Standards for Testing Biodegradability in Biomedical Polymers
OCT 24, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Biomedical Polymer Biodegradability Background and Objectives
Biodegradable polymers have emerged as a critical innovation in biomedical applications over the past four decades, evolving from simple suture materials to complex drug delivery systems and tissue engineering scaffolds. The development trajectory began in the 1960s with the introduction of synthetic biodegradable sutures, followed by significant advancements in the 1980s and 1990s that expanded applications to controlled drug release systems and implantable devices.
The fundamental principle driving this technological evolution is the ability of these materials to perform their intended therapeutic or diagnostic function for a predetermined period before undergoing controlled degradation and elimination from the body, thus eliminating the need for secondary removal procedures and reducing long-term foreign body responses.
Current biodegradable polymer technologies encompass a diverse range of materials including polyesters (PLA, PGA, PCL), polyanhydrides, polyorthoesters, and natural polymers such as collagen, chitosan, and alginate. Each category offers distinct degradation profiles, mechanical properties, and biocompatibility characteristics that determine their suitability for specific biomedical applications.
The technological landscape is rapidly evolving toward more sophisticated "smart" biodegradable systems that respond to specific biological triggers or environmental conditions. These advanced materials are designed to degrade at rates precisely matched to tissue regeneration timelines or drug release requirements, representing a paradigm shift from passive to active biomaterials.
Despite significant progress, standardization of biodegradability testing remains a critical challenge. Current testing protocols exhibit considerable variability across regulatory jurisdictions, research institutions, and industry practices. This inconsistency creates barriers to translational research and regulatory approval processes, ultimately delaying the clinical implementation of promising technologies.
The primary objective of this technical research is to comprehensively evaluate existing standards for testing biodegradability in biomedical polymers, identify critical gaps in current methodologies, and propose harmonized approaches that accurately predict in vivo performance. Secondary goals include mapping the correlation between in vitro degradation parameters and clinical outcomes, and developing accelerated testing protocols that maintain predictive validity while reducing development timelines.
This research aims to establish a framework for standardized biodegradability testing that addresses the unique requirements of diverse biomedical applications while providing sufficient flexibility to accommodate emerging polymer technologies and novel degradation mechanisms. The ultimate goal is to facilitate more efficient translation of biodegradable polymer innovations from laboratory research to clinical implementation.
The fundamental principle driving this technological evolution is the ability of these materials to perform their intended therapeutic or diagnostic function for a predetermined period before undergoing controlled degradation and elimination from the body, thus eliminating the need for secondary removal procedures and reducing long-term foreign body responses.
Current biodegradable polymer technologies encompass a diverse range of materials including polyesters (PLA, PGA, PCL), polyanhydrides, polyorthoesters, and natural polymers such as collagen, chitosan, and alginate. Each category offers distinct degradation profiles, mechanical properties, and biocompatibility characteristics that determine their suitability for specific biomedical applications.
The technological landscape is rapidly evolving toward more sophisticated "smart" biodegradable systems that respond to specific biological triggers or environmental conditions. These advanced materials are designed to degrade at rates precisely matched to tissue regeneration timelines or drug release requirements, representing a paradigm shift from passive to active biomaterials.
Despite significant progress, standardization of biodegradability testing remains a critical challenge. Current testing protocols exhibit considerable variability across regulatory jurisdictions, research institutions, and industry practices. This inconsistency creates barriers to translational research and regulatory approval processes, ultimately delaying the clinical implementation of promising technologies.
The primary objective of this technical research is to comprehensively evaluate existing standards for testing biodegradability in biomedical polymers, identify critical gaps in current methodologies, and propose harmonized approaches that accurately predict in vivo performance. Secondary goals include mapping the correlation between in vitro degradation parameters and clinical outcomes, and developing accelerated testing protocols that maintain predictive validity while reducing development timelines.
This research aims to establish a framework for standardized biodegradability testing that addresses the unique requirements of diverse biomedical applications while providing sufficient flexibility to accommodate emerging polymer technologies and novel degradation mechanisms. The ultimate goal is to facilitate more efficient translation of biodegradable polymer innovations from laboratory research to clinical implementation.
Market Demand Analysis for Biodegradable Medical Materials
The global market for biodegradable medical materials has experienced significant growth in recent years, driven by increasing environmental concerns and the need for sustainable healthcare solutions. The market value reached approximately $5.7 billion in 2022 and is projected to grow at a compound annual growth rate (CAGR) of 16.2% through 2030, potentially reaching $20.9 billion by the end of the forecast period.
Healthcare facilities worldwide generate substantial medical waste, with polymeric materials constituting a significant portion. According to the World Health Organization, high-income countries generate up to 0.5 kg of hazardous waste per hospital bed per day. This growing environmental burden has created urgent demand for biodegradable alternatives that can reduce medical waste accumulation.
The surgical and wound care segments currently dominate the biodegradable medical materials market, accounting for over 40% of total demand. Biodegradable sutures, in particular, have achieved widespread clinical adoption, with the market valued at $1.3 billion in 2022. Tissue engineering applications represent the fastest-growing segment, with an estimated CAGR of 18.7% through 2030, driven by innovations in regenerative medicine.
