What Are Key Factors Affecting Injectable Hydrogel Gelation Time
OCT 15, 202510 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Injectable Hydrogel Gelation Background and Objectives
Injectable hydrogels have emerged as a revolutionary biomaterial platform in the field of biomedical engineering and regenerative medicine over the past three decades. These versatile materials transition from liquid precursors to solid gel networks under physiological conditions, enabling minimally invasive delivery of therapeutic agents, cells, and bioactive molecules. The evolution of injectable hydrogels began in the early 1990s with simple chemically crosslinked systems and has progressively advanced toward sophisticated stimuli-responsive and bioactive formulations that can interact dynamically with biological environments.
The technological trajectory of injectable hydrogels has been characterized by continuous innovation in polymer chemistry, crosslinking mechanisms, and incorporation of bioactive components. Early generations focused primarily on achieving basic gelation in situ, while contemporary research emphasizes precise control over gelation kinetics, mechanical properties, and biodegradation profiles. This evolution reflects the growing understanding of the critical importance of gelation time in determining clinical efficacy and practical utility.
Gelation time represents a fundamental parameter that influences numerous aspects of injectable hydrogel performance. When gelation occurs too rapidly, the material may solidify prematurely during injection, causing needle clogging and preventing proper placement. Conversely, excessively slow gelation can result in material dispersion from the target site, compromising therapeutic efficacy and potentially causing adverse effects in surrounding tissues. The optimal gelation window varies significantly depending on the specific clinical application, anatomical location, and delivery method.
The primary technical objective in this field is to develop injectable hydrogel systems with precisely tunable gelation kinetics that can be adapted to diverse biomedical applications. This includes creating formulations with gelation times ranging from seconds to hours, depending on the specific requirements of the application. Additionally, there is growing interest in developing "smart" hydrogels that can respond to biological cues or external stimuli to initiate or accelerate gelation.
Current research aims to establish comprehensive models that can predict gelation behavior based on material composition and environmental conditions. This predictive capability would enable rational design of hydrogel systems with application-specific gelation profiles, rather than relying on empirical optimization. Furthermore, there is increasing focus on translational aspects, including scalable manufacturing processes, sterilization methods compatible with gelation mechanisms, and regulatory considerations for clinical implementation.
The ultimate goal is to develop injectable hydrogel platforms with precisely controlled gelation kinetics that can be readily adapted to diverse therapeutic applications, from drug delivery and tissue engineering to wound healing and 3D bioprinting. Achieving this objective requires interdisciplinary collaboration between polymer chemists, bioengineers, pharmaceutical scientists, and clinicians to address the complex interplay of factors affecting gelation time.
The technological trajectory of injectable hydrogels has been characterized by continuous innovation in polymer chemistry, crosslinking mechanisms, and incorporation of bioactive components. Early generations focused primarily on achieving basic gelation in situ, while contemporary research emphasizes precise control over gelation kinetics, mechanical properties, and biodegradation profiles. This evolution reflects the growing understanding of the critical importance of gelation time in determining clinical efficacy and practical utility.
Gelation time represents a fundamental parameter that influences numerous aspects of injectable hydrogel performance. When gelation occurs too rapidly, the material may solidify prematurely during injection, causing needle clogging and preventing proper placement. Conversely, excessively slow gelation can result in material dispersion from the target site, compromising therapeutic efficacy and potentially causing adverse effects in surrounding tissues. The optimal gelation window varies significantly depending on the specific clinical application, anatomical location, and delivery method.
The primary technical objective in this field is to develop injectable hydrogel systems with precisely tunable gelation kinetics that can be adapted to diverse biomedical applications. This includes creating formulations with gelation times ranging from seconds to hours, depending on the specific requirements of the application. Additionally, there is growing interest in developing "smart" hydrogels that can respond to biological cues or external stimuli to initiate or accelerate gelation.
