Current Advances in Gene Therapy for Cystic Fibrosis
SEP 19, 202510 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Gene Therapy Evolution and Objectives for Cystic Fibrosis
Gene therapy for cystic fibrosis (CF) has evolved significantly since the identification of the CFTR gene in 1989, which encodes the cystic fibrosis transmembrane conductance regulator protein. This discovery marked the beginning of a new era in CF treatment, offering the potential to address the root cause rather than merely managing symptoms. Early gene therapy approaches in the 1990s utilized viral vectors such as adenoviruses and adeno-associated viruses (AAVs) to deliver functional CFTR genes to airway epithelial cells, though these initial attempts faced significant challenges related to immune responses and transduction efficiency.
The evolution of gene therapy for CF has been characterized by three distinct phases. The first phase (1990-2000) focused on proof-of-concept studies and first-generation viral vectors. The second phase (2000-2010) saw the development of improved viral vectors with reduced immunogenicity and enhanced gene transfer capabilities, alongside the exploration of non-viral delivery methods such as lipid nanoparticles. The current phase (2010-present) has witnessed revolutionary advances with the emergence of CRISPR-Cas9 gene editing technology, offering unprecedented precision in correcting specific CFTR mutations.
Recent technological breakthroughs have significantly enhanced the potential of gene therapy for CF. The development of lentiviral vectors has improved gene transfer efficiency and duration of expression. Additionally, advances in mRNA delivery systems have opened new avenues for transient CFTR expression without genomic integration risks. The refinement of lipid nanoparticle formulations has also improved the delivery of genetic material to target tissues while minimizing immune responses.
The primary objectives of current gene therapy approaches for CF include achieving long-term expression of functional CFTR protein, developing delivery systems capable of penetrating the thick mucus barrier characteristic of CF airways, and ensuring the safety of genetic interventions by minimizing off-target effects and immunogenicity. Researchers aim to develop treatments that can be administered non-invasively, ideally through inhalation, to maximize patient compliance and quality of life.
Another critical objective is the development of personalized gene therapy approaches that address specific CFTR mutations, as over 2,000 different mutations have been identified. This personalization is essential given the heterogeneity of CF manifestations across patients with different genetic profiles. The ultimate goal remains the development of a one-time curative treatment that permanently corrects the genetic defect underlying CF, eliminating the need for lifelong symptom management.
The technological trajectory suggests that combining multiple approaches—such as CRISPR-based gene editing for permanent correction alongside mRNA-based therapies for immediate relief—may offer the most comprehensive treatment strategy. As these technologies continue to mature, the prospect of effectively treating or even curing cystic fibrosis through gene therapy becomes increasingly realistic, potentially transforming the lives of approximately 70,000 people worldwide affected by this debilitating condition.
The evolution of gene therapy for CF has been characterized by three distinct phases. The first phase (1990-2000) focused on proof-of-concept studies and first-generation viral vectors. The second phase (2000-2010) saw the development of improved viral vectors with reduced immunogenicity and enhanced gene transfer capabilities, alongside the exploration of non-viral delivery methods such as lipid nanoparticles. The current phase (2010-present) has witnessed revolutionary advances with the emergence of CRISPR-Cas9 gene editing technology, offering unprecedented precision in correcting specific CFTR mutations.
Recent technological breakthroughs have significantly enhanced the potential of gene therapy for CF. The development of lentiviral vectors has improved gene transfer efficiency and duration of expression. Additionally, advances in mRNA delivery systems have opened new avenues for transient CFTR expression without genomic integration risks. The refinement of lipid nanoparticle formulations has also improved the delivery of genetic material to target tissues while minimizing immune responses.
The primary objectives of current gene therapy approaches for CF include achieving long-term expression of functional CFTR protein, developing delivery systems capable of penetrating the thick mucus barrier characteristic of CF airways, and ensuring the safety of genetic interventions by minimizing off-target effects and immunogenicity. Researchers aim to develop treatments that can be administered non-invasively, ideally through inhalation, to maximize patient compliance and quality of life.
