What Are the Latest Standards in Wearable Biosensor Regulation
OCT 24, 202510 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Biosensor Regulation Background and Objectives
Wearable biosensors have evolved significantly over the past decade, transforming from simple fitness trackers to sophisticated medical devices capable of continuous health monitoring. The regulatory landscape governing these technologies has similarly undergone substantial evolution, reflecting the increasing complexity and healthcare integration of these devices. Initially, wearable biosensors were primarily regulated as consumer electronics with minimal oversight. However, as their capabilities expanded to include critical health parameters monitoring such as blood glucose, cardiac activity, and oxygen saturation, regulatory bodies worldwide began developing more comprehensive frameworks.
The current regulatory environment for wearable biosensors exists at the intersection of medical device regulation, data privacy legislation, and consumer protection standards. Key regulatory bodies including the FDA in the United States, the European Medicines Agency in Europe, and the NMPA in China have established varying approaches to biosensor oversight. The FDA's Digital Health Innovation Action Plan and the EU's Medical Device Regulation (MDR) represent significant milestones in establishing clearer pathways for innovative biosensor technologies while ensuring patient safety.
Recent technological advancements have accelerated the need for updated regulatory frameworks. The integration of artificial intelligence for real-time data analysis, the development of minimally invasive continuous monitoring systems, and the emergence of closed-loop therapeutic systems have pushed regulatory boundaries. These innovations enable not just passive monitoring but active intervention based on physiological data, raising the stakes for regulatory oversight.
The primary objective of contemporary biosensor regulation is to balance innovation facilitation with risk mitigation. Regulators aim to establish standards that ensure device safety, accuracy, and reliability without impeding technological advancement. This includes developing appropriate validation protocols for novel sensing modalities and establishing interoperability standards to support healthcare system integration.
Data security and privacy protection represent another critical regulatory focus area. As wearable biosensors collect increasingly sensitive health information, regulations such as GDPR in Europe and HIPAA in the US have become central to biosensor governance. These frameworks establish requirements for data encryption, user consent mechanisms, and breach notification protocols.
Looking forward, regulatory trends indicate movement toward more adaptive and collaborative approaches. Regulatory sandboxes, where innovative technologies can be tested under modified regulatory conditions, are gaining traction. Additionally, international harmonization efforts seek to reduce regulatory fragmentation across markets, potentially accelerating global access to innovative biosensor technologies while maintaining consistent safety standards.
The evolution of biosensor regulation reflects broader shifts in healthcare delivery models, with increasing emphasis on preventive care, remote monitoring, and personalized medicine. As these technologies become more integrated into clinical decision-making processes, regulatory frameworks continue to adapt to ensure appropriate oversight while supporting the transformative potential of wearable biosensor technologies.
The current regulatory environment for wearable biosensors exists at the intersection of medical device regulation, data privacy legislation, and consumer protection standards. Key regulatory bodies including the FDA in the United States, the European Medicines Agency in Europe, and the NMPA in China have established varying approaches to biosensor oversight. The FDA's Digital Health Innovation Action Plan and the EU's Medical Device Regulation (MDR) represent significant milestones in establishing clearer pathways for innovative biosensor technologies while ensuring patient safety.
Recent technological advancements have accelerated the need for updated regulatory frameworks. The integration of artificial intelligence for real-time data analysis, the development of minimally invasive continuous monitoring systems, and the emergence of closed-loop therapeutic systems have pushed regulatory boundaries. These innovations enable not just passive monitoring but active intervention based on physiological data, raising the stakes for regulatory oversight.
The primary objective of contemporary biosensor regulation is to balance innovation facilitation with risk mitigation. Regulators aim to establish standards that ensure device safety, accuracy, and reliability without impeding technological advancement. This includes developing appropriate validation protocols for novel sensing modalities and establishing interoperability standards to support healthcare system integration.
Data security and privacy protection represent another critical regulatory focus area. As wearable biosensors collect increasingly sensitive health information, regulations such as GDPR in Europe and HIPAA in the US have become central to biosensor governance. These frameworks establish requirements for data encryption, user consent mechanisms, and breach notification protocols.
