Immune-competent lung-on-chip models to study severe COVID-19 endothelial damage mechanisms
SEP 2, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
COVID-19 Lung-on-Chip Background and Objectives
The COVID-19 pandemic has emerged as one of the most significant global health crises of the 21st century, with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causing unprecedented morbidity and mortality worldwide. Since its identification in late 2019, the virus has demonstrated a remarkable ability to damage multiple organ systems, with the lungs being the primary target. The pathophysiology of severe COVID-19 is characterized by significant endothelial damage, leading to vascular leakage, inflammation, and thrombotic complications.
Traditional research models have proven insufficient in fully elucidating the complex mechanisms underlying COVID-19 pathogenesis. Animal models, while valuable, fail to recapitulate human-specific immune responses and vascular pathology. Conventional in vitro cell culture systems lack the architectural complexity and physiological relevance necessary to study the intricate interactions between the virus, lung epithelium, endothelium, and immune components.
Lung-on-chip technology represents a revolutionary approach in biomedical research, offering a dynamic microfluidic platform that mimics the structural and functional aspects of human lung tissue. These advanced microphysiological systems incorporate multiple cell types arranged in a three-dimensional architecture, subjected to mechanical forces that simulate breathing. The integration of immune components into these models marks a significant advancement, enabling the study of immune-mediated endothelial damage in COVID-19.
The evolution of lung-on-chip technology has accelerated in response to the pandemic, with researchers worldwide developing increasingly sophisticated models. Early iterations focused primarily on epithelial-endothelial interfaces, while newer generations incorporate immune cells, allowing for more comprehensive studies of inflammatory responses and cytokine storms characteristic of severe COVID-19.
The primary objective of immune-competent lung-on-chip models is to establish a physiologically relevant platform for investigating the mechanisms of SARS-CoV-2-induced endothelial damage. These models aim to elucidate the viral entry processes, the subsequent immune response, and the cascade of events leading to endothelial dysfunction and vascular complications.
Additional goals include identifying potential therapeutic targets by dissecting the molecular pathways involved in COVID-19 pathogenesis, evaluating the efficacy of existing and novel antiviral and anti-inflammatory agents, and developing personalized medicine approaches through patient-specific models. Furthermore, these platforms seek to predict long-term vascular consequences of COVID-19 infection, contributing to our understanding of "long COVID" syndrome.
The technological trajectory points toward increasingly complex models incorporating additional tissue components and systemic interactions, potentially leading to multi-organ-on-chip systems that can capture the systemic nature of severe COVID-19. The ultimate aim is to establish predictive models that can accelerate therapeutic development and improve clinical outcomes for COVID-19 patients with severe endothelial complications.
Traditional research models have proven insufficient in fully elucidating the complex mechanisms underlying COVID-19 pathogenesis. Animal models, while valuable, fail to recapitulate human-specific immune responses and vascular pathology. Conventional in vitro cell culture systems lack the architectural complexity and physiological relevance necessary to study the intricate interactions between the virus, lung epithelium, endothelium, and immune components.
Lung-on-chip technology represents a revolutionary approach in biomedical research, offering a dynamic microfluidic platform that mimics the structural and functional aspects of human lung tissue. These advanced microphysiological systems incorporate multiple cell types arranged in a three-dimensional architecture, subjected to mechanical forces that simulate breathing. The integration of immune components into these models marks a significant advancement, enabling the study of immune-mediated endothelial damage in COVID-19.
The evolution of lung-on-chip technology has accelerated in response to the pandemic, with researchers worldwide developing increasingly sophisticated models. Early iterations focused primarily on epithelial-endothelial interfaces, while newer generations incorporate immune cells, allowing for more comprehensive studies of inflammatory responses and cytokine storms characteristic of severe COVID-19.
The primary objective of immune-competent lung-on-chip models is to establish a physiologically relevant platform for investigating the mechanisms of SARS-CoV-2-induced endothelial damage. These models aim to elucidate the viral entry processes, the subsequent immune response, and the cascade of events leading to endothelial dysfunction and vascular complications.