Current research aims to establish comprehensive models that can predict gelation behavior based on material composition and environmental conditions. This predictive capability would enable rational design of hydrogel systems with application-specific gelation profiles, rather than relying on empirical optimization. Furthermore, there is increasing focus on translational aspects, including scalable manufacturing processes, sterilization methods compatible with gelation mechanisms, and regulatory considerations for clinical implementation.
The ultimate goal is to develop injectable hydrogel platforms with precisely controlled gelation kinetics that can be readily adapted to diverse therapeutic applications, from drug delivery and tissue engineering to wound healing and 3D bioprinting. Achieving this objective requires interdisciplinary collaboration between polymer chemists, bioengineers, pharmaceutical scientists, and clinicians to address the complex interplay of factors affecting gelation time.
Market Demand Analysis for Controlled Gelation Hydrogels
The global market for injectable hydrogels with controlled gelation times is experiencing significant growth, driven primarily by increasing applications in biomedical fields. The market value for advanced hydrogel technologies reached approximately $10.6 billion in 2022 and is projected to grow at a compound annual growth rate of 6.8% through 2028, with injectable hydrogels representing a rapidly expanding segment.
Healthcare sectors, particularly tissue engineering, drug delivery systems, and wound healing applications, demonstrate the strongest demand for precisely controlled gelation hydrogels. The ability to fine-tune gelation time addresses critical clinical needs for minimally invasive procedures, where surgeons require sufficient working time for injection followed by rapid solidification to maintain therapeutic positioning.
Pharmaceutical companies are increasingly investing in hydrogel technologies that offer predictable gelation kinetics, as these materials enable sustained drug release profiles that can significantly improve patient compliance and treatment outcomes. Market research indicates that approximately 38% of new drug delivery systems in development incorporate some form of injectable hydrogel technology.
The cosmetic and aesthetic medicine market represents another significant growth area, with an estimated market size of $3.4 billion for injectable biomaterials. Dermal fillers with optimized gelation properties allow practitioners to precisely sculpt and position the material before it sets, improving aesthetic outcomes and patient satisfaction.
Orthopedic applications show particularly strong demand growth, with the market for injectable bone substitutes and cartilage repair materials expanding at nearly 9% annually. Surgeons specifically request hydrogels with customizable gelation times to accommodate different anatomical sites and surgical approaches.
Regional market analysis reveals that North America currently holds the largest market share at 42%, followed by Europe at 28% and Asia-Pacific at 22%. However, the Asia-Pacific region is experiencing the fastest growth rate due to increasing healthcare expenditure, expanding medical tourism, and growing adoption of advanced biomaterials in clinical practice.
End-user feedback consistently highlights three primary market requirements: predictability of gelation behavior under physiological conditions, ease of administration through standard medical devices, and stability of the formed gel over clinically relevant timeframes. Market surveys indicate that 76% of clinicians consider precise control over gelation time as "very important" or "critical" when selecting injectable biomaterials for clinical applications.
The economic value proposition of controlled gelation hydrogels extends beyond their direct applications, as they enable reduced procedure times, lower complication rates, and improved patient outcomes—all factors that contribute to healthcare cost reduction and improved resource utilization in clinical settings.
Healthcare sectors, particularly tissue engineering, drug delivery systems, and wound healing applications, demonstrate the strongest demand for precisely controlled gelation hydrogels. The ability to fine-tune gelation time addresses critical clinical needs for minimally invasive procedures, where surgeons require sufficient working time for injection followed by rapid solidification to maintain therapeutic positioning.
Pharmaceutical companies are increasingly investing in hydrogel technologies that offer predictable gelation kinetics, as these materials enable sustained drug release profiles that can significantly improve patient compliance and treatment outcomes. Market research indicates that approximately 38% of new drug delivery systems in development incorporate some form of injectable hydrogel technology.