Another critical objective is the development of personalized gene therapy approaches that address specific CFTR mutations, as over 2,000 different mutations have been identified. This personalization is essential given the heterogeneity of CF manifestations across patients with different genetic profiles. The ultimate goal remains the development of a one-time curative treatment that permanently corrects the genetic defect underlying CF, eliminating the need for lifelong symptom management.
The technological trajectory suggests that combining multiple approaches—such as CRISPR-based gene editing for permanent correction alongside mRNA-based therapies for immediate relief—may offer the most comprehensive treatment strategy. As these technologies continue to mature, the prospect of effectively treating or even curing cystic fibrosis through gene therapy becomes increasingly realistic, potentially transforming the lives of approximately 70,000 people worldwide affected by this debilitating condition.
Market Analysis of CF Gene Therapy Demand
The global market for Cystic Fibrosis (CF) gene therapy has shown significant growth potential, driven by the increasing prevalence of CF and the limitations of current treatment options. With approximately 70,000-100,000 people worldwide affected by CF, the demand for curative therapies rather than symptom management continues to rise. Market research indicates that the CF therapeutics market is expected to reach $13.9 billion by 2025, with gene therapy representing a rapidly growing segment.
Patient advocacy has emerged as a powerful market driver, with organizations like the Cystic Fibrosis Foundation investing over $3 billion in research and development efforts. These investments have accelerated clinical trials and created a more favorable regulatory environment for gene therapy approaches. The foundation's venture philanthropy model has been particularly effective in bridging the gap between academic research and commercial development.
Healthcare systems worldwide are increasingly recognizing the economic burden of CF management, estimated at $15,000-150,000 per patient annually depending on disease severity. This economic pressure creates market pull for potentially curative gene therapies, despite their high initial costs. Payers are showing greater willingness to consider value-based payment models for gene therapies that could reduce long-term healthcare expenditures.
Regional market analysis reveals varying levels of demand and access. North America dominates the market with approximately 45% share, followed by Europe at 35%. The Asia-Pacific region represents the fastest-growing market segment with annual growth rates exceeding 12%, primarily due to improving diagnosis rates and healthcare infrastructure. However, access disparities remain significant, with high-income countries having substantially better access to advanced therapies.
Competitive landscape assessment shows increasing interest from both established pharmaceutical companies and biotech startups. Over 25 companies are actively developing CF gene therapy candidates, with 15 programs in clinical trials. This represents a 300% increase in development programs compared to five years ago, indicating strong market confidence in the technology's potential.
Market segmentation analysis reveals distinct patient populations with varying needs. Pediatric patients represent a critical market segment, as early intervention with gene therapy could prevent irreversible lung damage. Adult patients with advanced disease constitute another key segment seeking therapies that can halt disease progression. The heterogeneity of CF-causing mutations creates additional market niches for mutation-specific approaches.
Reimbursement challenges remain a significant market barrier, with concerns about the sustainability of high one-time costs for gene therapies. However, innovative payment models including outcomes-based agreements and annuity payments are emerging to address these concerns, potentially expanding market access.
Patient advocacy has emerged as a powerful market driver, with organizations like the Cystic Fibrosis Foundation investing over $3 billion in research and development efforts. These investments have accelerated clinical trials and created a more favorable regulatory environment for gene therapy approaches. The foundation's venture philanthropy model has been particularly effective in bridging the gap between academic research and commercial development.
Healthcare systems worldwide are increasingly recognizing the economic burden of CF management, estimated at $15,000-150,000 per patient annually depending on disease severity. This economic pressure creates market pull for potentially curative gene therapies, despite their high initial costs. Payers are showing greater willingness to consider value-based payment models for gene therapies that could reduce long-term healthcare expenditures.