Looking forward, regulatory trends indicate movement toward more adaptive and collaborative approaches. Regulatory sandboxes, where innovative technologies can be tested under modified regulatory conditions, are gaining traction. Additionally, international harmonization efforts seek to reduce regulatory fragmentation across markets, potentially accelerating global access to innovative biosensor technologies while maintaining consistent safety standards.
The evolution of biosensor regulation reflects broader shifts in healthcare delivery models, with increasing emphasis on preventive care, remote monitoring, and personalized medicine. As these technologies become more integrated into clinical decision-making processes, regulatory frameworks continue to adapt to ensure appropriate oversight while supporting the transformative potential of wearable biosensor technologies.
Market Demand Analysis for Regulated Wearable Biosensors
The global market for wearable biosensors is experiencing unprecedented growth, driven by increasing health consciousness, aging populations, and the rising prevalence of chronic diseases. Current market valuations place the regulated wearable biosensor sector at approximately 15 billion USD in 2023, with projections indicating a compound annual growth rate of 18-20% through 2028. This remarkable expansion reflects the growing consumer demand for continuous health monitoring solutions that can provide actionable insights while meeting regulatory standards.
Healthcare providers represent a significant market segment, increasingly adopting regulated wearable biosensors to enhance remote patient monitoring capabilities and improve clinical outcomes. The COVID-19 pandemic has accelerated this trend, with hospitals and clinics seeking FDA-cleared or CE-marked devices that can reliably monitor vital signs while reducing in-person visits. This shift toward telehealth integration has created a substantial market opportunity for biosensor manufacturers who can navigate the complex regulatory landscape.
Consumer demand is equally robust, with end-users showing strong preference for devices that offer both lifestyle tracking and medically validated health monitoring. Market research indicates that consumers are increasingly willing to pay premium prices for biosensors with regulatory clearance, perceiving them as more accurate and trustworthy than unregulated alternatives. This trend is particularly pronounced among older adults and individuals managing chronic conditions such as diabetes, cardiovascular disease, and respiratory disorders.
Geographically, North America currently dominates the regulated wearable biosensor market, accounting for approximately 40% of global revenue. However, the Asia-Pacific region is expected to witness the fastest growth rate in the coming years, driven by improving healthcare infrastructure, increasing disposable income, and supportive government initiatives promoting digital health technologies.
From a technological perspective, the market is witnessing a shift toward multimodal biosensors capable of monitoring multiple physiological parameters simultaneously. Continuous glucose monitoring systems represent the largest sub-segment by revenue, followed by cardiac monitoring devices and sleep tracking solutions. Emerging applications in sweat analysis, transcutaneous drug delivery monitoring, and neurological assessment are expected to create new market opportunities as regulatory frameworks evolve to accommodate these innovations.
Industry stakeholders identify regulatory compliance as both a significant barrier to entry and a competitive advantage. Market analysis reveals that products with FDA clearance or equivalent international certifications command price premiums of 30-45% compared to similar unregulated devices. This premium reflects not only the additional development costs associated with regulatory approval but also the enhanced market positioning and consumer trust these certifications provide.
Healthcare providers represent a significant market segment, increasingly adopting regulated wearable biosensors to enhance remote patient monitoring capabilities and improve clinical outcomes. The COVID-19 pandemic has accelerated this trend, with hospitals and clinics seeking FDA-cleared or CE-marked devices that can reliably monitor vital signs while reducing in-person visits. This shift toward telehealth integration has created a substantial market opportunity for biosensor manufacturers who can navigate the complex regulatory landscape.
Consumer demand is equally robust, with end-users showing strong preference for devices that offer both lifestyle tracking and medically validated health monitoring. Market research indicates that consumers are increasingly willing to pay premium prices for biosensors with regulatory clearance, perceiving them as more accurate and trustworthy than unregulated alternatives. This trend is particularly pronounced among older adults and individuals managing chronic conditions such as diabetes, cardiovascular disease, and respiratory disorders.
