Mechanisms of Viral Entry and Integration in Gene Therapy Constructs
SEP 19, 20259 MIN READ
Generate Your Research Report Instantly with AI Agent
Patsnap Eureka helps you evaluate technical feasibility & market potential.
Viral Vector Technology Evolution and Objectives
Viral vector technology has evolved significantly since its inception in the early 1970s when researchers first discovered the potential of using viruses as delivery vehicles for genetic material. The initial breakthrough came with the development of retroviral vectors, which demonstrated the ability to integrate genetic material into host cell genomes. This pioneering work laid the foundation for subsequent advancements in viral vector technology for gene therapy applications.
Throughout the 1980s and 1990s, researchers expanded the viral vector toolkit to include adenoviruses, adeno-associated viruses (AAVs), and lentiviruses, each offering distinct advantages for specific therapeutic applications. The evolution of these vectors has been driven by the need to address key challenges such as immunogenicity, payload capacity, tissue tropism, and integration specificity.
A significant paradigm shift occurred in the early 2000s with the development of self-inactivating vectors and the incorporation of tissue-specific promoters, enhancing both the safety and specificity of gene delivery. These innovations addressed critical concerns regarding insertional mutagenesis and off-target effects that had previously limited clinical applications.
Recent technological breakthroughs have focused on engineering viral capsids and envelope proteins to improve cellular entry mechanisms and target specific tissues. The development of hybrid vectors combining elements from different viral types represents another frontier in vector evolution, aiming to harness the advantageous properties of multiple viral systems while minimizing their limitations.
The primary objectives of current viral vector research for gene therapy constructs center on enhancing transduction efficiency, reducing immunogenicity, increasing payload capacity, and improving manufacturing scalability. Particular emphasis is placed on understanding and optimizing the mechanisms of viral entry and integration to ensure precise delivery of therapeutic genes to target cells while minimizing off-target effects.
Another critical objective involves developing vectors capable of crossing biological barriers, particularly the blood-brain barrier, to enable effective treatment of neurological disorders. Additionally, researchers are working to create vectors with controllable expression systems that allow for temporal regulation of therapeutic gene expression.
The field is now moving toward rational design approaches that leverage structural biology insights and computational modeling to engineer viral vectors with predetermined properties. This represents a shift from earlier trial-and-error methodologies to more predictive and systematic development strategies. The ultimate goal remains the creation of viral vectors that combine optimal safety profiles with maximal therapeutic efficacy across diverse clinical applications.
Throughout the 1980s and 1990s, researchers expanded the viral vector toolkit to include adenoviruses, adeno-associated viruses (AAVs), and lentiviruses, each offering distinct advantages for specific therapeutic applications. The evolution of these vectors has been driven by the need to address key challenges such as immunogenicity, payload capacity, tissue tropism, and integration specificity.
A significant paradigm shift occurred in the early 2000s with the development of self-inactivating vectors and the incorporation of tissue-specific promoters, enhancing both the safety and specificity of gene delivery. These innovations addressed critical concerns regarding insertional mutagenesis and off-target effects that had previously limited clinical applications.
Recent technological breakthroughs have focused on engineering viral capsids and envelope proteins to improve cellular entry mechanisms and target specific tissues. The development of hybrid vectors combining elements from different viral types represents another frontier in vector evolution, aiming to harness the advantageous properties of multiple viral systems while minimizing their limitations.
The primary objectives of current viral vector research for gene therapy constructs center on enhancing transduction efficiency, reducing immunogenicity, increasing payload capacity, and improving manufacturing scalability. Particular emphasis is placed on understanding and optimizing the mechanisms of viral entry and integration to ensure precise delivery of therapeutic genes to target cells while minimizing off-target effects.
Another critical objective involves developing vectors capable of crossing biological barriers, particularly the blood-brain barrier, to enable effective treatment of neurological disorders. Additionally, researchers are working to create vectors with controllable expression systems that allow for temporal regulation of therapeutic gene expression.
The field is now moving toward rational design approaches that leverage structural biology insights and computational modeling to engineer viral vectors with predetermined properties. This represents a shift from earlier trial-and-error methodologies to more predictive and systematic development strategies. The ultimate goal remains the creation of viral vectors that combine optimal safety profiles with maximal therapeutic efficacy across diverse clinical applications.