Additional goals include identifying potential therapeutic targets by dissecting the molecular pathways involved in COVID-19 pathogenesis, evaluating the efficacy of existing and novel antiviral and anti-inflammatory agents, and developing personalized medicine approaches through patient-specific models. Furthermore, these platforms seek to predict long-term vascular consequences of COVID-19 infection, contributing to our understanding of "long COVID" syndrome.
The technological trajectory points toward increasingly complex models incorporating additional tissue components and systemic interactions, potentially leading to multi-organ-on-chip systems that can capture the systemic nature of severe COVID-19. The ultimate aim is to establish predictive models that can accelerate therapeutic development and improve clinical outcomes for COVID-19 patients with severe endothelial complications.
Market Analysis for Advanced COVID-19 Research Platforms
The COVID-19 research platform market has experienced unprecedented growth since the pandemic's onset, with lung-on-chip technology emerging as a critical segment. Current market valuations indicate the global organ-on-chip market reached $112 million in 2022, with projections suggesting a compound annual growth rate of 29.2% through 2030, potentially reaching $1.24 billion.
Specifically for COVID-19 research applications, immune-competent lung-on-chip platforms represent approximately 18% of this market, with accelerated adoption rates observed since 2020. This growth is primarily driven by substantial research funding redirected toward understanding SARS-CoV-2 pathophysiology, particularly the endothelial damage mechanisms in severe cases.
Key market drivers include the urgent need for alternatives to traditional animal models, which have proven inadequate for studying COVID-19's unique human pathology. The lung-on-chip models offer superior translational value by incorporating human cells and mimicking the complex microenvironment of lung tissue, including immune components critical for understanding cytokine storms and endothelial damage.
Demand analysis reveals three primary market segments: pharmaceutical companies seeking drug development platforms, academic research institutions investigating disease mechanisms, and government agencies focused on pandemic preparedness. Pharmaceutical investment in these technologies has increased by 43% since 2020, reflecting the strategic value of these platforms in accelerating therapeutic development.
Regional market distribution shows North America leading with 42% market share, followed by Europe (31%) and Asia-Pacific (22%), with the latter showing the fastest growth rate at 34.5% annually. This geographic distribution correlates strongly with research funding allocation and biotechnology infrastructure development.
Customer needs assessment indicates growing demand for increasingly sophisticated models that can incorporate multiple immune cell types and reproduce vascular complications. End-users particularly value platforms that can maintain viable cultures for extended periods (14+ days) to study long-term effects of viral infection and potential treatments.
Market forecasts suggest the immune-competent lung-on-chip segment will outpace the broader organ-on-chip market growth by approximately 7-9 percentage points annually through 2025, driven by continued COVID-19 research needs and expanding applications to other respiratory conditions and drug development pipelines.
Specifically for COVID-19 research applications, immune-competent lung-on-chip platforms represent approximately 18% of this market, with accelerated adoption rates observed since 2020. This growth is primarily driven by substantial research funding redirected toward understanding SARS-CoV-2 pathophysiology, particularly the endothelial damage mechanisms in severe cases.
Key market drivers include the urgent need for alternatives to traditional animal models, which have proven inadequate for studying COVID-19's unique human pathology. The lung-on-chip models offer superior translational value by incorporating human cells and mimicking the complex microenvironment of lung tissue, including immune components critical for understanding cytokine storms and endothelial damage.
Demand analysis reveals three primary market segments: pharmaceutical companies seeking drug development platforms, academic research institutions investigating disease mechanisms, and government agencies focused on pandemic preparedness. Pharmaceutical investment in these technologies has increased by 43% since 2020, reflecting the strategic value of these platforms in accelerating therapeutic development.
Regional market distribution shows North America leading with 42% market share, followed by Europe (31%) and Asia-Pacific (22%), with the latter showing the fastest growth rate at 34.5% annually. This geographic distribution correlates strongly with research funding allocation and biotechnology infrastructure development.
Customer needs assessment indicates growing demand for increasingly sophisticated models that can incorporate multiple immune cell types and reproduce vascular complications. End-users particularly value platforms that can maintain viable cultures for extended periods (14+ days) to study long-term effects of viral infection and potential treatments.