Regional market analysis reveals varying levels of demand and access. North America dominates the market with approximately 45% share, followed by Europe at 35%. The Asia-Pacific region represents the fastest-growing market segment with annual growth rates exceeding 12%, primarily due to improving diagnosis rates and healthcare infrastructure. However, access disparities remain significant, with high-income countries having substantially better access to advanced therapies.
Competitive landscape assessment shows increasing interest from both established pharmaceutical companies and biotech startups. Over 25 companies are actively developing CF gene therapy candidates, with 15 programs in clinical trials. This represents a 300% increase in development programs compared to five years ago, indicating strong market confidence in the technology's potential.
Market segmentation analysis reveals distinct patient populations with varying needs. Pediatric patients represent a critical market segment, as early intervention with gene therapy could prevent irreversible lung damage. Adult patients with advanced disease constitute another key segment seeking therapies that can halt disease progression. The heterogeneity of CF-causing mutations creates additional market niches for mutation-specific approaches.
Reimbursement challenges remain a significant market barrier, with concerns about the sustainability of high one-time costs for gene therapies. However, innovative payment models including outcomes-based agreements and annuity payments are emerging to address these concerns, potentially expanding market access.
Current Landscape and Challenges in CF Gene Therapy
Gene therapy for Cystic Fibrosis (CF) has evolved significantly over the past three decades, yet remains at a critical juncture between promising laboratory results and clinical implementation. Currently, the global landscape shows varied approaches being pursued across research institutions and biotechnology companies, with notable advancements in viral vector design, non-viral delivery systems, and gene editing technologies specifically tailored for CF treatment.
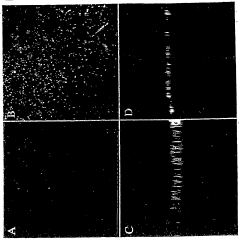
The primary challenge in CF gene therapy continues to be efficient delivery of the functional CFTR gene to airway epithelial cells. The lungs present formidable barriers including mucus obstruction, inflammatory environment, and immune responses that significantly reduce transfection efficiency. Vector systems must navigate these obstacles while maintaining sufficient payload capacity for the relatively large CFTR gene.
Adeno-associated virus (AAV) vectors have emerged as leading candidates due to their safety profile and tropism for airway cells, though their limited packaging capacity necessitates innovative approaches for CFTR delivery. Lentiviral vectors offer larger capacity but face concerns regarding integration safety and production scalability. Non-viral approaches using lipid nanoparticles show promise for repeated administration but currently demonstrate lower transfection efficiency.
Geographically, CF gene therapy research exhibits concentration in North America and Europe, with the UK CF Gene Therapy Consortium, US-based academic centers, and specialized biotechnology companies leading development efforts. Emerging research hubs in Australia and Asia are increasingly contributing to the field, though with varying regulatory frameworks that impact clinical translation timelines.
Durability of gene expression represents another significant hurdle, as current approaches typically achieve transient expression requiring repeated administration. This challenge is compounded by pre-existing and treatment-induced immune responses that can neutralize vectors upon subsequent dosing, particularly with viral delivery systems.
The heterogeneity of CF mutations presents an additional layer of complexity, with over 2,000 identified CFTR mutations requiring potentially different therapeutic approaches. While gene replacement strategies aim to address all mutations, gene editing approaches must be tailored to specific mutation classes, creating challenges for comprehensive treatment development.
Manufacturing scalability and cost considerations further constrain clinical implementation, with current production methods for clinical-grade vectors being resource-intensive and expensive. This economic barrier significantly impacts the potential accessibility of these therapies, particularly in healthcare systems with limited resources.
Recent clinical trials have demonstrated safety but modest efficacy, highlighting the gap between theoretical potential and practical application. The field now stands at a critical inflection point where technological innovations in delivery systems, gene editing precision, and manufacturing processes will determine the trajectory toward viable therapeutic options for CF patients.