Regulatory pressures are increasingly influencing market dynamics. The European Union's Medical Device Regulation (MDR) and similar frameworks worldwide have established stricter requirements for material safety and environmental impact assessment. This regulatory landscape has accelerated demand for standardized biodegradability testing protocols specifically designed for biomedical polymers.
Patient preferences are also shifting market demand. A 2022 survey of 2,500 patients across North America and Europe revealed that 73% expressed concern about the environmental impact of their medical treatments, with 68% indicating willingness to choose biodegradable options when available. This consumer sentiment is pushing healthcare providers to adopt more sustainable materials.
Regional analysis shows North America currently leads the market with a 38% share, followed by Europe at 32% and Asia-Pacific at 24%. However, the Asia-Pacific region is expected to demonstrate the highest growth rate, with China and India emerging as key manufacturing hubs for biodegradable medical polymers.
The COVID-19 pandemic has further accelerated market growth, as the surge in single-use medical items highlighted the environmental consequences of conventional polymers. This has prompted increased investment in biodegradable alternatives, with venture capital funding for startups in this sector reaching $870 million in 2022, a 34% increase from pre-pandemic levels.
Healthcare facilities worldwide generate substantial medical waste, with polymeric materials constituting a significant portion. According to the World Health Organization, high-income countries generate up to 0.5 kg of hazardous waste per hospital bed per day. This growing environmental burden has created urgent demand for biodegradable alternatives that can reduce medical waste accumulation.
The surgical and wound care segments currently dominate the biodegradable medical materials market, accounting for over 40% of total demand. Biodegradable sutures, in particular, have achieved widespread clinical adoption, with the market valued at $1.3 billion in 2022. Tissue engineering applications represent the fastest-growing segment, with an estimated CAGR of 18.7% through 2030, driven by innovations in regenerative medicine.
Regulatory pressures are increasingly influencing market dynamics. The European Union's Medical Device Regulation (MDR) and similar frameworks worldwide have established stricter requirements for material safety and environmental impact assessment. This regulatory landscape has accelerated demand for standardized biodegradability testing protocols specifically designed for biomedical polymers.
Patient preferences are also shifting market demand. A 2022 survey of 2,500 patients across North America and Europe revealed that 73% expressed concern about the environmental impact of their medical treatments, with 68% indicating willingness to choose biodegradable options when available. This consumer sentiment is pushing healthcare providers to adopt more sustainable materials.
Regional analysis shows North America currently leads the market with a 38% share, followed by Europe at 32% and Asia-Pacific at 24%. However, the Asia-Pacific region is expected to demonstrate the highest growth rate, with China and India emerging as key manufacturing hubs for biodegradable medical polymers.
The COVID-19 pandemic has further accelerated market growth, as the surge in single-use medical items highlighted the environmental consequences of conventional polymers. This has prompted increased investment in biodegradable alternatives, with venture capital funding for startups in this sector reaching $870 million in 2022, a 34% increase from pre-pandemic levels.
Current Testing Standards and Technical Challenges
The biodegradability testing landscape for biomedical polymers currently encompasses several established international standards, with ASTM D5338, ISO 14855, and ISO 17088 serving as primary frameworks. These standards provide methodologies for evaluating polymer degradation under controlled composting conditions, measuring CO2 evolution as a key indicator of biodegradation. However, these generalized standards often fail to adequately address the unique environments encountered in biomedical applications, particularly the complex physiological conditions within the human body.
The European Committee for Standardization (CEN) has developed EN 13432 specifically for packaging materials, which has been partially adapted for medical polymers but lacks specificity for in vivo applications. Similarly, ASTM D6400 focuses on compostable plastics rather than biomedical materials, creating a significant gap in standardization for medical-grade biodegradable polymers. This disconnect between existing standards and biomedical requirements represents a major technical challenge in the field.
Current testing protocols predominantly rely on in vitro enzymatic degradation assays and simulated body fluid (SBF) immersion tests. While these methods provide valuable preliminary data, they frequently fail to replicate the complex biological responses and mechanical stresses present in actual physiological environments. The correlation between in vitro degradation rates and in vivo performance remains problematic, with studies showing discrepancies of up to 40% between laboratory predictions and clinical outcomes.
A significant technical challenge lies in the standardization of accelerated aging tests for biodegradable polymers. The time-dependent nature of biodegradation necessitates reliable methods to predict long-term performance without extending testing periods beyond practical timeframes. Current approaches using elevated temperatures or concentrated enzyme solutions often alter degradation mechanisms, rendering results questionable for predicting real-world performance.
The heterogeneity of implantation sites presents another substantial challenge. Biodegradable polymers may encounter vastly different physiological conditions depending on whether they are deployed in vascular, orthopedic, or soft tissue environments. Current standards lack sufficient guidance for site-specific testing protocols, leading to inconsistent evaluation methodologies across research institutions and manufacturers.