Market forecasts suggest the immune-competent lung-on-chip segment will outpace the broader organ-on-chip market growth by approximately 7-9 percentage points annually through 2025, driven by continued COVID-19 research needs and expanding applications to other respiratory conditions and drug development pipelines.
Current Challenges in Modeling COVID-19 Endothelial Damage
Despite significant advancements in lung-on-chip technology, modeling COVID-19 endothelial damage presents numerous challenges that impede comprehensive understanding of disease mechanisms. Current in vitro models struggle to accurately replicate the complex immune-endothelial interactions characteristic of severe COVID-19 infection, particularly the cytokine storm and subsequent vascular damage.
A primary limitation is the difficulty in recreating the complete human immune response within these microfluidic systems. While some models incorporate selected immune cells, they rarely capture the full spectrum of immune components involved in COVID-19 pathogenesis, including various lymphocyte populations, complement activation, and antibody responses that contribute to endothelial damage.
The temporal dynamics of COVID-19 progression represent another significant challenge. Severe cases typically develop over days to weeks, with cascading inflammatory events that are difficult to sustain in chip-based systems, which often have limited viability periods. This temporal constraint restricts the ability to observe the complete evolution of endothelial damage from initial infection to severe manifestations.
Achieving physiologically relevant tissue architecture poses additional difficulties. The lung's complex three-dimensional structure, with its air-blood barrier and specialized endothelial cells, is challenging to recreate with current fabrication techniques. Most models simplify this architecture, potentially missing critical aspects of virus-endothelium interactions that occur at anatomically specific sites.
The integration of patient-specific factors remains problematic. Individual variations in ACE2 receptor expression, pre-existing endothelial dysfunction, and genetic predispositions significantly influence COVID-19 severity but are rarely incorporated into standardized models. This limits the translational value of research findings to diverse patient populations.
Technical challenges in maintaining sterile conditions while allowing viral infection further complicate research efforts. Introducing SARS-CoV-2 into lung-on-chip systems requires specialized containment facilities and protocols that are not widely available, restricting widespread adoption of these models for COVID-19 research.
The validation of model findings against clinical observations presents another hurdle. The rapid evolution of COVID-19 variants with different endothelial tropism and damage mechanisms necessitates continuous updating of models, creating a moving target for researchers attempting to establish clinically relevant systems.
Interdisciplinary expertise requirements further limit progress in this field. Effective COVID-19 endothelial damage modeling demands collaboration between virologists, immunologists, bioengineers, and clinicians—a combination that few research institutions can readily assemble, especially under pandemic conditions.
A primary limitation is the difficulty in recreating the complete human immune response within these microfluidic systems. While some models incorporate selected immune cells, they rarely capture the full spectrum of immune components involved in COVID-19 pathogenesis, including various lymphocyte populations, complement activation, and antibody responses that contribute to endothelial damage.
The temporal dynamics of COVID-19 progression represent another significant challenge. Severe cases typically develop over days to weeks, with cascading inflammatory events that are difficult to sustain in chip-based systems, which often have limited viability periods. This temporal constraint restricts the ability to observe the complete evolution of endothelial damage from initial infection to severe manifestations.
Achieving physiologically relevant tissue architecture poses additional difficulties. The lung's complex three-dimensional structure, with its air-blood barrier and specialized endothelial cells, is challenging to recreate with current fabrication techniques. Most models simplify this architecture, potentially missing critical aspects of virus-endothelium interactions that occur at anatomically specific sites.
The integration of patient-specific factors remains problematic. Individual variations in ACE2 receptor expression, pre-existing endothelial dysfunction, and genetic predispositions significantly influence COVID-19 severity but are rarely incorporated into standardized models. This limits the translational value of research findings to diverse patient populations.
Technical challenges in maintaining sterile conditions while allowing viral infection further complicate research efforts. Introducing SARS-CoV-2 into lung-on-chip systems requires specialized containment facilities and protocols that are not widely available, restricting widespread adoption of these models for COVID-19 research.
The validation of model findings against clinical observations presents another hurdle. The rapid evolution of COVID-19 variants with different endothelial tropism and damage mechanisms necessitates continuous updating of models, creating a moving target for researchers attempting to establish clinically relevant systems.