Geographically, North America currently dominates the regulated wearable biosensor market, accounting for approximately 40% of global revenue. However, the Asia-Pacific region is expected to witness the fastest growth rate in the coming years, driven by improving healthcare infrastructure, increasing disposable income, and supportive government initiatives promoting digital health technologies.
From a technological perspective, the market is witnessing a shift toward multimodal biosensors capable of monitoring multiple physiological parameters simultaneously. Continuous glucose monitoring systems represent the largest sub-segment by revenue, followed by cardiac monitoring devices and sleep tracking solutions. Emerging applications in sweat analysis, transcutaneous drug delivery monitoring, and neurological assessment are expected to create new market opportunities as regulatory frameworks evolve to accommodate these innovations.
Industry stakeholders identify regulatory compliance as both a significant barrier to entry and a competitive advantage. Market analysis reveals that products with FDA clearance or equivalent international certifications command price premiums of 30-45% compared to similar unregulated devices. This premium reflects not only the additional development costs associated with regulatory approval but also the enhanced market positioning and consumer trust these certifications provide.
Current Regulatory Landscape and Challenges
The wearable biosensor market is currently navigating a complex regulatory environment characterized by fragmented standards across different regions. In the United States, the FDA has established a risk-based classification system for wearable biosensors, with Class I devices (low risk) facing minimal regulation, while Class II and III devices undergo increasingly stringent review processes. The FDA's Digital Health Innovation Action Plan has created pathways for expedited approval of certain digital health technologies, though many wearable biosensors still face lengthy approval timelines averaging 18-24 months.
The European Union has implemented the Medical Device Regulation (MDR) and In Vitro Diagnostic Regulation (IVDR), which introduced more rigorous requirements for clinical evidence, post-market surveillance, and unique device identification. These regulations have significantly impacted wearable biosensor manufacturers, particularly regarding software classification as a medical device (SaMD) when health claims are made.
In Asia, regulatory frameworks vary substantially. Japan's Pharmaceuticals and Medical Devices Agency (PMDA) has established specific pathways for software-based medical technologies, while China's National Medical Products Administration (NMPA) has recently updated its regulations to address the growing wearable technology sector, though implementation remains inconsistent.
A significant challenge in the current landscape is the lack of harmonized international standards specifically designed for wearable biosensors. The International Medical Device Regulators Forum (IMDRF) has been working to develop consensus documents, but adoption remains voluntary and inconsistent across jurisdictions. This regulatory fragmentation increases compliance costs and delays market entry for manufacturers operating globally.
Data privacy and security regulations present another layer of complexity. The EU's General Data Protection Regulation (GDPR), the California Consumer Privacy Act (CCPA), and similar legislation worldwide impose strict requirements on the collection, processing, and storage of personal health data. Wearable biosensor manufacturers must navigate these regulations alongside traditional medical device requirements.
Technical standards also remain in flux. While organizations like IEEE, ISO, and IEC have developed standards relevant to aspects of wearable technology (such as IEEE 11073 for personal health devices), comprehensive standards specifically addressing the unique characteristics of wearable biosensors—including accuracy under various conditions, long-term reliability, and interoperability—are still evolving.
The rapid pace of technological innovation further complicates regulation, as regulatory frameworks struggle to keep pace with advancements in materials science, miniaturization, and artificial intelligence integration in biosensing technologies. This creates uncertainty for manufacturers and potentially delays innovative products from reaching consumers and patients.
The European Union has implemented the Medical Device Regulation (MDR) and In Vitro Diagnostic Regulation (IVDR), which introduced more rigorous requirements for clinical evidence, post-market surveillance, and unique device identification. These regulations have significantly impacted wearable biosensor manufacturers, particularly regarding software classification as a medical device (SaMD) when health claims are made.
In Asia, regulatory frameworks vary substantially. Japan's Pharmaceuticals and Medical Devices Agency (PMDA) has established specific pathways for software-based medical technologies, while China's National Medical Products Administration (NMPA) has recently updated its regulations to address the growing wearable technology sector, though implementation remains inconsistent.
