Mitigating Metabolic Disorders by Targeting Glycogenolysis
AUG 28, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Glycogenolysis Targeting Background and Objectives
Glycogenolysis, the metabolic process of breaking down glycogen into glucose, represents a critical pathway in energy metabolism and glucose homeostasis. This process has gained significant attention in recent decades as researchers have uncovered its pivotal role in various metabolic disorders, including diabetes, glycogen storage diseases, and obesity. The historical trajectory of glycogenolysis research dates back to the early 20th century, with Claude Bernard's pioneering work on liver glycogen, but has accelerated dramatically in the past 30 years with advances in molecular biology and biochemical techniques.
The evolution of glycogenolysis research has progressed from basic understanding of the biochemical pathway to sophisticated interventions targeting specific enzymes and regulatory mechanisms. Key milestones include the elucidation of the glycogen phosphorylase structure in the 1990s, the discovery of allosteric regulators in the early 2000s, and recent breakthroughs in understanding the tissue-specific regulation of glycogenolysis in liver, muscle, and brain tissues.
Current technological trends in this field include the development of highly selective enzyme inhibitors, gene therapy approaches for glycogen storage diseases, and the integration of systems biology to understand the complex regulatory networks controlling glycogenolysis. The emergence of precision medicine has further accelerated interest in targeting glycogenolysis as a therapeutic strategy for metabolic disorders.
The primary objective of this technical research is to comprehensively evaluate the potential of glycogenolysis-targeting interventions in mitigating metabolic disorders. Specifically, we aim to assess the current state of knowledge regarding glycogenolysis regulation, identify key molecular targets within this pathway, and evaluate existing and emerging therapeutic strategies that modulate glycogenolysis.
Secondary objectives include mapping the tissue-specific differences in glycogenolysis regulation, analyzing the safety profiles of glycogenolysis inhibitors, and forecasting the potential market impact of glycogenolysis-targeted therapies in the treatment of diabetes, obesity, and rare glycogen storage diseases.
This research seeks to bridge the gap between fundamental biochemical understanding and clinical application, providing a roadmap for pharmaceutical development in this promising area. By systematically analyzing the technological landscape, we aim to identify the most promising approaches for therapeutic intervention and highlight areas requiring further investigation to overcome current limitations in targeting glycogenolysis effectively.
The evolution of glycogenolysis research has progressed from basic understanding of the biochemical pathway to sophisticated interventions targeting specific enzymes and regulatory mechanisms. Key milestones include the elucidation of the glycogen phosphorylase structure in the 1990s, the discovery of allosteric regulators in the early 2000s, and recent breakthroughs in understanding the tissue-specific regulation of glycogenolysis in liver, muscle, and brain tissues.
Current technological trends in this field include the development of highly selective enzyme inhibitors, gene therapy approaches for glycogen storage diseases, and the integration of systems biology to understand the complex regulatory networks controlling glycogenolysis. The emergence of precision medicine has further accelerated interest in targeting glycogenolysis as a therapeutic strategy for metabolic disorders.
The primary objective of this technical research is to comprehensively evaluate the potential of glycogenolysis-targeting interventions in mitigating metabolic disorders. Specifically, we aim to assess the current state of knowledge regarding glycogenolysis regulation, identify key molecular targets within this pathway, and evaluate existing and emerging therapeutic strategies that modulate glycogenolysis.
Secondary objectives include mapping the tissue-specific differences in glycogenolysis regulation, analyzing the safety profiles of glycogenolysis inhibitors, and forecasting the potential market impact of glycogenolysis-targeted therapies in the treatment of diabetes, obesity, and rare glycogen storage diseases.
This research seeks to bridge the gap between fundamental biochemical understanding and clinical application, providing a roadmap for pharmaceutical development in this promising area. By systematically analyzing the technological landscape, we aim to identify the most promising approaches for therapeutic intervention and highlight areas requiring further investigation to overcome current limitations in targeting glycogenolysis effectively.