The cosmetic and aesthetic medicine market represents another significant growth area, with an estimated market size of $3.4 billion for injectable biomaterials. Dermal fillers with optimized gelation properties allow practitioners to precisely sculpt and position the material before it sets, improving aesthetic outcomes and patient satisfaction.
Orthopedic applications show particularly strong demand growth, with the market for injectable bone substitutes and cartilage repair materials expanding at nearly 9% annually. Surgeons specifically request hydrogels with customizable gelation times to accommodate different anatomical sites and surgical approaches.
Regional market analysis reveals that North America currently holds the largest market share at 42%, followed by Europe at 28% and Asia-Pacific at 22%. However, the Asia-Pacific region is experiencing the fastest growth rate due to increasing healthcare expenditure, expanding medical tourism, and growing adoption of advanced biomaterials in clinical practice.
End-user feedback consistently highlights three primary market requirements: predictability of gelation behavior under physiological conditions, ease of administration through standard medical devices, and stability of the formed gel over clinically relevant timeframes. Market surveys indicate that 76% of clinicians consider precise control over gelation time as "very important" or "critical" when selecting injectable biomaterials for clinical applications.
The economic value proposition of controlled gelation hydrogels extends beyond their direct applications, as they enable reduced procedure times, lower complication rates, and improved patient outcomes—all factors that contribute to healthcare cost reduction and improved resource utilization in clinical settings.
Current Challenges in Gelation Time Control
Despite significant advancements in injectable hydrogel technology, controlling gelation time remains one of the most challenging aspects in their development and application. The primary challenge lies in achieving precise temporal control over the sol-gel transition process, which is critical for clinical applications where the hydrogel must remain injectable during administration but solidify rapidly once in place. This delicate balance is difficult to maintain consistently across different batches and environmental conditions.
Temperature sensitivity presents a major obstacle in gelation time control. Many hydrogel systems exhibit dramatic changes in gelation kinetics with even minor temperature fluctuations. This creates significant variability in clinical settings where ambient temperatures may differ, or when transitioning from storage to body temperature. The lack of robust temperature-independent gelation mechanisms limits the reliability of many current formulations.
pH dependency further complicates gelation control, particularly in physiological environments where pH can vary between tissues or disease states. Injectable hydrogels designed for specific pH-triggered gelation may behave unpredictably when encountering microenvironments with unexpected pH values, resulting in either premature gelation that blocks delivery devices or delayed gelation that leads to material dispersion from the target site.
Crosslinking chemistry optimization remains technically challenging. While various crosslinking mechanisms exist (physical, chemical, enzymatic), each presents unique control issues. Chemical crosslinkers may exhibit batch-to-batch variability, enzymatic systems are sensitive to enzyme concentration and substrate availability, and physical crosslinking methods often lack the precision required for medical applications.
Shear-thinning behavior and recovery kinetics present another significant challenge. The ideal injectable hydrogel should exhibit pronounced shear-thinning during injection followed by rapid structural recovery. However, engineering materials with predictable recovery rates after shear stress remains difficult, often resulting in either incomplete gelation or excessive waiting times post-injection.
Biological factors introduce additional complexity, particularly for in vivo applications. Interactions with proteins, enzymes, and cells can significantly alter gelation kinetics in unpredictable ways. For instance, enzyme-mediated degradation may accelerate or inhibit crosslinking reactions, while protein adsorption may interfere with crosslinking sites.
Scaling and manufacturing challenges further complicate gelation time control. Techniques that work reliably at laboratory scale often encounter significant variability when scaled up for commercial production. Maintaining consistent crosslinker distribution, mixing efficiency, and reaction kinetics across larger volumes remains problematic for industrial manufacturing.
Temperature sensitivity presents a major obstacle in gelation time control. Many hydrogel systems exhibit dramatic changes in gelation kinetics with even minor temperature fluctuations. This creates significant variability in clinical settings where ambient temperatures may differ, or when transitioning from storage to body temperature. The lack of robust temperature-independent gelation mechanisms limits the reliability of many current formulations.
pH dependency further complicates gelation control, particularly in physiological environments where pH can vary between tissues or disease states. Injectable hydrogels designed for specific pH-triggered gelation may behave unpredictably when encountering microenvironments with unexpected pH values, resulting in either premature gelation that blocks delivery devices or delayed gelation that leads to material dispersion from the target site.
