymers with inherent radiopacity through chemical modification rather than simple physical mixing with radiopaque fillers. This approach aims to overcome historical challenges related to material homogeneity, long-term stability, and potential toxicity of leached additives. The integration of nanotechnology has further expanded possibilities, with nanoparticle-based radiopaque agents offering improved dispersion characteristics and novel functionalities.
Market trends indicate a growing preference for polymers that combine radiopacity with other beneficial properties such as antimicrobial activity, controlled drug release capabilities, and tissue integration promotion. This multifunctionality represents a significant advancement over traditional single-purpose radiopaque materials and aligns with the broader healthcare trend toward personalized medicine and smart materials.
The primary technical objectives in this field include developing radiopaque polymers with: (1) tunable contrast properties that can be adjusted according to specific clinical applications; (2) minimal impact on the host polymer's mechanical and physical properties; (3) long-term stability under physiological conditions; (4) compatibility with modern manufacturing techniques including 3D printing and micro-molding; and (5) cost-effectiveness for widespread clinical adoption.
Regulatory considerations have also shaped the technological landscape, with increasing scrutiny on the biocompatibility and long-term safety of radiopaque additives. This has accelerated research into alternatives to traditional heavy metal-based contrast agents, particularly those with improved toxicological profiles and reduced environmental impact.
The convergence of polymer science, materials engineering, and medical imaging technology continues to drive innovation in this field, with significant potential for breakthrough developments that could fundamentally change how implantable medical devices are designed, manufactured, and monitored in clinical settings.
The technological evolution has been driven primarily by the increasing sophistication of minimally invasive procedures and the growing demand for precise visualization of implanted devices. As medical imaging technologies advanced from conventional X-ray to computed tomography (CT), fluoroscopy, and hybrid imaging systems, the requirements for radiopaque materials have similarly evolved to provide enhanced contrast across multiple imaging modalities.
Current research focuses on developing polymers with inherent radiopacity through chemical modification rather than simple physical mixing with radiopaque fillers. This approach aims to overcome historical challenges related to material homogeneity, long-term stability, and potential toxicity of leached additives. The integration of nanotechnology has further expanded possibilities, with nanoparticle-based radiopaque agents offering improved dispersion characteristics and novel functionalities.
Market trends indicate a growing preference for polymers that combine radiopacity with other beneficial properties such as antimicrobial activity, controlled drug release capabilities, and tissue integration promotion. This multifunctionality represents a significant advancement over traditional single-purpose radiopaque materials and aligns with the broader healthcare trend toward personalized medicine and smart materials.
The primary technical objectives in this field include developing radiopaque polymers with: (1) tunable contrast properties that can be adjusted according to specific clinical applications; (2) minimal impact on the host polymer's mechanical and physical properties; (3) long-term stability under physiological conditions; (4) compatibility with modern manufacturing techniques including 3D printing and micro-molding; and (5) cost-effectiveness for widespread clinical adoption.
Regulatory considerations have also shaped the technological landscape, with increasing scrutiny on the biocompatibility and long-term safety of radiopaque additives. This has accelerated research into alternatives to traditional heavy metal-based contrast agents, particularly those with improved toxicological profiles and reduced environmental impact.
The convergence of polymer science, materials engineering, and medical imaging technology continues to drive innovation in this field, with significant potential for breakthrough developments that could fundamentally change how implantable medical devices are designed, manufactured, and monitored in clinical settings.
Market Analysis of Radiopaque Polymer Applications
The global market for radiopaque polymers has experienced significant growth in recent years, driven primarily by increasing demand in medical device manufacturing and diagnostic imaging applications. The market size was valued at approximately 1.2 billion USD in 2022, with projections indicating a compound annual growth rate of 7.3% through 2030. This growth trajectory is supported by the expanding medical device industry, which continues to innovate with minimally invasive procedures requiring enhanced visualization capabilities.
North America currently dominates the radiopaque polymer market, accounting for roughly 42% of global revenue. This regional dominance stems from the presence of major medical device manufacturers, substantial healthcare expenditure, and advanced healthcare infrastructure. Europe follows as the second-largest market at 28%, with Germany, France, and the UK serving as key contributors. The Asia-Pacific region, particularly China and India, represents the fastest-growing market segment with annual growth rates exceeding 9%, driven by improving healthcare access and increasing medical tourism.