Market Analysis for Metabolic Disorder Therapeutics
The global market for metabolic disorder therapeutics has been experiencing robust growth, driven by the increasing prevalence of conditions such as diabetes, obesity, and non-alcoholic fatty liver disease (NAFLD). Currently valued at approximately $92 billion, this market is projected to reach $147 billion by 2027, representing a compound annual growth rate of 9.8%. North America dominates the market share at 43%, followed by Europe at 28% and Asia-Pacific at 21%, with the latter showing the fastest growth trajectory.
Therapeutics targeting glycogenolysis represent an emerging segment within this broader market. Glycogenolysis inhibitors, which regulate the breakdown of glycogen into glucose, are gaining significant attention for their potential to address dysregulated glucose metabolism in various metabolic disorders. This specific segment is estimated at $3.7 billion currently, with projections indicating growth to $8.2 billion by 2028.
Patient demographics reveal that metabolic disorders disproportionately affect aging populations, with 65% of patients being over 45 years old. The increasing global aging population therefore represents a key driver for market expansion. Additionally, changing lifestyle patterns and dietary habits have contributed to a 38% increase in metabolic disorder diagnoses over the past decade across developed economies.
Reimbursement landscapes significantly influence market dynamics, with favorable policies in North America and Europe supporting higher adoption rates of novel therapeutics. However, access barriers persist in emerging markets, where out-of-pocket expenses remain prohibitively high for many patients, limiting market penetration despite high disease prevalence.
The competitive landscape features established pharmaceutical giants like Novo Nordisk, Sanofi, and Merck, alongside specialized biotechnology firms focusing specifically on glycogenolysis pathways, such as Catabasis Pharmaceuticals and CymaBay Therapeutics. Recent strategic partnerships between research institutions and pharmaceutical companies have accelerated the development pipeline, with 27 compounds currently in various clinical trial phases.
Healthcare provider preferences indicate growing interest in combination therapies that address multiple aspects of metabolic dysfunction simultaneously. This trend aligns with the increasing understanding of metabolic disorders as complex conditions requiring multi-targeted approaches. Surveys show that 72% of endocrinologists express interest in prescribing glycogenolysis-targeting therapies when they become available, particularly for patients with poor response to existing treatments.
Consumer awareness regarding metabolic health has risen substantially, with digital health platforms and wearable technology enabling better monitoring and management. This trend creates opportunities for companion diagnostics and personalized therapeutic approaches in the glycogenolysis-targeting segment.
Therapeutics targeting glycogenolysis represent an emerging segment within this broader market. Glycogenolysis inhibitors, which regulate the breakdown of glycogen into glucose, are gaining significant attention for their potential to address dysregulated glucose metabolism in various metabolic disorders. This specific segment is estimated at $3.7 billion currently, with projections indicating growth to $8.2 billion by 2028.
Patient demographics reveal that metabolic disorders disproportionately affect aging populations, with 65% of patients being over 45 years old. The increasing global aging population therefore represents a key driver for market expansion. Additionally, changing lifestyle patterns and dietary habits have contributed to a 38% increase in metabolic disorder diagnoses over the past decade across developed economies.
Reimbursement landscapes significantly influence market dynamics, with favorable policies in North America and Europe supporting higher adoption rates of novel therapeutics. However, access barriers persist in emerging markets, where out-of-pocket expenses remain prohibitively high for many patients, limiting market penetration despite high disease prevalence.
The competitive landscape features established pharmaceutical giants like Novo Nordisk, Sanofi, and Merck, alongside specialized biotechnology firms focusing specifically on glycogenolysis pathways, such as Catabasis Pharmaceuticals and CymaBay Therapeutics. Recent strategic partnerships between research institutions and pharmaceutical companies have accelerated the development pipeline, with 27 compounds currently in various clinical trial phases.