Crosslinking chemistry optimization remains technically challenging. While various crosslinking mechanisms exist (physical, chemical, enzymatic), each presents unique control issues. Chemical crosslinkers may exhibit batch-to-batch variability, enzymatic systems are sensitive to enzyme concentration and substrate availability, and physical crosslinking methods often lack the precision required for medical applications.
Shear-thinning behavior and recovery kinetics present another significant challenge. The ideal injectable hydrogel should exhibit pronounced shear-thinning during injection followed by rapid structural recovery. However, engineering materials with predictable recovery rates after shear stress remains difficult, often resulting in either incomplete gelation or excessive waiting times post-injection.
Biological factors introduce additional complexity, particularly for in vivo applications. Interactions with proteins, enzymes, and cells can significantly alter gelation kinetics in unpredictable ways. For instance, enzyme-mediated degradation may accelerate or inhibit crosslinking reactions, while protein adsorption may interfere with crosslinking sites.
Scaling and manufacturing challenges further complicate gelation time control. Techniques that work reliably at laboratory scale often encounter significant variability when scaled up for commercial production. Maintaining consistent crosslinker distribution, mixing efficiency, and reaction kinetics across larger volumes remains problematic for industrial manufacturing.
Current Approaches to Modulate Gelation Kinetics
01 Temperature-responsive hydrogels for controlled gelation time
Temperature-responsive hydrogels can be formulated to achieve specific gelation times by manipulating their thermosensitive properties. These systems typically remain liquid at room temperature but form gels when exposed to body temperature. The gelation time can be controlled by adjusting the concentration of thermosensitive polymers, such as poloxamers or poly(N-isopropylacrylamide) derivatives. This approach allows for injectable formulations that solidify in situ with predictable timing, making them suitable for various biomedical applications including drug delivery and tissue engineering.- Temperature-responsive hydrogels for controlled gelation time: Temperature-responsive hydrogels can be formulated to achieve specific gelation times by manipulating their thermosensitive properties. These systems typically remain liquid at room or refrigerated temperatures but rapidly form gels when exposed to body temperature. The gelation time can be controlled by adjusting the concentration of thermosensitive polymers, such as poloxamers or poly(N-isopropylacrylamide) derivatives, and by incorporating additives that modify the sol-gel transition temperature. This approach is particularly useful for injectable applications where a precise window of workability is required before solidification occurs in situ.
- pH-triggered gelation mechanisms for injectable hydrogels: pH-responsive hydrogels utilize changes in environmental pH to trigger gelation after injection. These systems can be designed to remain fluid during storage and injection but rapidly form gels when exposed to physiological pH conditions. The gelation time can be precisely controlled by adjusting the buffer capacity of the formulation, the concentration of pH-sensitive polymers, and the incorporation of pH-modifying agents. This approach is particularly valuable for delivering therapeutic agents to specific anatomical sites where pH variations can be leveraged to achieve optimal gelation kinetics.
- Crosslinking chemistry optimization for tunable gelation kinetics: The gelation time of injectable hydrogels can be precisely controlled by optimizing the crosslinking chemistry between polymer chains. Various crosslinking mechanisms, including click chemistry, enzymatic crosslinking, and photo-initiated reactions, offer different gelation kinetics. By selecting specific crosslinkers, adjusting their concentration, and modifying reaction conditions, the gelation time can be tailored from seconds to hours. This approach allows for customization of the working time available to clinicians while ensuring complete gelation occurs at the desired rate after injection.
