Studying endothelial dysfunction in atherosclerosis using LDL-loaded vascular chips
SEP 2, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Atherosclerosis Endothelial Dysfunction Background and Objectives
Atherosclerosis is a chronic inflammatory disease characterized by the accumulation of lipids, particularly low-density lipoprotein (LDL), in the arterial wall. This progressive condition remains a leading cause of cardiovascular morbidity and mortality worldwide, accounting for approximately 31% of global deaths annually. The pathogenesis of atherosclerosis involves a complex interplay between lipid metabolism, inflammation, and vascular biology, with endothelial dysfunction recognized as a critical initiating event.
Endothelial cells form the innermost layer of blood vessels and serve as a dynamic interface between circulating blood and vascular tissues. Under normal physiological conditions, these cells maintain vascular homeostasis through the regulation of vascular tone, permeability, and inflammatory responses. However, exposure to cardiovascular risk factors such as hyperlipidemia, hypertension, and smoking disrupts this balance, leading to endothelial dysfunction.
The historical understanding of atherosclerosis has evolved significantly over the past century. Initially viewed as a passive lipid storage disease in the 1950s, subsequent research revealed its inflammatory nature and the central role of endothelial dysfunction in disease initiation and progression. The "response to injury" hypothesis proposed by Ross and Glomset in the 1970s highlighted endothelial damage as the triggering event in atherogenesis, a concept that continues to inform current research directions.
Recent technological advances have enabled more sophisticated approaches to studying endothelial dysfunction. Traditional in vitro models using static cell cultures fail to recapitulate the complex hemodynamic forces and cell-cell interactions present in vivo. Animal models, while valuable, present limitations in translating findings to human pathophysiology due to species-specific differences in lipoprotein metabolism and vascular biology.
The emergence of organ-on-chip technology represents a paradigm shift in atherosclerosis research. These microfluidic devices can simulate the vascular microenvironment, incorporating controlled fluid dynamics, multiple cell types, and physiologically relevant biochemical cues. LDL-loaded vascular chips specifically aim to model the early stages of atherosclerosis by exposing endothelial cells to pathological levels of LDL under controlled conditions.
The primary objectives of studying endothelial dysfunction using LDL-loaded vascular chips are multifaceted. First, to elucidate the molecular mechanisms underlying endothelial activation and dysfunction in response to LDL exposure. Second, to identify potential biomarkers for early detection of atherosclerosis before clinical manifestations. Third, to establish a reliable platform for screening novel therapeutic compounds targeting endothelial dysfunction. Finally, to develop personalized medicine approaches by incorporating patient-derived cells into the chip system, enabling individualized risk assessment and treatment strategies.
This research direction aligns with the broader goal of reducing the global burden of cardiovascular disease through improved understanding of pathophysiology, earlier intervention, and more effective therapeutic strategies targeting the earliest stages of atherosclerosis.
Endothelial cells form the innermost layer of blood vessels and serve as a dynamic interface between circulating blood and vascular tissues. Under normal physiological conditions, these cells maintain vascular homeostasis through the regulation of vascular tone, permeability, and inflammatory responses. However, exposure to cardiovascular risk factors such as hyperlipidemia, hypertension, and smoking disrupts this balance, leading to endothelial dysfunction.
The historical understanding of atherosclerosis has evolved significantly over the past century. Initially viewed as a passive lipid storage disease in the 1950s, subsequent research revealed its inflammatory nature and the central role of endothelial dysfunction in disease initiation and progression. The "response to injury" hypothesis proposed by Ross and Glomset in the 1970s highlighted endothelial damage as the triggering event in atherogenesis, a concept that continues to inform current research directions.
Recent technological advances have enabled more sophisticated approaches to studying endothelial dysfunction. Traditional in vitro models using static cell cultures fail to recapitulate the complex hemodynamic forces and cell-cell interactions present in vivo. Animal models, while valuable, present limitations in translating findings to human pathophysiology due to species-specific differences in lipoprotein metabolism and vascular biology.
The emergence of organ-on-chip technology represents a paradigm shift in atherosclerosis research. These microfluidic devices can simulate the vascular microenvironment, incorporating controlled fluid dynamics, multiple cell types, and physiologically relevant biochemical cues. LDL-loaded vascular chips specifically aim to model the early stages of atherosclerosis by exposing endothelial cells to pathological levels of LDL under controlled conditions.