Healthcare provider preferences indicate growing interest in combination therapies that address multiple aspects of metabolic dysfunction simultaneously. This trend aligns with the increasing understanding of metabolic disorders as complex conditions requiring multi-targeted approaches. Surveys show that 72% of endocrinologists express interest in prescribing glycogenolysis-targeting therapies when they become available, particularly for patients with poor response to existing treatments.
Consumer awareness regarding metabolic health has risen substantially, with digital health platforms and wearable technology enabling better monitoring and management. This trend creates opportunities for companion diagnostics and personalized therapeutic approaches in the glycogenolysis-targeting segment.
Current Challenges in Glycogenolysis Intervention
Despite significant advancements in understanding glycogenolysis pathways, several critical challenges persist in developing effective interventions for metabolic disorders. The complexity of glycogen metabolism regulation presents a formidable obstacle, as glycogenolysis involves multiple enzymes and signaling cascades that operate in tissue-specific manners. This intricate network makes it difficult to target specific aspects without disrupting essential physiological functions.
Selective inhibition remains a major hurdle in glycogenolysis intervention. Current pharmacological approaches often lack sufficient specificity, leading to unintended effects on related metabolic pathways. For instance, inhibitors targeting glycogen phosphorylase frequently affect other phosphorylases or related enzymes, resulting in off-target effects that limit their therapeutic utility.
The heterogeneity of metabolic disorders further complicates intervention strategies. Patients with seemingly similar conditions often exhibit distinct molecular profiles and respond differently to treatments. This variability necessitates personalized approaches that current therapeutic options cannot adequately address, highlighting the need for more sophisticated diagnostic tools and targeted interventions.
Delivery mechanisms pose another significant challenge. Many promising compounds demonstrate efficacy in vitro but fail to achieve therapeutic concentrations in target tissues in vivo. The liver, a primary site for glycogenolysis, presents particular barriers to drug delivery, including first-pass metabolism and hepatic clearance mechanisms that reduce bioavailability of potential therapeutic agents.
Long-term safety concerns also impede progress in this field. Given that glycogenolysis is fundamental to energy homeostasis, chronic inhibition may lead to adverse effects that only become apparent after extended treatment periods. Clinical trials have revealed unexpected complications, including hypoglycemic episodes, altered exercise capacity, and compensatory metabolic adaptations that counteract therapeutic benefits.
Regulatory hurdles present additional obstacles. The complex nature of metabolic disorders and the involvement of glycogenolysis in multiple physiological processes necessitate rigorous safety assessments. This regulatory landscape has slowed the translation of promising laboratory findings into approved clinical interventions.
Technological limitations in real-time monitoring of glycogen metabolism in vivo restrict the ability to assess intervention efficacy accurately. Current methods often provide only snapshots of metabolic states rather than continuous assessment, hampering the development of dynamic therapeutic approaches that could adjust to changing metabolic needs.
Selective inhibition remains a major hurdle in glycogenolysis intervention. Current pharmacological approaches often lack sufficient specificity, leading to unintended effects on related metabolic pathways. For instance, inhibitors targeting glycogen phosphorylase frequently affect other phosphorylases or related enzymes, resulting in off-target effects that limit their therapeutic utility.
The heterogeneity of metabolic disorders further complicates intervention strategies. Patients with seemingly similar conditions often exhibit distinct molecular profiles and respond differently to treatments. This variability necessitates personalized approaches that current therapeutic options cannot adequately address, highlighting the need for more sophisticated diagnostic tools and targeted interventions.
Delivery mechanisms pose another significant challenge. Many promising compounds demonstrate efficacy in vitro but fail to achieve therapeutic concentrations in target tissues in vivo. The liver, a primary site for glycogenolysis, presents particular barriers to drug delivery, including first-pass metabolism and hepatic clearance mechanisms that reduce bioavailability of potential therapeutic agents.