Gene Therapy Market Landscape Analysis
The gene therapy market has experienced remarkable growth over the past decade, evolving from a niche experimental field to a commercially viable therapeutic approach. Currently valued at approximately $7.6 billion in 2023, the market is projected to reach $25 billion by 2030, representing a compound annual growth rate (CAGR) of 18.3%. This exponential growth is primarily driven by increasing prevalence of genetic disorders, advancements in viral vector technologies, and substantial investments from pharmaceutical companies and venture capital firms.
North America dominates the global gene therapy market, accounting for roughly 48% of the market share, followed by Europe at 28% and Asia-Pacific at 18%. The United States leads in terms of clinical trials and commercial approvals, with the FDA having approved several gene therapy products including Luxturna, Zolgensma, and Hemgenix, which command premium prices ranging from $425,000 to $3.5 million per treatment.
The competitive landscape is characterized by a mix of established pharmaceutical giants and specialized biotech companies. Key players include Novartis, Pfizer, Roche, Spark Therapeutics (acquired by Roche), BioMarin, bluebird bio, and UniQure. These companies are actively developing viral vector-based gene therapies, with particular focus on adeno-associated virus (AAV) and lentiviral vectors due to their favorable safety profiles and efficient gene delivery capabilities.
Regarding viral entry and integration mechanisms, the market shows clear preferences. AAV vectors dominate approximately 60% of clinical trials due to their non-integrating nature and reduced risk of insertional mutagenesis. Lentiviral vectors account for about 25% of trials, primarily in ex vivo applications for hematopoietic stem cell modification. Retroviral vectors, despite integration concerns, still maintain about 10% market share in specific applications.
Significant market barriers include manufacturing challenges, with viral vector production capacity constraints limiting scalability. The high cost of gene therapies presents reimbursement challenges, with payers increasingly demanding outcomes-based pricing models. Regulatory frameworks continue to evolve, creating uncertainty but also opportunities for companies with regulatory expertise.
Emerging trends include the development of non-viral delivery systems, gene editing technologies like CRISPR-Cas9, and in vivo gene therapy approaches that eliminate the need for ex vivo cell manipulation. These innovations are expected to expand the addressable market by enabling treatment of a broader range of diseases and potentially reducing manufacturing costs.
North America dominates the global gene therapy market, accounting for roughly 48% of the market share, followed by Europe at 28% and Asia-Pacific at 18%. The United States leads in terms of clinical trials and commercial approvals, with the FDA having approved several gene therapy products including Luxturna, Zolgensma, and Hemgenix, which command premium prices ranging from $425,000 to $3.5 million per treatment.
The competitive landscape is characterized by a mix of established pharmaceutical giants and specialized biotech companies. Key players include Novartis, Pfizer, Roche, Spark Therapeutics (acquired by Roche), BioMarin, bluebird bio, and UniQure. These companies are actively developing viral vector-based gene therapies, with particular focus on adeno-associated virus (AAV) and lentiviral vectors due to their favorable safety profiles and efficient gene delivery capabilities.
Regarding viral entry and integration mechanisms, the market shows clear preferences. AAV vectors dominate approximately 60% of clinical trials due to their non-integrating nature and reduced risk of insertional mutagenesis. Lentiviral vectors account for about 25% of trials, primarily in ex vivo applications for hematopoietic stem cell modification. Retroviral vectors, despite integration concerns, still maintain about 10% market share in specific applications.
Significant market barriers include manufacturing challenges, with viral vector production capacity constraints limiting scalability. The high cost of gene therapies presents reimbursement challenges, with payers increasingly demanding outcomes-based pricing models. Regulatory frameworks continue to evolve, creating uncertainty but also opportunities for companies with regulatory expertise.
Emerging trends include the development of non-viral delivery systems, gene editing technologies like CRISPR-Cas9, and in vivo gene therapy approaches that eliminate the need for ex vivo cell manipulation. These innovations are expected to expand the addressable market by enabling treatment of a broader range of diseases and potentially reducing manufacturing costs.
Current Viral Entry Mechanisms and Barriers
Viral vectors remain the predominant delivery vehicles for gene therapy, with each vector type exhibiting unique cellular entry mechanisms and facing distinct barriers. Adeno-associated viruses (AAVs) primarily enter cells through receptor-mediated endocytosis, utilizing primary receptors such as heparan sulfate proteoglycans and co-receptors including fibroblast growth factor receptor or αVβ5 integrin. Following endocytosis, AAVs must escape endosomal compartments, traffic to the nucleus, uncoat, and convert their single-stranded DNA genome to double-stranded DNA for transgene expression.