The primary challenge in CF gene therapy continues to be efficient delivery of the functional CFTR gene to airway epithelial cells. The lungs present formidable barriers including mucus obstruction, inflammatory environment, and immune responses that significantly reduce transfection efficiency. Vector systems must navigate these obstacles while maintaining sufficient payload capacity for the relatively large CFTR gene.
Adeno-associated virus (AAV) vectors have emerged as leading candidates due to their safety profile and tropism for airway cells, though their limited packaging capacity necessitates innovative approaches for CFTR delivery. Lentiviral vectors offer larger capacity but face concerns regarding integration safety and production scalability. Non-viral approaches using lipid nanoparticles show promise for repeated administration but currently demonstrate lower transfection efficiency.
Geographically, CF gene therapy research exhibits concentration in North America and Europe, with the UK CF Gene Therapy Consortium, US-based academic centers, and specialized biotechnology companies leading development efforts. Emerging research hubs in Australia and Asia are increasingly contributing to the field, though with varying regulatory frameworks that impact clinical translation timelines.
Durability of gene expression represents another significant hurdle, as current approaches typically achieve transient expression requiring repeated administration. This challenge is compounded by pre-existing and treatment-induced immune responses that can neutralize vectors upon subsequent dosing, particularly with viral delivery systems.
The heterogeneity of CF mutations presents an additional layer of complexity, with over 2,000 identified CFTR mutations requiring potentially different therapeutic approaches. While gene replacement strategies aim to address all mutations, gene editing approaches must be tailored to specific mutation classes, creating challenges for comprehensive treatment development.
Manufacturing scalability and cost considerations further constrain clinical implementation, with current production methods for clinical-grade vectors being resource-intensive and expensive. This economic barrier significantly impacts the potential accessibility of these therapies, particularly in healthcare systems with limited resources.
Recent clinical trials have demonstrated safety but modest efficacy, highlighting the gap between theoretical potential and practical application. The field now stands at a critical inflection point where technological innovations in delivery systems, gene editing precision, and manufacturing processes will determine the trajectory toward viable therapeutic options for CF patients.
Current Delivery Systems for CFTR Gene Transfer
01 Viral vector-based gene therapy efficacy
Viral vectors are widely used in gene therapy to deliver therapeutic genes to target cells. The efficacy of viral vector-based gene therapies depends on factors such as vector design, transduction efficiency, and immune responses. Various viral vectors including adeno-associated virus (AAV), lentivirus, and adenovirus are employed for different therapeutic applications, with each offering distinct advantages in terms of tissue tropism, payload capacity, and safety profile.- Viral vector-based gene therapy efficacy: Viral vectors are widely used in gene therapy to deliver therapeutic genes to target cells. The efficacy of viral vector-based gene therapies depends on factors such as vector design, transduction efficiency, and immune responses. Adeno-associated virus (AAV) and lentiviral vectors are commonly used due to their ability to provide long-term gene expression. Methods to enhance viral vector efficacy include optimizing vector design, improving targeting specificity, and minimizing immune responses against the vector.
- Monitoring and assessment of gene therapy efficacy: Various methods and technologies are used to monitor and assess the efficacy of gene therapy treatments. These include biomarker analysis, imaging techniques, genetic testing, and functional assessments. Real-time monitoring systems can track gene expression levels and therapeutic outcomes over time. Advanced diagnostic tools help in evaluating treatment response, optimizing dosing regimens, and identifying potential adverse effects, ultimately improving the overall efficacy of gene therapy approaches.
- Cell-based gene therapy approaches: Cell-based gene therapy involves genetically modifying cells ex vivo before reintroducing them into patients. This approach includes CAR-T cell therapy for cancer treatment and stem cell-based gene therapies for various genetic disorders. The efficacy of these therapies depends on cell viability, engraftment, persistence, and functional gene expression. Strategies to enhance efficacy include optimizing cell culture conditions, improving genetic modification techniques, and developing methods to enhance cell survival and function after transplantation.