The primary objectives of studying endothelial dysfunction using LDL-loaded vascular chips are multifaceted. First, to elucidate the molecular mechanisms underlying endothelial activation and dysfunction in response to LDL exposure. Second, to identify potential biomarkers for early detection of atherosclerosis before clinical manifestations. Third, to establish a reliable platform for screening novel therapeutic compounds targeting endothelial dysfunction. Finally, to develop personalized medicine approaches by incorporating patient-derived cells into the chip system, enabling individualized risk assessment and treatment strategies.
This research direction aligns with the broader goal of reducing the global burden of cardiovascular disease through improved understanding of pathophysiology, earlier intervention, and more effective therapeutic strategies targeting the earliest stages of atherosclerosis.
Market Analysis for Vascular-on-Chip Technologies
The vascular-on-chip technology market is experiencing significant growth, driven by increasing prevalence of cardiovascular diseases and the need for more effective drug development platforms. The global market for organ-on-chip technologies was valued at approximately $21 million in 2019 and is projected to reach $220 million by 2025, with a compound annual growth rate of 39.9%. Within this broader market, vascular chips represent a crucial segment due to the high mortality rates associated with cardiovascular diseases worldwide.
Atherosclerosis research using vascular chip models presents a particularly promising market opportunity. With cardiovascular diseases accounting for nearly 18 million deaths annually according to the World Health Organization, pharmaceutical companies are actively seeking improved preclinical models that better predict human responses to potential therapies.
The primary market segments for LDL-loaded vascular chips include pharmaceutical research and development, academic research institutions, and contract research organizations. Pharmaceutical companies represent the largest market share, allocating substantial budgets to cardiovascular drug development programs. These companies are increasingly adopting organ-on-chip technologies to reduce the high failure rates of cardiovascular drugs in clinical trials, which currently exceed 90%.
Geographic distribution of the market shows North America leading with approximately 45% market share, followed by Europe at 30% and Asia-Pacific at 20%. The remaining 5% is distributed across other regions. The United States dominates the North American market due to substantial research funding and the presence of major pharmaceutical companies and technology developers.
Key market drivers include increasing R&D investments in cardiovascular disease treatments, growing recognition of the limitations of animal models, and regulatory pressure to reduce animal testing. The FDA's Modernization Act 2.0, which encourages alternative testing methods, has further accelerated market growth for these technologies.
Market restraints include the high cost of vascular chip systems, technical challenges in achieving physiologically relevant models, and the need for standardization across platforms. The average cost per vascular chip system ranges from $50,000 to $150,000, limiting adoption by smaller research institutions.
Customer demand is increasingly focused on chips that can accurately model specific disease states, particularly endothelial dysfunction in atherosclerosis. End-users are seeking systems that integrate multiple tissue types, allow for long-term culture, and provide real-time monitoring capabilities. The ability to incorporate patient-specific cells for personalized medicine applications represents an emerging market requirement with significant growth potential.
Atherosclerosis research using vascular chip models presents a particularly promising market opportunity. With cardiovascular diseases accounting for nearly 18 million deaths annually according to the World Health Organization, pharmaceutical companies are actively seeking improved preclinical models that better predict human responses to potential therapies.
The primary market segments for LDL-loaded vascular chips include pharmaceutical research and development, academic research institutions, and contract research organizations. Pharmaceutical companies represent the largest market share, allocating substantial budgets to cardiovascular drug development programs. These companies are increasingly adopting organ-on-chip technologies to reduce the high failure rates of cardiovascular drugs in clinical trials, which currently exceed 90%.
Geographic distribution of the market shows North America leading with approximately 45% market share, followed by Europe at 30% and Asia-Pacific at 20%. The remaining 5% is distributed across other regions. The United States dominates the North American market due to substantial research funding and the presence of major pharmaceutical companies and technology developers.
Key market drivers include increasing R&D investments in cardiovascular disease treatments, growing recognition of the limitations of animal models, and regulatory pressure to reduce animal testing. The FDA's Modernization Act 2.0, which encourages alternative testing methods, has further accelerated market growth for these technologies.