Lentiviral vectors, derived from HIV-1, engage with specific cell surface receptors like CD4 and chemokine receptors CCR5 or CXCR4. Their entry process involves membrane fusion facilitated by the viral envelope glycoprotein, followed by reverse transcription of the RNA genome into DNA in the cytoplasm. The pre-integration complex must then navigate the cytoskeletal network and enter the nucleus through nuclear pores, where integration into the host genome occurs.
Adenoviral vectors demonstrate high transduction efficiency across various cell types by binding to the coxsackievirus and adenovirus receptor (CAR) through fiber proteins, with subsequent internalization mediated by penton base interactions with cellular integrins. Once internalized, adenoviruses disrupt endosomes, traffic to the nuclear pore complex, and deliver their DNA payload into the nucleus without integration.
Significant barriers impede efficient viral vector transduction. The innate immune system presents a formidable obstacle, with pattern recognition receptors detecting viral components and triggering inflammatory responses. Pre-existing neutralizing antibodies from previous viral exposures can rapidly clear administered vectors before they reach target tissues. Physical barriers such as the blood-brain barrier, extracellular matrix, and mucosal surfaces restrict vector access to intended cell populations.
Intracellular barriers further complicate vector delivery. Endosomal entrapment and subsequent lysosomal degradation significantly reduce transduction efficiency. Nuclear entry represents a major bottleneck, particularly for non-dividing cells where the nuclear membrane remains intact. Additionally, epigenetic silencing mechanisms can suppress transgene expression even after successful delivery.
Recent advances have focused on engineering viral capsids and envelopes to overcome these barriers. Directed evolution and rational design approaches have yielded vectors with enhanced tissue tropism, reduced immunogenicity, and improved intracellular trafficking. Peptide insertions that facilitate endosomal escape or nuclear localization have shown promise in enhancing transduction efficiency. Despite these innovations, the complexity of viral-host interactions continues to present challenges for achieving optimal gene delivery in therapeutic applications.
Lentiviral vectors, derived from HIV-1, engage with specific cell surface receptors like CD4 and chemokine receptors CCR5 or CXCR4. Their entry process involves membrane fusion facilitated by the viral envelope glycoprotein, followed by reverse transcription of the RNA genome into DNA in the cytoplasm. The pre-integration complex must then navigate the cytoskeletal network and enter the nucleus through nuclear pores, where integration into the host genome occurs.
Adenoviral vectors demonstrate high transduction efficiency across various cell types by binding to the coxsackievirus and adenovirus receptor (CAR) through fiber proteins, with subsequent internalization mediated by penton base interactions with cellular integrins. Once internalized, adenoviruses disrupt endosomes, traffic to the nuclear pore complex, and deliver their DNA payload into the nucleus without integration.
Significant barriers impede efficient viral vector transduction. The innate immune system presents a formidable obstacle, with pattern recognition receptors detecting viral components and triggering inflammatory responses. Pre-existing neutralizing antibodies from previous viral exposures can rapidly clear administered vectors before they reach target tissues. Physical barriers such as the blood-brain barrier, extracellular matrix, and mucosal surfaces restrict vector access to intended cell populations.
Intracellular barriers further complicate vector delivery. Endosomal entrapment and subsequent lysosomal degradation significantly reduce transduction efficiency. Nuclear entry represents a major bottleneck, particularly for non-dividing cells where the nuclear membrane remains intact. Additionally, epigenetic silencing mechanisms can suppress transgene expression even after successful delivery.
Recent advances have focused on engineering viral capsids and envelopes to overcome these barriers. Directed evolution and rational design approaches have yielded vectors with enhanced tissue tropism, reduced immunogenicity, and improved intracellular trafficking. Peptide insertions that facilitate endosomal escape or nuclear localization have shown promise in enhancing transduction efficiency. Despite these innovations, the complexity of viral-host interactions continues to present challenges for achieving optimal gene delivery in therapeutic applications.