- Gene editing technologies for therapeutic applications: Gene editing technologies such as CRISPR-Cas9, zinc finger nucleases, and TALENs are being used to correct genetic mutations directly. The efficacy of these approaches depends on editing efficiency, specificity, and delivery methods. Factors affecting treatment efficacy include off-target effects, immune responses to editing components, and the persistence of edited cells. Advances in delivery systems and editing precision continue to improve the therapeutic potential of gene editing technologies.
- Enhancing gene therapy delivery and expression: Various strategies are employed to enhance gene therapy delivery and expression, directly impacting treatment efficacy. These include the development of novel delivery systems such as nanoparticles, liposomes, and exosomes; optimization of gene expression cassettes with tissue-specific promoters; and use of immune modulation to prevent clearance of gene therapy vectors. Controlled release systems and targeted delivery approaches help improve the biodistribution of therapeutic genes, increasing efficacy while reducing off-target effects.
02 Assessment methods for gene therapy efficacy
Various methods and technologies are used to evaluate the efficacy of gene therapy treatments. These include biomarker analysis, imaging techniques, functional assays, and genetic sequencing to monitor gene expression and therapeutic outcomes. Advanced diagnostic tools enable researchers and clinicians to assess treatment response, optimize dosing regimens, and predict long-term efficacy of gene therapy interventions.Expand Specific Solutions03 Gene delivery systems and enhancement strategies
Innovative delivery systems and enhancement strategies are crucial for improving gene therapy efficacy. These include non-viral delivery methods such as lipid nanoparticles, polymeric carriers, and physical methods like electroporation. Additionally, strategies to enhance gene expression, improve cellular uptake, and overcome biological barriers are employed to maximize therapeutic outcomes while minimizing off-target effects.Expand Specific Solutions04 Gene editing technologies for therapeutic applications
Gene editing technologies such as CRISPR-Cas9, zinc finger nucleases, and TALENs are revolutionizing gene therapy by enabling precise modification of genetic material. These technologies allow for correction of disease-causing mutations, gene knockout, or insertion of therapeutic genes. The efficacy of gene editing approaches depends on factors such as editing precision, off-target effects, and delivery efficiency to target tissues.Expand Specific Solutions05 Clinical outcomes and patient-specific factors
The efficacy of gene therapy treatments varies based on clinical outcomes and patient-specific factors. These include disease stage, genetic background, immune status, and age of the patient. Personalized approaches that consider these factors can optimize treatment efficacy. Long-term follow-up studies are essential to evaluate durability of therapeutic effects and identify potential delayed adverse events that may impact overall treatment success.Expand Specific Solutions
Leading Organizations in CF Gene Therapy Research
Gene therapy for Cystic Fibrosis is currently in the early commercialization phase, with a growing market projected to reach $2.5 billion by 2027. The technology is advancing from preclinical to clinical stages, with varying degrees of maturity across approaches. Vertex Pharmaceuticals leads the field with approved CFTR modulators, while emerging players like Spirovant Sciences and SpliSense are developing novel gene therapy solutions. Academic institutions including Yale University, Johns Hopkins, and UNC Chapel Hill contribute significant research advancements. The competitive landscape features pharmaceutical giants (AbbVie, Boehringer Ingelheim) alongside specialized biotechs (Editas Medicine, Galapagos) pursuing different technological approaches, indicating a diversifying but still maturing therapeutic area.
Vertex Pharmaceuticals, Inc.