Market restraints include the high cost of vascular chip systems, technical challenges in achieving physiologically relevant models, and the need for standardization across platforms. The average cost per vascular chip system ranges from $50,000 to $150,000, limiting adoption by smaller research institutions.
Customer demand is increasingly focused on chips that can accurately model specific disease states, particularly endothelial dysfunction in atherosclerosis. End-users are seeking systems that integrate multiple tissue types, allow for long-term culture, and provide real-time monitoring capabilities. The ability to incorporate patient-specific cells for personalized medicine applications represents an emerging market requirement with significant growth potential.
Current Challenges in Atherosclerosis Modeling
Despite significant advancements in atherosclerosis research, current modeling approaches face substantial limitations in replicating the complex pathophysiology of this disease. Traditional in vitro models often fail to capture the dynamic interplay between endothelial cells, blood flow, and lipoproteins that characterizes atherosclerotic progression. Animal models, while valuable, present translational challenges due to species-specific differences in lipoprotein metabolism and vascular biology.
A critical challenge in atherosclerosis modeling is accurately simulating the hemodynamic forces that influence endothelial dysfunction. Conventional static cell culture systems cannot replicate the shear stress patterns found at arterial bifurcations and curvatures—regions particularly susceptible to atherosclerotic plaque formation. This limitation significantly hampers our understanding of how biomechanical forces contribute to endothelial activation and subsequent inflammatory responses.
The temporal aspect of atherosclerosis progression presents another major hurdle. The disease develops over decades in humans, making it difficult to model the slow progression from initial endothelial dysfunction to advanced plaque formation. Current accelerated models often sacrifice physiological relevance for experimental expediency, creating a significant gap between laboratory findings and clinical reality.
Reproducing the complex cellular interactions within the vascular microenvironment remains challenging. Atherosclerosis involves multiple cell types beyond endothelial cells, including smooth muscle cells, macrophages, and platelets. Existing models struggle to incorporate these diverse cellular components while maintaining their natural spatial organization and communication networks.
The biochemical complexity of lipoprotein modification represents another significant modeling challenge. The oxidative modification of LDL particles is a key event in atherosclerosis initiation, yet replicating the precise conditions under which this occurs in vivo has proven difficult. Most models rely on artificially oxidized LDL, which may not accurately reflect the gradual modifications that occur within the arterial wall.
Patient-specific modeling presents additional complications. Individual variations in genetic predisposition, lipoprotein profiles, and inflammatory responses significantly influence atherosclerosis progression. Current standardized models cannot adequately account for this heterogeneity, limiting their predictive value for personalized medicine applications.
Technical limitations in imaging and quantification methods further complicate atherosclerosis research. Real-time visualization of endothelial dysfunction and early plaque formation remains challenging, particularly at the microscopic level where critical cellular events occur. This creates significant barriers to understanding the initial stages of disease progression.
A critical challenge in atherosclerosis modeling is accurately simulating the hemodynamic forces that influence endothelial dysfunction. Conventional static cell culture systems cannot replicate the shear stress patterns found at arterial bifurcations and curvatures—regions particularly susceptible to atherosclerotic plaque formation. This limitation significantly hampers our understanding of how biomechanical forces contribute to endothelial activation and subsequent inflammatory responses.
The temporal aspect of atherosclerosis progression presents another major hurdle. The disease develops over decades in humans, making it difficult to model the slow progression from initial endothelial dysfunction to advanced plaque formation. Current accelerated models often sacrifice physiological relevance for experimental expediency, creating a significant gap between laboratory findings and clinical reality.
Reproducing the complex cellular interactions within the vascular microenvironment remains challenging. Atherosclerosis involves multiple cell types beyond endothelial cells, including smooth muscle cells, macrophages, and platelets. Existing models struggle to incorporate these diverse cellular components while maintaining their natural spatial organization and communication networks.
The biochemical complexity of lipoprotein modification represents another significant modeling challenge. The oxidative modification of LDL particles is a key event in atherosclerosis initiation, yet replicating the precise conditions under which this occurs in vivo has proven difficult. Most models rely on artificially oxidized LDL, which may not accurately reflect the gradual modifications that occur within the arterial wall.
Patient-specific modeling presents additional complications. Individual variations in genetic predisposition, lipoprotein profiles, and inflammatory responses significantly influence atherosclerosis progression. Current standardized models cannot adequately account for this heterogeneity, limiting their predictive value for personalized medicine applications.