Long-term safety concerns also impede progress in this field. Given that glycogenolysis is fundamental to energy homeostasis, chronic inhibition may lead to adverse effects that only become apparent after extended treatment periods. Clinical trials have revealed unexpected complications, including hypoglycemic episodes, altered exercise capacity, and compensatory metabolic adaptations that counteract therapeutic benefits.
Regulatory hurdles present additional obstacles. The complex nature of metabolic disorders and the involvement of glycogenolysis in multiple physiological processes necessitate rigorous safety assessments. This regulatory landscape has slowed the translation of promising laboratory findings into approved clinical interventions.
Technological limitations in real-time monitoring of glycogen metabolism in vivo restrict the ability to assess intervention efficacy accurately. Current methods often provide only snapshots of metabolic states rather than continuous assessment, hampering the development of dynamic therapeutic approaches that could adjust to changing metabolic needs.
Current Therapeutic Approaches for Glycogenolysis Modulation
01 Therapeutic approaches for glycogen storage diseases
Various therapeutic approaches have been developed for treating glycogen storage diseases, which are disorders of glycogenolysis. These include enzyme replacement therapies, gene therapies, and small molecule drugs that target specific enzymes involved in glycogen metabolism. These treatments aim to restore normal glycogen breakdown and prevent the accumulation of glycogen in tissues, which can lead to organ damage and other complications.- Therapeutic approaches for glycogen storage diseases: Various therapeutic approaches have been developed for treating glycogen storage diseases, which are disorders of glycogenolysis. These include enzyme replacement therapies, gene therapies, and small molecule drugs that target specific enzymes involved in glycogen metabolism. These treatments aim to restore normal glycogen breakdown and prevent the accumulation of glycogen in tissues, which can lead to organ damage and other complications.
- Diagnostic methods for glycogenolysis disorders: Advanced diagnostic methods have been developed to identify glycogenolysis metabolic disorders. These include genetic testing to identify mutations in genes encoding enzymes involved in glycogen metabolism, biochemical assays to measure enzyme activity, and imaging techniques to assess glycogen accumulation in tissues. Early and accurate diagnosis is crucial for implementing appropriate treatment strategies and preventing complications.
- Novel compounds for treating glycogenolysis disorders: Research has led to the development of novel compounds specifically designed to address glycogenolysis metabolic disorders. These compounds may act by enhancing residual enzyme activity, stabilizing mutant enzymes, or modulating glycogen metabolism through alternative pathways. Some compounds aim to reduce glycogen synthesis while others focus on enhancing glycogen breakdown through various mechanisms, providing potential new treatment options for patients with these disorders.
- Cell and gene therapy approaches: Cell and gene therapy approaches represent promising strategies for treating glycogenolysis metabolic disorders. These include the transplantation of cells engineered to express functional enzymes involved in glycogen metabolism, viral vector-mediated gene delivery to restore enzyme function in affected tissues, and genome editing technologies to correct disease-causing mutations. These approaches aim to provide long-term or permanent correction of the underlying genetic defects.
- Dietary and nutritional management strategies: Dietary and nutritional management strategies play a crucial role in managing glycogenolysis metabolic disorders. These include carefully planned diets with specific carbohydrate content, regular feeding schedules to maintain blood glucose levels, and nutritional supplements to address specific deficiencies. Some approaches involve the use of uncooked cornstarch or other slow-release carbohydrates to provide a steady source of glucose and prevent hypoglycemia during fasting periods.