Regulatory frameworks further complicate standardization efforts. The FDA's guidance on biodegradable polymers emphasizes safety and efficacy but provides limited direction on specific testing methodologies. Similarly, the European Medicines Agency (EMA) requires demonstration of degradation profiles but has not established harmonized testing protocols. This regulatory ambiguity has resulted in fragmented approaches to biodegradability testing, hindering cross-comparison of different biomedical polymers and slowing innovation in the field.
The European Committee for Standardization (CEN) has developed EN 13432 specifically for packaging materials, which has been partially adapted for medical polymers but lacks specificity for in vivo applications. Similarly, ASTM D6400 focuses on compostable plastics rather than biomedical materials, creating a significant gap in standardization for medical-grade biodegradable polymers. This disconnect between existing standards and biomedical requirements represents a major technical challenge in the field.
Current testing protocols predominantly rely on in vitro enzymatic degradation assays and simulated body fluid (SBF) immersion tests. While these methods provide valuable preliminary data, they frequently fail to replicate the complex biological responses and mechanical stresses present in actual physiological environments. The correlation between in vitro degradation rates and in vivo performance remains problematic, with studies showing discrepancies of up to 40% between laboratory predictions and clinical outcomes.
A significant technical challenge lies in the standardization of accelerated aging tests for biodegradable polymers. The time-dependent nature of biodegradation necessitates reliable methods to predict long-term performance without extending testing periods beyond practical timeframes. Current approaches using elevated temperatures or concentrated enzyme solutions often alter degradation mechanisms, rendering results questionable for predicting real-world performance.
The heterogeneity of implantation sites presents another substantial challenge. Biodegradable polymers may encounter vastly different physiological conditions depending on whether they are deployed in vascular, orthopedic, or soft tissue environments. Current standards lack sufficient guidance for site-specific testing protocols, leading to inconsistent evaluation methodologies across research institutions and manufacturers.
Regulatory frameworks further complicate standardization efforts. The FDA's guidance on biodegradable polymers emphasizes safety and efficacy but provides limited direction on specific testing methodologies. Similarly, the European Medicines Agency (EMA) requires demonstration of degradation profiles but has not established harmonized testing protocols. This regulatory ambiguity has resulted in fragmented approaches to biodegradability testing, hindering cross-comparison of different biomedical polymers and slowing innovation in the field.
Established Testing Protocols and Validation Methods
01 Biodegradable polymers for medical implants
Biodegradable polymers are used in medical implants to provide temporary support before being absorbed by the body. These polymers can be engineered with specific degradation rates to match tissue healing times. Common biodegradable polymers for implants include polylactic acid (PLA), polyglycolic acid (PGA), and their copolymers. These materials eliminate the need for secondary surgeries to remove implants and reduce long-term foreign body reactions.- Biodegradable polymers for medical implants: Biodegradable polymers are used in medical implants to provide temporary support before being absorbed by the body. These polymers can be engineered with specific degradation rates to match tissue healing times. Common biodegradable polymers for implants include polylactic acid (PLA), polyglycolic acid (PGA), and their copolymers. These materials eliminate the need for secondary surgeries to remove implants and reduce long-term foreign body reactions.
- Drug delivery systems using biodegradable polymers: Biodegradable polymers are formulated into drug delivery systems that release therapeutic agents as they degrade. These systems can provide controlled release of medications over extended periods, improving patient compliance and therapeutic outcomes. The degradation rate can be tailored by adjusting polymer composition, molecular weight, and crystallinity to achieve desired drug release profiles. These systems are particularly valuable for delivering drugs to specific tissues or for extended-release applications.
- Natural and synthetic biodegradable polymer blends: Blending natural polymers (like collagen, chitosan, or alginate) with synthetic biodegradable polymers creates materials with enhanced properties for biomedical applications. These blends combine the biocompatibility of natural polymers with the tunable mechanical properties of synthetic ones. The resulting composites often show improved cell adhesion, proliferation, and tissue integration compared to purely synthetic materials, while maintaining predictable degradation profiles.