Interdisciplinary expertise requirements further limit progress in this field. Effective COVID-19 endothelial damage modeling demands collaboration between virologists, immunologists, bioengineers, and clinicians—a combination that few research institutions can readily assemble, especially under pandemic conditions.
Existing Immune-Competent Lung Models
01 Lung-on-chip models with immune cell integration
Advanced lung-on-chip platforms that incorporate immune cells to create immune-competent microenvironments. These models integrate various immune cell types with lung epithelial and endothelial cells to simulate immune responses in the lung microenvironment. The immune cells can interact with the endothelial layer, allowing researchers to study immune-mediated endothelial damage and inflammatory responses in conditions such as viral infections or autoimmune disorders.- Microfluidic lung-on-chip models with immune components: Microfluidic devices that mimic the structure and function of human lungs, incorporating immune cells to create immune-competent models. These systems typically include multiple chambers representing different lung compartments with endothelial cells forming blood vessel barriers. The models allow for the study of immune responses to various stimuli and can be used to investigate endothelial damage mechanisms in a controlled environment.
- Endothelial barrier function assessment in lung models: Methods for evaluating endothelial damage and barrier integrity in lung-on-chip models. These approaches include measuring permeability, electrical resistance, and molecular markers of endothelial dysfunction. The techniques enable quantitative assessment of how various stimuli, including inflammatory cytokines, pathogens, or therapeutic agents, affect the endothelial barrier, which is crucial for understanding pulmonary diseases involving vascular damage.
- Immune cell-endothelial interactions in lung models: Studies of the interactions between immune cells and endothelial cells in lung-on-chip platforms. These models incorporate various immune cell types such as neutrophils, macrophages, and lymphocytes to investigate their roles in endothelial damage or protection. The systems allow for real-time visualization and measurement of immune cell recruitment, adhesion, migration through the endothelial barrier, and the resulting effects on endothelial integrity.
- Disease modeling of endothelial damage in lung-on-chip: Application of immune-competent lung-on-chip models to replicate specific disease conditions that involve endothelial damage. These models simulate pathological conditions such as acute respiratory distress syndrome, COVID-19 lung injury, pulmonary hypertension, and inflammatory lung diseases. By recreating disease microenvironments, researchers can study the mechanisms of endothelial dysfunction and test potential therapeutic interventions in a physiologically relevant context.
- Therapeutic testing for endothelial protection in lung models: Utilization of immune-competent lung-on-chip models for screening and evaluating therapeutic compounds that may protect or repair damaged endothelium. These platforms enable testing of anti-inflammatory agents, endothelial stabilizers, and novel biologics designed to preserve vascular integrity. The models provide insights into drug efficacy, mechanisms of action, and potential side effects in a system that recapitulates key aspects of human lung physiology and pathology.
02 Endothelial damage assessment in lung models
Methods and systems for evaluating endothelial damage in lung-on-chip models. These approaches include measuring barrier integrity, permeability changes, expression of damage markers, and functional alterations in endothelial cells. The models allow for real-time monitoring of endothelial responses to various stimuli, including inflammatory cytokines, pathogens, or mechanical stress, providing insights into mechanisms of vascular injury in lung diseases.Expand Specific Solutions03 Microfluidic systems for lung-endothelial interactions
Specialized microfluidic platforms designed to model the lung microvasculature and its interaction with other lung components. These systems incorporate flow dynamics to simulate blood circulation and can be used to study how shear stress affects endothelial function and damage. The microfluidic nature allows for precise control of the microenvironment and facilitates the study of complex cell-cell interactions between endothelial cells and other lung cell types under physiologically relevant conditions.Expand Specific Solutions04 Therapeutic testing for endothelial protection
Utilization of immune-competent lung-on-chip models to evaluate potential therapeutic agents that can protect against or repair endothelial damage. These models serve as platforms for screening compounds that may reduce inflammation, prevent vascular leakage, or promote endothelial repair. The integration of immune components allows for assessment of how immunomodulatory therapies might affect endothelial health in the context of lung diseases.Expand Specific Solutions05 Disease modeling of endothelial dysfunction
Application of lung-on-chip technology to model specific diseases characterized by endothelial dysfunction. These models recreate pathological conditions such as acute respiratory distress syndrome (ARDS), pulmonary hypertension, or COVID-19-related vascular complications. By incorporating disease-specific stimuli and measuring endothelial responses, researchers can better understand the mechanisms of endothelial damage in various lung pathologies and develop targeted interventions.Expand Specific Solutions
Leading Organizations in Organ-on-Chip Research
The COVID-19 lung-on-chip technology market is in an early growth phase, with increasing research interest but limited commercial deployment. Market size is expanding as healthcare institutions seek better disease models, potentially reaching significant value as COVID-19 research continues globally. Technologically, the field shows promising development with academic institutions leading innovation. Emulate, Inc. stands as the primary commercial player with established organ-on-chip platforms, while academic institutions like Zhejiang University, Fudan University, and Washington University in St. Louis contribute significant research advances. Research organizations including Institut National de la Santé et de la Recherche Médicale and The Georgia Tech Research Corp are developing complementary technologies, while biopharmaceutical companies like IncellDx, Aethlon Medical, and Akeso Biopharma are exploring clinical applications, indicating a collaborative ecosystem advancing toward more mature solutions.