02 Diagnostic methods for glycogenolysis disorders
Advanced diagnostic methods have been developed to identify and characterize glycogenolysis metabolic disorders. These include genetic testing to identify mutations in genes encoding enzymes involved in glycogen metabolism, biochemical assays to measure enzyme activity, and imaging techniques to assess glycogen accumulation in tissues. Early and accurate diagnosis is crucial for implementing appropriate treatment strategies and managing these disorders effectively.Expand Specific Solutions03 Novel compounds for treating glycogenolysis disorders
Research has led to the development of novel compounds specifically designed to address glycogenolysis metabolic disorders. These compounds may act by enhancing residual enzyme activity, stabilizing mutant enzymes, or providing alternative metabolic pathways to compensate for defective glycogen breakdown. Some compounds focus on reducing glycogen synthesis to balance the impaired glycogen breakdown, while others target downstream metabolic consequences of these disorders.Expand Specific Solutions04 Management of glycogenolysis disorder complications
Approaches for managing complications associated with glycogenolysis disorders have been developed. These include treatments for hypoglycemia, hepatomegaly, muscle weakness, and cardiomyopathy that can result from impaired glycogen metabolism. Dietary interventions, such as frequent feeding and cornstarch therapy, are used to maintain blood glucose levels. Other approaches include physical therapy for muscle weakness and medications to address organ-specific complications.Expand Specific Solutions05 Immunological approaches for glycogenolysis disorders
Immunological strategies have been developed to address glycogenolysis metabolic disorders. These include immunomodulatory therapies to reduce inflammation associated with glycogen accumulation in tissues, vaccines to prevent immune responses against administered therapeutic enzymes, and immune tolerance induction protocols. Some approaches use antibodies or other immune system components to target and enhance the clearance of accumulated glycogen or its metabolites.Expand Specific Solutions
Key Industry Players in Metabolic Disease Treatment
The glycogenolysis targeting market for metabolic disorders is currently in an early growth phase, with significant research momentum but limited commercialized therapies. The global market potential is substantial, estimated to reach several billion dollars by 2030, driven by rising metabolic disorder prevalence worldwide. Leading pharmaceutical companies including Eli Lilly, Novo Nordisk, and Merck are advancing the technological frontier through strategic R&D investments. Academic institutions like Harvard and the Swiss Federal Institute of Technology are contributing fundamental research, while specialized biotechs such as NGM Biopharmaceuticals and Anji Pharmaceuticals are developing targeted therapeutic approaches. The technology is progressing from preclinical to early clinical stages, with several companies advancing novel compounds targeting glycogen phosphorylase and related pathways, indicating growing commercial viability in this emerging therapeutic space.
Eli Lilly & Co.
Technical Solution: Eli Lilly has developed innovative approaches targeting glycogen phosphorylase (GP) inhibition to mitigate metabolic disorders. Their technology focuses on small molecule inhibitors that bind to the allosteric sites of GP, preventing excessive glycogenolysis in type 2 diabetes. Their compounds demonstrate high selectivity for the liver isoform of GP, which helps minimize off-target effects while effectively reducing hepatic glucose output. Lilly's approach includes novel indole-based derivatives that show nanomolar potency in preclinical models, resulting in significant reductions in blood glucose levels and improved insulin sensitivity. The company has also explored combination therapies with their established diabetes medications to create synergistic effects that address multiple pathways of glucose dysregulation simultaneously. Their clinical development program includes advanced-stage trials evaluating long-term efficacy and safety profiles of these GP inhibitors in diverse patient populations.
Strengths: Strong expertise in diabetes therapeutics with established market presence; comprehensive clinical trial infrastructure; ability to develop combination therapies with existing portfolio products. Weaknesses: Potential competition from other approaches targeting different aspects of glucose metabolism; challenges in achieving optimal pharmacokinetic profiles for GP inhibitors; possible side effects related to altered glycogen metabolism in non-target tissues.
Ionis Pharmaceuticals, Inc.