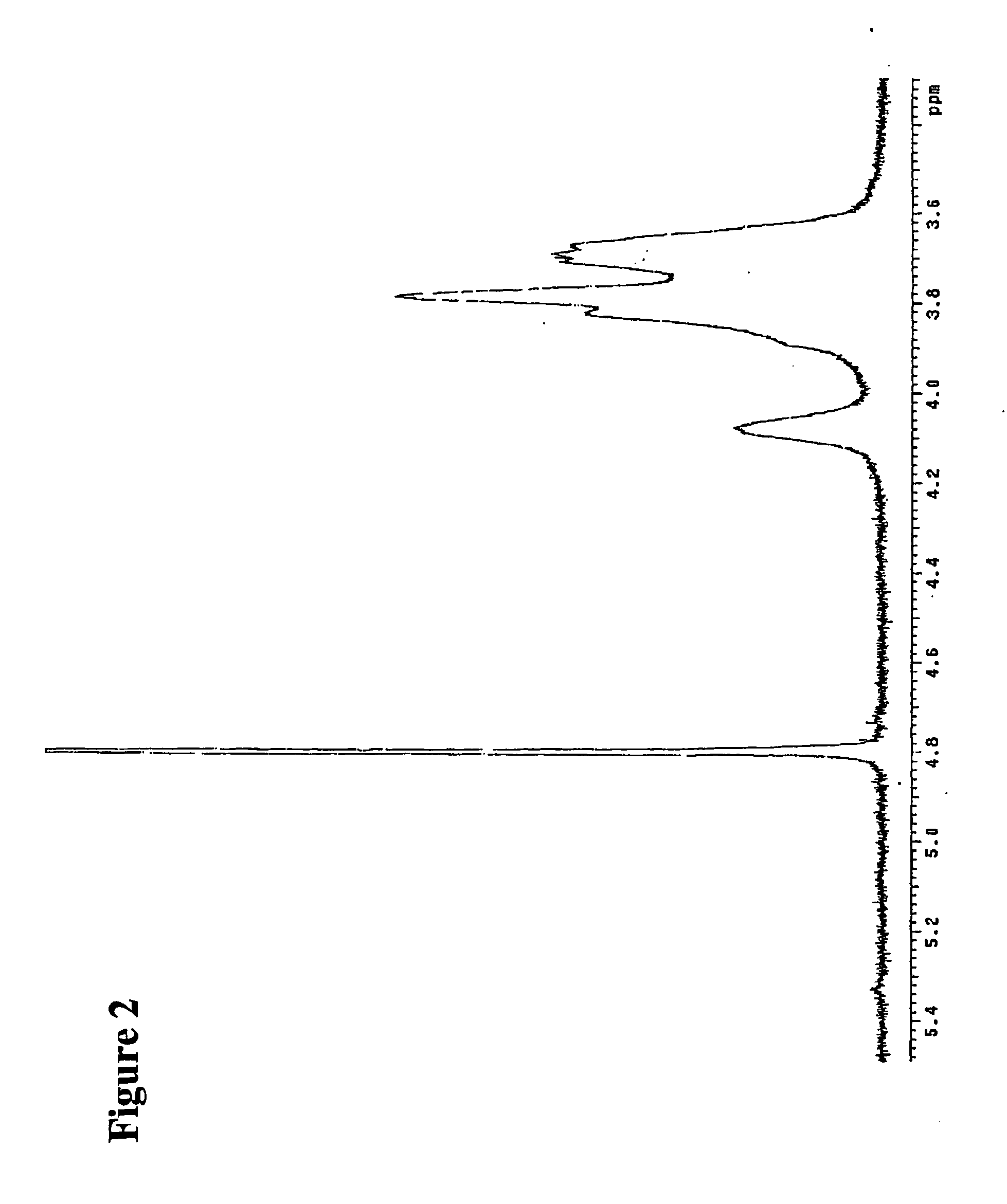
- Enzymatic and hydrolytic degradation mechanisms: Biodegradable polymers in biomedical applications degrade through enzymatic and/or hydrolytic mechanisms. Hydrolytic degradation occurs when water molecules cleave polymer chains, while enzymatic degradation involves specific biological catalysts. Understanding these mechanisms allows for designing polymers with predictable degradation rates in various biological environments. Factors affecting degradation include polymer chemistry, crystallinity, hydrophilicity, molecular weight, and the presence of specific functional groups that are susceptible to enzymatic attack.
- Surface modifications to control biodegradation: Surface modifications of biodegradable polymers can control their degradation rates and improve biocompatibility. Techniques include plasma treatment, chemical grafting, and coating with bioactive molecules. These modifications can enhance cell adhesion, reduce inflammatory responses, and provide antimicrobial properties while maintaining the bulk degradation characteristics. By creating specific surface chemistries, the initial biological response to the material can be optimized without significantly altering the mechanical properties or overall degradation timeline.
02 Drug delivery systems using biodegradable polymers
Biodegradable polymers are formulated into drug delivery systems that release therapeutic agents as they degrade. These systems can provide controlled release of medications over extended periods, improving treatment efficacy and patient compliance. The degradation rate can be tailored by modifying polymer composition, molecular weight, and crystallinity. This approach is particularly valuable for delivering drugs to specific tissues or for maintaining therapeutic drug levels without frequent dosing.Expand Specific Solutions03 Natural and synthetic biodegradable polymer blends
Blending natural polymers (like collagen, chitosan, or alginate) with synthetic biodegradable polymers creates materials with enhanced properties for biomedical applications. These blends combine the biocompatibility of natural polymers with the tunable mechanical properties of synthetic ones. The resulting composites can better mimic natural tissue environments while maintaining controlled degradation profiles. Such blends are used in tissue engineering scaffolds, wound dressings, and other regenerative medicine applications.Expand Specific Solutions04 Enzymatic and hydrolytic degradation mechanisms
Biodegradable polymers in biomedical applications degrade through enzymatic and/or hydrolytic mechanisms. Hydrolytic degradation occurs when water molecules break polymer chains, while enzymatic degradation involves specific biological catalysts. Understanding these mechanisms allows for designing polymers with predictable degradation rates in physiological environments. Factors affecting degradation include polymer chemistry, crystallinity, hydrophilicity, molecular weight, and the presence of specific functional groups that are susceptible to enzymatic attack.Expand Specific Solutions05 Novel biodegradable polymer synthesis techniques
Advanced synthesis techniques are being developed to create biodegradable polymers with enhanced properties for biomedical applications. These include ring-opening polymerization, controlled radical polymerization, and click chemistry approaches. Such methods allow for precise control over molecular architecture, incorporation of functional groups, and creation of block copolymers with specific degradation profiles. These novel polymers can be designed with stimuli-responsive degradation triggered by pH, temperature, or specific biological environments.Expand Specific Solutions
Leading Organizations and Regulatory Bodies in Biodegradability Standards
The biodegradability testing standards for biomedical polymers market is in a growth phase, with increasing regulatory focus driving market expansion. The global market is estimated to reach $2.5-3 billion by 2025, growing at 8-10% CAGR. Technologically, the field shows moderate maturity with established protocols but ongoing innovation. Key players represent diverse sectors: healthcare institutions (The General Hospital Corp.), chemical giants (BASF, Sinopec), specialized polymer developers (Kingfa Sci. & Tech.), pharmaceutical companies (Mersana Therapeutics, Allergan), and research institutions (MIT, Tsinghua University). Companies like Exotech Bio Solutions and Medtronic Vascular are specifically advancing biodegradable medical polymers, while academic-industry partnerships are accelerating standardization efforts and commercial applications.