A significant challenge in the current landscape is the lack of harmonized international standards specifically designed for wearable biosensors. The International Medical Device Regulators Forum (IMDRF) has been working to develop consensus documents, but adoption remains voluntary and inconsistent across jurisdictions. This regulatory fragmentation increases compliance costs and delays market entry for manufacturers operating globally.
Data privacy and security regulations present another layer of complexity. The EU's General Data Protection Regulation (GDPR), the California Consumer Privacy Act (CCPA), and similar legislation worldwide impose strict requirements on the collection, processing, and storage of personal health data. Wearable biosensor manufacturers must navigate these regulations alongside traditional medical device requirements.
Technical standards also remain in flux. While organizations like IEEE, ISO, and IEC have developed standards relevant to aspects of wearable technology (such as IEEE 11073 for personal health devices), comprehensive standards specifically addressing the unique characteristics of wearable biosensors—including accuracy under various conditions, long-term reliability, and interoperability—are still evolving.
The rapid pace of technological innovation further complicates regulation, as regulatory frameworks struggle to keep pace with advancements in materials science, miniaturization, and artificial intelligence integration in biosensing technologies. This creates uncertainty for manufacturers and potentially delays innovative products from reaching consumers and patients.
Current Compliance Frameworks and Standards
01 FDA and international regulatory frameworks for wearable biosensors
Wearable biosensors must comply with various regulatory frameworks established by agencies like the FDA in the US and similar bodies internationally. These regulations typically classify biosensors based on their intended use, risk level, and functionality. Compliance requirements include clinical validation, safety testing, data security protocols, and quality management systems. Manufacturers must navigate these regulatory pathways to obtain necessary approvals before marketing their devices.- FDA and international regulatory frameworks for wearable biosensors: Wearable biosensors must comply with various regulatory frameworks, including FDA guidelines in the US and international standards. These regulations cover aspects such as medical device classification, clinical validation requirements, and approval processes. Manufacturers must navigate these regulatory pathways to ensure their wearable biosensors meet safety and effectiveness standards before market entry.
- Data privacy and security standards for biosensor information: Wearable biosensors collect sensitive health data that requires protection under various privacy regulations. Standards address data encryption, secure transmission protocols, user consent mechanisms, and storage requirements. Compliance with regulations such as HIPAA in the US, GDPR in Europe, and other regional data protection laws is essential for manufacturers developing biosensor technologies that collect, process, and transmit personal health information.
- Technical performance and accuracy standards: Regulatory standards establish minimum requirements for the technical performance and accuracy of wearable biosensors. These include specifications for measurement precision, reliability, sensitivity, and specificity across different environmental conditions and user populations. Standardized testing protocols ensure that biosensors provide consistent and clinically meaningful data for their intended use cases.
- Biocompatibility and safety requirements: Wearable biosensors that contact the skin or other body tissues must meet biocompatibility standards to prevent adverse reactions. Regulations specify testing requirements for material toxicity, irritation, sensitization, and long-term wear effects. Safety standards also address electrical safety, electromagnetic compatibility, and thermal considerations to protect users from potential hazards during normal operation and foreseeable misuse.
- Quality management systems and manufacturing standards: Manufacturers of wearable biosensors must implement quality management systems that comply with standards such as ISO 13485 for medical devices. These standards govern design controls, risk management processes, manufacturing practices, and post-market surveillance. Regulatory frameworks require documentation of quality processes, validation of production methods, and ongoing monitoring to ensure consistent product quality and safety throughout the product lifecycle.