Contemporary Viral Vector Design Strategies
01 Viral vector design and optimization for gene therapy
Viral vectors are engineered to efficiently deliver therapeutic genes to target cells while minimizing immunogenicity and toxicity. Design considerations include capsid modifications, promoter selection, and payload capacity optimization. Advanced vector engineering techniques aim to improve transduction efficiency, target specificity, and expression durability for various therapeutic applications.- Viral vector design for efficient cell entry: Viral vectors are engineered to optimize cell entry mechanisms for gene therapy applications. These designs focus on modifying viral envelope proteins or capsids to enhance binding to specific cell surface receptors, improving tropism for target tissues. Advanced vector designs incorporate elements that facilitate endosomal escape and cytoplasmic trafficking to increase transduction efficiency. These modifications can significantly improve the delivery of therapeutic genes to specific cell types while reducing off-target effects.
- Integration mechanisms of viral vectors in host genome: Different viral vectors employ distinct mechanisms for integrating genetic material into host cells. Retroviral and lentiviral vectors integrate their genetic payload into the host genome through viral integrase enzymes, enabling long-term gene expression. Non-integrating vectors like adeno-associated virus (AAV) primarily exist as episomal DNA in the nucleus. Understanding these integration patterns is crucial for predicting long-term expression stability and assessing potential genotoxicity risks associated with insertional mutagenesis.
- Safety enhancements for viral vector integration: Safety improvements in viral vector technology focus on controlling integration site selection to minimize insertional mutagenesis risks. Strategies include using self-inactivating vectors with deleted promoter elements, site-specific integration systems, and integration-deficient vectors. Novel approaches incorporate insulator elements to prevent activation of neighboring genes and employ tissue-specific promoters to restrict transgene expression to target cells. These advancements significantly improve the safety profile of integrating viral vectors for clinical applications.
- Novel viral entry pathways and cellular receptors: Research on viral entry mechanisms has identified specific cellular receptors and entry pathways that can be exploited for gene therapy. Understanding the interaction between viral surface proteins and cellular receptors enables the development of vectors with enhanced tissue specificity. Engineered viral vectors can utilize alternative entry pathways to overcome barriers in difficult-to-transduce cell types. These discoveries facilitate the creation of vectors with improved transduction efficiency and reduced immunogenicity for various therapeutic applications.
- Methods for monitoring viral vector integration: Advanced techniques have been developed to track and analyze viral vector integration sites in host genomes. These methods include next-generation sequencing approaches, PCR-based integration site analysis, and bioinformatic tools for mapping integration events. Real-time monitoring systems can assess integration patterns during preclinical and clinical studies, providing crucial safety data. These analytical tools help evaluate genotoxicity risks, optimize vector design, and ensure the long-term safety of gene therapy treatments.
02 Mechanisms of viral entry into host cells
Viral vectors utilize specific cellular receptors and entry pathways to gain access to target cells. This process involves receptor binding, membrane fusion or endocytosis, and trafficking through cellular compartments. Understanding these mechanisms allows for the development of vectors with enhanced cell-type specificity and improved transduction efficiency in gene therapy applications.Expand Specific Solutions03 Genomic integration strategies and safety considerations
Integration of viral vector genetic material into the host genome can provide long-term therapeutic gene expression but raises safety concerns regarding insertional mutagenesis. Various approaches are employed to control integration site selection, develop non-integrating vectors, or create site-specific integration systems to enhance safety while maintaining therapeutic efficacy.Expand Specific Solutions04 Novel viral vector delivery systems
Innovative delivery systems for viral vectors enhance their therapeutic potential by improving targeting, reducing immunogenicity, and increasing stability. These systems include hybrid vectors, pseudotyped vectors, and vectors combined with nanoparticles or biomaterials. Such approaches aim to overcome biological barriers and improve the pharmacokinetics of gene therapy vectors.Expand Specific Solutions05 Analytical methods for characterizing viral vector entry and integration
Advanced analytical techniques are essential for characterizing viral vector behavior, including entry mechanisms and integration patterns. These methods include high-throughput sequencing, single-cell analysis, molecular imaging, and computational modeling. Such tools enable better understanding of vector biology and facilitate the development of safer and more effective gene therapy products.Expand Specific Solutions
Leading Organizations in Gene Therapy Vector Development
The gene therapy viral entry and integration landscape is currently in a growth phase, with an estimated market size of $5-7 billion and projected annual growth of 25-30%. The technology is transitioning from early clinical applications to broader therapeutic implementation, though challenges in delivery mechanisms and safety profiles persist. Key players demonstrate varying levels of technical maturity: Oxford Biomedica leads with advanced lentiviral vector platforms, while Roche and Amicus Therapeutics have made significant investments in viral delivery systems. Emerging companies like CyGenica and GenomIdea are developing novel approaches to cellular entry. Academic institutions including Boston University and The Scripps Research Institute continue to drive fundamental research in viral vector design and integration mechanisms, creating a competitive ecosystem balancing established pharmaceutical companies with specialized biotechnology firms.