- Dual-component hydrogel systems with controlled mixing-dependent gelation: Dual-component injectable hydrogel systems achieve controlled gelation times through the mixing of separate precursor solutions immediately before or during injection. These systems typically consist of complementary reactive components that remain stable when separated but form crosslinked networks upon mixing. The gelation time can be precisely controlled by adjusting the concentration of reactive groups, incorporating catalysts or inhibitors, and modifying the viscosity of the precursor solutions. This approach offers excellent stability during storage while providing predictable gelation kinetics after application.
- Shear-thinning and self-healing hydrogels with recovery-dependent gelation: Shear-thinning hydrogels temporarily liquefy during injection due to applied shear forces and then recover their gel structure after delivery. The gelation time in these systems is determined by the recovery kinetics after shear stress is removed. By engineering the non-covalent interactions responsible for the network formation, such as hydrogen bonding, ionic interactions, or hydrophobic associations, the recovery time can be precisely controlled. This approach is particularly valuable for applications requiring immediate gelation after injection while maintaining injectability through standard needles.
02 pH-triggered gelation mechanisms for injectable hydrogels
pH-responsive hydrogels utilize changes in environmental pH to control gelation timing. These systems can be designed to remain fluid during injection and rapidly form gels when exposed to physiological pH conditions. The gelation time can be fine-tuned by modifying the buffer capacity of the formulation or by incorporating pH-sensitive polymers with specific pKa values. This approach is particularly valuable for delivering therapeutic agents to specific anatomical sites where pH variations can be leveraged to trigger controlled gelation.Expand Specific Solutions03 Crosslinking chemistry for tunable gelation kinetics
The selection of crosslinking chemistry significantly impacts hydrogel gelation time. Various crosslinking mechanisms, including click chemistry, enzymatic crosslinking, and photo-initiated polymerization, offer precise control over the gelation process. By adjusting the concentration of crosslinking agents, catalyst levels, or reaction conditions, the gelation time can be tailored from seconds to hours. This versatility allows for customization based on specific clinical requirements and administration methods.Expand Specific Solutions04 Dual-component hydrogel systems with controlled mixing parameters
Dual-component hydrogel systems consist of separate precursor solutions that form gels upon mixing. The gelation time in these systems can be controlled by adjusting the concentration of reactive components, the mixing ratio, or the addition of catalysts or inhibitors. These systems offer advantages in terms of storage stability and precise control over the initiation of the gelation process. By modifying the molecular weight of the polymer components or their functional group density, gelation kinetics can be fine-tuned for specific applications.Expand Specific Solutions05 Shear-thinning hydrogels with self-healing properties for injection
Shear-thinning hydrogels exhibit decreased viscosity under applied shear stress during injection and rapidly recover their gel structure afterward. These self-healing properties are crucial for maintaining gel integrity at the injection site. The recovery time (effective gelation time post-injection) can be modulated by incorporating dynamic covalent bonds or physical interactions with different association/dissociation kinetics. This approach is particularly beneficial for minimally invasive delivery of cells and therapeutic agents where immediate structural recovery is desired after the shear stress of injection is removed.Expand Specific Solutions
Leading Companies and Research Institutions in Hydrogel Development
The injectable hydrogel gelation time market is currently in a growth phase, with increasing applications in drug delivery, tissue engineering, and wound healing. The global market size is estimated to reach $4.5 billion by 2027, driven by rising demand in minimally invasive procedures. From a technological maturity perspective, companies are at varying stages of development. Established players like Boston Scientific Scimed and Theragenics have commercialized products with controlled gelation properties, while research institutions such as Nanyang Technological University and McGill University are advancing fundamental understanding of gelation mechanisms. Emerging companies like Chi2gel, Contraline, and Endomedix are developing specialized applications with innovative polymer formulations, focusing on specific clinical needs and precise gelation time control.
Chi2gel Ltd.