02 Data privacy and security standards for biosensor information
Wearable biosensors collect sensitive health data that must be protected according to specific standards and regulations. These include requirements for secure data transmission, storage encryption, user consent mechanisms, and breach notification protocols. Standards such as HIPAA in the US, GDPR in Europe, and similar regulations worldwide govern how biosensor data must be handled, shared, and protected to maintain user privacy while enabling appropriate healthcare applications.Expand Specific Solutions03 Technical performance and accuracy standards
Regulatory standards specify minimum performance requirements for wearable biosensors, including measurement accuracy, precision, reliability, and consistency. These standards often require validation against reference methods, stability testing under various environmental conditions, and demonstration of reproducibility. Performance standards may vary based on the specific physiological parameters being measured, such as heart rate, blood oxygen levels, or glucose concentration.Expand Specific Solutions04 Biocompatibility and safety requirements
Wearable biosensors that contact the skin or other body tissues must meet strict biocompatibility and safety standards. These include testing for skin irritation, sensitization, cytotoxicity, and other potential adverse effects. Materials used in biosensor construction must be evaluated for long-term safety, and devices must demonstrate electrical safety compliance. Standards also address physical safety aspects such as heat generation, mechanical stress, and potential injury risks during normal use.Expand Specific Solutions05 Interoperability and communication protocol standards
Regulatory frameworks increasingly address the need for interoperability between wearable biosensors and healthcare systems. Standards specify communication protocols, data formats, and integration requirements to ensure biosensor data can be reliably transmitted to electronic health records and other medical systems. These standards promote consistent data exchange, reduce implementation barriers, and enable the integration of biosensor information into clinical decision-making processes while maintaining data integrity.Expand Specific Solutions
Key Regulatory Bodies and Industry Stakeholders
The wearable biosensor regulation landscape is evolving rapidly, currently positioned at the growth stage with an estimated market value exceeding $15 billion and projected annual growth of 25-30%. Major technology companies like Samsung Electronics, Google, and LG Electronics are driving commercial adoption, while academic institutions including MIT, Caltech, and Peking University focus on fundamental research advancements. Healthcare specialists such as Philips, Siemens Healthcare Diagnostics, and i-SENS are developing medical-grade applications with regulatory compliance. The regulatory framework remains fragmented globally, with companies like Goodix Technology and Polar Electro working to navigate FDA, CE, and regional certification requirements while balancing innovation with patient safety and data privacy concerns.
Samsung Electronics Co., Ltd.
Technical Solution: Samsung has developed a comprehensive approach to wearable biosensor regulation compliance through their Samsung Health platform. Their technology integrates FDA-cleared biosensors in devices like the Galaxy Watch series, which includes ECG monitoring, blood pressure tracking, and blood oxygen measurement capabilities. Samsung implements a multi-layered regulatory compliance framework that addresses both hardware certification and software validation requirements across different global markets. Their biosensors undergo rigorous clinical validation studies to meet regional regulatory standards including FDA (US), CE marking (Europe), and MFDS (Korea) requirements. Samsung's approach includes continuous remote monitoring capabilities with data encryption that complies with HIPAA and GDPR standards, ensuring both regulatory compliance and user privacy protection[1][3]. The company has also established partnerships with healthcare providers to ensure their biosensor data can be integrated into clinical workflows while maintaining regulatory compliance.
Strengths: Global regulatory expertise across multiple markets; established relationships with regulatory bodies; comprehensive validation protocols for biosensors. Weaknesses: Regulatory approval processes can delay product launches in certain markets; compliance requirements vary significantly by region requiring substantial resources to maintain multiple certifications.
Google LLC
Technical Solution: Google has developed a sophisticated regulatory compliance framework for wearable biosensors through its Fitbit and Pixel Watch product lines. The company employs a dual-track approach to regulation: consumer wellness features operate under less stringent requirements, while medical-grade functionalities undergo full regulatory clearance processes. Google's strategy includes obtaining FDA clearances for specific health monitoring features like the ECG app and Irregular Rhythm Notifications. Their regulatory approach incorporates continuous software validation through a dedicated Quality Management System (QMS) that meets ISO 13485 standards for medical devices. Google has pioneered the use of large-scale virtual clinical trials to validate biosensor accuracy across diverse populations, addressing regulatory concerns about inclusivity in medical device testing[2]. The company maintains a dedicated regulatory affairs team that works directly with global regulatory bodies to shape emerging standards for AI-powered health algorithms in wearables, particularly focusing on how continuous monitoring data should be regulated compared to traditional spot-check measurements.