Technical limitations in imaging and quantification methods further complicate atherosclerosis research. Real-time visualization of endothelial dysfunction and early plaque formation remains challenging, particularly at the microscopic level where critical cellular events occur. This creates significant barriers to understanding the initial stages of disease progression.
LDL-Loading Methodologies for Vascular Chips
01 Microfluidic vascular chip models for endothelial dysfunction studies
Microfluidic devices designed to mimic vascular structures can be used to study endothelial dysfunction. These chips incorporate channels lined with endothelial cells that can be exposed to LDL to simulate pathological conditions. The controlled environment allows for precise monitoring of endothelial responses to LDL loading, including changes in permeability, inflammation markers, and cellular morphology. These models provide valuable insights into the mechanisms of endothelial dysfunction in cardiovascular diseases.- Microfluidic vascular chip models for endothelial dysfunction studies: Microfluidic vascular chips are designed to mimic blood vessels and can be used to study endothelial dysfunction. These chips contain channels lined with endothelial cells that can be exposed to LDL to simulate vascular conditions. The chips allow for real-time monitoring of endothelial cell responses to LDL loading, including changes in permeability, inflammation markers, and cellular morphology. These models provide a controlled environment for studying the mechanisms of endothelial dysfunction in atherosclerosis.
- LDL modification and oxidation effects on endothelial function: Modified and oxidized forms of LDL play a crucial role in endothelial dysfunction. When LDL becomes oxidized, it triggers inflammatory responses in endothelial cells, leading to increased expression of adhesion molecules, reduced nitric oxide production, and impaired vasodilation. Studies using vascular chip models have demonstrated that different modifications of LDL particles can induce varying degrees of endothelial dysfunction, providing insights into the progression of atherosclerosis and potential therapeutic targets.
- Biomarkers for LDL-induced endothelial dysfunction: Various biomarkers can be used to assess LDL-induced endothelial dysfunction in vascular chip models. These include inflammatory cytokines, adhesion molecules, reactive oxygen species, and endothelial nitric oxide synthase activity. By measuring these biomarkers in response to LDL loading, researchers can evaluate the severity of endothelial dysfunction and test the efficacy of potential therapeutic interventions. The identification of specific biomarkers helps in understanding the molecular mechanisms underlying endothelial dysfunction.
- Therapeutic approaches targeting LDL-induced endothelial dysfunction: Various therapeutic approaches have been developed to target LDL-induced endothelial dysfunction. These include antioxidants that prevent LDL oxidation, compounds that enhance nitric oxide production, anti-inflammatory agents, and lipid-lowering drugs. Vascular chip models loaded with LDL provide an effective platform for screening and evaluating these therapeutic agents. The efficacy of these interventions can be assessed by measuring improvements in endothelial function markers after treatment.
- Advanced imaging and analysis techniques for vascular chips: Advanced imaging and analysis techniques are essential for studying LDL-induced endothelial dysfunction in vascular chips. These include confocal microscopy, fluorescence imaging, and computational fluid dynamics. These techniques allow for the visualization of endothelial cell morphology, quantification of LDL uptake, and assessment of flow patterns within the chips. By combining these imaging methods with molecular analysis, researchers can gain comprehensive insights into the mechanisms of endothelial dysfunction and potential therapeutic interventions.