Oxford Biomedica (UK) Ltd.
Technical Solution: Oxford Biomedica has developed a proprietary lentiviral vector platform called LentiVector® that addresses key challenges in viral entry and integration for gene therapy. Their technology utilizes modified lentivirus vectors with pseudotyped envelope proteins (primarily VSV-G) to enhance tropism across multiple cell types while maintaining safety profiles. The platform incorporates self-inactivating (SIN) designs with deleted 3' LTR U3 regions to prevent mobilization after integration[1]. Their vectors feature internal promoters rather than LTR-driven expression, reducing the risk of insertional mutagenesis. Oxford Biomedica has engineered specific integration mechanisms that favor integration into active transcriptional units while avoiding promoter regions, significantly reducing oncogenic potential compared to gamma-retroviral vectors[2]. Their manufacturing process includes proprietary suspension culture systems that enhance scalability and consistency of vector production, critical for clinical applications requiring high-titer, purified vector preparations.
Strengths: Superior payload capacity (8-10kb) compared to AAV vectors; stable gene expression through genomic integration; reduced immunogenicity allowing for potential re-administration; demonstrated safety in multiple clinical trials. Weaknesses: Integration still carries theoretical insertional mutagenesis risk; manufacturing complexity and costs remain higher than some competing platforms; limited targeting specificity to particular cell types without additional engineering.
Hoffmann-La Roche, Inc.
Technical Solution: Roche has pioneered advanced viral entry mechanisms through their Antibody-Drug Conjugate (ADC) technology, which they've adapted for gene therapy applications. Their platform combines viral vectors with tissue-specific antibodies to enhance targeting precision. For viral entry, Roche employs a hybrid system utilizing both receptor-mediated endocytosis and membrane fusion mechanisms. Their proprietary "TRojan" technology incorporates modified envelope proteins with engineered furin cleavage sites that activate only in specific cellular environments, enhancing safety profiles[3]. For integration, Roche has developed a site-specific recombination system using engineered zinc-finger nucleases (ZFNs) that direct integration to predetermined genomic safe harbors, significantly reducing random integration events. This approach combines viral delivery efficiency with precise genomic modification capabilities. Their vectors incorporate insulator sequences that prevent interaction between vector promoters and neighboring genes, reducing the risk of activating proto-oncogenes[4]. Roche has also developed non-integrating lentiviral vectors for applications where transient expression is preferred, expanding their therapeutic range.
Strengths: Highly targeted delivery through antibody-directed tropism; reduced off-target effects; precise integration reduces insertional mutagenesis risk; versatile platform applicable to multiple disease indications. Weaknesses: Complex vector design increases manufacturing challenges and costs; potential immunogenicity of antibody components may limit repeat dosing; ZFN-mediated integration efficiency remains lower than natural viral integration mechanisms in some cell types.
Critical Patents in Viral Entry and Integration
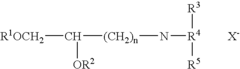
Expression of exogenous polynucleotide sequences in a vertebrate
PatentInactiveUS20040023911A1
Innovation
- Introducing naked polynucleotides, such as DNA or RNA sequences, directly into the interstitial space of tissues to be taken up by cells, allowing for controlled expression of polypeptides, thereby avoiding integration into the genome and eliciting targeted immune responses without systemic side effects.
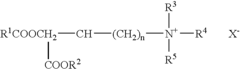
Targeted gene delivery to non-phagocytic mammalian cells via bacterially derived intact minicells
PatentWO2005056749A2
Innovation
- The use of bispecific ligands that specifically bind to both bacterial minicells and non-phagocytic mammalian cell surface structures, enabling targeted delivery of therapeutic nucleic acids into these cells by facilitating receptor-mediated endocytosis and ensuring sufficient payload release and expression.