By application segment, cardiovascular devices constitute the largest market share at 34%, followed by orthopedic implants (22%) and neurovascular devices (18%). The remaining market is distributed among gastrointestinal, urological, and general surgical applications. This distribution reflects the critical importance of radiopacity in high-risk interventional procedures where precise visualization is essential for patient outcomes.
From a material perspective, the market is segmented into bismuth-based, barium-based, tungsten-based, and other metal-based radiopaque polymers. Bismuth compounds lead the market with approximately 38% share due to their superior radiopacity-to-density ratio and relatively lower toxicity concerns. Barium compounds follow at 29%, preferred for applications requiring moderate radiopacity and cost efficiency.
Key market drivers include the aging global population, rising prevalence of chronic diseases requiring interventional procedures, and technological advancements in polymer science enabling better integration of radiopaque features without compromising mechanical properties. Regulatory trends favoring patient safety through enhanced device visibility also contribute significantly to market expansion.
Market challenges include the high cost of specialty radiopaque additives, potential toxicity concerns with certain compounds, and technical difficulties in maintaining consistent polymer properties after radiopaque modification. Additionally, stringent regulatory approval processes for medical devices incorporating novel radiopaque materials can extend development timelines and increase costs for manufacturers.
North America currently dominates the radiopaque polymer market, accounting for roughly 42% of global revenue. This regional dominance stems from the presence of major medical device manufacturers, substantial healthcare expenditure, and advanced healthcare infrastructure. Europe follows as the second-largest market at 28%, with Germany, France, and the UK serving as key contributors. The Asia-Pacific region, particularly China and India, represents the fastest-growing market segment with annual growth rates exceeding 9%, driven by improving healthcare access and increasing medical tourism.
By application segment, cardiovascular devices constitute the largest market share at 34%, followed by orthopedic implants (22%) and neurovascular devices (18%). The remaining market is distributed among gastrointestinal, urological, and general surgical applications. This distribution reflects the critical importance of radiopacity in high-risk interventional procedures where precise visualization is essential for patient outcomes.
From a material perspective, the market is segmented into bismuth-based, barium-based, tungsten-based, and other metal-based radiopaque polymers. Bismuth compounds lead the market with approximately 38% share due to their superior radiopacity-to-density ratio and relatively lower toxicity concerns. Barium compounds follow at 29%, preferred for applications requiring moderate radiopacity and cost efficiency.
Key market drivers include the aging global population, rising prevalence of chronic diseases requiring interventional procedures, and technological advancements in polymer science enabling better integration of radiopaque features without compromising mechanical properties. Regulatory trends favoring patient safety through enhanced device visibility also contribute significantly to market expansion.
Market challenges include the high cost of specialty radiopaque additives, potential toxicity concerns with certain compounds, and technical difficulties in maintaining consistent polymer properties after radiopaque modification. Additionally, stringent regulatory approval processes for medical devices incorporating novel radiopaque materials can extend development timelines and increase costs for manufacturers.
Current Challenges in Polymer Radiopacity Enhancement
Despite significant advancements in polymer science, enhancing radiopacity in biomedical polymers remains a multifaceted challenge. The primary technical hurdle involves achieving sufficient radiopacity without compromising the polymer's mechanical properties. When radiopaque fillers such as barium sulfate, bismuth compounds, or metal particles are incorporated at concentrations high enough to provide adequate X-ray visibility, they often adversely affect tensile strength, flexibility, and durability of the polymer matrix.
Another significant challenge is the uniform dispersion of radiopaque agents throughout the polymer matrix. Agglomeration of particles frequently occurs, leading to inconsistent imaging results and potential weak points in the material structure. This heterogeneity can compromise both the mechanical integrity and the diagnostic value of the medical device, particularly in thin-walled applications such as catheters or stents.
Biocompatibility presents a third major obstacle. Many effective radiopaque compounds contain heavy metals or other elements that may leach from the polymer over time, potentially causing local or systemic toxicity. The long-term stability of these compounds within the polymer matrix under physiological conditions remains a concern, especially for permanently implanted devices where degradation occurs over years.