02 LDL modification techniques for vascular dysfunction research
Various methods for modifying LDL particles are employed to enhance their atherogenic properties for research purposes. These include oxidation, acetylation, and glycation of LDL, which can then be introduced to vascular chip models. Modified LDL particles demonstrate increased uptake by endothelial cells and greater potential to induce dysfunction. These techniques allow researchers to study specific pathways involved in endothelial damage and potential therapeutic interventions.Expand Specific Solutions03 Biomarkers for assessing LDL-induced endothelial dysfunction
Several biomarkers can be used to evaluate endothelial dysfunction in LDL-loaded vascular chips. These include adhesion molecules (VCAM-1, ICAM-1), inflammatory cytokines (IL-6, TNF-α), nitric oxide production, reactive oxygen species, and endothelial permeability markers. Measurement of these biomarkers in chip-based models provides quantitative assessment of endothelial health and dysfunction progression when exposed to varying concentrations of LDL under different conditions.Expand Specific Solutions04 Therapeutic compounds for preventing LDL-induced endothelial damage
Various compounds have been tested in vascular chip models to prevent or reverse LDL-induced endothelial dysfunction. These include antioxidants, anti-inflammatory agents, statins, and natural compounds with vasoprotective properties. The chip-based platforms allow for high-throughput screening of potential therapeutic agents and assessment of their efficacy in maintaining endothelial integrity under LDL challenge conditions.Expand Specific Solutions05 Advanced imaging techniques for visualizing endothelial-LDL interactions
Sophisticated imaging methods are employed to visualize and quantify the interactions between LDL particles and endothelial cells in vascular chips. These include confocal microscopy, fluorescence imaging, and label-free techniques that can track LDL uptake, endothelial barrier function, and cellular responses in real-time. These imaging approaches provide detailed insights into the temporal and spatial aspects of endothelial dysfunction development following LDL exposure.Expand Specific Solutions
Key Industry and Academic Players in Vascular Modeling
The atherosclerosis vascular chip market is in an early growth phase, characterized by increasing research adoption but limited commercial applications. The global market for organ-on-chip technologies is projected to reach $220 million by 2025, with vascular models representing approximately 15%. Academic institutions like The Regents of the University of California, Emory University, and Yale University are leading fundamental research, while biopharmaceutical companies including Vascular Biogenics, Reata Pharmaceuticals, and CSL Behring are advancing clinical applications. The technology remains in early-to-mid maturity, with research institutions developing proof-of-concept models while companies like Ionis Pharmaceuticals and Resverlogix focus on translating these platforms for drug discovery applications targeting endothelial dysfunction in atherosclerosis.
The Regents of the University of California
Technical Solution: The University of California has developed advanced microfluidic vascular chip platforms that recreate the human vascular microenvironment for studying atherosclerosis progression. Their technology incorporates endothelial cells cultured under physiologically relevant flow conditions with controlled LDL exposure. These organ-on-chip systems feature multiple chambers that allow simultaneous testing of different conditions, including varying LDL concentrations and flow rates. The platform enables real-time imaging of endothelial dysfunction markers, including adhesion molecule expression, permeability changes, and inflammatory responses. Their approach integrates computational fluid dynamics modeling to ensure physiologically accurate shear stress conditions, critical for maintaining endothelial cell phenotype and function.
Strengths: Exceptional interdisciplinary research combining microfluidics, vascular biology, and computational modeling; extensive validation against human tissue samples. Weaknesses: Complex fabrication process may limit widespread adoption; higher cost compared to traditional cell culture models; requires specialized expertise for operation and data interpretation.
Emory University
Technical Solution: Emory University has pioneered a vascular chip technology specifically designed for atherosclerosis research that incorporates a three-dimensional architecture mimicking arterial bifurcations—regions prone to atherosclerotic plaque formation. Their system features a gradient generator that creates controlled LDL concentration profiles across the chip, enabling studies of dose-dependent endothelial responses. The platform incorporates oxygen sensing capabilities to monitor real-time metabolic changes in endothelial cells exposed to oxidized LDL. Emory's technology also allows co-culture of endothelial cells with smooth muscle cells and macrophages to study cell-cell interactions during atherosclerosis progression. Their system has been validated using patient-derived cells to model genetic predispositions to atherosclerosis.
Strengths: Sophisticated modeling of arterial geometry including bifurcations where atherosclerosis preferentially develops; integrated sensors for real-time monitoring. Weaknesses: Limited throughput compared to some competing platforms; relatively new technology with fewer published validation studies; higher technical complexity requiring specialized training.
Critical Innovations in Endothelial Dysfunction Assessment
Nitric oxide donating derivatives for the treatment of cardiovascular disorders
PatentWO2005032559A8
Innovation
- Development of novel compounds that simultaneously donate nitric oxide and release anti-oxidant molecules, inducing ApoAl expression to increase HDL levels, lower LDL and triglycerides, while inhibiting HMG-CoA reductase and ACAT, thereby addressing hyperlipidemia and endothelial dysfunction.