Zhejiang University
Technical Solution: Zhejiang University has pioneered an advanced immune-competent lung-on-chip platform specifically engineered to investigate COVID-19 endothelial pathology. Their system integrates primary human pulmonary microvascular endothelial cells with alveolar epithelial cells and circulating immune components, particularly neutrophils and monocytes, in a microfluidic device that replicates the alveolar-capillary interface. The platform incorporates cyclic mechanical stretching to simulate breathing mechanics and enables controlled introduction of SARS-CoV-2 spike proteins or viral particles. Their research has demonstrated how the virus triggers endothelial activation, disrupts intercellular junctions, and promotes neutrophil extracellular trap (NET) formation, which contributes to microvascular thrombosis. The system allows for real-time monitoring of endothelial permeability changes, immune cell adhesion, and transmigration processes that characterize severe COVID-19 pathology.
Strengths: Comprehensive integration of immune components with lung tissue structures; ability to precisely control mechanical forces that influence disease progression; capacity to study temporal dynamics of endothelial damage. Weaknesses: Requires specialized expertise in microfluidics and cell culture; limited throughput for large-scale drug screening; challenges in maintaining long-term culture stability for chronic disease modeling.
Emulate, Inc.
Technical Solution: Emulate has developed advanced Lung-Chip technology specifically designed to model COVID-19 pathophysiology. Their platform incorporates human lung alveolar epithelial cells, pulmonary microvascular endothelial cells, and immune cells in a dynamic microfluidic environment that mimics breathing motions and blood flow. This system enables the study of SARS-CoV-2 infection mechanisms, particularly focusing on endothelial damage, cytokine storm modeling, and immune cell recruitment. The Lung-Chip incorporates mechanical forces that simulate breathing, allowing researchers to observe how these physiological stresses affect viral infection and endothelial response. Emulate's technology permits real-time visualization of cellular interactions and barrier function disruption during infection, providing insights into the mechanisms of vascular leakage and thrombosis formation that characterize severe COVID-19.
Strengths: Superior physiological relevance compared to traditional 2D cultures; ability to incorporate multiple cell types including immune components; capacity to measure real-time barrier function changes. Limitations: Higher technical complexity and cost compared to conventional models; challenges in standardization across different research settings; limited throughput compared to simpler screening platforms.
Key Innovations in COVID-19 Endothelial Damage Modeling
A device and method to design a cost-effective organ-on-chip prototype for drug toxicity testing in lung and liver tissues
PatentInactiveAU2021104949A4
Innovation
- Development of a cost-effective organ-on-chip prototype for drug toxicity testing in lung and liver tissues, specifically designed to study COVID-19 related acute respiratory distress syndrome (ARDS).
- Novel membrane processing method for improved bonding between membranes and upper/lower channel layers in the microfluidic platform.
- Modified fabrication techniques and materials selection to significantly reduce the manufacturing cost of lung-on-chip and liver-on-chip platforms.