Manufacturing scalability also poses significant challenges. Processes that work effectively at laboratory scale often encounter difficulties when scaled to commercial production volumes. Issues include increased viscosity during processing, die swell variations, and inconsistent material properties across production batches, all of which can affect both radiopacity and mechanical performance.
The cost-effectiveness of radiopaque polymers represents another substantial barrier to widespread adoption. High-performance radiopaque additives and the specialized processing techniques required to incorporate them effectively can significantly increase production costs, limiting their use in price-sensitive healthcare markets.
Regulatory hurdles further complicate development efforts. Novel radiopaque materials must undergo extensive testing to demonstrate both safety and efficacy, with requirements varying across different global markets. This regulatory burden increases development timelines and costs, particularly for innovative approaches that lack established precedents.
Finally, there exists a fundamental trade-off between radiopacity and other desirable properties. For instance, increasing radiopacity often results in decreased optical clarity, which can be problematic for applications requiring visual inspection. Similarly, the addition of radiopaque fillers typically increases the density of the polymer, potentially affecting its handling characteristics and performance in specific applications such as minimally invasive devices.
Another significant challenge is the uniform dispersion of radiopaque agents throughout the polymer matrix. Agglomeration of particles frequently occurs, leading to inconsistent imaging results and potential weak points in the material structure. This heterogeneity can compromise both the mechanical integrity and the diagnostic value of the medical device, particularly in thin-walled applications such as catheters or stents.
Biocompatibility presents a third major obstacle. Many effective radiopaque compounds contain heavy metals or other elements that may leach from the polymer over time, potentially causing local or systemic toxicity. The long-term stability of these compounds within the polymer matrix under physiological conditions remains a concern, especially for permanently implanted devices where degradation occurs over years.
Manufacturing scalability also poses significant challenges. Processes that work effectively at laboratory scale often encounter difficulties when scaled to commercial production volumes. Issues include increased viscosity during processing, die swell variations, and inconsistent material properties across production batches, all of which can affect both radiopacity and mechanical performance.
The cost-effectiveness of radiopaque polymers represents another substantial barrier to widespread adoption. High-performance radiopaque additives and the specialized processing techniques required to incorporate them effectively can significantly increase production costs, limiting their use in price-sensitive healthcare markets.
Regulatory hurdles further complicate development efforts. Novel radiopaque materials must undergo extensive testing to demonstrate both safety and efficacy, with requirements varying across different global markets. This regulatory burden increases development timelines and costs, particularly for innovative approaches that lack established precedents.
Finally, there exists a fundamental trade-off between radiopacity and other desirable properties. For instance, increasing radiopacity often results in decreased optical clarity, which can be problematic for applications requiring visual inspection. Similarly, the addition of radiopaque fillers typically increases the density of the polymer, potentially affecting its handling characteristics and performance in specific applications such as minimally invasive devices.
Comparative Analysis of Existing Radiopaque Solutions
01 Radiopaque polymer compositions for medical devices
Biomedical polymers can be formulated with radiopaque materials to enhance visibility under imaging techniques. These compositions typically incorporate radiopaque elements or compounds into polymer matrices to create medical devices that are visible during procedures. The radiopaque agents are distributed throughout the polymer structure or as coatings, allowing for precise visualization while maintaining the mechanical and biocompatible properties required for medical applications.- Radiopaque polymer compositions for medical devices: Biomedical polymers can be formulated with radiopaque materials to enhance visibility under imaging techniques such as X-ray and fluoroscopy. These compositions typically incorporate radiopaque elements or compounds into the polymer matrix, allowing medical devices to be tracked and monitored during procedures. The radiopaque agents can include heavy metals, metal salts, or iodinated compounds that are dispersed throughout the polymer or applied as coatings to achieve the desired level of radiopacity while maintaining biocompatibility.
- Biodegradable radiopaque polymers for implantable devices: Biodegradable polymers with radiopaque properties are designed to provide temporary visibility during implantation and subsequent monitoring, while eventually being absorbed by the body. These materials combine the benefits of biodegradability with radiopacity, eliminating the need for device removal and reducing long-term complications. The polymers can be engineered to control degradation rates and maintain radiopaque features for specific durations, making them suitable for applications such as temporary stents, sutures, and drug delivery systems.