Receptor for modified low-density lipoprotein
PatentInactiveEP1717314A1
Innovation
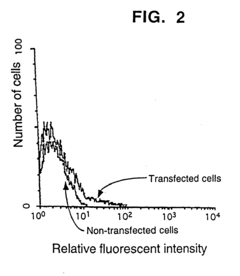
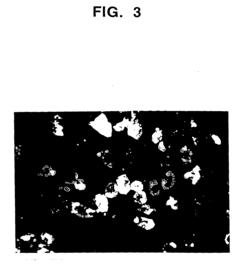
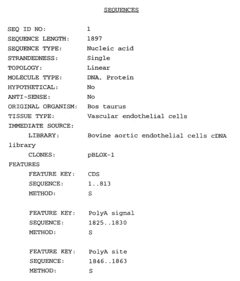
- The DNA sequence encoding the mammalian vascular endothelial receptor for modified LDL is identified, allowing for the production of a biologically active receptor and its use in assays and antibody preparation for diagnosing atherosclerosis.
Translational Potential for Drug Discovery
The vascular chip technology for studying endothelial dysfunction in atherosclerosis presents significant translational potential for drug discovery. This platform offers a physiologically relevant microenvironment that closely mimics human vascular conditions, providing a more accurate prediction of drug efficacy and toxicity compared to traditional cell culture or animal models.
The technology bridges the critical gap between preclinical testing and clinical trials by enabling high-throughput screening of potential therapeutic compounds targeting endothelial dysfunction. Pharmaceutical companies can utilize these chips to evaluate drug candidates' effects on LDL-induced endothelial damage, inflammatory responses, and plaque formation in a controlled environment that replicates human pathophysiology.
A major advantage of this platform is its ability to incorporate patient-specific cells, allowing for personalized medicine approaches. By using endothelial cells derived from patients with different genetic backgrounds or risk factors, researchers can identify which therapeutic compounds might be most effective for specific patient populations, potentially reducing clinical trial failures and accelerating drug development timelines.
The technology also enables mechanistic studies of drug action at the cellular and molecular levels. Researchers can observe in real-time how compounds affect endothelial barrier function, inflammatory signaling pathways, and interactions between endothelial cells and circulating immune cells or lipoproteins, providing valuable insights for drug optimization.
Cost reduction represents another significant translational benefit. By identifying ineffective or potentially toxic compounds earlier in the development pipeline, pharmaceutical companies can avoid investing in candidates unlikely to succeed in clinical trials. Industry estimates suggest that eliminating a single failed drug candidate before clinical testing can save tens of millions of dollars.
Regulatory agencies have shown increasing interest in organ-on-chip technologies as complementary or alternative methods to animal testing. The vascular chip model could potentially satisfy regulatory requirements while reducing animal use, aligning with global efforts toward more ethical and human-relevant testing paradigms.
Furthermore, the platform's versatility allows for integration with other organ chips to create multi-organ systems, enabling assessment of drug effects on vascular health in the context of liver metabolism or kidney clearance, providing a more comprehensive understanding of drug safety and efficacy profiles before human testing.
The technology bridges the critical gap between preclinical testing and clinical trials by enabling high-throughput screening of potential therapeutic compounds targeting endothelial dysfunction. Pharmaceutical companies can utilize these chips to evaluate drug candidates' effects on LDL-induced endothelial damage, inflammatory responses, and plaque formation in a controlled environment that replicates human pathophysiology.
A major advantage of this platform is its ability to incorporate patient-specific cells, allowing for personalized medicine approaches. By using endothelial cells derived from patients with different genetic backgrounds or risk factors, researchers can identify which therapeutic compounds might be most effective for specific patient populations, potentially reducing clinical trial failures and accelerating drug development timelines.
The technology also enables mechanistic studies of drug action at the cellular and molecular levels. Researchers can observe in real-time how compounds affect endothelial barrier function, inflammatory signaling pathways, and interactions between endothelial cells and circulating immune cells or lipoproteins, providing valuable insights for drug optimization.
Cost reduction represents another significant translational benefit. By identifying ineffective or potentially toxic compounds earlier in the development pipeline, pharmaceutical companies can avoid investing in candidates unlikely to succeed in clinical trials. Industry estimates suggest that eliminating a single failed drug candidate before clinical testing can save tens of millions of dollars.
Regulatory agencies have shown increasing interest in organ-on-chip technologies as complementary or alternative methods to animal testing. The vascular chip model could potentially satisfy regulatory requirements while reducing animal use, aligning with global efforts toward more ethical and human-relevant testing paradigms.