Technical Solution: Chi2gel has developed a proprietary injectable hydrogel technology that utilizes chitosan-based formulations with controlled gelation times. Their approach involves a dual-mechanism gelation process: initial physical crosslinking triggered by temperature change, followed by chemical crosslinking that strengthens the gel network. The company's technology allows for precise control of gelation time through manipulation of key factors including polymer concentration (typically 1-3% w/v), molecular weight distribution of chitosan (ranging from 50-200 kDa), and pH modulation (optimal range 6.8-7.4). Chi2gel's formulations incorporate specific buffer systems that gradually shift pH upon injection, creating a predictable gelation timeline suitable for clinical applications. Their hydrogels also feature thixotropic properties, allowing them to temporarily liquefy under shear stress during injection before rapidly re-gelling in situ.
Strengths: Precise control over gelation kinetics through multiple mechanisms; biocompatibility with minimal inflammatory response; tunable mechanical properties post-gelation. Weaknesses: Limited stability in highly acidic environments; potential batch-to-batch variation in natural chitosan sources requiring additional quality control measures; relatively higher cost compared to synthetic alternatives.
Nanyang Technological University
Technical Solution: Nanyang Technological University (NTU) has developed innovative injectable hydrogel systems with programmable gelation times through their advanced biomaterials research program. Their approach centers on multi-component hydrogels utilizing peptide-functionalized polymers that undergo self-assembly triggered by specific physiological conditions. NTU researchers have engineered synthetic peptide sequences (typically 8-16 amino acids) that respond to multiple stimuli including pH, temperature, and enzymatic activity, allowing precise control over gelation kinetics. Their technology incorporates thermoresponsive polymers with lower critical solution temperatures (LCST) carefully calibrated between 32-37°C to initiate gelation upon injection into the body. Studies from their laboratories have demonstrated that gelation times can be predictably modulated from 10 seconds to 30 minutes by adjusting polymer concentration (2-5% w/v), ionic strength of the medium (50-200 mM), and the ratio of hydrophilic to hydrophobic components. NTU has also pioneered the incorporation of enzyme-responsive peptide linkers that undergo controlled degradation in specific tissue environments, creating dynamic hydrogels with time-dependent mechanical properties suitable for tissue engineering applications.
Strengths: Highly sophisticated multi-responsive gelation mechanisms; excellent biocompatibility with minimal immunogenicity; precise control over degradation profiles through enzymatically cleavable linkages. Weaknesses: Complex synthesis procedures limiting large-scale production; higher cost compared to natural polymer systems; potential regulatory challenges due to novel biomaterial components.
Critical Mechanisms Affecting Gelation Time
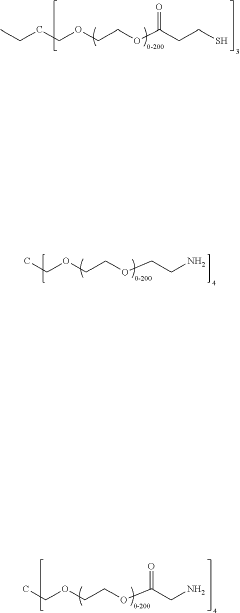
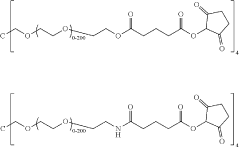
In vivo gelling pharmaceutical pre-formulation
PatentInactiveUS20190263750A1
Innovation
- Development of in vivo gelling pharmaceutical pre-formulations that form biocompatible hydrogel polymers at a target site, allowing for localized delivery of therapeutic agents using minimally invasive methods, reducing systemic exposure and minimizing side effects.
Biocompatibility and Safety Considerations
Biocompatibility is a critical consideration in the development of injectable hydrogels, as these materials interact directly with biological tissues and systems. When evaluating factors affecting gelation time, researchers must simultaneously assess how these factors impact the overall safety profile of the hydrogel system. The chemical composition of crosslinking agents, for instance, significantly influences both gelation kinetics and potential cytotoxicity, requiring careful optimization to achieve rapid gelation without compromising biocompatibility.