- Nanoparticle-enhanced radiopaque polymer systems: Incorporating radiopaque nanoparticles into biomedical polymers creates advanced materials with enhanced imaging capabilities while maintaining mechanical properties. These nanoparticles, which may include gold, silver, bismuth compounds, or metal oxides, are dispersed throughout the polymer matrix at the nanoscale level. This approach allows for lower concentrations of radiopaque agents while achieving superior contrast under imaging. The nanoparticle systems can be tailored to specific applications by controlling particle size, distribution, and surface modifications to ensure compatibility with the host polymer.
- Radiopaque polymer coatings for medical instruments: Specialized radiopaque coatings can be applied to medical instruments and devices to enhance their visibility during procedures without altering their core structure or function. These coatings typically consist of polymers loaded with radiopaque materials that adhere strongly to the underlying substrate while providing clear visualization under imaging. The coating technology allows for precise application thickness, flexibility, and durability to withstand sterilization and mechanical stress during use. Applications include catheters, guidewires, surgical tools, and minimally invasive instruments.
- Imaging and analysis techniques for radiopaque polymers: Advanced imaging and analysis methods have been developed specifically for evaluating and optimizing radiopaque polymer materials in biomedical applications. These techniques include specialized X-ray protocols, computed tomography algorithms, and image processing software that can quantify radiopacity, detect defects, and assess material distribution within devices. The imaging approaches enable researchers and manufacturers to validate the performance of radiopaque polymers, ensure quality control during production, and monitor their behavior in simulated or actual clinical environments.
02 Metal-based radiopaque additives in biomedical polymers
Metal compounds such as barium sulfate, bismuth compounds, tantalum, and tungsten are commonly incorporated into biomedical polymers to impart radiopacity. These metal-based additives can be dispersed within the polymer matrix at various concentrations to achieve the desired level of radiopacity. The selection of specific metal compounds depends on the required imaging contrast, biocompatibility considerations, and the effect on the mechanical properties of the resulting polymer composite.Expand Specific Solutions03 Radiopaque polymers for implantable medical devices
Specialized radiopaque polymers are designed specifically for implantable medical devices such as stents, catheters, and orthopedic implants. These polymers combine long-term biocompatibility with persistent radiopacity to enable monitoring of the implant position and integrity over time. The radiopaque features can be engineered to provide uniform visibility throughout the device or targeted visibility at specific markers, allowing clinicians to track the implant's position and assess its performance non-invasively.Expand Specific Solutions04 Iodinated polymers for enhanced radiopacity
Iodine-containing polymers represent an important class of inherently radiopaque materials for biomedical applications. These polymers incorporate iodine atoms directly into the polymer backbone or as pendant groups, providing excellent X-ray visibility without the need for additional radiopaque fillers. The covalent bonding of iodine to the polymer structure prevents leaching of the radiopaque component, ensuring long-term imaging capability while maintaining the mechanical properties and biocompatibility of the material.Expand Specific Solutions05 Advanced imaging techniques for radiopaque biomedical polymers
Novel imaging methodologies have been developed to optimize the visualization of radiopaque biomedical polymers. These techniques include specialized X-ray protocols, dual-energy CT imaging, and computer-assisted image processing algorithms that enhance the contrast between the radiopaque polymer and surrounding tissues. These advanced imaging approaches improve the detection sensitivity for radiopaque features in biomedical polymers, enabling more precise guidance during interventional procedures and better long-term monitoring of implanted devices.Expand Specific Solutions
Leading Manufacturers and Research Institutions
The radiopaque features in biomedical polymers market is currently in a growth phase, with increasing adoption across medical device applications. The global market size is expanding due to rising demand for minimally invasive procedures and improved imaging capabilities. Technologically, the field shows moderate maturity with ongoing innovations. Leading players include Boston Scientific and its subsidiaries, which dominate with comprehensive radiopaque polymer solutions for cardiovascular applications. Medtronic and Abbott (St. Jude Medical) maintain strong positions through proprietary technologies. Specialized companies like Biocompatibles UK and BioSphere Medical focus on interventional medicine applications with products like radiopaque embolic beads. Materials suppliers Avient Corp. and DSM IP Assets provide enabling technologies, while academic institutions like Fudan University and Maastricht University contribute to fundamental research advancements.