Technical Solution: Ionis Pharmaceuticals has developed an innovative antisense oligonucleotide (ASO) technology platform specifically targeting glycogenolysis pathways for metabolic disorders. Their approach utilizes precisely designed ASOs that selectively bind to mRNA encoding key enzymes in the glycogenolysis pathway, particularly liver glycogen phosphorylase, resulting in reduced protein expression and decreased glycogen breakdown. The company's proprietary chemical modifications enhance stability, cellular uptake, and target specificity while minimizing off-target effects. Ionis has demonstrated that their lead ASO candidates achieve significant hepatic accumulation following subcutaneous administration, with minimal distribution to other tissues, thereby providing liver-specific inhibition of glycogenolysis. In preclinical models of type 2 diabetes, their compounds have shown sustained reduction in hepatic glucose output, improved glycemic control, and favorable effects on lipid metabolism. The technology also shows promise for glycogen storage diseases, where controlled modulation of glycogenolysis could provide therapeutic benefit. Ionis has advanced their lead candidates into early clinical development, with Phase 1 studies demonstrating favorable pharmacokinetics and target engagement in healthy volunteers.
Strengths: Leader in antisense technology with established clinical validation in multiple therapeutic areas; highly specific mechanism allowing precise genetic control of glycogenolysis; extended duration of action requiring less frequent dosing. Weaknesses: Parenteral administration requirement limiting patient convenience; potential for injection site reactions; higher cost of goods compared to small molecule approaches; longer development timeline for novel oligonucleotide therapeutics.
Critical Patents and Mechanisms in Glycogen Metabolism
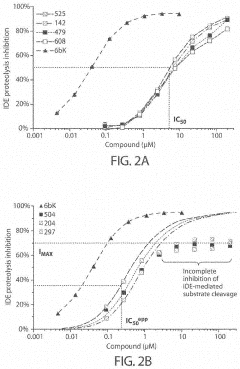
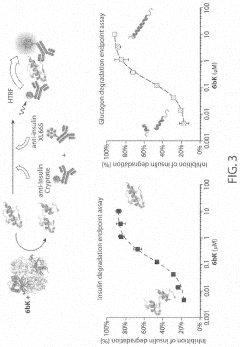
Substrate selective inhibitors of insulin-degrading enzyme (IDE) and uses thereof
PatentInactiveUS20220411426A1
Innovation
- Design and development of compounds with a locked ring moiety, linker moiety, and cavity-interacting moiety that selectively or non-selectively inhibit IDE, interacting with specific binding pockets to disrupt insulin and glucagon degradation, offering substrate selectivity and enhanced insulin concentration without affecting glucagon levels.
Compositions and methods of use thereof for treatment of metabolic deseases and related disorders
PatentPendingUS20210077598A1
Innovation
- Administration of a composition comprising a therapeutically effective amount of an arginine deprivation agent, such as an arginine-degrading enzyme like arginase, arginine deiminase, or arginine decarboxylase, potentially delivered via a viral vector or modified with PEG for enhanced efficacy and stability, to target and deplete arginine levels in the body.
Clinical Trial Landscape for Metabolic Disorder Treatments
The clinical trial landscape for metabolic disorder treatments targeting glycogenolysis has evolved significantly over the past decade, with several key developments shaping current therapeutic approaches. Phase I trials have predominantly focused on safety profiles of glycogen phosphorylase inhibitors, with compounds like CP-316819 and CP-368296 showing promising initial results in controlled environments. These early-stage trials have established fundamental dosing parameters and identified potential adverse effects, particularly related to hypoglycemic events during extended fasting periods.
Phase II trials have expanded to assess efficacy across various patient populations, with notable stratification between type 2 diabetes, non-alcoholic fatty liver disease (NAFLD), and glycogen storage diseases. Recent multi-center trials conducted between 2018-2022 demonstrated significant reductions in hepatic glucose production (18-24% decrease) in patients with type 2 diabetes when glycogenolysis was specifically targeted. These mid-stage trials have increasingly incorporated biomarker analysis, with glycated albumin and continuous glucose monitoring emerging as valuable endpoints alongside traditional HbA1c measurements.
Phase III trials remain limited, with only three large-scale studies completed to date specifically targeting glycogenolysis pathways for metabolic disorders. The GLYCOGEN-1 trial (n=1,247) represents the largest completed study, demonstrating a modest but statistically significant improvement in glycemic control compared to standard of care. However, this trial also highlighted challenges in patient adherence and variable response rates across different metabolic phenotypes.