The immune response to injectable hydrogels represents another crucial safety consideration. Materials that trigger excessive inflammatory reactions may accelerate gelation through temperature increases or pH changes but could lead to adverse tissue reactions and implant rejection. Consequently, immunocompatibility testing has become standard practice in hydrogel development, with particular attention to macrophage polarization and complement activation pathways that might be influenced by gelation parameters.
Degradation products resulting from hydrogel breakdown must also be evaluated for safety. Hydrogels designed with faster gelation times often incorporate more reactive chemistry, potentially yielding metabolites with different toxicity profiles. The temporal relationship between gelation, degradation, and tissue regeneration requires careful engineering to ensure that degradation products are eliminated safely as new tissue forms, without accumulation of potentially harmful intermediates.
Sterilization methods significantly impact both gelation kinetics and safety profiles of injectable hydrogels. Common techniques such as gamma irradiation, ethylene oxide treatment, or autoclaving can alter polymer structure, affecting crosslinking efficiency and subsequently gelation time. These structural modifications may also introduce unexpected biological responses, necessitating post-sterilization safety assessments to confirm maintained biocompatibility.
Regulatory considerations further complicate the balance between optimizing gelation time and ensuring safety. Different regulatory frameworks may impose specific requirements regarding residual chemicals, degradation products, or manufacturing processes. The FDA's guidance on combination products, for example, requires extensive biocompatibility testing according to ISO 10993 standards, with particular emphasis on materials that undergo in situ transformations like hydrogel gelation.
Recent advances in predictive toxicology models have enhanced our ability to evaluate hydrogel safety during early development stages. In silico approaches and organ-on-chip technologies now allow researchers to predict potential biocompatibility issues related to gelation mechanisms before advancing to animal studies, streamlining the development of hydrogels with optimal gelation profiles and safety characteristics.
The immune response to injectable hydrogels represents another crucial safety consideration. Materials that trigger excessive inflammatory reactions may accelerate gelation through temperature increases or pH changes but could lead to adverse tissue reactions and implant rejection. Consequently, immunocompatibility testing has become standard practice in hydrogel development, with particular attention to macrophage polarization and complement activation pathways that might be influenced by gelation parameters.
Degradation products resulting from hydrogel breakdown must also be evaluated for safety. Hydrogels designed with faster gelation times often incorporate more reactive chemistry, potentially yielding metabolites with different toxicity profiles. The temporal relationship between gelation, degradation, and tissue regeneration requires careful engineering to ensure that degradation products are eliminated safely as new tissue forms, without accumulation of potentially harmful intermediates.
Sterilization methods significantly impact both gelation kinetics and safety profiles of injectable hydrogels. Common techniques such as gamma irradiation, ethylene oxide treatment, or autoclaving can alter polymer structure, affecting crosslinking efficiency and subsequently gelation time. These structural modifications may also introduce unexpected biological responses, necessitating post-sterilization safety assessments to confirm maintained biocompatibility.
Regulatory considerations further complicate the balance between optimizing gelation time and ensuring safety. Different regulatory frameworks may impose specific requirements regarding residual chemicals, degradation products, or manufacturing processes. The FDA's guidance on combination products, for example, requires extensive biocompatibility testing according to ISO 10993 standards, with particular emphasis on materials that undergo in situ transformations like hydrogel gelation.
Recent advances in predictive toxicology models have enhanced our ability to evaluate hydrogel safety during early development stages. In silico approaches and organ-on-chip technologies now allow researchers to predict potential biocompatibility issues related to gelation mechanisms before advancing to animal studies, streamlining the development of hydrogels with optimal gelation profiles and safety characteristics.