BASF Corp.
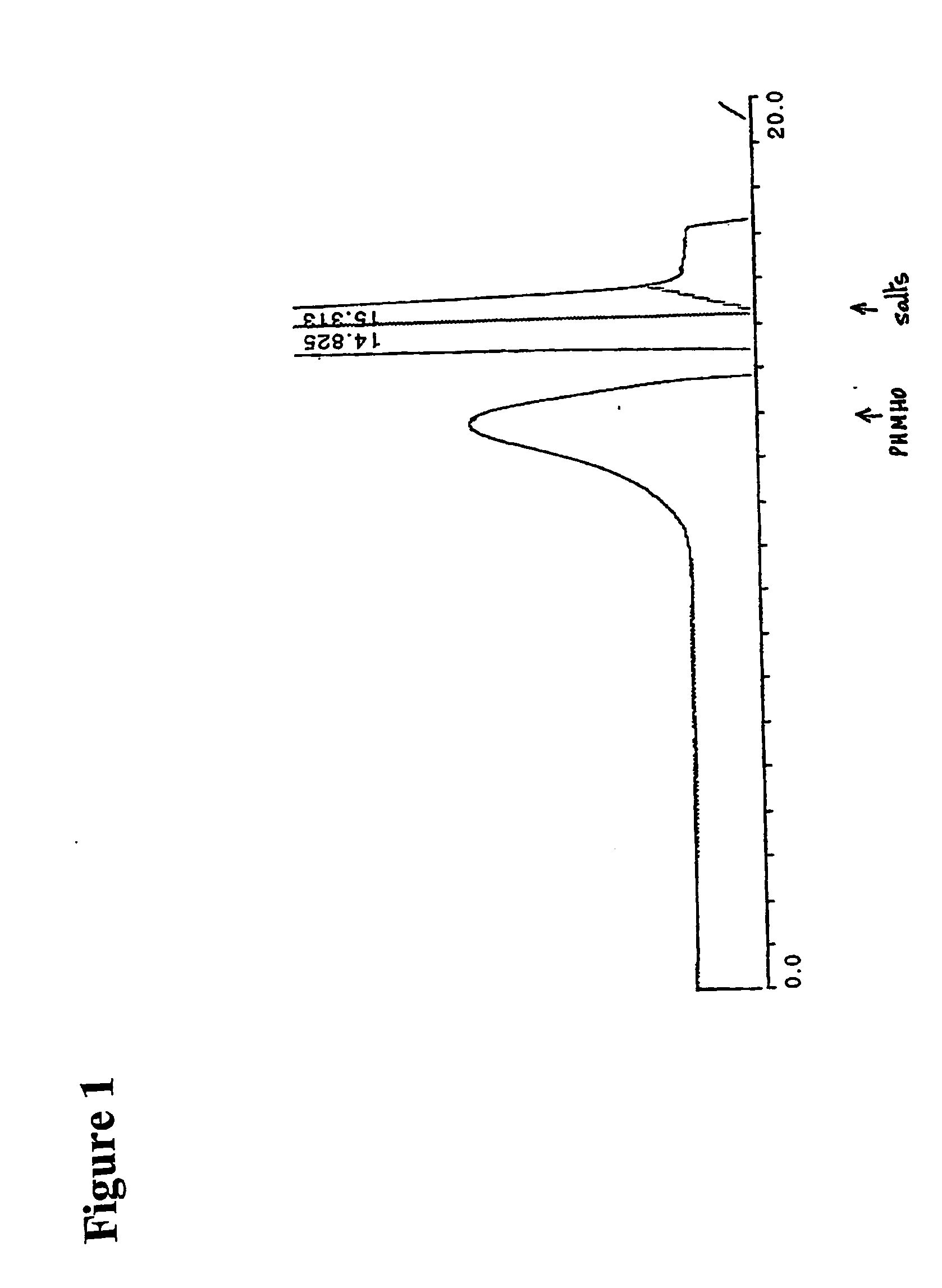
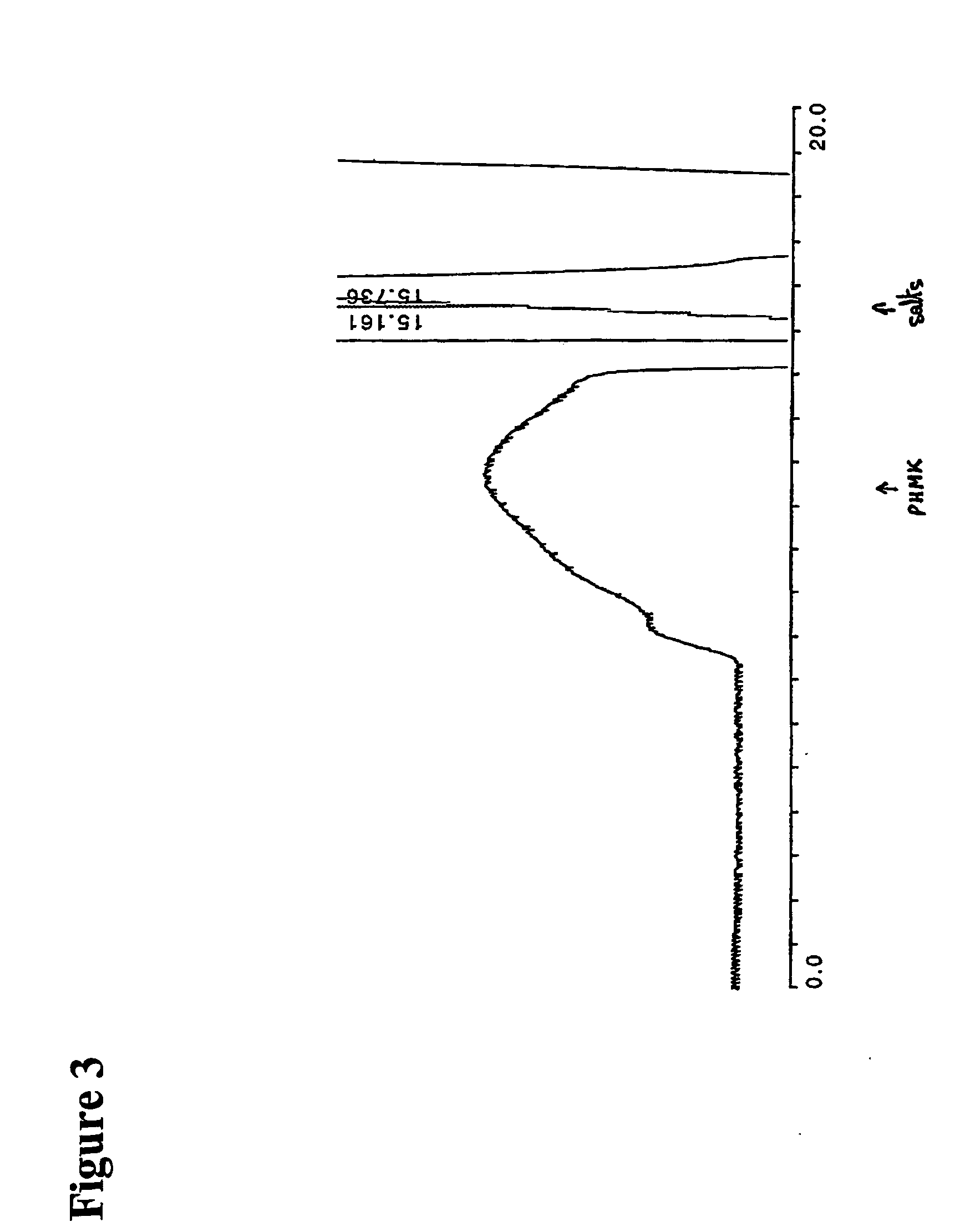
Technical Solution: BASF has established a comprehensive biodegradability testing platform for biomedical polymers that integrates standardized methods with application-specific protocols. Their approach begins with material characterization using differential scanning calorimetry (DSC), thermogravimetric analysis (TGA), and Fourier-transform infrared spectroscopy (FTIR) to establish baseline properties. BASF employs multiple standardized biodegradation tests including ISO 14851 (aqueous medium), ISO 14852 (CO2 evolution), and ASTM D5338 (controlled composting conditions), adapting these established protocols specifically for biomedical applications. Their testing framework incorporates specialized enzymatic degradation studies using relevant human enzymes like lipases and esterases at physiological concentrations. BASF has developed accelerated aging protocols that correlate with real-time degradation through mathematical modeling, allowing for reliable prediction of long-term performance. Their methodology includes cytotoxicity testing of degradation products using standardized cell lines and assessment of local tissue response through histopathological evaluation.
Strengths: Comprehensive integration of established international standards with biomedical-specific protocols; extensive material characterization capabilities; strong correlation between accelerated and real-time testing. Weaknesses: Testing framework primarily optimized for thermoplastic polymers rather than all biomedical polymer types; some protocols may overestimate degradation rates compared to actual in vivo performance.