Strengths: Extensive data science capabilities for biosensor validation; strong relationships with regulatory bodies; ability to conduct large-scale clinical studies. Weaknesses: Balancing consumer technology innovation pace with slower regulatory approval timelines; managing privacy concerns while collecting sufficient data for regulatory submissions.
Critical Regulatory Documents and Guidelines
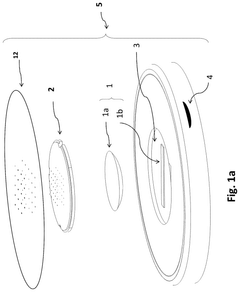
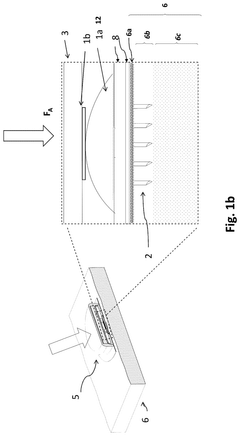
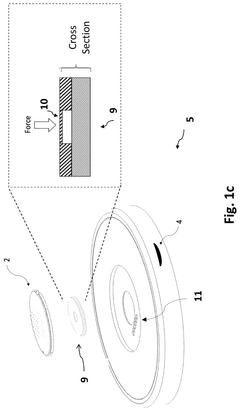
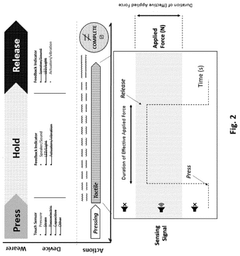
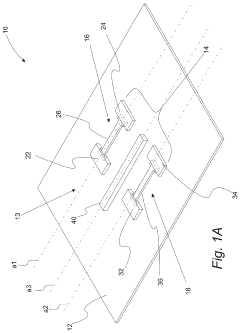
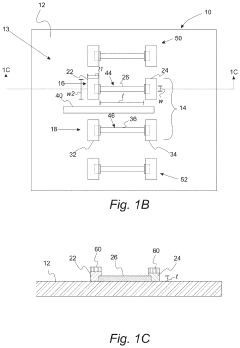
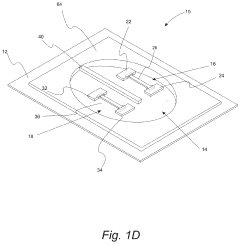
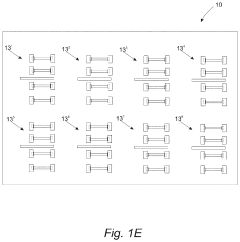
Wearable Biosensor Device With Improved Microneedle Array Placement
PatentPendingUS20250025077A1
Innovation
- A wearable biosensor device system that incorporates a microneedle array with a force touch sensor and feedback indicator, which guides users in applying the correct pressure for proper insertion and provides real-time feedback to ensure continuous accurate placement.
Wearable biosensors and applications thereof
PatentActiveUS20230060118A9
Innovation
- Development of highly sensitive In2O3 nanoribbon transistor biosensors with integrated on-chip gold gate electrodes, functionalized with glucose oxidase, chitosan, and single-walled carbon nanotubes, capable of detecting glucose concentrations between 10 nM to 1 mM in external body fluids without breaking the skin, and integrated into flexible, conformable devices like skin patches and contact lenses.
Cross-Border Regulatory Harmonization Efforts
The global nature of wearable biosensor markets necessitates coordinated regulatory approaches across different jurisdictions. Recent years have witnessed significant efforts toward harmonizing regulatory frameworks for wearable biosensors, with international organizations playing pivotal roles in establishing common standards and protocols.
The International Medical Device Regulators Forum (IMDRF) has emerged as a key facilitator in cross-border harmonization, developing guidance documents specifically addressing software as a medical device (SaMD) that applies to many wearable biosensors. Their risk-based classification system provides a unified approach that regulatory bodies worldwide increasingly reference in their national frameworks.