Avient Corp.
Technical Solution: Avient Corporation (formerly PolyOne) has developed specialized radiopaque polymer compounds under their "Trilliant Healthcare" product line. Their technology focuses on custom-engineered polymer blends incorporating multiple radiopaque fillers including bismuth oxychloride, bismuth subcarbonate, and tungsten at concentrations ranging from 10-40% depending on application requirements[7]. Avient's proprietary processing technology enables the production of ultra-thin radiopaque components while maintaining structural integrity. Their "GLS" technology combines radiopaque fillers with thermoplastic elastomers to create flexible, kink-resistant materials for catheter applications. Avient has also pioneered color-coded radiopaque polymers that provide both visual differentiation and x-ray visibility, addressing the need for component identification during complex procedures[8]. Recent innovations include their "Gradient Technology" that creates controlled variations in radiopacity along the length of a single component, enabling precise positioning while maintaining overall visibility.
Strengths: Highly customizable radiopacity levels; excellent processing characteristics for complex geometries; ability to combine radiopacity with other functional properties like antimicrobial performance. Weaknesses: Batch-to-batch variation can be challenging to control; higher filler loadings may impact long-term durability; potential for increased water absorption in certain formulations.
Boston Scientific Scimed, Inc.
Technical Solution: Boston Scientific Scimed has pioneered hybrid radiopaque polymer systems that combine multiple visualization technologies. Their primary approach utilizes barium sulfate particles (15-25% by weight) embedded in medical-grade polymers like polyurethane and polyethylene[2]. For enhanced visibility, they've developed a dual-layer technology where the inner layer contains higher concentrations of radiopaque materials while the outer layer maintains optimal biocompatibility. Their proprietary "OptiMark" technology incorporates metallic markers at strategic locations combined with uniformly distributed radiopaque fillers, providing both precise positioning capabilities and overall visibility. Boston Scientific has also developed temperature-responsive radiopaque polymers that change visibility characteristics during deployment of certain implantable devices[4]. Their recent innovations include biodegradable radiopaque polymers for temporary implants that maintain visibility during critical healing periods but gradually eliminate foreign material from the body.
Strengths: Excellent balance between radiopacity and mechanical performance; versatile application across multiple device platforms; innovative dual-layer technology provides targeted visibility. Weaknesses: Complex manufacturing processes increase production costs; potential for particle leaching in certain formulations; higher stiffness compared to non-radiopaque alternatives in some applications.
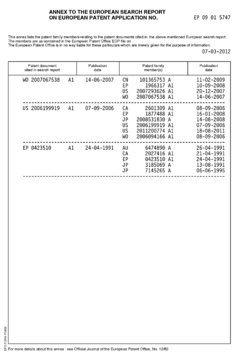
Key Patents and Scientific Breakthroughs
Biocompatible polycarbonate and radiopaque polymer compositions and methods of manufacturing medical devices with same
PatentInactiveEP2204419A3
Innovation
- A biocompatible radiopaque polymer composition combining poly(bisphenol A carbonate) with polyamide and an inorganic radiopaque filler, along with additives like phosphites and functionalized polyolefins, to enhance melt processability and mechanical properties, allowing for improved visualization and mechanical performance in medical devices.
Radiopaque iodinated and iodide-containing crystalline absorbable aliphatic polymeric materials and applications thereof
PatentActiveUS20140336277A1
Innovation
- Development of radiopaque, iodinated, crystalline, aliphatic absorbable polyesters with molecular weights exceeding 5 kDa and specific heat of fusion values, produced through ring-opening polymerization using iodohydroxylic initiators and organometallic catalysts, suitable for medical devices, coatings, and markers.
Biocompatibility and Safety Considerations
The biocompatibility and safety of radiopaque polymers represent critical considerations in their medical application. When introducing radiopaque agents into biomedical polymers, the resulting composite must maintain compatibility with biological systems while providing the desired imaging functionality. The integration of radiopaque elements often alters the material's surface properties, potentially affecting protein adsorption, cellular interactions, and inflammatory responses.