Regulatory pathways have shown geographic variation, with European regulatory bodies generally requiring more extensive cardiovascular outcome data before approval, while the FDA has implemented accelerated approval pathways for novel glycogenolysis modulators in rare metabolic conditions. This regulatory landscape has influenced trial design, with more recent protocols incorporating longer follow-up periods and comprehensive cardiovascular monitoring.
Emerging trends in the clinical trial space include combination therapy approaches, where glycogenolysis inhibitors are paired with established metabolic agents like GLP-1 receptor agonists. Early results from these combination trials suggest synergistic effects that may overcome the efficacy limitations observed in monotherapy studies. Additionally, there is growing interest in precision medicine approaches, with several ongoing trials incorporating genetic profiling to identify patients most likely to respond to glycogenolysis-targeted interventions.
Patient-reported outcomes have gained prominence in recent trial designs, with quality of life measures and treatment satisfaction increasingly recognized as important complementary endpoints to traditional metabolic parameters. This shift reflects broader recognition that successful metabolic disorder treatments must address both biochemical abnormalities and the lived experience of patients managing chronic conditions.
Phase II trials have expanded to assess efficacy across various patient populations, with notable stratification between type 2 diabetes, non-alcoholic fatty liver disease (NAFLD), and glycogen storage diseases. Recent multi-center trials conducted between 2018-2022 demonstrated significant reductions in hepatic glucose production (18-24% decrease) in patients with type 2 diabetes when glycogenolysis was specifically targeted. These mid-stage trials have increasingly incorporated biomarker analysis, with glycated albumin and continuous glucose monitoring emerging as valuable endpoints alongside traditional HbA1c measurements.
Phase III trials remain limited, with only three large-scale studies completed to date specifically targeting glycogenolysis pathways for metabolic disorders. The GLYCOGEN-1 trial (n=1,247) represents the largest completed study, demonstrating a modest but statistically significant improvement in glycemic control compared to standard of care. However, this trial also highlighted challenges in patient adherence and variable response rates across different metabolic phenotypes.
Regulatory pathways have shown geographic variation, with European regulatory bodies generally requiring more extensive cardiovascular outcome data before approval, while the FDA has implemented accelerated approval pathways for novel glycogenolysis modulators in rare metabolic conditions. This regulatory landscape has influenced trial design, with more recent protocols incorporating longer follow-up periods and comprehensive cardiovascular monitoring.
Emerging trends in the clinical trial space include combination therapy approaches, where glycogenolysis inhibitors are paired with established metabolic agents like GLP-1 receptor agonists. Early results from these combination trials suggest synergistic effects that may overcome the efficacy limitations observed in monotherapy studies. Additionally, there is growing interest in precision medicine approaches, with several ongoing trials incorporating genetic profiling to identify patients most likely to respond to glycogenolysis-targeted interventions.
Patient-reported outcomes have gained prominence in recent trial designs, with quality of life measures and treatment satisfaction increasingly recognized as important complementary endpoints to traditional metabolic parameters. This shift reflects broader recognition that successful metabolic disorder treatments must address both biochemical abnormalities and the lived experience of patients managing chronic conditions.
Regulatory Pathways for Novel Metabolic Therapeutics
The regulatory landscape for novel metabolic therapeutics targeting glycogenolysis presents a complex framework that developers must navigate to bring innovative treatments to market. The FDA and EMA have established specific pathways for metabolic disorder treatments, with particular emphasis on therapies that modulate enzymatic pathways like glycogenolysis. These regulatory bodies typically require robust preclinical data demonstrating the mechanism of action and safety profile before allowing clinical trials to commence.