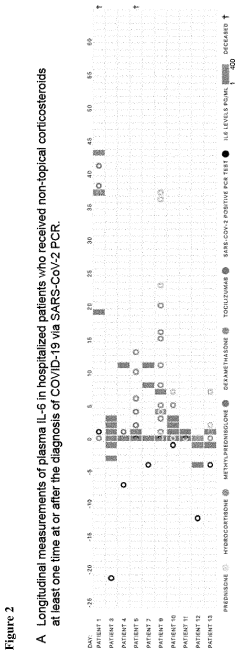
Methods for treating and evaluating covid-19 patients
PatentPendingUS20230075138A1
Innovation
- Determining the expression level of the corticosteroid receptor NR3C1 in patient samples to identify responders or non-responders to immunomodulating therapies, allowing for personalized treatment decisions and monitoring of treatment effectiveness by comparing gene expression profiles over time.
Regulatory Framework for Organ-on-Chip Validation
The regulatory landscape for organ-on-chip (OOC) technologies, particularly immune-competent lung-on-chip models for COVID-19 research, remains in nascent stages of development. Current frameworks primarily derive from broader tissue engineering and in vitro diagnostic regulatory pathways, creating significant challenges for validation and standardization.
The FDA has initiated preliminary guidance through its Emerging Technology Program, recognizing OOC platforms as potential alternatives to animal testing under the Modernization Act of 2019. However, specific validation protocols for immune-competent lung models studying endothelial damage mechanisms in severe COVID-19 remain undefined, creating regulatory uncertainty for researchers and developers.
European regulatory bodies, through the European Medicines Agency (EMA), have established the Innovation Task Force to address novel methodologies including OOC technologies. Their qualification advice procedure offers a pathway for validating these models as drug development tools, though comprehensive standards specifically addressing immune component integration remain underdeveloped.
International harmonization efforts through the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) have begun incorporating discussions on microphysiological systems, but consensus on validation requirements for complex immune-competent models remains elusive.
Key validation challenges include establishing reproducibility metrics across different laboratory settings, defining appropriate reference standards for immune responses, and determining acceptable correlation parameters between chip-based observations and clinical manifestations of COVID-19 endothelial damage.
Regulatory acceptance currently follows a case-by-case evaluation approach, with authorities requiring extensive comparison data between traditional methods and OOC models. This creates significant barriers to widespread adoption in pharmaceutical development and clinical research pipelines.
Industry consortia such as the Organ-on-Chip Technologies Network and the European Organ-on-Chip Society are working to establish voluntary standards and best practices for validation. Their efforts focus on creating reproducible protocols for immune cell integration, endothelial barrier function assessment, and cytokine response quantification in the context of viral infections.
Moving forward, a fit-for-purpose validation framework appears most promising, where regulatory requirements align with the specific intended use of the lung-on-chip model rather than imposing universal standards across all applications.
The FDA has initiated preliminary guidance through its Emerging Technology Program, recognizing OOC platforms as potential alternatives to animal testing under the Modernization Act of 2019. However, specific validation protocols for immune-competent lung models studying endothelial damage mechanisms in severe COVID-19 remain undefined, creating regulatory uncertainty for researchers and developers.
European regulatory bodies, through the European Medicines Agency (EMA), have established the Innovation Task Force to address novel methodologies including OOC technologies. Their qualification advice procedure offers a pathway for validating these models as drug development tools, though comprehensive standards specifically addressing immune component integration remain underdeveloped.
International harmonization efforts through the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) have begun incorporating discussions on microphysiological systems, but consensus on validation requirements for complex immune-competent models remains elusive.
Key validation challenges include establishing reproducibility metrics across different laboratory settings, defining appropriate reference standards for immune responses, and determining acceptable correlation parameters between chip-based observations and clinical manifestations of COVID-19 endothelial damage.
Regulatory acceptance currently follows a case-by-case evaluation approach, with authorities requiring extensive comparison data between traditional methods and OOC models. This creates significant barriers to widespread adoption in pharmaceutical development and clinical research pipelines.
Industry consortia such as the Organ-on-Chip Technologies Network and the European Organ-on-Chip Society are working to establish voluntary standards and best practices for validation. Their efforts focus on creating reproducible protocols for immune cell integration, endothelial barrier function assessment, and cytokine response quantification in the context of viral infections.