Primary biocompatibility concerns include cytotoxicity, genotoxicity, and immunogenicity of both the base polymer and the radiopaque additives. Studies have demonstrated varying degrees of cellular response depending on the specific radiopaque agent utilized. Barium sulfate, a commonly employed radiopaque filler, generally exhibits good biocompatibility at appropriate concentrations, though particle size and distribution significantly impact tissue response. Bismuth compounds, while effective for radiopacity, have shown potential cytotoxicity at higher concentrations, necessitating careful dosage control.
Leaching of radiopaque agents presents another significant safety consideration. The stability of the radiopaque element within the polymer matrix determines long-term performance and safety. Covalently bound radiopaque moieties typically demonstrate superior retention compared to physically blended additives, reducing the risk of migration and subsequent tissue exposure. Accelerated aging studies reveal that some iodinated compounds may gradually release from polymer matrices, potentially causing localized or systemic toxicity.
Sterilization compatibility represents an additional challenge for radiopaque polymers. Common sterilization methods such as ethylene oxide treatment, gamma irradiation, and steam autoclaving can potentially degrade certain radiopaque additives or alter their distribution within the polymer matrix. This may compromise both imaging efficacy and biocompatibility profiles. Research indicates that iodine-containing compounds often demonstrate superior stability during sterilization compared to some metal-based alternatives.
Regulatory frameworks for radiopaque materials have evolved to address these safety concerns. ISO 10993 standards provide comprehensive guidelines for biological evaluation, including specific protocols for assessing the biocompatibility of materials containing radiopaque elements. The FDA has established additional guidance for radiopaque device submissions, emphasizing the need for thorough characterization of leachable compounds and degradation products.
Recent advances in biocompatibility testing include the development of in vitro models that better simulate in vivo conditions, allowing more accurate prediction of biological responses to radiopaque materials. These models incorporate dynamic flow conditions, three-dimensional tissue structures, and extended exposure periods to better represent clinical scenarios. Such testing methodologies have revealed that surface modification techniques can significantly improve the biocompatibility of radiopaque polymers without compromising their imaging capabilities.
Primary biocompatibility concerns include cytotoxicity, genotoxicity, and immunogenicity of both the base polymer and the radiopaque additives. Studies have demonstrated varying degrees of cellular response depending on the specific radiopaque agent utilized. Barium sulfate, a commonly employed radiopaque filler, generally exhibits good biocompatibility at appropriate concentrations, though particle size and distribution significantly impact tissue response. Bismuth compounds, while effective for radiopacity, have shown potential cytotoxicity at higher concentrations, necessitating careful dosage control.
Leaching of radiopaque agents presents another significant safety consideration. The stability of the radiopaque element within the polymer matrix determines long-term performance and safety. Covalently bound radiopaque moieties typically demonstrate superior retention compared to physically blended additives, reducing the risk of migration and subsequent tissue exposure. Accelerated aging studies reveal that some iodinated compounds may gradually release from polymer matrices, potentially causing localized or systemic toxicity.
Sterilization compatibility represents an additional challenge for radiopaque polymers. Common sterilization methods such as ethylene oxide treatment, gamma irradiation, and steam autoclaving can potentially degrade certain radiopaque additives or alter their distribution within the polymer matrix. This may compromise both imaging efficacy and biocompatibility profiles. Research indicates that iodine-containing compounds often demonstrate superior stability during sterilization compared to some metal-based alternatives.
Regulatory frameworks for radiopaque materials have evolved to address these safety concerns. ISO 10993 standards provide comprehensive guidelines for biological evaluation, including specific protocols for assessing the biocompatibility of materials containing radiopaque elements. The FDA has established additional guidance for radiopaque device submissions, emphasizing the need for thorough characterization of leachable compounds and degradation products.
Recent advances in biocompatibility testing include the development of in vitro models that better simulate in vivo conditions, allowing more accurate prediction of biological responses to radiopaque materials. These models incorporate dynamic flow conditions, three-dimensional tissue structures, and extended exposure periods to better represent clinical scenarios. Such testing methodologies have revealed that surface modification techniques can significantly improve the biocompatibility of radiopaque polymers without compromising their imaging capabilities.