Furthermore, the platform's versatility allows for integration with other organ chips to create multi-organ systems, enabling assessment of drug effects on vascular health in the context of liver metabolism or kidney clearance, providing a more comprehensive understanding of drug safety and efficacy profiles before human testing.
Regulatory Considerations for Organ-on-Chip Validation
The regulatory landscape for organ-on-chip (OOC) technologies, particularly vascular chips used for studying endothelial dysfunction in atherosclerosis, presents significant challenges for researchers and developers. These microphysiological systems occupy a unique position between traditional in vitro models and animal testing, necessitating careful consideration of validation requirements to ensure their acceptance by regulatory bodies.
The FDA and EMA have begun developing frameworks for qualifying OOC technologies as drug development tools, though specific guidelines for vascular chips loaded with LDL to study atherosclerosis remain limited. Current regulatory approaches typically require demonstration of physiological relevance, reproducibility, and predictive capacity compared to established models.
For LDL-loaded vascular chips, validation must address multiple dimensions: biological fidelity (accurate representation of endothelial dysfunction mechanisms), technical reproducibility (consistent chip manufacturing and operation), and clinical correlation (relationship between chip responses and human pathophysiology).
Standardization represents a critical regulatory hurdle. Researchers must establish standard operating procedures for chip fabrication, cell sourcing and characterization, LDL preparation, flow conditions, and analytical endpoints. The International Council for Harmonisation of Technical Requirements (ICH) guidelines provide useful reference points, particularly regarding quality control and validation methodologies.
Data quality and integrity considerations are paramount for regulatory acceptance. Comprehensive documentation of experimental design, execution, and analysis is essential, with particular attention to statistical power calculations and minimizing batch effects between chip preparations.
Qualification pathways for these technologies typically involve staged validation: first establishing technical performance characteristics, then demonstrating biological relevance through comparison with established atherosclerosis models, and finally correlating with clinical outcomes. The FDA's Biomarker Qualification Program offers a potential framework for this process.
Ethical and privacy considerations also factor into regulatory requirements, particularly regarding human cell sourcing and data management. Informed consent procedures for donor cells and compliance with data protection regulations must be addressed in validation protocols.
Looking forward, collaborative efforts between academic researchers, industry partners, and regulatory agencies will be crucial for developing consensus standards specifically tailored to vascular chip technologies. Participation in pre-submission meetings with regulatory bodies can provide valuable guidance on validation requirements for specific research applications.
The FDA and EMA have begun developing frameworks for qualifying OOC technologies as drug development tools, though specific guidelines for vascular chips loaded with LDL to study atherosclerosis remain limited. Current regulatory approaches typically require demonstration of physiological relevance, reproducibility, and predictive capacity compared to established models.
For LDL-loaded vascular chips, validation must address multiple dimensions: biological fidelity (accurate representation of endothelial dysfunction mechanisms), technical reproducibility (consistent chip manufacturing and operation), and clinical correlation (relationship between chip responses and human pathophysiology).
Standardization represents a critical regulatory hurdle. Researchers must establish standard operating procedures for chip fabrication, cell sourcing and characterization, LDL preparation, flow conditions, and analytical endpoints. The International Council for Harmonisation of Technical Requirements (ICH) guidelines provide useful reference points, particularly regarding quality control and validation methodologies.
Data quality and integrity considerations are paramount for regulatory acceptance. Comprehensive documentation of experimental design, execution, and analysis is essential, with particular attention to statistical power calculations and minimizing batch effects between chip preparations.
Qualification pathways for these technologies typically involve staged validation: first establishing technical performance characteristics, then demonstrating biological relevance through comparison with established atherosclerosis models, and finally correlating with clinical outcomes. The FDA's Biomarker Qualification Program offers a potential framework for this process.
Ethical and privacy considerations also factor into regulatory requirements, particularly regarding human cell sourcing and data management. Informed consent procedures for donor cells and compliance with data protection regulations must be addressed in validation protocols.
Looking forward, collaborative efforts between academic researchers, industry partners, and regulatory agencies will be crucial for developing consensus standards specifically tailored to vascular chip technologies. Participation in pre-submission meetings with regulatory bodies can provide valuable guidance on validation requirements for specific research applications.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!