Technical Solution: Vertex Pharmaceuticals has pioneered a dual approach to cystic fibrosis (CF) treatment combining small molecule CFTR modulators with gene therapy. Their mRNA-based therapy VX-522 delivers functional copies of the CFTR gene to airway cells using lipid nanoparticles (LNPs). This approach bypasses the need for viral vectors, potentially reducing immunogenicity concerns. In 2023, Vertex initiated Phase 1 clinical trials for VX-522 in collaboration with Moderna, representing the first inhaled mRNA therapy for CF. Their technology enables repeated dosing, addressing the transient expression limitation of traditional gene therapies. Vertex's platform builds upon their expertise in CF biology and complements their existing portfolio of CFTR modulators like Trikafta, potentially offering solutions for the 10% of CF patients with nonsense or other mutations not addressable by current modulators.
Strengths: Established expertise in CF therapeutics; complementary approach to existing treatments; non-viral delivery system allowing repeat dosing; advanced clinical stage development. Weaknesses: Challenges in achieving sufficient lung tissue penetration; potential for mRNA instability; competition from other emerging gene therapy approaches; uncertainty about long-term efficacy of mRNA delivery.
SpliSense Ltd.
Technical Solution: SpliSense has developed an innovative antisense oligonucleotide (ASO) platform specifically targeting splicing mutations in the CFTR gene that cause cystic fibrosis. Their lead candidate, SPL84-23, addresses the 3849+10kb C>T mutation by correcting aberrant splicing, enabling the production of functional CFTR protein. The therapy utilizes proprietary chemistry modifications to enhance stability and cellular uptake when delivered via inhalation. SpliSense's technology employs a unique sequence design algorithm that identifies optimal binding sites to maximize splicing correction efficiency while minimizing off-target effects. In preclinical studies, their ASOs demonstrated restoration of CFTR function in patient-derived cell models and showed promising distribution throughout lung tissue in animal models. The company received FDA Orphan Drug Designation for SPL84-23 and is advancing toward clinical trials. Their platform has potential applications beyond the initial target mutation, with development programs for additional CFTR splicing mutations that collectively affect approximately 10-15% of CF patients worldwide.
Strengths: Mutation-specific approach with high precision; delivery via simple inhalation; potential for repeated administration; less complex manufacturing compared to viral vectors. Weaknesses: Limited to specific mutation types (primarily splicing mutations); potential need for frequent redosing; challenges in achieving sufficient tissue concentration; competition from broader-spectrum approaches.
Breakthrough Technologies in CF Gene Editing
Conductance of improperly folded proteins through the secretory pathway and related methods for treating disease
PatentWO2005086954A2
Innovation
- Inhibiting the ER-chaperon retention machinery, specifically UGGT and other elements, to allow mis-folded proteins like ΔF508 CFTR and α-antitrypsin to exit the ER and reach the plasma membrane, where they can function despite mutations, using agents like thapsigargin, curcuminoids, and siRNA to reduce UGGT activity and deplete ER Ca++ stores.
Safety and Efficacy Considerations in CF Gene Therapy
Safety considerations in gene therapy for cystic fibrosis (CF) remain paramount as clinical applications advance. Vector-related immune responses pose significant challenges, with both viral and non-viral vectors potentially triggering inflammatory reactions that can compromise therapeutic efficacy and patient safety. Recent studies have demonstrated that adeno-associated virus (AAV) vectors show reduced immunogenicity compared to earlier adenoviral vectors, though pre-existing immunity to AAV serotypes remains problematic in approximately 30-50% of the population.
Off-target effects represent another critical safety concern, as unintended genetic modifications could lead to insertional mutagenesis or disruption of essential cellular functions. Modern CRISPR-Cas9 approaches for CF gene therapy have shown improved targeting precision, with recent studies reporting off-target rates below 1% when using optimized guide RNAs. However, long-term surveillance remains essential as even rare off-target events could potentially lead to oncogenic transformations.
Dosing considerations present a delicate balance between achieving therapeutic efficacy and minimizing toxicity. Clinical trials have demonstrated that repeated administrations may be necessary to maintain therapeutic gene expression levels, yet this increases the risk of immune sensitization. Recent phase II trials have explored immunomodulatory co-treatments to mitigate these effects, showing promising results in extending the therapeutic window for repeated administrations.