Safety and Immunogenicity Considerations
Safety and immunogenicity considerations represent critical challenges in the development of viral vectors for gene therapy applications. The immune response to viral vectors can significantly impact both the safety profile and therapeutic efficacy of gene therapy constructs. Innate immune responses, including the activation of pattern recognition receptors (PRRs) such as Toll-like receptors (TLRs) and cytosolic DNA sensors, can be triggered by viral capsid proteins or nucleic acids, leading to the production of pro-inflammatory cytokines and interferons.
Adaptive immune responses pose additional challenges, particularly pre-existing neutralizing antibodies against common viral vectors like adeno-associated virus (AAV) and adenovirus. These antibodies, present in a significant percentage of the human population due to natural exposure, can rapidly neutralize administered vectors, preventing successful transduction of target tissues. Furthermore, cellular immune responses against viral capsid proteins or transgene products can lead to the elimination of transduced cells, limiting therapeutic durability.
Vector-related toxicity manifests through various mechanisms, including direct cellular damage from viral proteins, insertional mutagenesis with integrating vectors, and off-target effects. Lentiviral and retroviral vectors, which integrate into the host genome, carry the risk of insertional oncogenesis through activation of proto-oncogenes or disruption of tumor suppressor genes. This risk has been observed in clinical trials for X-linked severe combined immunodeficiency (X-SCID), where integration near the LMO2 proto-oncogene led to leukemia development in some patients.
Strategies to mitigate immunogenicity include vector engineering approaches such as capsid modification to reduce recognition by neutralizing antibodies, use of tissue-specific promoters to limit transgene expression to target cells, and incorporation of microRNA target sequences to prevent expression in antigen-presenting cells. Transient immunosuppression during vector administration has shown promise in reducing anti-vector immune responses.
Regulatory considerations for safety assessment have evolved significantly, with comprehensive guidelines established by agencies like the FDA and EMA. These include rigorous testing for replication-competent viruses, characterization of integration profiles for integrating vectors, and long-term follow-up studies to monitor for delayed adverse events. The implementation of suicide genes or inducible systems that allow for selective elimination of transduced cells represents an additional safety feature being incorporated into modern vector designs.
Recent advances in non-viral delivery systems and genome editing technologies offer potential alternatives that may circumvent some immunogenicity concerns associated with viral vectors, though these approaches present their own unique safety considerations that require thorough evaluation.
Adaptive immune responses pose additional challenges, particularly pre-existing neutralizing antibodies against common viral vectors like adeno-associated virus (AAV) and adenovirus. These antibodies, present in a significant percentage of the human population due to natural exposure, can rapidly neutralize administered vectors, preventing successful transduction of target tissues. Furthermore, cellular immune responses against viral capsid proteins or transgene products can lead to the elimination of transduced cells, limiting therapeutic durability.
Vector-related toxicity manifests through various mechanisms, including direct cellular damage from viral proteins, insertional mutagenesis with integrating vectors, and off-target effects. Lentiviral and retroviral vectors, which integrate into the host genome, carry the risk of insertional oncogenesis through activation of proto-oncogenes or disruption of tumor suppressor genes. This risk has been observed in clinical trials for X-linked severe combined immunodeficiency (X-SCID), where integration near the LMO2 proto-oncogene led to leukemia development in some patients.
Strategies to mitigate immunogenicity include vector engineering approaches such as capsid modification to reduce recognition by neutralizing antibodies, use of tissue-specific promoters to limit transgene expression to target cells, and incorporation of microRNA target sequences to prevent expression in antigen-presenting cells. Transient immunosuppression during vector administration has shown promise in reducing anti-vector immune responses.
Regulatory considerations for safety assessment have evolved significantly, with comprehensive guidelines established by agencies like the FDA and EMA. These include rigorous testing for replication-competent viruses, characterization of integration profiles for integrating vectors, and long-term follow-up studies to monitor for delayed adverse events. The implementation of suicide genes or inducible systems that allow for selective elimination of transduced cells represents an additional safety feature being incorporated into modern vector designs.
Recent advances in non-viral delivery systems and genome editing technologies offer potential alternatives that may circumvent some immunogenicity concerns associated with viral vectors, though these approaches present their own unique safety considerations that require thorough evaluation.