Regulatory Pathways for Radiopaque Medical Materials
The regulatory landscape for radiopaque medical materials varies significantly across global markets, with different regions implementing distinct approval pathways and requirements. In the United States, the Food and Drug Administration (FDA) oversees radiopaque materials through either the 510(k) premarket notification process or the more rigorous Premarket Approval (PMA) pathway, depending on the risk classification of the device incorporating these materials. For most radiopaque polymers used in Class II devices, manufacturers must demonstrate substantial equivalence to a legally marketed predicate device through the 510(k) process.
The European Union has transitioned from the Medical Device Directive (MDD) to the more stringent Medical Device Regulation (MDR), which came into full effect in May 2021. Under the MDR, radiopaque materials face enhanced scrutiny regarding biocompatibility, leachables, and long-term safety profiles. Manufacturers must compile comprehensive technical documentation and clinical evidence to obtain CE marking, with particular emphasis on the chemical characterization of radiopaque additives.
In Japan, the Pharmaceuticals and Medical Devices Agency (PMDA) requires specific testing protocols for radiopaque materials, particularly focusing on their stability under sterilization conditions and potential degradation products. The Japanese regulatory framework places significant emphasis on quality management systems and manufacturing controls for these specialized materials.
International standards play a crucial role in harmonizing regulatory approaches across jurisdictions. ISO 10993 series for biocompatibility testing is particularly relevant for radiopaque polymers, with ISO 10993-18 addressing chemical characterization and ISO 10993-17 focusing on toxicological risk assessment of leachable substances. ASTM F640 specifically addresses radiographic visualization requirements for medical devices.
Recent regulatory trends indicate increasing scrutiny of radiopaque additives, particularly heavy metal-based compounds like barium sulfate and bismuth subcarbonate. Regulatory bodies are requiring more comprehensive leachability studies and long-term biocompatibility data, especially for implantable devices. The FDA's recent guidance on biocompatibility testing emphasizes the need for chemical characterization as a complement to traditional biocompatibility testing.
Emerging regulatory considerations include the environmental impact of radiopaque materials and their disposal, particularly for materials containing heavy metals. Additionally, regulatory bodies are developing frameworks to address novel radiopaque technologies, such as nanoparticle-based contrast agents and biodegradable radiopaque polymers, which present unique safety and efficacy challenges not fully addressed by existing regulatory paradigms.
The European Union has transitioned from the Medical Device Directive (MDD) to the more stringent Medical Device Regulation (MDR), which came into full effect in May 2021. Under the MDR, radiopaque materials face enhanced scrutiny regarding biocompatibility, leachables, and long-term safety profiles. Manufacturers must compile comprehensive technical documentation and clinical evidence to obtain CE marking, with particular emphasis on the chemical characterization of radiopaque additives.
In Japan, the Pharmaceuticals and Medical Devices Agency (PMDA) requires specific testing protocols for radiopaque materials, particularly focusing on their stability under sterilization conditions and potential degradation products. The Japanese regulatory framework places significant emphasis on quality management systems and manufacturing controls for these specialized materials.
International standards play a crucial role in harmonizing regulatory approaches across jurisdictions. ISO 10993 series for biocompatibility testing is particularly relevant for radiopaque polymers, with ISO 10993-18 addressing chemical characterization and ISO 10993-17 focusing on toxicological risk assessment of leachable substances. ASTM F640 specifically addresses radiographic visualization requirements for medical devices.
Recent regulatory trends indicate increasing scrutiny of radiopaque additives, particularly heavy metal-based compounds like barium sulfate and bismuth subcarbonate. Regulatory bodies are requiring more comprehensive leachability studies and long-term biocompatibility data, especially for implantable devices. The FDA's recent guidance on biocompatibility testing emphasizes the need for chemical characterization as a complement to traditional biocompatibility testing.
Emerging regulatory considerations include the environmental impact of radiopaque materials and their disposal, particularly for materials containing heavy metals. Additionally, regulatory bodies are developing frameworks to address novel radiopaque technologies, such as nanoparticle-based contrast agents and biodegradable radiopaque polymers, which present unique safety and efficacy challenges not fully addressed by existing regulatory paradigms.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!