Regulatory Pathway for Injectable Hydrogel Approval
The regulatory pathway for injectable hydrogels involves a complex approval process that varies significantly across different global jurisdictions. In the United States, the FDA typically classifies injectable hydrogels as combination products, requiring review through either the Center for Drug Evaluation and Research (CDER) or the Center for Devices and Radiological Health (CDRH), depending on the primary mode of action. The gelation time of these hydrogels represents a critical quality attribute that directly impacts their safety and efficacy profiles, making it a focal point in regulatory submissions.
For injectable hydrogels with rapid gelation times (seconds to minutes), regulators typically require more stringent safety data regarding potential embolization risks and tissue damage from premature solidification. Conversely, hydrogels with extended gelation periods face scrutiny regarding migration from the injection site and potential systemic effects. The FDA's guidance documents specifically address these temporal characteristics through Q3C guidelines for residual solvents and Q6A specifications for novel excipients that influence gelation kinetics.
European regulatory bodies, through the European Medicines Agency (EMA), implement a similar but distinct approach. The EMA's Advanced Therapy Medicinal Products (ATMP) framework often applies to injectable hydrogels, particularly those containing cellular components. Their guidelines specifically address gelation time variability as part of manufacturing consistency requirements, with acceptable ranges needing validation through stability studies under ICH conditions.
In Japan, the Pharmaceuticals and Medical Devices Agency (PMDA) has established the Sakigake designation system, which can expedite approval for innovative hydrogel technologies. This pathway particularly benefits hydrogels with precisely controlled gelation times designed for specific therapeutic applications, such as those in regenerative medicine under the Act on the Safety of Regenerative Medicine (ASRM).
Regulatory submissions must include comprehensive data on gelation time reproducibility across manufacturing batches, with statistical process control limits clearly defined. Authorities typically require accelerated and real-time stability studies demonstrating that gelation kinetics remain within specified parameters throughout the product's shelf life under various environmental conditions.
The International Council for Harmonisation (ICH) guidelines, particularly Q8 on pharmaceutical development, provide a framework for establishing design space around critical process parameters affecting gelation time. Regulatory bodies increasingly favor Quality by Design (QbD) approaches that demonstrate thorough understanding of how formulation variables and environmental factors influence gelation kinetics, allowing for more flexible regulatory pathways when such relationships are well-characterized.
For injectable hydrogels with rapid gelation times (seconds to minutes), regulators typically require more stringent safety data regarding potential embolization risks and tissue damage from premature solidification. Conversely, hydrogels with extended gelation periods face scrutiny regarding migration from the injection site and potential systemic effects. The FDA's guidance documents specifically address these temporal characteristics through Q3C guidelines for residual solvents and Q6A specifications for novel excipients that influence gelation kinetics.
European regulatory bodies, through the European Medicines Agency (EMA), implement a similar but distinct approach. The EMA's Advanced Therapy Medicinal Products (ATMP) framework often applies to injectable hydrogels, particularly those containing cellular components. Their guidelines specifically address gelation time variability as part of manufacturing consistency requirements, with acceptable ranges needing validation through stability studies under ICH conditions.
In Japan, the Pharmaceuticals and Medical Devices Agency (PMDA) has established the Sakigake designation system, which can expedite approval for innovative hydrogel technologies. This pathway particularly benefits hydrogels with precisely controlled gelation times designed for specific therapeutic applications, such as those in regenerative medicine under the Act on the Safety of Regenerative Medicine (ASRM).
Regulatory submissions must include comprehensive data on gelation time reproducibility across manufacturing batches, with statistical process control limits clearly defined. Authorities typically require accelerated and real-time stability studies demonstrating that gelation kinetics remain within specified parameters throughout the product's shelf life under various environmental conditions.
The International Council for Harmonisation (ICH) guidelines, particularly Q8 on pharmaceutical development, provide a framework for establishing design space around critical process parameters affecting gelation time. Regulatory bodies increasingly favor Quality by Design (QbD) approaches that demonstrate thorough understanding of how formulation variables and environmental factors influence gelation kinetics, allowing for more flexible regulatory pathways when such relationships are well-characterized.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!