Regulatory Framework for Gene Therapy Vectors
The regulatory landscape for gene therapy vectors has evolved significantly over the past three decades, reflecting the growing understanding of viral entry mechanisms and integration processes. The U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) have established comprehensive frameworks that govern the development, testing, and approval of gene therapy products. These frameworks specifically address safety concerns related to viral vector design, including the potential for insertional mutagenesis and immunogenicity.
Current regulatory guidelines require extensive characterization of viral vector components, including capsid proteins that facilitate cellular entry and genetic elements that control integration. For AAV vectors, which predominantly remain episomal, regulatory focus centers on capsid serotype selection and manufacturing consistency. In contrast, lentiviral vectors, which integrate into the host genome, face more stringent oversight regarding integration site preferences and long-term safety monitoring.
The International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) has developed specific guidelines for viral vector-based therapies, emphasizing the need for standardized testing protocols to assess vector purity, potency, and safety. These guidelines mandate detailed analysis of vector tropism and transduction efficiency across different tissue types, directly addressing the mechanisms of viral entry.
Regulatory bodies have implemented tiered risk assessment approaches based on vector type and integration profile. Non-integrating vectors like AAV generally face fewer regulatory hurdles compared to integrating vectors like lentiviruses or retroviruses. This distinction acknowledges the fundamental differences in how these vectors interact with host cells and chromosomes.
Recent regulatory developments have focused on establishing clear pathways for novel vector designs that incorporate synthetic biology approaches to modify viral entry mechanisms. The FDA's Cellular, Tissue, and Gene Therapies Advisory Committee has issued specific recommendations for engineered viral capsids and non-viral delivery systems, recognizing the rapid innovation in this field.
Global harmonization efforts are underway to standardize regulatory requirements across different jurisdictions, particularly regarding vector characterization and integration site analysis. The World Health Organization has established an expert committee on biological standardization that provides international reference materials for gene therapy vector testing, facilitating consistent quality assessment worldwide.
Regulatory compliance now requires implementation of advanced analytical methods to monitor vector biodistribution and persistence, with particular emphasis on understanding the fate of vector genomes following administration. These requirements directly inform vector design strategies aimed at optimizing cellular entry while minimizing off-target effects and integration-related risks.
Current regulatory guidelines require extensive characterization of viral vector components, including capsid proteins that facilitate cellular entry and genetic elements that control integration. For AAV vectors, which predominantly remain episomal, regulatory focus centers on capsid serotype selection and manufacturing consistency. In contrast, lentiviral vectors, which integrate into the host genome, face more stringent oversight regarding integration site preferences and long-term safety monitoring.
The International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) has developed specific guidelines for viral vector-based therapies, emphasizing the need for standardized testing protocols to assess vector purity, potency, and safety. These guidelines mandate detailed analysis of vector tropism and transduction efficiency across different tissue types, directly addressing the mechanisms of viral entry.
Regulatory bodies have implemented tiered risk assessment approaches based on vector type and integration profile. Non-integrating vectors like AAV generally face fewer regulatory hurdles compared to integrating vectors like lentiviruses or retroviruses. This distinction acknowledges the fundamental differences in how these vectors interact with host cells and chromosomes.
Recent regulatory developments have focused on establishing clear pathways for novel vector designs that incorporate synthetic biology approaches to modify viral entry mechanisms. The FDA's Cellular, Tissue, and Gene Therapies Advisory Committee has issued specific recommendations for engineered viral capsids and non-viral delivery systems, recognizing the rapid innovation in this field.
Global harmonization efforts are underway to standardize regulatory requirements across different jurisdictions, particularly regarding vector characterization and integration site analysis. The World Health Organization has established an expert committee on biological standardization that provides international reference materials for gene therapy vector testing, facilitating consistent quality assessment worldwide.
Regulatory compliance now requires implementation of advanced analytical methods to monitor vector biodistribution and persistence, with particular emphasis on understanding the fate of vector genomes following administration. These requirements directly inform vector design strategies aimed at optimizing cellular entry while minimizing off-target effects and integration-related risks.
Unlock deeper insights with Patsnap Eureka Quick Research — get a full tech report to explore trends and direct your research. Try now!
Generate Your Research Report Instantly with AI Agent
Supercharge your innovation with Patsnap Eureka AI Agent Platform!