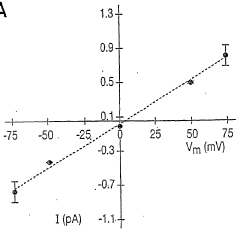
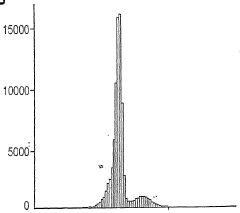
Regarding efficacy, gene therapy approaches for CF must demonstrate meaningful clinical improvements beyond laboratory markers. Current benchmarks include sustained increases in CFTR function (measured by sweat chloride concentration and nasal potential difference), improved lung function parameters (FEV1), reduced pulmonary exacerbations, and enhanced quality of life metrics. The 2021 phase IIb trial using lipid nanoparticle-delivered CFTR mRNA showed encouraging results with mean FEV1 improvements of 6.2% in treated patients versus placebo controls.
Durability of therapeutic effect remains challenging, with most current approaches showing declining efficacy over 3-6 months. This necessitates repeated administrations, which compounds safety concerns. Emerging strategies utilizing genome editing technologies aim to achieve permanent correction of CFTR mutations, potentially offering lifelong therapeutic benefits from a single treatment, though these approaches remain in preclinical development.
Regulatory frameworks for CF gene therapies continue to evolve, with the FDA and EMA implementing specialized pathways for advanced therapy medicinal products. These frameworks emphasize rigorous pre-clinical safety testing, phased clinical trials with extended follow-up periods, and comprehensive post-marketing surveillance to monitor for delayed adverse effects that may not be apparent during initial clinical testing.
Off-target effects represent another critical safety concern, as unintended genetic modifications could lead to insertional mutagenesis or disruption of essential cellular functions. Modern CRISPR-Cas9 approaches for CF gene therapy have shown improved targeting precision, with recent studies reporting off-target rates below 1% when using optimized guide RNAs. However, long-term surveillance remains essential as even rare off-target events could potentially lead to oncogenic transformations.
Dosing considerations present a delicate balance between achieving therapeutic efficacy and minimizing toxicity. Clinical trials have demonstrated that repeated administrations may be necessary to maintain therapeutic gene expression levels, yet this increases the risk of immune sensitization. Recent phase II trials have explored immunomodulatory co-treatments to mitigate these effects, showing promising results in extending the therapeutic window for repeated administrations.
Regarding efficacy, gene therapy approaches for CF must demonstrate meaningful clinical improvements beyond laboratory markers. Current benchmarks include sustained increases in CFTR function (measured by sweat chloride concentration and nasal potential difference), improved lung function parameters (FEV1), reduced pulmonary exacerbations, and enhanced quality of life metrics. The 2021 phase IIb trial using lipid nanoparticle-delivered CFTR mRNA showed encouraging results with mean FEV1 improvements of 6.2% in treated patients versus placebo controls.
Durability of therapeutic effect remains challenging, with most current approaches showing declining efficacy over 3-6 months. This necessitates repeated administrations, which compounds safety concerns. Emerging strategies utilizing genome editing technologies aim to achieve permanent correction of CFTR mutations, potentially offering lifelong therapeutic benefits from a single treatment, though these approaches remain in preclinical development.
Regulatory frameworks for CF gene therapies continue to evolve, with the FDA and EMA implementing specialized pathways for advanced therapy medicinal products. These frameworks emphasize rigorous pre-clinical safety testing, phased clinical trials with extended follow-up periods, and comprehensive post-marketing surveillance to monitor for delayed adverse effects that may not be apparent during initial clinical testing.