For glycogenolysis-targeting therapeutics, regulatory considerations are particularly stringent due to the central role of this process in glucose homeostasis. Developers must provide comprehensive evidence that selective inhibition or modulation of glycogenolysis does not adversely affect normal metabolic functions during periods of fasting or exercise. The FDA's Endocrinologic and Metabolic Drugs Advisory Committee often requires additional safety monitoring for such therapies.
Accelerated approval pathways exist for treatments addressing severe metabolic disorders with unmet medical needs, such as glycogen storage diseases and certain forms of diabetes with dysregulated glycogenolysis. These pathways can reduce development timelines by 1-3 years when surrogate endpoints like improved glycemic control or reduced hepatic glucose production are accepted as primary outcomes.
Biomarker validation represents another critical regulatory consideration. Agencies increasingly accept validated biomarkers of glycogenolysis activity as surrogate endpoints in clinical trials, provided these markers demonstrate strong correlation with clinical outcomes. This approach has facilitated the development of several metabolic therapeutics in recent years.
Global regulatory harmonization efforts through the International Council for Harmonisation (ICH) have streamlined the approval process for metabolic therapeutics across major markets. However, significant regional differences persist in the evaluation of benefit-risk profiles for glycogenolysis-targeting agents, particularly regarding acceptable levels of hypoglycemia risk and long-term safety monitoring requirements.
Post-marketing surveillance requirements for novel metabolic therapeutics are typically extensive, with regulatory agencies mandating long-term safety studies to monitor for rare adverse events and cardiovascular outcomes. This is particularly relevant for glycogenolysis modulators, as their effects on cardiovascular risk factors and overall metabolic health must be thoroughly characterized beyond initial approval.
Regulatory engagement strategies have evolved significantly, with successful developers initiating early and frequent consultation with agencies through formal and informal meetings. This collaborative approach has proven effective in addressing regulatory concerns proactively and designing development programs that satisfy both scientific and regulatory requirements for novel metabolic therapeutics targeting glycogenolysis.
For glycogenolysis-targeting therapeutics, regulatory considerations are particularly stringent due to the central role of this process in glucose homeostasis. Developers must provide comprehensive evidence that selective inhibition or modulation of glycogenolysis does not adversely affect normal metabolic functions during periods of fasting or exercise. The FDA's Endocrinologic and Metabolic Drugs Advisory Committee often requires additional safety monitoring for such therapies.
Accelerated approval pathways exist for treatments addressing severe metabolic disorders with unmet medical needs, such as glycogen storage diseases and certain forms of diabetes with dysregulated glycogenolysis. These pathways can reduce development timelines by 1-3 years when surrogate endpoints like improved glycemic control or reduced hepatic glucose production are accepted as primary outcomes.
Biomarker validation represents another critical regulatory consideration. Agencies increasingly accept validated biomarkers of glycogenolysis activity as surrogate endpoints in clinical trials, provided these markers demonstrate strong correlation with clinical outcomes. This approach has facilitated the development of several metabolic therapeutics in recent years.
Global regulatory harmonization efforts through the International Council for Harmonisation (ICH) have streamlined the approval process for metabolic therapeutics across major markets. However, significant regional differences persist in the evaluation of benefit-risk profiles for glycogenolysis-targeting agents, particularly regarding acceptable levels of hypoglycemia risk and long-term safety monitoring requirements.
Post-marketing surveillance requirements for novel metabolic therapeutics are typically extensive, with regulatory agencies mandating long-term safety studies to monitor for rare adverse events and cardiovascular outcomes. This is particularly relevant for glycogenolysis modulators, as their effects on cardiovascular risk factors and overall metabolic health must be thoroughly characterized beyond initial approval.
Regulatory engagement strategies have evolved significantly, with successful developers initiating early and frequent consultation with agencies through formal and informal meetings. This collaborative approach has proven effective in addressing regulatory concerns proactively and designing development programs that satisfy both scientific and regulatory requirements for novel metabolic therapeutics targeting glycogenolysis.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!