Medtronic Vascular, Inc.
Technical Solution: Medtronic has developed a proprietary testing framework for biodegradable polymers used in vascular stents and other implantable devices. Their approach centers on a multi-phase evaluation system that begins with basic material characterization and progresses through increasingly complex biological environments. The company employs specialized bioreactors that simulate physiological conditions including pulsatile flow, temperature fluctuations, and enzymatic activity to assess degradation under clinically relevant conditions. Medtronic's testing standards incorporate both surface and bulk erosion measurements using scanning electron microscopy (SEM) and gel permeation chromatography (GPC) to track morphological and molecular weight changes over time. Their methodology includes standardized protocols for extracting and analyzing degradation products to assess potential toxicity and inflammatory responses. Medtronic has also developed computational models that can predict degradation behavior based on initial polymer characteristics and environmental conditions.
Strengths: Highly specialized testing environments that closely mimic in vivo conditions; comprehensive toxicological assessment of degradation products; strong regulatory acceptance of testing protocols. Weaknesses: Testing methods are primarily optimized for vascular applications and may require modification for other biomedical contexts; proprietary nature of some testing protocols limits broader standardization across the industry.
Critical Analysis of Standardized Testing Procedures
Biodegradable polyketal polymers and methods for their formation and use
PatentInactiveUS20060069230A1
Innovation
- Development of biodegradable biocompatible polyketals with ketal groups within the main chain, which are hydrophilic and pharmaceutically useful, allowing for controlled drug release and chiral separation through the use of polyketal structures that can be modified for specific properties and applications.
A container
PatentWO2020240001A1
Innovation
- A container formed from bioplastic materials, specifically biodegradable biopolymers like polylactic acid or polyhydroxyalkanoate, combined with plant fibers for reinforcement, which are impermeable to moisture and conform to European standards for biodegradability, disintegrability, and ecotoxicity, ensuring minimal environmental impact.
Environmental Impact and Sustainability Considerations
The environmental impact of biomedical polymers represents a critical consideration in the development and implementation of biodegradability standards. The healthcare industry generates substantial plastic waste, with an estimated 25% of hospital waste consisting of plastic materials. Biomedical polymers, when improperly disposed of, contribute significantly to environmental pollution, persisting in ecosystems for decades or centuries.
Biodegradable biomedical polymers offer a promising solution to mitigate these environmental concerns. However, comprehensive assessment of their environmental footprint requires evaluation beyond mere degradation rates. Life cycle assessment (LCA) methodologies have emerged as essential tools for quantifying the environmental impact of these materials from production to disposal. Recent studies indicate that some biodegradable alternatives may actually require more energy during manufacturing than conventional polymers, potentially offsetting their end-of-life benefits.
Water consumption represents another crucial environmental factor. The production of certain biodegradable polymers, particularly those derived from agricultural feedstocks, can require substantial water resources. Standards for biodegradability testing must therefore incorporate metrics for water efficiency throughout the material's life cycle, not merely during the degradation phase.
Carbon footprint considerations have gained prominence in biodegradability standards development. The greenhouse gas emissions associated with biomedical polymer production, use, and degradation must be systematically quantified. Research indicates that some biodegradable polymers release methane during decomposition, a greenhouse gas with warming potential 25 times greater than carbon dioxide, necessitating careful evaluation of degradation byproducts.
Toxicity of degradation products presents another environmental challenge. As biomedical polymers break down, they may release compounds that impact aquatic ecosystems or soil health. Standardized testing protocols must assess the ecotoxicological profile of these degradation intermediates and end products across various environmental compartments.
Resource conservation principles increasingly influence biodegradability standards. The concept of circular economy has gained traction, emphasizing the importance of designing biomedical polymers that not only degrade safely but also enable resource recovery. Standards are evolving to evaluate whether degradation products can serve as nutrients for subsequent biological processes, truly closing the material loop.
Regulatory frameworks worldwide are increasingly incorporating sustainability metrics into biodegradability standards. The European Union's Single-Use Plastics Directive and similar initiatives in other regions are driving the development of more comprehensive testing protocols that address environmental impact throughout the material lifecycle, not merely end-of-life degradation.
Biodegradable biomedical polymers offer a promising solution to mitigate these environmental concerns. However, comprehensive assessment of their environmental footprint requires evaluation beyond mere degradation rates. Life cycle assessment (LCA) methodologies have emerged as essential tools for quantifying the environmental impact of these materials from production to disposal. Recent studies indicate that some biodegradable alternatives may actually require more energy during manufacturing than conventional polymers, potentially offsetting their end-of-life benefits.
Water consumption represents another crucial environmental factor. The production of certain biodegradable polymers, particularly those derived from agricultural feedstocks, can require substantial water resources. Standards for biodegradability testing must therefore incorporate metrics for water efficiency throughout the material's life cycle, not merely during the degradation phase.
Carbon footprint considerations have gained prominence in biodegradability standards development. The greenhouse gas emissions associated with biomedical polymer production, use, and degradation must be systematically quantified. Research indicates that some biodegradable polymers release methane during decomposition, a greenhouse gas with warming potential 25 times greater than carbon dioxide, necessitating careful evaluation of degradation byproducts.