Patient Access and Reimbursement Strategies
Patient access to gene therapy for cystic fibrosis represents a significant challenge due to the high costs associated with these innovative treatments. Current gene therapy approaches under development may cost between $1-3 million per patient, creating substantial barriers for healthcare systems worldwide. This economic reality necessitates the development of comprehensive reimbursement strategies to ensure equitable access while maintaining healthcare system sustainability.
Insurance providers and national health systems are exploring various payment models to accommodate gene therapies. Value-based agreements, where payment is linked to treatment outcomes, have emerged as a promising approach. Under these arrangements, manufacturers receive full reimbursement only if predetermined clinical benchmarks are achieved, thereby sharing financial risk between payers and developers. For cystic fibrosis gene therapies, such benchmarks might include sustained improvement in lung function or reduction in pulmonary exacerbations.
Annuity payment models represent another innovative approach, allowing healthcare systems to spread costs over multiple years rather than bearing the entire financial burden upfront. This aligns payment timelines with the long-term benefits expected from gene therapies and helps mitigate immediate budget impacts. Several European countries and select U.S. insurance providers have begun implementing such models for other gene therapies, establishing precedents that could benefit cystic fibrosis treatments.
Patient assistance programs sponsored by pharmaceutical companies play a crucial role in expanding access. These programs typically provide financial support for out-of-pocket expenses, navigational assistance through complex insurance processes, and in some cases, complete coverage for uninsured or underinsured patients. As gene therapies for cystic fibrosis advance toward commercialization, developers are establishing foundations and partnerships with patient advocacy organizations to ensure broader accessibility.
International access presents additional complexities, particularly in low and middle-income countries. Global health initiatives and cross-border collaborations are exploring tiered pricing strategies, technology transfer agreements, and capacity-building programs to extend the reach of gene therapies beyond wealthy nations. The World Health Organization has established working groups focused specifically on ensuring equitable access to advanced therapies for genetic disorders.
Early engagement with health technology assessment bodies has become essential for developers of cystic fibrosis gene therapies. By initiating discussions about value demonstration, outcome measurements, and pricing considerations during clinical development phases, companies can better align their evidence generation strategies with payer requirements, potentially accelerating post-approval reimbursement decisions and patient access.
Insurance providers and national health systems are exploring various payment models to accommodate gene therapies. Value-based agreements, where payment is linked to treatment outcomes, have emerged as a promising approach. Under these arrangements, manufacturers receive full reimbursement only if predetermined clinical benchmarks are achieved, thereby sharing financial risk between payers and developers. For cystic fibrosis gene therapies, such benchmarks might include sustained improvement in lung function or reduction in pulmonary exacerbations.
Annuity payment models represent another innovative approach, allowing healthcare systems to spread costs over multiple years rather than bearing the entire financial burden upfront. This aligns payment timelines with the long-term benefits expected from gene therapies and helps mitigate immediate budget impacts. Several European countries and select U.S. insurance providers have begun implementing such models for other gene therapies, establishing precedents that could benefit cystic fibrosis treatments.
Patient assistance programs sponsored by pharmaceutical companies play a crucial role in expanding access. These programs typically provide financial support for out-of-pocket expenses, navigational assistance through complex insurance processes, and in some cases, complete coverage for uninsured or underinsured patients. As gene therapies for cystic fibrosis advance toward commercialization, developers are establishing foundations and partnerships with patient advocacy organizations to ensure broader accessibility.
International access presents additional complexities, particularly in low and middle-income countries. Global health initiatives and cross-border collaborations are exploring tiered pricing strategies, technology transfer agreements, and capacity-building programs to extend the reach of gene therapies beyond wealthy nations. The World Health Organization has established working groups focused specifically on ensuring equitable access to advanced therapies for genetic disorders.
Early engagement with health technology assessment bodies has become essential for developers of cystic fibrosis gene therapies. By initiating discussions about value demonstration, outcome measurements, and pricing considerations during clinical development phases, companies can better align their evidence generation strategies with payer requirements, potentially accelerating post-approval reimbursement decisions and patient access.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!