Between the United States and European Union, the Medical Device Single Audit Program (MDSAP) represents a landmark achievement in regulatory cooperation. This program allows manufacturers to undergo a single audit that satisfies requirements across multiple regulatory jurisdictions, significantly reducing redundant compliance processes for wearable biosensor developers operating internationally.
The Asia-Pacific Economic Cooperation (APEC) Life Sciences Innovation Forum has established working groups focused on regulatory convergence for medical devices, including wearable biosensors. Their Regulatory Harmonization Steering Committee has developed roadmaps for implementation of harmonized approaches across member economies, with particular attention to emerging technologies like biosensors.
Mutual Recognition Agreements (MRAs) between major markets have expanded in scope to include aspects of wearable technology regulation. The EU-US MRA for conformity assessment of medical devices now encompasses certain categories of wearable biosensors, allowing manufacturers to reduce duplicate testing requirements when entering both markets.
The Global Harmonization Working Party (GHWP) has developed specific technical documents addressing the unique challenges of wearable biosensors, including guidance on validation protocols for continuous monitoring devices and standardized approaches to evaluating sensor accuracy across different physiological parameters and user demographics.
Challenges remain in achieving full harmonization, particularly regarding data privacy regulations that vary significantly across regions. The intersection of medical device regulation and data protection laws creates complex compliance landscapes for wearable biosensor manufacturers. Efforts to develop internationally recognized frameworks for health data governance, such as those proposed by the OECD and WHO, represent important steps toward resolving these cross-border regulatory challenges.
Looking forward, regulatory science initiatives focused specifically on wearable biosensors are emerging through international collaborations between academic institutions, industry consortia, and regulatory bodies. These initiatives aim to develop evidence-based approaches to regulation that can be implemented consistently across borders while accommodating the rapid pace of technological innovation in this field.
The International Medical Device Regulators Forum (IMDRF) has emerged as a key facilitator in cross-border harmonization, developing guidance documents specifically addressing software as a medical device (SaMD) that applies to many wearable biosensors. Their risk-based classification system provides a unified approach that regulatory bodies worldwide increasingly reference in their national frameworks.
Between the United States and European Union, the Medical Device Single Audit Program (MDSAP) represents a landmark achievement in regulatory cooperation. This program allows manufacturers to undergo a single audit that satisfies requirements across multiple regulatory jurisdictions, significantly reducing redundant compliance processes for wearable biosensor developers operating internationally.
The Asia-Pacific Economic Cooperation (APEC) Life Sciences Innovation Forum has established working groups focused on regulatory convergence for medical devices, including wearable biosensors. Their Regulatory Harmonization Steering Committee has developed roadmaps for implementation of harmonized approaches across member economies, with particular attention to emerging technologies like biosensors.
Mutual Recognition Agreements (MRAs) between major markets have expanded in scope to include aspects of wearable technology regulation. The EU-US MRA for conformity assessment of medical devices now encompasses certain categories of wearable biosensors, allowing manufacturers to reduce duplicate testing requirements when entering both markets.
The Global Harmonization Working Party (GHWP) has developed specific technical documents addressing the unique challenges of wearable biosensors, including guidance on validation protocols for continuous monitoring devices and standardized approaches to evaluating sensor accuracy across different physiological parameters and user demographics.
Challenges remain in achieving full harmonization, particularly regarding data privacy regulations that vary significantly across regions. The intersection of medical device regulation and data protection laws creates complex compliance landscapes for wearable biosensor manufacturers. Efforts to develop internationally recognized frameworks for health data governance, such as those proposed by the OECD and WHO, represent important steps toward resolving these cross-border regulatory challenges.
Looking forward, regulatory science initiatives focused specifically on wearable biosensors are emerging through international collaborations between academic institutions, industry consortia, and regulatory bodies. These initiatives aim to develop evidence-based approaches to regulation that can be implemented consistently across borders while accommodating the rapid pace of technological innovation in this field.