Moving forward, a fit-for-purpose validation framework appears most promising, where regulatory requirements align with the specific intended use of the lung-on-chip model rather than imposing universal standards across all applications.
Translational Potential to Clinical Applications
The immune-competent lung-on-chip models studying COVID-19 endothelial damage mechanisms hold significant translational potential for clinical applications. These advanced in vitro platforms bridge the gap between traditional cell culture systems and human clinical trials, offering a physiologically relevant environment to study disease mechanisms and test therapeutic interventions.
The immediate clinical translation potential lies in drug repurposing and screening. These models enable rapid testing of existing FDA-approved medications against COVID-19-induced endothelial damage, potentially accelerating the identification of effective treatments. Several antiviral, anti-inflammatory, and endothelial-protective agents have already shown promising results in these systems, providing valuable insights for clinical decision-making during the pandemic and for future coronavirus outbreaks.
Beyond drug screening, these models offer personalized medicine applications. By incorporating patient-derived cells, clinicians could potentially predict individual responses to various therapeutic regimens, enabling tailored treatment approaches for severe COVID-19 cases. This personalization is particularly valuable given the heterogeneous nature of COVID-19 manifestations across different patient populations.
The models also serve as valuable tools for understanding long COVID mechanisms. The persistent endothelial dysfunction observed in many post-COVID patients can be modeled and studied longitudinally, potentially revealing therapeutic targets for this emerging clinical challenge. The ability to maintain these systems for extended periods makes them ideal for studying such chronic manifestations.
For vaccine development, these platforms provide a human-relevant system to assess potential endothelial side effects of vaccine candidates before clinical trials. This application has gained particular relevance following reports of rare thrombotic events associated with certain COVID-19 vaccines.
Regulatory agencies have shown increasing interest in organ-on-chip technologies as complementary or alternative methods to animal testing. The immune-competent lung-on-chip models could potentially reduce the need for animal studies in COVID-19 research, aligning with global efforts to implement the 3Rs principle (Replacement, Reduction, Refinement) in biomedical research.
The translation of these models into clinical practice faces challenges including standardization, scalability, and validation against clinical outcomes. However, collaborative efforts between academic institutions, regulatory bodies, and pharmaceutical companies are actively addressing these limitations, with several platforms progressing toward commercial availability and regulatory acceptance.
The immediate clinical translation potential lies in drug repurposing and screening. These models enable rapid testing of existing FDA-approved medications against COVID-19-induced endothelial damage, potentially accelerating the identification of effective treatments. Several antiviral, anti-inflammatory, and endothelial-protective agents have already shown promising results in these systems, providing valuable insights for clinical decision-making during the pandemic and for future coronavirus outbreaks.
Beyond drug screening, these models offer personalized medicine applications. By incorporating patient-derived cells, clinicians could potentially predict individual responses to various therapeutic regimens, enabling tailored treatment approaches for severe COVID-19 cases. This personalization is particularly valuable given the heterogeneous nature of COVID-19 manifestations across different patient populations.
The models also serve as valuable tools for understanding long COVID mechanisms. The persistent endothelial dysfunction observed in many post-COVID patients can be modeled and studied longitudinally, potentially revealing therapeutic targets for this emerging clinical challenge. The ability to maintain these systems for extended periods makes them ideal for studying such chronic manifestations.
For vaccine development, these platforms provide a human-relevant system to assess potential endothelial side effects of vaccine candidates before clinical trials. This application has gained particular relevance following reports of rare thrombotic events associated with certain COVID-19 vaccines.
Regulatory agencies have shown increasing interest in organ-on-chip technologies as complementary or alternative methods to animal testing. The immune-competent lung-on-chip models could potentially reduce the need for animal studies in COVID-19 research, aligning with global efforts to implement the 3Rs principle (Replacement, Reduction, Refinement) in biomedical research.
The translation of these models into clinical practice faces challenges including standardization, scalability, and validation against clinical outcomes. However, collaborative efforts between academic institutions, regulatory bodies, and pharmaceutical companies are actively addressing these limitations, with several platforms progressing toward commercial availability and regulatory acceptance.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!