Toxicity of degradation products presents another environmental challenge. As biomedical polymers break down, they may release compounds that impact aquatic ecosystems or soil health. Standardized testing protocols must assess the ecotoxicological profile of these degradation intermediates and end products across various environmental compartments.
Resource conservation principles increasingly influence biodegradability standards. The concept of circular economy has gained traction, emphasizing the importance of designing biomedical polymers that not only degrade safely but also enable resource recovery. Standards are evolving to evaluate whether degradation products can serve as nutrients for subsequent biological processes, truly closing the material loop.
Regulatory frameworks worldwide are increasingly incorporating sustainability metrics into biodegradability standards. The European Union's Single-Use Plastics Directive and similar initiatives in other regions are driving the development of more comprehensive testing protocols that address environmental impact throughout the material lifecycle, not merely end-of-life degradation.
Clinical Safety and Biocompatibility Requirements
The clinical safety and biocompatibility requirements for biodegradable polymers in biomedical applications are governed by stringent regulatory frameworks established by organizations such as the FDA, EMA, and ISO. These requirements ensure that materials implanted in the human body do not elicit adverse biological responses and degrade in a controlled, predictable manner without producing toxic byproducts.
ISO 10993 series, particularly ISO 10993-1, provides a comprehensive framework for evaluating the biocompatibility of medical devices, including those made from biodegradable polymers. This standard outlines a systematic approach to biological evaluation, requiring manufacturers to assess cytotoxicity, sensitization, irritation, acute systemic toxicity, and genotoxicity at minimum. For long-term implantable devices, additional tests for subchronic toxicity, carcinogenicity, and reproductive/developmental toxicity may be necessary.
For biodegradable polymers specifically, the degradation products require particular scrutiny. ASTM F1635 addresses the in vitro degradation testing of hydrolytically degradable polymers, while ASTM F2902 covers the standard guide for assessment of absorbable polymeric implants. These standards help evaluate whether degradation byproducts might cause local or systemic toxicity over time.
The FDA's guidance document "Use of International Standard ISO 10993-1" provides additional context for applying these standards in regulatory submissions. It emphasizes the importance of considering the final finished form of the device, processing methods, sterilization procedures, and the nature and duration of body contact when assessing biocompatibility.
Clinical safety assessment must also consider the mechanical properties of biodegradable polymers during degradation. As these materials break down, their structural integrity changes, potentially affecting device functionality and safety. Standards such as ASTM F2150 address the characterization of degradation behavior under physiological conditions.
Immunological considerations form another critical aspect of clinical safety requirements. Biodegradable polymers must not trigger excessive inflammatory responses or foreign body reactions. Tests for complement activation, immunogenicity, and inflammatory cytokine production are often required to ensure immunological compatibility.
The regulatory landscape continues to evolve as new biodegradable materials emerge. Recent updates to standards increasingly emphasize the need for real-time degradation studies that better simulate in vivo conditions, moving beyond simplified accelerated testing methods. Additionally, there is growing recognition of the importance of patient-specific factors in biodegradation rates, necessitating more personalized approaches to safety assessment.
ISO 10993 series, particularly ISO 10993-1, provides a comprehensive framework for evaluating the biocompatibility of medical devices, including those made from biodegradable polymers. This standard outlines a systematic approach to biological evaluation, requiring manufacturers to assess cytotoxicity, sensitization, irritation, acute systemic toxicity, and genotoxicity at minimum. For long-term implantable devices, additional tests for subchronic toxicity, carcinogenicity, and reproductive/developmental toxicity may be necessary.
For biodegradable polymers specifically, the degradation products require particular scrutiny. ASTM F1635 addresses the in vitro degradation testing of hydrolytically degradable polymers, while ASTM F2902 covers the standard guide for assessment of absorbable polymeric implants. These standards help evaluate whether degradation byproducts might cause local or systemic toxicity over time.
The FDA's guidance document "Use of International Standard ISO 10993-1" provides additional context for applying these standards in regulatory submissions. It emphasizes the importance of considering the final finished form of the device, processing methods, sterilization procedures, and the nature and duration of body contact when assessing biocompatibility.
Clinical safety assessment must also consider the mechanical properties of biodegradable polymers during degradation. As these materials break down, their structural integrity changes, potentially affecting device functionality and safety. Standards such as ASTM F2150 address the characterization of degradation behavior under physiological conditions.
Immunological considerations form another critical aspect of clinical safety requirements. Biodegradable polymers must not trigger excessive inflammatory responses or foreign body reactions. Tests for complement activation, immunogenicity, and inflammatory cytokine production are often required to ensure immunological compatibility.
The regulatory landscape continues to evolve as new biodegradable materials emerge. Recent updates to standards increasingly emphasize the need for real-time degradation studies that better simulate in vivo conditions, moving beyond simplified accelerated testing methods. Additionally, there is growing recognition of the importance of patient-specific factors in biodegradation rates, necessitating more personalized approaches to safety assessment.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!