Data Privacy and Security Compliance Requirements
The regulatory landscape for wearable biosensors has evolved significantly in recent years, with data privacy and security compliance requirements becoming increasingly stringent. The Health Insurance Portability and Accountability Act (HIPAA) in the United States remains a cornerstone regulation, mandating strict protection of personally identifiable health information collected by wearable biosensors. Manufacturers must implement comprehensive security measures including end-to-end encryption, secure authentication protocols, and regular security audits to achieve compliance.
The European Union's General Data Protection Regulation (GDPR) has established even more rigorous standards, requiring explicit user consent for data collection, processing transparency, and the right to data portability and deletion. Wearable biosensor companies operating in the EU market must demonstrate robust data protection impact assessments and implement privacy by design principles throughout product development cycles.
In Asia, regulations vary significantly by country, with Japan's Act on the Protection of Personal Information (APPI) and China's Personal Information Protection Law (PIPL) emerging as influential frameworks. These regulations emphasize localized data storage requirements and restrictions on cross-border data transfers, creating additional compliance challenges for global wearable biosensor manufacturers.
Industry standards organizations have responded with specialized frameworks addressing the unique security challenges of wearable health technologies. The ISO/IEEE 11073 Personal Health Device standards provide technical specifications for secure data exchange, while the NIST Cybersecurity Framework offers risk management guidelines specifically adapted for healthcare IoT devices including wearable biosensors.
Emerging compliance requirements increasingly focus on continuous monitoring capabilities, with regulatory bodies now expecting manufacturers to implement real-time vulnerability detection and automated security patch deployment systems. This shift represents a move from point-in-time compliance to ongoing security assurance throughout the device lifecycle.
Biometric data protection has received particular regulatory attention, with specialized requirements for securing physiological measurements like heart rate, blood oxygen levels, and glucose readings. Regulations increasingly mandate sophisticated anonymization techniques and granular access controls to prevent unauthorized use of sensitive biometric information.
The integration of artificial intelligence in wearable biosensors has introduced additional regulatory considerations regarding algorithmic transparency and data governance. Regulators now require documentation of AI training methodologies and validation processes to ensure that automated health insights derived from biosensor data meet clinical accuracy standards while maintaining privacy safeguards.
The European Union's General Data Protection Regulation (GDPR) has established even more rigorous standards, requiring explicit user consent for data collection, processing transparency, and the right to data portability and deletion. Wearable biosensor companies operating in the EU market must demonstrate robust data protection impact assessments and implement privacy by design principles throughout product development cycles.
In Asia, regulations vary significantly by country, with Japan's Act on the Protection of Personal Information (APPI) and China's Personal Information Protection Law (PIPL) emerging as influential frameworks. These regulations emphasize localized data storage requirements and restrictions on cross-border data transfers, creating additional compliance challenges for global wearable biosensor manufacturers.
Industry standards organizations have responded with specialized frameworks addressing the unique security challenges of wearable health technologies. The ISO/IEEE 11073 Personal Health Device standards provide technical specifications for secure data exchange, while the NIST Cybersecurity Framework offers risk management guidelines specifically adapted for healthcare IoT devices including wearable biosensors.
Emerging compliance requirements increasingly focus on continuous monitoring capabilities, with regulatory bodies now expecting manufacturers to implement real-time vulnerability detection and automated security patch deployment systems. This shift represents a move from point-in-time compliance to ongoing security assurance throughout the device lifecycle.
Biometric data protection has received particular regulatory attention, with specialized requirements for securing physiological measurements like heart rate, blood oxygen levels, and glucose readings. Regulations increasingly mandate sophisticated anonymization techniques and granular access controls to prevent unauthorized use of sensitive biometric information.
The integration of artificial intelligence in wearable biosensors has introduced additional regulatory considerations regarding algorithmic transparency and data governance. Regulators now require documentation of AI training methodologies and validation processes to ensure that automated health insights derived from biosensor data meet clinical accuracy standards while maintaining privacy safeguards.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!